Abstract
We present a rare case of internal carotid artery pseudoocclusion (ICAPO) in a 60-year-old male Caucasian patient who experienced a reversible sudden loss of vision of the right eye for 10 min followed by recurrent blurring of vision as well as dysarthria and numbness in the left face. The referring ophthalmologist admitted the patient for suspicious occlusion of the internal carotid artery causing anterior ischemic optic neuropathy (AION).
Key words: pseudoocclusion, internal carotid artery, ischemia, low flow, retinal artery.
Introduction
Internal carotid artery pseudoocclusion (ICAPO) can still be a major challenge for non-invasive neuroimaging such as color-coded neurosonography, computed tomography angiography (CTA) and magnetic resonance angiography (MRA).1,2 To date ICAPO remains one of the most important indications for digital subtraction angiography (DSA).3 Due to sufficient collateralisation pathways into the middle cerebral artery via the communicating arteries and the ophthalmic collateral pathway ICAPO can be either asymptomatic or cause recurrent embolic events from the distal carotid stump. Standard therapy consists of carotid endarterectomy in order to prevent distal embolisation from residual clot in the cervical and/or petrous ICA segment yet first larger studies employing ICA stenting have recently been published.
Case Report
We present a rare case of ICAPO in a 60-year-old male Caucasian patient who experienced a reversible sudden loss of vision of the right eye for 10min followed by recurrent blurring of vision as well as dysarthria and numbness in the left face. The referring ophthalmologist admitted the patient for suspicious occlusion of the internal carotid artery causing anterior ischemic optic neuropathy (AION). Diffusion weighted magnetic resonance imaging (MRI) (Sonata, Siemens Medical Solutions, Erlangen, Germany) demonstrated right ischemic infarct in the insular cortex while time-of-flight and contrast enhanced angiography (CE-MRA) revealed a totally occluded ICA with a suspicious proximal stump (Figure 1A). Transcranial color-coded sonography (TCCS) (Siemens Sequoia, 3V2 transducer, Acuson Corp., Mountain View, CA, USA) showed complete and sufficient cross filling via the anterior communicating artery into the MCA territory (Figure 1B). Immediate digital subtraction angiography (DSA) showed in the early phase of the series in agreement with MRA a seemingly occluded right ICA (Figure 1C). However, the pregression of contrast finally demonstrated a patent ICA (Figure 1D). The patient was transferred to vascular surgery for carotid eversion endarterectomy and underwent surgery the same day. The postoperative course was unremarkable except persistent visual loss on the right eye. Post-operative CE-MRA showed no residual stenosis (Figure 1e) and TCCS found normalized ante grade flow in the anterior cerebral artery and good perfusion in the MCA (Figure 1F).
Figure 1.
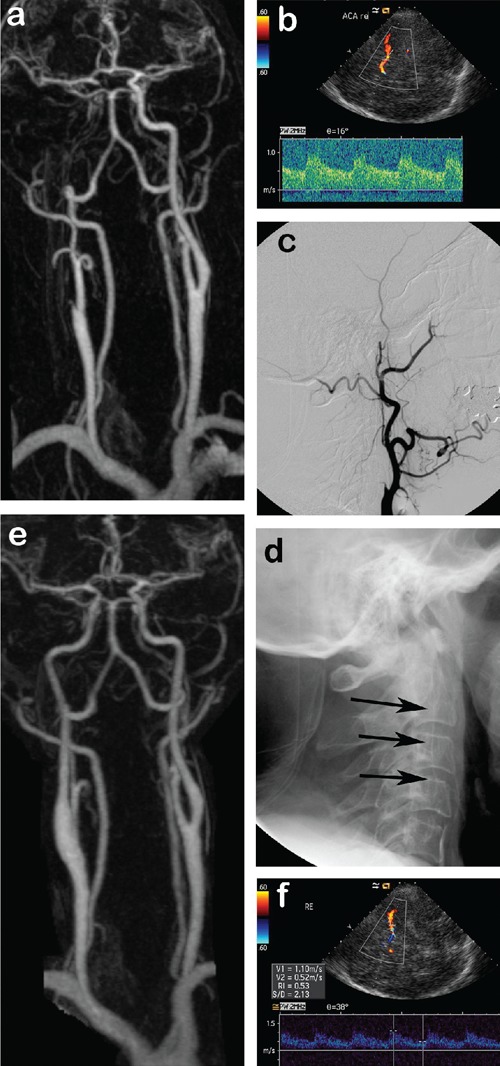
A) Contrast enhanced magnetic resonance angiography (CE-MRA) shows occlusion of the right internal carotid artery. B) Axial transcranial color-coded sonography (TCCS) through the right temporal bone window demonstrating reversal of flow in the right anterior cerebral artery into the middle cerebral artery (both in red) with blood flow velocities within normal limits. C) Lateral DSA of the right common carotid artery showing stump of the inter-nal carotid artery which appears totally occluded. D) Late phase of the DSA series re-veals delayed antegrade filling of the ICA. E) Postoperative CE-MRA with regular filling of the right internal carotid artery. F) Postoperative TCCS with normal blood velocities in the right middle cerebral artery (in red) and normalization of flow in the anterior cerebral artery (now blue).
