Abstract
Mesenteric cysts are uncommon benign abdominal lesions with no classical clinical features. The preoperative diagnosis requires the common imaging modalities but the final diagnosis is established only during surgery or histological analysis. The treatment of choice is complete surgical excision. We report an 18-year-old female with a non-specific abdominal pain and discomfort since 3 weeks. Her CT scan showed a huge cystic swelling, which necessitated surgical exploration. Preoperatively, a giant cyst was encountered with displacement of bowel loops. The cyst was completely removed and histology report confirmed mesenteric cyst without evidence of malignancy.
Key words: mesenteric cyst, laparotomy, abdominal pain.
Introduction
Mesenteric cysts are rare, usually benign tumors, with an incidence of 1/105,000–250,000 in the admitted surgical patients1. The cyst was first described in 1507 by the Florentine anatomist Benevieni2 during the autopsy of a 7-year-old boy while the first successful resection was performed in 1880 by Tilaux3. About half of these cysts are chylous in nature, first reported at necropsy by Rokitansky in 18424. Majority of cysts are single, but can be uni- or multi-locular5. Mesenteric cysts are lined by a single layer of columnar or cuboidal epithelial cells6. This layer is sometimes destroyed as a result of pressure exerted by the cyst fluid. Consequently, the cyst wall becomes composed of fibrocollagenous tissues along with chronic inflammatory cells7. The average size of mesenteric cysts ranges from 2 to 35 cm.8 The present case report describes the surgical management of a giant mesenteric cyst in a young girl.
Case Report
An unmarried 18-year-old girl presented to the surgical clinic of Ohud Hospital Al Madina Al Munawara Saudi Arabia with the history of dragging pain in the lower part of abdomen since 3 weeks. She denied any history of trauma or previous abdominal surgery. The patient had normal vital signs. Her abdominal examination demonstrated slight distension with a cystic and fluctuant mass measuring 30 × 25 cm in the suprapubic region. Bowel sounds were audible with normal frequency. All baseline blood investigations were normal. The computed tomography (CT) scan revealed a huge cystic mass in the abdomen and pelvis measuring 30 ×27 cm, displacing the bowel loops and urinary bladder (Figure 1). The patient was prepared for operation and an exploratory laparotomy, which revealed a giant cystic mass, originating from the mesentery of small bowel, occupying almost entire abdominal cavity (Figure 2). The cyst was completely excised which was not found to be infiltrating the surrounding structures (Figure 3). Layered closure of the abdomen was done after the placement of a suction drain. The patient made uneventful recovery and was discharged home on 5th postoperative day. The histological report showed a mesenteric cyst lined by columnar epithelial cells and contained sterile fluid with few neutrophils.
Figure 1.

Contrast enhanced computed tomography scan of abdomen showing soft tissue density homogenous mass occupying whole of the abdominal cavity displacing the bowel loops to the periphery.
Figure 2.
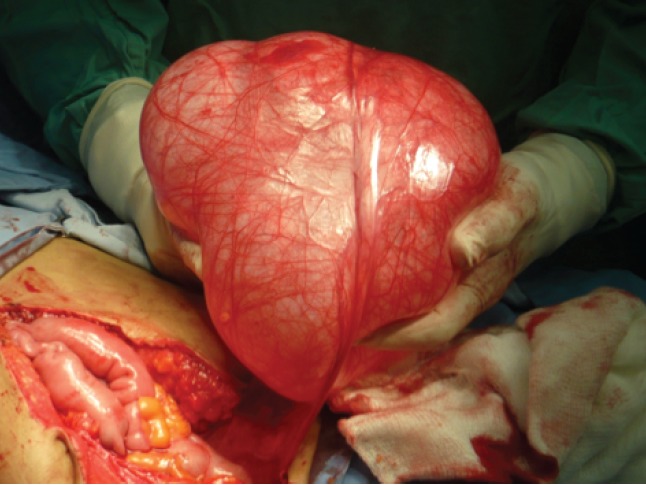
Peroperative view of the cystic mass while being resected.
Figure 3.
