Abstract
Management of a solitary pancreatic pseudocyst with endoscopic transpapillary stent drainage is a well recognized treatment modality. Endoscopic options are however limited in the presence of multiple pancreatic pseudocysts. Conventionally surgery has been the mainstay of treatment in this situation. In this case report, we present a patient with multiple pancreatic pseudocysts who was successfully treated via transpapillary placement of pancreatic duct stent.
Key words: pancreatic pseudocyst, endoscopy.
Introduction
Multiple pancreatic pseudocysts occur in 5-20% of all patients with pseudocysts, most often in the setting of chronic pancreatitis.1 In comparison with solitary pseudocysts, they are more symptomatic, less likely to regress spontaneously and are more difficult to treat.1 Such a patient ends up being a candidate for surgical drainage of the pseudocysts with minimal application of endoscopic techniques. However, with increasing experience using endoscopic techniques and better equipment availability, the role of endoscopy in multiple pseudocysts needs to be explored. We present here a patient with alcoholic pancreatitis with several pseudocysts that resolved completely with transpapillary drainage.
Case Report
Our patient is a 44-year old African American lady who presented to the emergency room with acutely worsened abdominal pain on a background of several week history of chronic abdominal pain associated with nausea and vomiting. Patient had a history of alcohol abuse. She had a laparoscopic cholecystectomy done 10 years prior for acute calculous cholecystitis. A computed tomography (CT) scan was performed which showed multiple pseudocysts in relation to the body and tail of pancreas (Figure 1). Pancreatic enzymes, amylase and lipase, were borderline abnormal. She was diagnosed with alcohol induced pancreatitis complicated with pseudocysts. In view of symptomatic mature pseudocysts, a drainage procedure was mandated. Endoscopic retrograde pancreatogram was performed which showed a markedly dilated pancreatic duct and filling of a saccular structure inferior to the pancreatic tail, consistent with a visible communication with the cyst(s) (Figure 2). We attempted transpapillary drainage of the cystic spaces through placement of a 5 French×7 cm (Cook Medical, Limerick, Ireland) pancreatic duct stent. Patient did well post-procedure and was discharged home after 72 h with good pain control.
Figure 1.
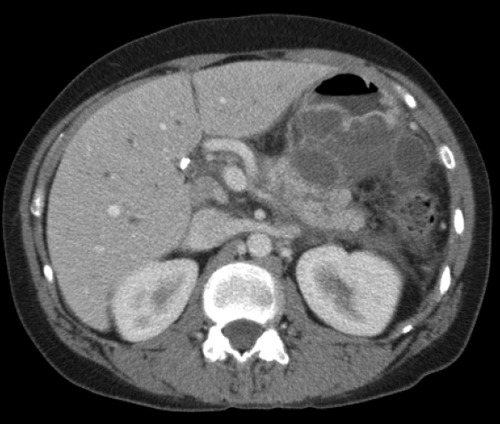
Computed tomography scan showing several pancreatic pseudocysts in relation to the body and tail of pancreas.
Figure 2.
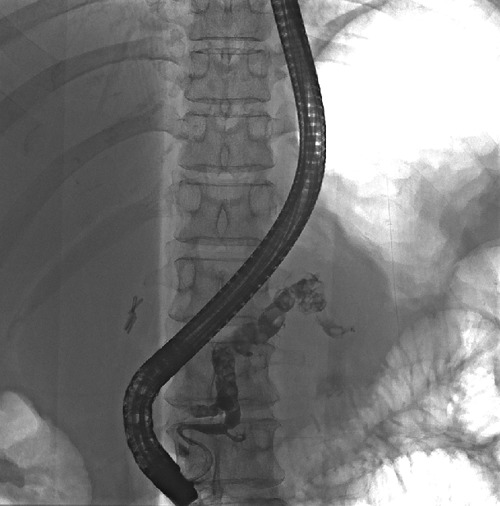
Endoscopic retrograde cholangiopancreatography showing filling of a saccular structure inferior to the pancreatic tail consistent with a visible connection with a pseudocyst.
