Abstract
The aims and objectives of this study were: i) to evaluate the efficacy of computed tomography (CT) imaging in diagnosing the presence, level, degree, and cause of intestinal obstruction, and the role of CT in detecting presence of complications; ii) to assess impact of CT in decision making and management (surgical/conservative); iii) to correlate CT findings with intra operative findings whenever possible. A prospective study of 40 patients presented in outpatient/emergency department with features suggestive of intestinal obstruction. Multislice contrast enhanced computed tomography of whole abdomen was done in all patients after preliminary investigations. Whenever indicated, patients were explored. Statistical analysis was performed to determine the efficacy of multidetector computed tomography (MDCT) in diagnosing intestinal obstruction and its complications. Out of 40, 30 patients underwent exploratory laparotomy and it was found that MDCT was 85% sensitive and 70% specific in diagnosing bowel obstruction. Association between MDCT findings suggestive of obstruction and intra-operative findings turn out to be significant (P=0.003). MDCT findings were consistent with intraoperative findings in 22 out of 30 patients (73%). MDCT is sensitive and specific in determining the presence of bowel obstruction and should be recommended for patients with suspected bowel obstruction because it affects outcome in these patients.
Key words: intestinal obstruction, multidetector computed tomography, conservative management, laparotomy
Introduction
Bowel obstruction was recognized, described and treated by Hippocrates. The earliest recorded operation as treatment was performed by Praxagoras circa 350 BC, when he created an enterocutaneous fistula to relieve the obstruction of a segment of bowel.1 On plain supine and upright radiographs of the abdomen, the cardinal findings that suggest the diagnosis of small bowel obstruction are the accumulation of air and fluid proximal to the point of obstruction and clearance or absence of fluid and air distal to the obstruction. On ultrasonography, bowel obstruction is considered to be present when dilated loop measures >2.5 cm and length of segment is >10 cm. The etiology can sometimes be determined, but ultrasonography is less accurate than computed tomography (CT). When dilute barium is used for the luminal contrast, the obstructing segment can usually be localized and characterized as complete or incomplete,2 just as with oral contrast radiography. Unlike oral contrast radiography, which provides imaging of only the luminal surface, CT allows imaging of the abdominal contents outside the lumen. Because of this advantage, the nature of the obstruction, especially when secondary to an extraluminal or intramural malignant process, can be established.3 Additional abdominal pathology, such as the presence of nodal or liver metastases, ascites, and solidorgan parenchymal abnormalities, can often be identified, thereby helping to define the cause of the obstruction.
Abdominal ultrasound, small bowel follow through, and enteroclysis are being superseded by CT for more rapid and more accurate diagnosis. Non-visualization of oral contrast in the colon on CT 12 h after administration is a reliable indicator of complete obstruction, whereas visualization of oral contrast in the colon indicates incomplete small bowel obstruction. In a meta-analysis, conventional CT had a sensitivity of 92% (range 81-100%) and specificity of 93% (range 68-100%) in detecting complete obstruction.4 Intravenous contrast helps in diagnosing strangulation, in identifying the specific cause of small bowel obstruction and in characterizing other pathology such as superior mesenteric artery or superior mesenteric vein thrombosis, which can produce an ileus that mimics mechanical obstruction.5
This prospective study group comprised of 40 patients who presented clinically as intestinal obstruction and were selected according to inclusion and exclusion criteria. All patients underwent multidetector computed tomography (MDCT) of abdomen. As most of the reported studies were retrospective, the effective role and impact of MDCT on diagnosis and management of bowel obstruction still remains to be explored further. The purpose of our prospective study was to determine whether MDCT is superior to the traditional clinical-radiographic methods of diagnosing bowel obstruction.
