Abstract
Isolated sphenoid pathology is uncommon. Nasal polyps that originate from the anterior wall of the sphenoid sinus and reach the nasopharynx are called sphenochoanal polyps. The atypical location of sphenochoanal polyps leads to misdiagnosis, and surgery risks injuring the surrounding structures, such as the optic nerve, carotid artery, and brain. For the differential diagnosis of sphenochoanal polyps, nasal endoscopy and computed tomography are very important. We present the clinical and radiological features of a sphenochoanal polyp and review the status of the optic nerve during endoscopic surgery for a sphenochoanal polyp.
Key words: sphenochoanal polyp, optic nerve, injury.
Introduction
Nasal polyps are polypoidal masses arising mainly from the mucous membranes of the nose and paranasal sinuses. When they extend to the choana, they are called choanal polyps, which constitute 3–6% of all nasal polyps.1 Nasal choanal polyps occur in three different forms, which produce similar symptoms: sphenochoanal, antrochoanal, and ethmoido-choanal polyps. Sphenochoanal polyps are rare, while antrochoanal polyps are the most frequent and originate from the inflamed sinus mucosa.2
The etiology of sphenochoanal polyps is not clear. They are most frequent in adolescents and young adults.3 They may occur with concomitant nasal polyps. Isolated sphenoid sinus pathology is relatively uncommon. Most nasal polyps produce the same symptoms: nasal obstruction, nasal discharge, and headache. Nasal polyps are seen in anterior rhinoscopy, while an endoscopic examination or computed tomography (CT) is needed to differentiate sphenochoanal polyps.4
Nasal polyps can be removed via endoscopic sinus surgery, but the site of origin is very important, especially for polyps originating from the sphenoid sinus because the carotid artery and optic nerve are located near the sphenoid sinus. Any uncontrolled maneuver in endoscopic sinus surgery can damage these essential structures, so a preoperative diagnosis of the polyp origin is essential.
Case Report
A 16-year-old boy presented to our outpatient clinic with a 1-year history of bilateral nasal obstruction and discharge. He had no significant medical history or drug allergy. In the nasal examination, the nasal cavity was filled with a nasal polyp and there was right septal deviation. At nasal endoscopy, the origin of the nasal polyp was not clear; it seemed to originate posteriorly, occupying the left choana. Skin-prick testing was negative for the main commercial allergens. The total immunoglobulin E was within normal limits. Paranasal coronal images showed a homogeneously opacified maxillary sinus, totally opacified left sphenoid sinus, and obliterated choanal passage. The middle meatus was also opacified (Figure 1).
Figure 1.

Paranasal sinus computed tomography shows homogeneously opacified maxillary sinus walls, a totally opacified left sphenoid sinus, and an obliterated choanal passage.
Endoscopic sinus surgery was performed under general anesthesia. After decongestion, the polyp was seen to originate from the sphenoethmoidal recess, not the maxillary sinus. Using nasal forceps, the nasal polyp was excised totally with its stalk (Figure 2). The sphenoidal ostium was naturally dilated (Figure 3). The polyp originated from the posterior wall of the sphenoid sinus. While attempting to excise the polyp stalk, dehiscence in the course of the optic nerve was observed. The operation finished after that.
Figure 2.

The sphenochoanal polyp specimen after surgery. The stalk is seen at the bottom of the specimen.
Figure 3.
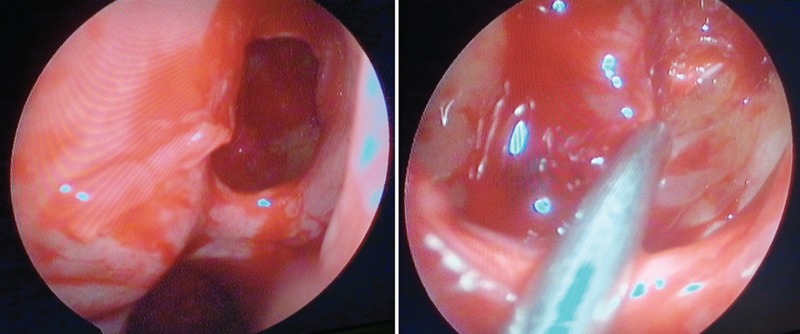
Endoscopic view of the dilated ostium of the sphenoid polyp caused by the sphenochoanal polyp. The posterior wall of the sphenoid sinus is seen after excising its stalk.
Postoperatively, saline was applied for one week and antibiotic was given to the patient. The nasal cavity was free of polyps and the sphenoid sinus was clear radiologically. Histopathologically, the specimen was an inflammatory polyp.
Discussion
Sphenochoanal polyps originate from the sphenoid sinus and are an uncommon form of choanal polyp. They are usually solitary. The etiology is not well understood, but allergy and chronic sinusitis might contribute.5 Intramural cysts can give rise to choanal polyps.2
Most frequently, they originate from the maxillary sinus.6 However, nasal polyps can arise from the sphenoid or ethmoid sinus.
Sphenochoanal polyps have to be differentiated from antrochoanal polyps to choose the correct surgery.