Two weeks later the patient was readmitted with high fevers and worsening abdominal pain. A repeat endoscopic pancreatogram showed a dilated pancreatic duct in the body of pancreas with tapering in the region of head, suggesting occlusion of the stent. This was treated by balloon dilatation and replacement with a single pigtail stent, 5 French×10 cm (Cook Medical) in the pancreatic duct. Postprocedure, the patient recovered well with 7 day antibiotic treatment. A follow up CT scan after 3 and 6 months showed significant resolution in the pseudocysts (Figures 3 and 4) with remarkable improvement in symptoms of abdominal pain. Patient was referred to the deaddiction clinic to prevent further attacks of alcoholic pancreatitis.
Figure 3.
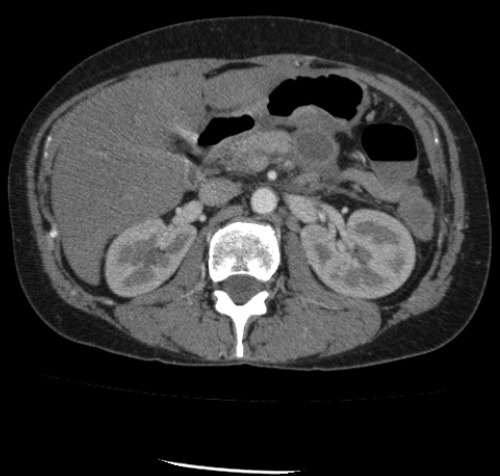
Computed tomography scan showing significant resolution of pancreatic pseudocysts 3 months post stent placement.
Figure 4.
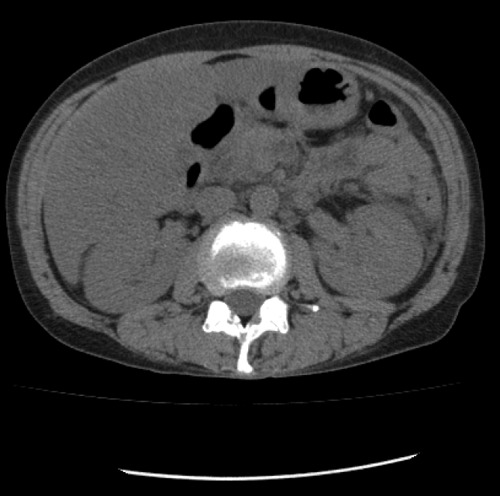
Computed tomography scan showing significant resolution of pancreatic pseudocysts 6 months post stent placement.
Discussion
The various modalities available for treatment of pancreatic pseudocyst include endoscopic transgastric or transpapillary drainage, percutaneous drainage and surgical cystogastrostomy or cystoenterostomy. Percutaneous drainage is usually indicated in the setting of an infection. When performed, recurrence rates as high as 60% are seen and treatment is often complicated by a pancreatic fistula.2 Surgical drainage procedures, although very effective, have been reported to have a morbidity of 16% and a mortality of 2.5%.3 Therefore, it is not surprising that the role of surgery for drainage of pseudocysts has become less prominent. If feasible, use of endoscopic techniques is preferable and should be attempted as the first line treatment for management of pancreatic pseudocyst. This approach is minimally invasive and predisposed to the least post-procedural complications.3
Transpapillary drainage is a relatively newer endoscopic method in which an internal stent is left in situ in the pancreatic duct permitting adequate drainage of the pancreatic pseudocyst. This technique has been reported to be successful when i) pseudocyst is less than 7 cm in size, ii) there is evidence of pancreatic duct obstruction and iii) pseudocyst communicates with the pancreatic duct.4 The technique involves first performing a pancreatogram to confirm the above characteristics and subsequently cannulating the pancreatic duct with a stent over a guide wire. The stent is left in place for an average of 3 months or until pseudocyst resolution is confirmed on imaging. Nevertheless transpapillary drainage is not without its complications. There is documented high risk of infection when transpapillary drainage alone is used for treatment.5 However the recent literature indicates that perhaps with advancing techniques infection rates have been decreasing.4-8 Stent occlusion is another limitation which required re-intervention as seen in our patient. Another complication to consider is that the pancreatic duct stent may induce long term changes in duct and pancreatic parenchyma.9 Though these changes may been seen in over 35% of patients who undergo stenting, it seems the majority of the changes improve with time after removal of the stent.9
Historically, the outcomes of endoscopic modalities have not been very encouraging in the setting of multiple pseudocysts. Surgical drainage is often required due to high recurrence rates when managed endoscopically.