Materials and Methods
Study design
This was a single centre prospective follow up study. Following confirmation of eligibility, 40 patients with intestinal obstruction were included in the study. After preliminary hematological and radiological investigation viz (complete hemogram, random blood sugar, blood urea, serum electrolytes, x-ray chest and abdomen, ultrasound abdomen), patients were then subjected to MDCT of abdomen. In this study, we used multislice (16 slice) Siemens (EMOTION; Siemens AG Healthcare Sector, Erlangen, Germany) CT scanner. The patients were given 720 mL of 1.5% water soluble contrast medium orally 2 h prior to the scanning. Then a bolus dose of intra venous contrast medium with 35-40 gm of iodine was given. CT scanning of entire abdomen and pelvis was done with contiguous axial 10 mm sections with pitch of 1-1.5. The protocol was approved by the Ethical Review Board of the hospital. According to the principles of the declaration of Helsinki 1975, written, informed consent was obtained from all participants.
Participants
All the patients presented in surgical outpatient department as well as the emergency, with complaints suggestive of intestinal obstruction were assessed, 50 enrolled, 10 excluded. Inclusion criteria were- all patients who reported to emergency or outpatient department (OPD), who clinically presented as intestinal obstruction, patients diagnosed of having intestinal obstruction by conventional methods (ultrasonography/x-ray abdomen). Exclusion criteria were: severely decompensated patients, pregnancy, patients with deranged kidney function test, and patients below 14 years of age.
Statistical analysis
Statistical analysis was performed using Pearson’s chi-squared test as applicable. Chisquared test was performed on categorical variables to test their associations. The level of significance was set at P<0.05.
Specificity, sensitivity, positive and negative predictive values and P value of different parameters were calculated.
Results
General characteristics
Out of 40 patients, 27 were males (67 %), and 13 were females (33%). There were 11 (27%) patients between the age 15 and 30 years, 13 (33%) patients between the age 31 and 45 years, 12 (30%) patients between the age 46 and 60 years, and 4 (10%) patients above 60 years of age.
Distribution of clinical symptoms and signs
A percentage of 100 patients had pain abdomen while distension, vomiting and constipation/ obstipation were present in decreasing order. Tachycardia was the most common sign seen in patients (80%) followed by abdominal tenderness, absent or exaggerated bowel sounds, and guarding (Figures 1 and 2).
Figure 1.
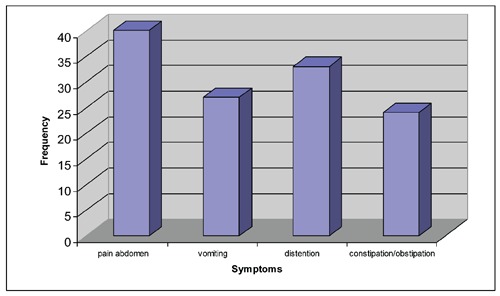
Showing distribution of clinical symptoms [pain abdomen (100%), vomiting (67.5%), distension (82.5%), constipation/ obstipation (60%)].
Figure 2.
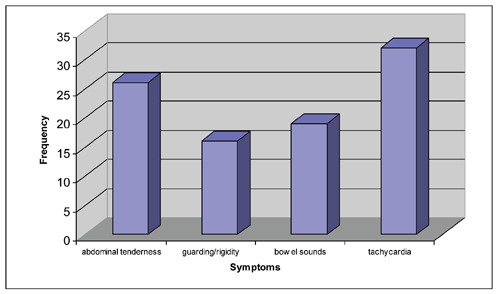
Showing distribution of clinical signs [abdominal tenderness (65%), guarding/rigidity (40%), bowel sounds (47.5%), tachycardia (80%)].
Comparison of x-ray and computed tomography scan for diagnosis of bowel obstruction
Since the P value of the test is 0.009 (<0.05), therefore the association between xray and CT findings for diagnosis of obstruction is significant. As shown in Tables 1 and 2 there is a 30/38=78.95% of agreement between both the investigations and 8/38=21.05% disagreement. Since the P value is significant, we conclude that this percentage of disagreement is insignificant.
