Abstract
Intraventricular rupture of a brain abscess is still associated with a high mortality rate. Here, we report such a case in a patient with normal immunity that was treated successfully using neuroendoscopic approach. A 69-year-old man who had presented with headache and fever developed confusion and restlessness. Magnetic resonance imaging revealed a mass with ring enhancement extending to the right ventricle. Emergency aspiration of cerebrospinal fluid (CSF) from the spinal canal revealed severe purulent meningitis. Bacterial culture of the CSF and blood was negative. Because of prolonged consciousness disturbance, the patient underwent evacuation of the intraventrcular abscess using a neuroendoscope. The pus was centrifuged and collected for bacterial culture, and this revealed Streptococcus intermedius/milleri. After implantation of a ventricular catheter, gentamicin sulfate was administered twice a day for 9 days. Cefotaxime sodium was also administered intravenously for 14 days, followed by oral administration of cefcapene pivoxil hydrochloride for 10 days. The patient made a complete recovery, and was discharged 31 days after admission. After 20 months of follow-up, he is doing well and has returned to his work. In cases of intraventricular rupture of a brain abscess, a neuroendoscopic approach is useful for evacuation of intraventricular debris or septum, and identification of the causative bacterium for selection of antibiotics, possibly reducing the period of hospitalization.
Key words: intraventricular rupture, brain abscess, neuroendoscope.
Introduction
Although the rate of mortality due to brain abscess has recently been decreasing,1,2 patients with intraventricular rupture of such abscesses have a poorer outcome, and the mortality rate may be as high as 85%.3–5 No definitive therapeutic regimens for intraventricular rupture of brain abscesses have been reported, and most patients are treated by aggressive surgery.3,6 Even when patients have a favorable outcome, long-term hospitalization is usually required. To our knowledge, there have been no detailed reports of such cases treated using a neuroendoscopic approach. Here, we report a case of intraventricular brain abscess rupture in a patient with normal immunity that was treated successfully by neuroendoscopic aspiration of the intraventricular abscess, followed by simple ventricular drainage with intraventricular and intravenous administration of antibiotics.
Case Report
A 69-year-old man presented at a local clinic with headache and fever. Twelve hours later, his condition deteriorated to confusion and restlessness with nuchal stiffness after severe exacerbation of the headache and vomiting. The patient was therefore transferred to our hospital. Magnetic resonance imaging (MRI) revealed a mass with ring enhancement extending to the right ventricle (Figure 1). Emergency aspiration of cerebrospinal fluid (CSF) from the spinal canal revealed severe purulent meningitis; cells 10,112/ 3 mm3 (neutrophils: 87%), protein: 326 mg/dL, sugar: 4 mg/dL. Bacterial culture of the CSF and blood was negative, and no positivity for serum endotoxin, β-D glucan, or aspergillus was evident. Imipenem-cilastatin was tentatively administered intravenously. As confusion and restlessness were still present on the second day, the patient underwent evacuation of the intraventrcular abscess via the right lateral ventricle using a neuroendoscope. In the posterior horn of the lateral ventricle, whitish, soft pus was observed. Using a forceps, the pus was removed, and then as much of it as possible was aspirated using a 5-mL syringe. The pus was centrifuged and collected for bacterial culture. A catheter was implanted into the ventricle, and gentamicin sulfate was administered twice a day. Nine days after the operation, the CSF findings recovered to normal, and the catheter was removed. Culture revealed Streptococcus intermedius/milleri, and therefore cefotaxime sodium was administered intravenously for 14 days, followed by oral administration of cefcapene pivoxil hydrochloride for 10 days. Postoperative MRI showed gradual shrinkage of the mass (Figure 2). The patient recovered completely, and was discharged 31 days after admission. MRI demonstrated no enhanced mass 15 months later (Figure 3). After 20 months of follow-up, the patient is doing well and has returned to his work. He had a history of traumatic subarachnoid hemorrhage causing mild right lower limb paresis 40 years previously, but was running a cardboard recycling company. He also had a history of tinea pedis, but had normal immunity. Dermatological and cardiovascular examinations revealed no evidence of similar bacteria.
Figure 1.