The most common symptoms are nasal obstruction, snoring, and unilateral nasal discharge, although the polyps can sometimes be asymptomatic. Sphenochoanal and antrochoanal polyps can be misdiagnosed as hypertrophied inferior turbinate, adenoid vegetation, pansinusitis, and nasal polyps. The presentation of a sphenochoanal polyp is similar to that of the more common antrochoanal polyp. A sphenochoanal polyp can be diagnosed preoperatively using nasal endoscopy and paranasal sinus tomography.7
Antrochoanal polyps are treated successfully with endoscopic sinus surgery, which allows complete removal of the polyp, including its site of origin, which minimizes the risk of recurrence.8,9 As choanal polyps arise from inflamed, edematous mucosa in the paranasal sinuses, at sinus surgery the origin of the polyp and diseased mucosa must be excised carefully to prevent recurrence. Our patient had an inflammatory polyp.
A sphenochoanal polyp has intrasinusoidal, ostial, and extra-sinusoidal components. They originate from the sphenoid sinus wall, exiting the sinus via the sphenoid ostium, passing through the sphenoethmoidal recess, and reaching the choana. In this case, the nasal polyp was not diagnosed as a sphenochoanal polyp preoperatively as the polyp obscured the cavity and was not clear radiologically. When there is a lack of maxillary opacity with choanal polyps, one should think of the possibility of sphenochoanal polyp. Sphenochoanal polyps usually pass through the sphenoethmoidal recess directly and do not reach the middle meatus unless very large. Opacification in the maxillary sinus, such as in our case, might lead to a misdiagnosis. In addition, a large polyp can fill the middle meatus.
There have been recent technical improvements in surgical procedures. Intraoperative CT surgery provides additional information about the surgical site in difficult anatomical situations. Intraoperative imaging provides near real-time imaging that has the potential to improve surgical outcomes and reduce operative morbidity. Complications can be avoided in nasal polyposis with CT-guided surgery. CT can also help to assess the origin of nasal polyps and surrounding essential structures, such as the carotid artery and optic nerve.10
At surgery, the polyp was diagnosed as a sphenochoanal polyp. The polyp stalk was not from the maxillary sinus, but from the sphenoid sinus through an enlarged sphenoid sinus. Forceps are also used to excise the polyp instead of a microdebrider, as the latter might damage the optic nerve and carotid artery when used inside the sphenoid sinus. Uncontrolled pulling on the nasal polyp with forceps is dangerous due to the proximity of the carotid artery and optic nerve, which can be damaged during surgery.11,12 In our case, the sphenochoanal polyp was excised en bloc and there were no complications involving the optic nerve. The patient's ophthalmic examination and vision were normal postoperatively.
Conclusions
Sphenochoanal polyps can be diagnosed at nasal endoscopy or with paranasal tomography. Isolated sphenoid sinus disease is under-reported due to a lack of recognition and experience. The symptoms are nonspecific. An adequate preoperative evaluation is necessary for a correct diagnosis. The stalk of the polyp should not be excised in an uncontrolled manner due to the proximity of the optic nerve and carotid artery.
References
- 1.Frosini P, Picarella G, De Campora E. Antrochoanal polyp: Analysis of 200 cases. Acta Otorhinolaryngol Ital. 2009;29(1):21–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Berg O, Carenfeld C, Silfversward, Sobin A. Origin of the choanal polyp. Arch Otorhinolaryngol. 1998;114:1270–1. doi: 10.1001/archotol.1988.01860230064025. [DOI] [PubMed] [Google Scholar]
- 3.Crampette L, Mondain M, Rombaux P. Sphenochoanal polyp in children. Diagnosis and treatment. Rhinology. 1995;33:43–5. [PubMed] [Google Scholar]
- 4.Al-Qudah MA. Sphenochoanal polyp: current diagnosis and management. Ear Nose Throat J. 2010;89:311–7. [PubMed] [Google Scholar]
- 5.Cook PR, Davis WE, McDonald R, McKinsey JP. Antrochoanal polyposis: a review of 33 cases. Ear Nose Throat J. 1993;72:401–2. 404–10. [PubMed] [Google Scholar]
- 6.Gordts F, Clement PA. Unusual choanal polyps. Acta Otorhinolaryngol Belg. 1997;51:177–80. [PubMed] [Google Scholar]
- 7.Weissman JL, Tabor EK, Curtin HD. Sphenochoanal polyps: evaluation with CT and MR imaging. Radiology. 1991;178:145–8. doi: 10.1148/radiology.178.1.1984293. [DOI] [PubMed] [Google Scholar]
- 8.Aktas D, Yetiser S, Gerek M, et al. Antrochoanal polyps: analysis of 16 cases. Rhinology. 1998;36:81–5. [PubMed] [Google Scholar]
- 9.Rugina MD, Dam-Hieu Z, Bedbeder P, et al. [Treatment of antrochoanal polyp by enlarged endoscopic meatotomy. Apropos of 19 cases] Ann Otolaryngol Chir Cervicofac. 1996;113:348–51. [Article in French] [PubMed] [Google Scholar]
- 10.Isaacs S, Fakhri S, Luong A, Citardi MJ. Intraoperative imaging for otorhinolaryngology-head and neck surgery. Otolaryngol Clin North Am. 2009;42:765–79. doi: 10.1016/j.otc.2009.08.014. viii. [DOI] [PubMed] [Google Scholar]
- 11.Kim JY, Kim HJ, Kim CH, et al. Optic nerve injury secondary to endoscopic sinus surgery: an analysis of three cases. Yonsei Med J. 2005;46:300–4. doi: 10.3349/ymj.2005.46.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vásquez LM, González-Candial M. Permanent blindness after endoscopic sinus surgery. Orbit. 2011;30:108–10. doi: 10.3109/01676830.2010.546554. [DOI] [PubMed] [Google Scholar]