Table 1.
X-ray (dilated bowel loop/multiple air fluid level) versus computed tomography finding presence of obstruction: cross tabulation.
| CT finding-presence of obstruction | Total | ||
|---|---|---|---|
| No | Yes | ||
| X-ray (dilated bowel loop/multiple air fluid level) | |||
| No | 7 | 4 | 11 |
| Yes | 4 | 23 | 27 |
| Total | 11 | 27 | 38 |
CT, computed tomography.
Table 2.
X-ray (dilated bowel loop/multiple air fluid level) versus computed tomography finding presence of obstruction: Pearson’s chi-squared test.
| Value | df | Asymptomatic sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson’s chi-squared test | 9.057* | 1 | 0.003 | - | - |
| Continuity correction° | 6.839 | 1 | 0.009 | - | - |
| Likelihood ratio | 8.655 | 1 | 0.003 | - | - |
| Fisher’s exact test | - | - | - | 0.005 | 0.005 |
| Linear-by-linear association | 8.819 | 1 | 0.003 | - | - |
| No. of valid cases | 38 | - | - | - | - |
df, degree of freedom; sig., significance. 1 cell (25.0%) has expected count less than 5. The minimum expected count is 3.18; °computed only for a 2x2 table.
X-ray (dilated bowel loop/multiple air fluid level) versus per-operative obstruction
Since the P value of the test is 0.240 (>0.05), which is insignificant so the association between x-ray and per-operative findings for diagnosis of obstruction is insignificant. As we can see from Tables 3 and 4 there is a 18/28=64.28% of agreement between both the investigations and 10/28=35.71% disagreement. Since the P value is insignificant, we conclude that this percentage of disagreement is significant.
Table 3.
X-ray (dilated bowel loop/multiple air fluid level) versus per-operative obstruction: cross tabulation.
| Per-operative obstruction | Total | ||
|---|---|---|---|
| No | Yes | ||
| X-ray (dilated bowel loop/multiple air fluid level) | |||
| No | 5 | 5 | 10 |
| Yes | 5 | 13 | 18 |
| Total | 10 | 18 | 28 |
Table 4.
X-ray (dilated bowel loop/multiple air fluid level) versus per-operative obstruction: Pearson’s chi-squared test.
| Value | df | Asymptomatic sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson’s chi-squared test | 1.383* | 1 | 0.240 | - | - |
| Continuity correction° | 0.584 | 1 | 0.445 | - | - |
| Likelihood ratio | 1.365 | 1 | 0.243 | - | - |
| Fisher’s exact test | - | - | - | 0.412 | 0.221 |
| Linear-by-linear association | 1.333 | 1 | 0.248 | - | - |
| No. of valid cases | 28 | - | - | - | - |
df, degree of freedom; sig., significance.*1 cell (25.0%) has expected count less than 5. The minimum expected count is 3.57; °computed only for a 2x2 table.
Computed tomography findings suggestive of obstruction versus per-operative obstruction
Tables 5 and 6 show agreement in 24/30=80% patients and disagreement in 6/30=20% of patients. On application of chisquared test P value is 0.003, which is insignificant for disagreement.
Table 5.
Computed tomography findings suggestive of obstruction versus per-operative obstruction: cross tabulation.
| Per-operative obstruction | Total | ||
|---|---|---|---|
| No | Yes | ||
| CT finding-presence of obstruction | |||
| No | 7 | 3 | 10 |
| Yes | 3 | 17 | 20 |
| Total | 10 | 20 | 30 |
CT, computed tomography.
Computed tomography severity versus per-operative severity
Tables 7 and 8 show comparison of severity of obstruction made by CT scan vs severity found intra-operatively. The agreement between these two is 14/17=82.35% and disagreement is 3/17=17.64%. P value is 0.013 significant for disagreement, it is concluded that association between these two is insignificant.
Table 7.