In addition to conventional neurosonography we examined the blood flow velocities in the right central retinal artery (CRA) pre- and post-operatively (Figure 2) due to fluctuating AION. Before the operation the flow was 1.45 cm/s and after operation 10 cm/s now within the normal published limits for CRA flow of 9.5±3.1 cm/s.4
Figure 2.
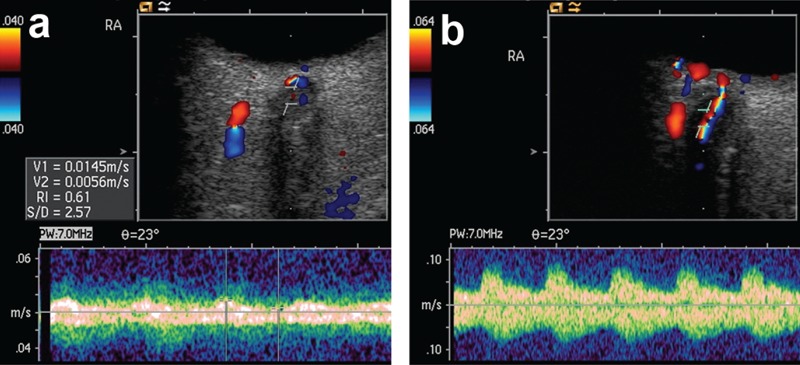
A) High resolution orbital sonography with the doppler sample volume placed into the hypoechoic optical nerve with the residual low flow in the central retinal artery. B) Post-operatively orbital sonography demonstrates normal flow in the central retinal artery which can now be easily delineated together with its vein in red and blue.
The case illustrates the need for careful neuroradiological examination in order not to miss ICAPO as well as the potential of color-coded neurosonography including the orbital vessel for functional characterization of the hemodynamic situation. Despite excellent non-invasive imaging angiography remains the gold standard for the detection of ICAPO and should be considered in patient presenting with symptoms ipsilateral to an occluded ICA. In this patient we found both hemodynamic compromise in the central retinal artery as well as embolic in-farcts in the MCA territory as a result of ICAPO.
References
- 1.Droste DW, Kaps M, Navabi DG, Ringelstein EB. Ultrasound contrast enhancing agents in neurosonology: principles, methods, future possibilities. Acta Neurol Scand. 2000;102:1–10. doi: 10.1034/j.1600-0404.2000.102001001.x. [DOI] [PubMed] [Google Scholar]
- 2.Okamoto K, Ito J, Furusawa T, et al. “Pseudoocclusion” of the internal carotid artery: a pitfall on intracranial MRA. J Comput Assist Tomogr. 1997;21:831–3. doi: 10.1097/00004728-199709000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Kniemeyer HW, Aulich A, Schlachetzki F, et al. Pseudo- and segmental occlusion of the internal carotid artery: a new classification, surgical treatment and results. Eur J Vasc Endovasc Surg. 1996;12:310–20. doi: 10.1016/s1078-5884(96)80250-4. [DOI] [PubMed] [Google Scholar]
- 4.Guthoff RF, Berger RW, Winkler P, et al. Doppler ultrasonography of the ophthalmic and central retinal vessels. Arch Ophthalmol. 1991;109:532–6. doi: 10.1001/archopht.1991.01080040100037. [DOI] [PubMed] [Google Scholar]