There is however recent evidence that endoscopic techniques may be effective in the treatment of multiple pancreatic pseudocysts as well.4,6,7 Smits et al. reported on the endoscopic drainage of 12 patients with multiple pancreatic pseudocysts by endoscopic techniques including - transpapillary, cystogastrostomy and cystoduodenostomy.10 Six out of the 12 patients had complete resolution of the pseudocyst. Authors concluded that the size or number of pseudocysts did not impact the outcome of drainage procedure. Barthet et al. also described endoscopic transpapillary drainage in 5 patients who had multiple pseudocysts with good success.6
Conclusions
The index case reported here illustrates that endoscopic transpapillary drainage is a feasible, safe and effective alternative to surgery in patients with multiple, communicating pancreatic pseudocysts. In our patient, the follow up CT scan showed significant clinical and radiological improvement. For endoscopic management to be successful, patient selection is paramount. Lack of expertise may be another limiting factor in widespread implementation of this technique. If available, it may be a useful approach in the armamentarium for treating multiple pancreatic pseudocysts.
References
- 1.Fedorak IJ, Rao R, Prinz RA. The clinical challenge of multiple pancreatic pseudocysts. Am J Surg 1994;168:22-8 [DOI] [PubMed] [Google Scholar]
- 2.Heider R, Meyer AA, Galanko JA, Behrns KE. Percutaneous drainage of pancreatic pseudocysts is associated with a higher failure rate than surgical treatment in unselected patients. Ann Surg 1999;229: 781-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lerch M, Stier A, Wahnschaffe U, Mayerle J. Pancreatic pseudocysts: observation, endoscopic drainage, or resection? Dtsch Arztebl Int 2009;106:614-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hookey LC, Debroux S, Delhaye M, et al. , Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Gastrointest Endosc 2006;63: 635-43 [DOI] [PubMed] [Google Scholar]
- 5.Delhaye M, Matos C, Deviere J. Endoscopic management of chronic pancreatitis. Gastrointest Endosc Clin N Am 2003;13: 717-42 [DOI] [PubMed] [Google Scholar]
- 6.Barthet M, Sahei J, Bodiou-Bertei C, Bernard JP. Endoscopic transpapillary drainage of pancreatic pseudocysts. Gastrointest Endosc 1995;42:208-13 [DOI] [PubMed] [Google Scholar]
- 7.Catalano M, Raijman I, Nayar R. Endoscopic drainage of patients presenting with multiple pancreatic pseudocysts (abstract). Gastroenterology 1999;98:A1115 [Google Scholar]
- 8.Bhasin DK, Rana SS, Udawat HP, et al. Management of multiple and large pancreatic pseudocysts by endoscopic transpapillary nasopancreatic drainage alone. Am J Gastroenterol 2006;101:1780-6 [DOI] [PubMed] [Google Scholar]
- 9.Sherman S, Hawes RH, Savides TJ, et al. Stent induced pancreatic ductal and parenchymal changes: correlation of endoscopic ultrasound with ERCP. Gastrointest Endosc 1996;44:276-82 [DOI] [PubMed] [Google Scholar]
- 10.Smits ME, Rauws EA, Tytgat GN, Huibregtse K. The efficacy of endoscopic treatment of pancreatic pseudocysts. Gastrointest Endosc 1995;42:202-7 [DOI] [PubMed] [Google Scholar]