Computed tomography severity versus per-operative severity: cross tabulation.
| Per-operative obstruction | Total | ||
|---|---|---|---|
| Partial | Compete | ||
| CT finding-presence of obstruction | |||
| Partial | 10 | 2 | 12 |
| Complete | 1 | 4 | 5 |
| Total | 11 | 6 | 17 |
CT, computed tomography.
Table 8.
Computed tomography severity versus per-operative severity: Pearson’s chisquared test.
| Value | df | Asymptomatic sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson’s chi-squared test | 6.199 | 1 | 0.013 | - | - |
| Continuity correction* | 3.736 | 1 | 0.053 | - | - |
| Likelihood ratio | 6.257 | 1 | 0.012 | - | - |
| Fisher’s exact test | - | - | - | 0.028 | 0.028 |
| Linear-by-linear association | 5.834 | 1 | 0.016 | - | - |
| No. of valid cases | 17 | - | - | - | - |
df, degree of freedom; sig., significance. *Computed only for a 2x2 table.
Table 9 shows statistical values of CT scan in bowel obstruction. In this study, the sensitivity and specificity of CT scan bowel obstruction were 85% and 70% respectively.
Table 9.
Statistical values of computed tomography scan in bowel obstruction.
| Values | Percentage 1 |
|---|---|
| Sensitivity | 85 |
| Specificity | 70 |
| Predictive value of positive test | 85 |
| Predictive value of negative test | 70 |
| % of false negative | 15 |
| % of false positive | 30 |
Discussion
Several studies have shown the accuracy of MDCT scan in diagnosis of bowel obstruction. However, as most of these studies were retrospective, the effective role and impact of MDCT on diagnosis and management of bowel obstruction still remains to be explored further. The purpose of our prospective study was to determine whether MDCT is superior to the traditional clinical-radiographic evaluation in establishing the etiology, diagnosis and severity in cases of suspected obstruction of the small bowel and to see what impact this information has on treatment. We have considered exploratory laparotomy as the gold standard.
Our study group comprised of 40 patients, who presented in emergency or OPD. All the patients had pain in abdomen while vomiting, distention and constipation/obstipation were present in 67.5%, 82.5% and 60% patients respectively. On clinical examination tenderness was found in 65% of patients, guarding/rigidity in 40% of patients and 80% of them had tachycardia. All patients had their MDCT scan done and x-ray was done in 38 patients. On applying chi-squared test P value was 0.003, which suggests association between x-ray and MDCT scan findings for presence of obstruction. Findings of the x-ray correlated with the MDCT in 78.95%, whereas there was no correlation in 21.05%. Out of total 40 patients, 30 were taken for exploratory laparotomy and 10 patients were managed conservatively. Out of these 30 patients considered for exploratory laparotomy, 20 patients had pre-operative diagnosis of intestinal obstruction confirmed by MDCT scan while rest of the 10 patients were taken up for laparotomy due to inability to show symptomatic improvement on conservative management, although preoperative CT was not consistent with diagnosis of intestinal obstruction. Out of 20 patients with pre-operative diagnosis of intestinal obstruction on MDCT, 17 had per-operative finding consistent with intestinal obstruction, however, 3 patients turned out to be negative for intestinal obstruction on laparotomy. 1 patient had passable stricture of ileum while 2 patients had adhesions of small bowel without causing obstruction. Ten patients were explored for intestinal obstruction due to inability to respond to conservative management, 3 patients had per-operative findings consistent with intestinal obstruction. The causes of obstruction in these 3 patients were adhesions in 2 and stricture in 1 patient. In rest of 7 patients, laparotomy revealed no evidence of obstruction. The per-operative findings in these patients were appendicitis in 3, passable stricture in 1, pancreatitis in 1, adhesions in 1, and bilioma in 1 patient. On statistical analysis, intra-operative findings were in agreement with MDCT scan in 80% of cases only. P value for this association is 0.003 (<0.05) that is significant. In 3 out of 4 patients, the sign of ischemia as seen on MDCT scan were found to be present on exploration. It