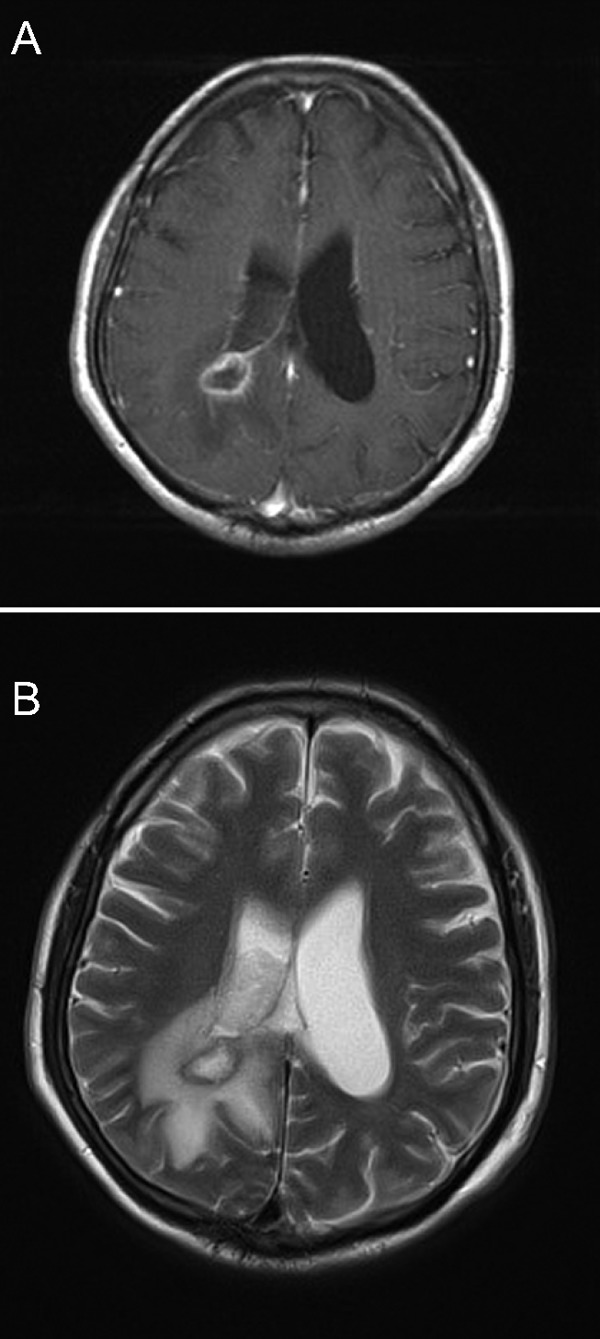
Magnetic resonance imaging revealing an area of ring enhancement in the occipital lobe with ventricular debris. (A) T1-weighted image with gadolinium enhancement, (B) T2-weighted image.
Figure 2.
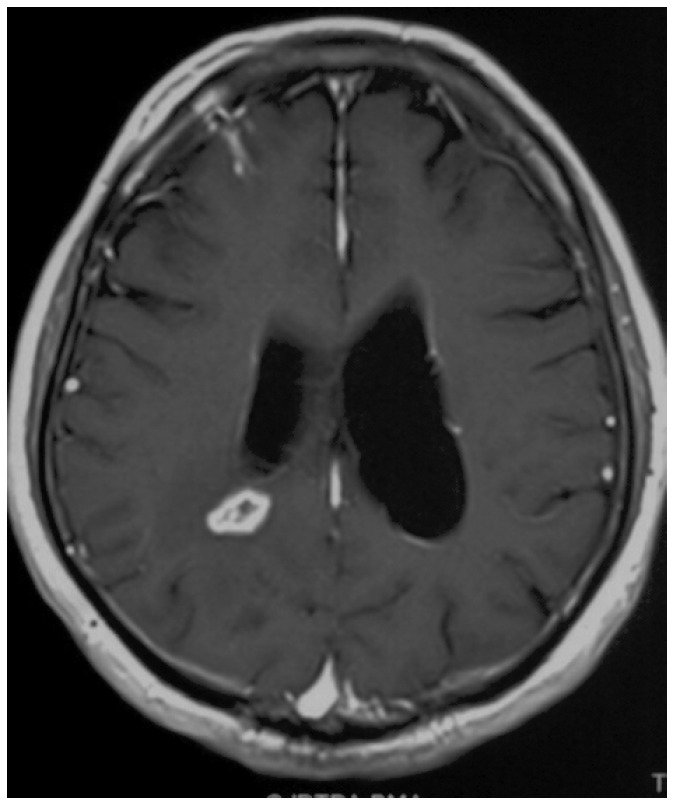
Magnetic resonance imaging showing gradual shrinkage of the mass and intraventricular debris.
Figure 3.