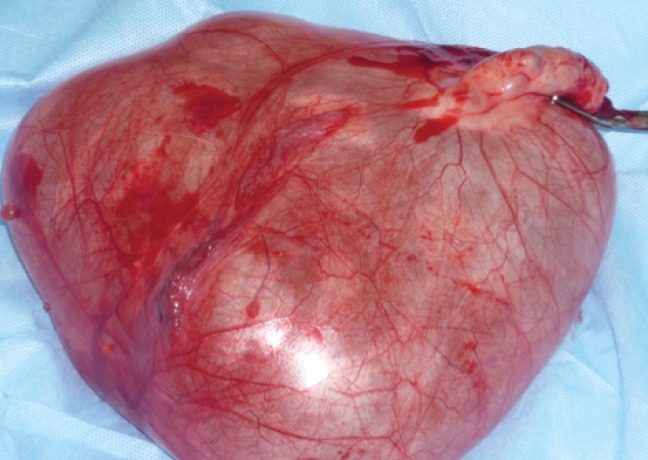
Resected specimen of mesenteric cyst.
Discussion
Majority of mesenteric cysts are congenital, but may be related to previous abdominal surgery, pelvic diseases, and trauma.8,9 The most common presentation is non specific abdominal pain (55–82%), followed by the complaint of abdominal mass (54–61%), and abdominal distension (17–61%).10,11,12 Physical examination is often unremarkable but reveals a mass in 66.8% of cases12 while the average duration of symptoms are 2–6 months (range; 12 h to 12 months).13
The precise cause of mesenteric cyst is not clear. The most accepted theory, purposed by Gross, is benign proliferation of ectopic lymphatics in the mesentery that lacks communication with the remainder of the lymphatic system.14 Viola et al. hypothesized that mesenteric cystic lymphangioma is an acquired anomaly due to chronic intermittent volvulus.15 The most widely accepted classification was coined by Beahrs et al. in 1955.16 According to this classification, there are four types of mesenteric cysts; developmental, traumatic, infective, and neoplastic. The malignant cystic mesothelioma is the only mesenteric cystic tumor that carries malignant potential and has tendency to recur after surgical excision.17 Mesenteric cysts in the pediatric age group occur more often in males (62.5%) and the majority of the patients are younger than 10 years, 75% were younger than 5 years of age.18 Ros et al.19 have extensively reviewed the correlation of histological classification and imaging correlation of mesenteric and omental cysts. Accordingly, a nonpancreatic pseudocyst is usually a unilocular or multilocular cyst located in either the mesentery or the omentum, with abundant debris sonographically and an enhancing wall on CT. An enteric duplication cyst is a unilocular cyst with an enhancing wall on CT. Such striking features help understand the diverse nature of mesenteric and omental cysts. Mesothelial and enteric cysts are anechoic, thin-walled cysts.
Mesenteric cysts can develop anywhere in the mesentery of GIT from duodenum to rectum. In a review series of 162 cases, 60% occurred in the small bowel mesentry, 24% in the large bowel mesentery, and 14.5% in the retroperitoneum.20 50–60% of mesenteric cysts occur in the mesentery of ileum.21 A variety of diagnostic modalities are applied to confirm the presence of mesenteric cyst, but ultrasonography (USG) and CT scan of the abdomen tend to be the favored methods.22 USG of the abdomen reveals a hypoechoic cystic mass with or without intense echos and can also show septa, debris, abdominal fluid levels. The CT scan allows determining the size, and sometimes the point of origin of the mass, the relation to the neighboring organs and depicts better wall calcification.20 MRI offers more information and accurately describes the relation between the mass and soft tissues. MRI-MRCP appeared to be more specific, defining the dimensions of the cyst, its origin, and its cystic component.23
The treatment of choice for mesenteric cyst is surgery. Simple evacuation and marsupialization are not recommended because both are associated with unacceptably high recurrence and infection rate.24,25 The procedure of choice for benign mesenteric cyst is complete enucleation.12 Localized resection of intestine or surrounding structures may be required to excise the cyst en bloc;26 our case did not require this step. Wiesen et al.27 described the complete enteroscopic excision of a mesenteric chylous cyst that developed in the lumen of the proximal jejunum. Some authors performed laparoscopic fenestration of the cyst, if located near a major abdominal vessel.26 Tebala et al.28 performed successful laparoscopic excision of a huge mesenteric chylous cyst in a 58-year-old man. Similarly, Shimura et al.11 and Vu et al.29 have reported laparoscopic excision of mesenteric cysts. In the former case, the cyst contents were aspirated before resection for the ease of handling. In the later, aspiration was only performed after mobilization to aid extraction. In both reports complete resection was achieved without any recurrence. The operating time was longer in laparoscopic resection, but the hospital stay was shorter and resulted in postoperative pain earlier return to normal activity.11
In conclusion, mesenteric cysts are extremely rare benign lesions arising from various sites. These cysts present with vague symptoms, there are no specific investigative tools to diagnose these lesions. Surgical excision offers the best curative measure.