occurs in about 10% of patients with small bowel obstruction and has a mortality rate of 10-37%.6 In these patients, the draining mesenteric veins are occluded first, leading to severe congestive failure affecting the wall of bowel and mesentery. Increased venous and capillary pressure leads to edema, rupture of small vessels and intramural and mesenteric hemorrhage. Arterial insufficiency usually follows, aggravating anoxia and further contributing to the rapid development of ischemia, infarction and perforation. Strangulation is more common with adhesions, internal or external hernias. Occasionally, it may develop as a consequence of an idiopathic small bowel volvulus without associated intraperitoneal abnormality. A definite distinction should always be made between closed loop obstruction and ischemia. These are related phenomena but separate pathologic entities. Strangulation always develops because of a closed loop; however, a closed loop may not be associated with strangulation and can resolve spontaneously. The MDCT signs of strangulation like those of intestinal ischemia include: a thickened bowel wall due to edema, inflammation, or intramural hemorrhage; mural thumb printing from intramural hemorrhage or edema; pneumatosis intestinalis from intramural gas produced by bacteria; absence of enhancement with intramural contrast because of vascular hypoperfusion; hazy or streaky mesentery or dirty fat from inflammatory infiltration; portal venous gas; target sign; and ascitis5 is occasionally present.
In this study, 7 (24.13%) patients showed adhesions as cause of obstruction on MDCT scan. 3 of them were managed conservatively, while per-operatively impassable stricture was seen in 1 patient and in other 2 patients, adhesions without causing obstruction were seen during laparotomy. For diagnosis of obstruction due to adhesions, an indirect diagnosis of adhesive obstruction was entertained when no mass or apparent cause was noted in the transition zone from dilated to non-dilated bowel. Frager et al.7 found adhesions as cause of intestinal obstruction in 75% of cases. In developing countries including India, adhesions are less common cause of intestinal obstruction as compared to developed countries. In 3 (10.34%) patients, hernia was found as cause of obstruction on CT scan. Out of these 3 patients, 1 patient had internal hernia on MDCT. On laparotomy, band was the cause of obstruction in this patient. The other 2 cases were obstructed inguinal hernia and obstructed umbilical hernia. Miller et al.8 in their study found hernia as cause of intestinal obstruction in 15% patients. Due to increasing trend towards early surgical intervention in hernia cases, the incidence of hernia as the cause of obstruction is declining.
In one patient, small bowel volvulus was diagnosed on MDCT due to presence of whirl sign. In another patient, malrotation of gut was diagnosed on MDCT scan which was confirmed on exploration. 1 case was diagnosed pre-operatively as ileocolic intussusceptions with lipoma as the leading point on MDCT scan. Exploratory laparotomy revealed findings consistent with MDCT scan. Intussusception in adults is a relatively rare condition that accounts for less than 5% of cases of bowel obstruction.9 In contrast to cases involving infants, 80% of the cases are associated with underlying causes such as neoplasm, adhesion, inverted Meckel’s diverticulum, foreign body, and prior history of abdominal surgery.10 MDCT depicts the collapsed, intussuscepted proximal bowel with mesenteric fat and vessels lying within the wall of the distal bowel. On cross-sectional images, the intussusception has a target-like appearance. The underlying lesion may also be observed as the leading point.11
Gossypiboma is an iatrogenic cause of intestinal obstruction formed due to abdominal sponge left inadvertently during surgery. It appears as extensive heterogeneous mass with surrounding mesenteric inflammation on MDCT scan. In our study, one patient was diagnosed as having gossypiboma in right iliac fossa on CT scan. This patient was referred to us from some other institution after surgery, as patient was not improving post-operatively. On exploration, the offending sponge was removed and patient had uneventful recovery.