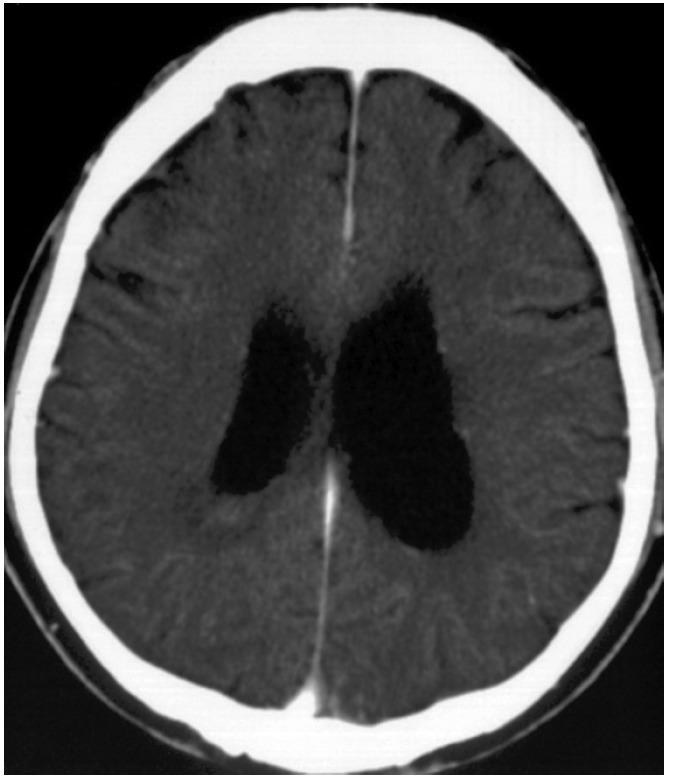
Magnetic resonance imaging demonstrating no enhanced mass.
Discussion
Intraventricular rupture of a brain abscess is still a life-threatening condition, in comparison with simple brain abscess. There are several reports of cases that have been treated successfully.3,6 Zeidman et al. recommended an aggressive therapeutic plan involving open craniotomy with debridement of the abscess and ventricle lavage, followed by postoperative intravenous and intraventricular administration of antibiotics, and intraventricular drainage for 6 weeks.3 Sato et al. suggested a minimally invasive regimen involving 14 days of intraventricular irrigation with antibiotics between the bilateral anterior horns of the lateral ventricle.6 However, even when the patients had a favorable outcome, long-term hospitalization was usually required. Our patient was discharged only one month after admission, and intraventricular and intravenous administration of antibiotics was done for 9 days and 21 days, respectively. In cases of cerebral abscess rupturing into the ventricle,7 the ventricles sometimes become loculated with fibrous bands that prevent free circulation of the CSF. This phenomenon sometimes prevents antibiotics from entering the infected ventricular spaces. A neuroendoscope can perforate such fibrous bands or thickened pus, and directly remove them. Intrathecal and intravenous administration of antibiotics after this procedure is therefore possible and effective. In this case, it was also intriguing that bacterial cultures of CSF taken via spinal puncture and from blood were negative, whereas the causative bacterium was identified from the pus collected using the neuroendoscope, even after the antibiotics had been administered. This allowed the selection of an appropriate intravenous antibiotic, followed by oral administration. The present case may have been less serious than a number that have been reported previously. Although investigation of the present procedure in such serious cases will therefore be required, we believe that an endoscopic approach is useful for minimally invasive treatment of intraventricular rupture of a brain abscess.
References
- 1.Alderson D, Strong AJ, Ingham HR, Selkon JB. Fifteen-year review of the mortality of brain abscess. Neurosurgery. 1981;8:1–6. doi: 10.1227/00006123-198101000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Mampalam TJ, Rosenblum ML. Trends in the management of bacterial brain abscesses: a review of 102 cases over 17 years. Neurosurgery. 1988;23:451–8. doi: 10.1227/00006123-198810000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Zeidman SM, Geisler FH, Olivi A. Intraventricular rupture of a purulent brain abscess: case report. Neurosurgery. 1995;36:189–93. doi: 10.1227/00006123-199501000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Fukui MB, Williams RL, Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. AJNR Am J Neuroradiol. 2001;22:1510–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Black PM, Levine BW, Picard EH, Nirmel K. Asymmetrical hydrocephalus following ventriculitis from rupture of a thalamic abscess. Surg Neurol. 1983;19:524–7. doi: 10.1016/0090-3019(83)90376-2. [DOI] [PubMed] [Google Scholar]
- 6.Sato M, Oikawa T, Sasaki T, Kodama N. [Brain abscess ruptured into the lateral ventricle: the usefulness of treatment by intraventricular irrigation with antibiotics. A case report] No Shinkei Geka. 1994;22:689–93. [PubMed] [Google Scholar]
- 7.Haines SJ, Mampalam T, Rosenblum ML, Nagib MG. Cranial and intracranial bacterial infections. In: Youmans JR, editor. Neurological Surgery. Vol. 6. Philadelphia: WE Saunders; 1990. pp. 3730–3731. [Google Scholar]