In this study, sensitivity and specificity of MDCT scan for diagnosis of bowel obstruction came out to be 85% and 70% respectively. Mallo et al.4 in 2005 stated in their review that sensitivity of MDCT scan in diagnosing bowel obstruction ranges between 81-100% and specificity between 68-100% which is consistent with our results. However other authors have reported sensitivity and specificity of MDCT scan in diagnosis of bowel obstruction as high as 94% and 96% respectively.12,13 This discrepancy could be due to patient selection in these studies favoring patients with higher grades of obstruction. In low-grade obstruction, significance of mild or localized dilatation may be overlooked, adversely affecting the sensitivity and specificity of MDCT scan in diagnosis of bowel obstruction. Attention to this relatively subtle finding may increase the accuracy of MDCT scan in diagnosis of bowel obstruction.
On cross tabulation of severity of obstruction (partial/complete) on MDCT scan and peroperatively agreement was found in 82.35%. P value for this association was 0.013, which is significant. In 73.33% (22 out of 30) patients, the cause of obstruction as evident on MDCT scan was correctly matched with the cause found during exploratory laparotomy. In 3 out of 5 patients the signs of ischemia as seen on MDCT scan were found to be present during laparotomy.10 out of 30 patients, who underwent laparotomy were negative for presence of obstruction on pre-operative MDCT, in remaining 20 patients cause of obstruction could be matched in 13 (65%).
Peck et al.14 performed a retrospective study over a period of 1 year. Fifty-five patients had both computed tomography and small bowel follow-through studies. The gold standard for diagnosis was laparotomy in 42 patients and clinical follow-up in 13 patients. Thirty-six out of 42 patients had proven intestinal obstruction at the time of laparotomy. Computed tomography identified 32 out of the 36 highgrade and complete mechanical obstructions. Computed tomography was superior to small bowel follow-through in identifying masses, malignancies, and features of strangulation.
Maglinte et al.15 found reliability of abdominal CT in the assessment of varying degrees of small bowel obstruction by using enteroclysis and clinical outcome as standards of reference. A blinded retrospective analysis was performed of the studies of 55 patients who underwent both CT and enteroclysis. Nine patients had no obstruction, 40 patients had obstruction due to adhesions, and 6 patients had tumor-related obstruction. CT results were used to identify correctly 63% (29 of 46) of those who had small bowel obstruction and 78% (7 of 9) of the patients who did not. The overall accuracy of the CT interpretations to help establish diagnosis was 65% (36 of 55).
Daneshmand et al.16 in their study documented that plain films are a less sensitive and less specific method of diagnosing bowel obstruction. Study advised that CT scan should be considered as the primary test for patients with suspected bowel obstruction.
Conclusions
We conclude that: i) MDCT is highly sensitive and specific in determining the presence of bowel obstruction; ii) in addition to presence of obstruction MDCT also demonstrates the site and cause of obstruction; iii) MDCT has high sensitivity in diagnosing high-grade obstruction but has relatively low sensitivity in diagnosing low-grade obstruction; iv) patients with partial low grade obstruction can be treated conservatively initially unless an associated surgical lesion is detected on MDCT; v) MDCT should be recommended for patients with suspected bowel obstruction when clinical and conventional radiographic findings remain indeterminate or strangulation is suspected; vi) with contrast administration or by pointing out special type of bowel obstruction (i.e. closed loop obstruction) the possibility of associated strangulation can be assessed; vii) when MDCT is used with comprehensive approach it not only helps in making correct diagnosis but also affects outcome in patients with bowel obstruction.
Table 6.
Computed tomography findings suggestive of obstruction versus per-operative obstruction: Pearson’s chi-squared test.
| Value | df | Asymptomatic sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson’s chi-squared test | 9.075* | 1 | 0.003 | - | - |
| Continuity correction0 | 6.769 | 1 | 0.009 | - | - |
| Likelihood ratio | 9.065 | 1 | 0.003 | - | - |
| Fisher’s exact test | - | - | - | 0.005 | 0.005 |
| Linear-by-linear association | 8.772 | 1 | 0.003 | - | - |
| No. of valid cases | 30 | - | - | - | - |
df, degree of freedom; sig., significance. *1 cell (25.0%) has expected count less than 5. The minimum expected count is 3.33; °computed only for a 2x2 table.
References
- 1.Evers BM.Sabiston textbook of surgery. 18th ed Noida: Elsevier; 2009. p 1289 [Google Scholar]
- 2.Frager D, Medwin SW, Baer JW.CT of small bowel obstruction: value in establishing the diagnosis and determining the degree and cause. Am J Roentgenol 1994;162:37-41 [DOI] [PubMed] [Google Scholar]
- 3.Gazekke GS, Goldberg MA, Wittenberg J, Halpern EF.Efficacy of CT in distinguishing small-bowel obstruction from other causes of small-bowel dilatation. Am J Roentgenol. 1994; 162:43-7 [DOI] [PubMed] [Google Scholar]
- 4.Mallo RD, Salem R, Lalani T.Computed tomography diagnosis of ischemia and complete obstruction in small bowel obstruction: a systematic review. J Gastrointest Surg. 2005; 9:690-4 [DOI] [PubMed] [Google Scholar]
- 5.Frager D.Intestinal obstruction role of CT. Gastroenterol Clin North Am. 2002; 31:777-99 [DOI] [PubMed] [Google Scholar]
- 6.Sarr MG, Bulkley GB, Zuidema GD.Preoperative recognition of intestinal strangulation obstruction: prospective evaluation of diagnostic capability. Am J Surg. 1983; 145:176-82 [DOI] [PubMed] [Google Scholar]
- 7.Frager DH, Baer JW.Role of CT in evaluating patients with small-bowel obstruction. Semin Ultrasound CT MR. 1995; 16:127-40 [DOI] [PubMed] [Google Scholar]
- 8.Miller G, Boman J, Shrier I.Natural history of patients with adhesive small bowel obstruction. Br J Surg. 2000; 87:1240-7 [DOI] [PubMed] [Google Scholar]
- 9.Reijnen-Han AM, Joosten-Harrie JM, deBoer-Herman HM.Diagnosis and treatment of adult intussusception. Am J Surg 1989;158:25-8 [DOI] [PubMed] [Google Scholar]
- 10.Herlinger H, Rubesin SE, Morris JB.Small bowel obstruction. Gore RM, Levine MS, Textbook of gastrointestinal radiology. 2nd ed Philadelphia, PA: Saunders; 2000. pp 815-837 [Google Scholar]
- 11.Lorgan JG, DuBrow RA.The computed tomographic appearances and clinical significance of intussusception in adults with malignant neoplasms. Br J Radiol 1990;63:257-63 [DOI] [PubMed] [Google Scholar]
- 12.Megibow AJ, Balthazar EJ, Cho CK.Bowel obstruction: evaluation with CT. Radiology. 1991; 180:313-8 [DOI] [PubMed] [Google Scholar]
- 13.Fukuya T, Hawes D, Lu C.CT diagnosis of small-bowel obstruction: efficacy in 60 patients. Am J Roentgenol. 1992; 158:765-9 [DOI] [PubMed] [Google Scholar]
- 14.Peck JJ, Milleson T, Phelan J.The role of computed tomography with contrast and small bowel follow-through in management of small bowel obstruction. Am J Surg. 1999; 177:375-8 [DOI] [PubMed] [Google Scholar]
- 15.Maglinte DD, Ryes BL, Harmon BH.Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. Am J Roentgenol 1996;167:1451-5 [DOI] [PubMed] [Google Scholar]
- 16.Daneshmand S, Hedley CG, Stain SC.The utility and reliability of computed tomography scan in the diagnosis of small bowel obstruction. Am Surg. 1999; 65:922-6 [PubMed] [Google Scholar]