References
- 1.Kurtz MD, Heiman TM, Berk AR, Holt J. Mesenteric and retopancreatic cysts. Ann Surg. 1986;203:109–12. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braquehaye A. Des Kystes du mesentery. Arch Gen. 1892:170–291. [Google Scholar]
- 3.Tilaux P. Millard and cyst du mesentere chez une home. Bull Acad Med. 1880;7:831–831. [Google Scholar]
- 4.Levison CG, Wolfssohn M. A mesenteric chylous cyst. Aust NZ J Surg. 1994;62:641–4. [PMC free article] [PubMed] [Google Scholar]
- 5.Burker JS, Pickleman J. The rationale for surgical treatment of mesenteric and retropancreatic cysts. Am Surg. 1994;60:432–5. [PubMed] [Google Scholar]
- 6.Bury TF, Pricolo VE. Malignant transformation of benign mesenteric cyst. Am J Gastroenterol. 1994;89:2085–7. [PubMed] [Google Scholar]
- 7.Sardi A, Parikh KJ, Singer JA, Minken SL. Mesenteric cysts. Am Surg. 1987;53:58–60. [PubMed] [Google Scholar]
- 8.De Perrot M, Brundler MA, Totsch M, et al. Mesenteric cysts. Towards less confusion? Dig Surg. 2000;17:323–8. doi: 10.1159/000018872. [DOI] [PubMed] [Google Scholar]
- 9.Wykypiel HF, Margreiter R. Chylous cyst formation following laparoscopic fundoplication. Wien Klinh Wochenschr. 2007;119:729–32. doi: 10.1007/s00508-007-0912-2. [DOI] [PubMed] [Google Scholar]
- 10.Liew SC, Glenn DC, Storey DW. Mesenteric cyst. ANZ J Surg. 1994;64:741–4. doi: 10.1111/j.1445-2197.1994.tb04530.x. [DOI] [PubMed] [Google Scholar]
- 11.Shimmura H, Ueda J, Ogawa Y, et al. Total excision of mesenteric cysts by laparoscipoc surgery; report of 2 cases. Surg Laparosc Endosc. 1997;7:173–6. [PubMed] [Google Scholar]
- 12.Tan JY, Tan KK, Chew SP. Mesenteric cysts: An institution experience over 14 years and review of literature. World HJ Surg. 2009;33:1961–5. doi: 10.1007/s00268-009-0133-0. [DOI] [PubMed] [Google Scholar]
- 13.Kurtz RJ, Heimann TM, Beck AR, Holt J. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109–12. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richard RR. Mesenteric and omental cysts. In: Grosfeld JL, O'Neill JA Jr, Coran AG Jr, Fonkalsrud EW, editors. Pediatric Surgery. 6th ed. Philadelphia: Mosby Elsevier; 2006. pp. 1399–1406. [Google Scholar]
- 15.Weeda VB, Booij KA, Aronson DC. Mesenteric cystic lymphangioma: A congenital and an acquired anomaly? Two cases and a review of the literature. J Pediatr Surg. 2008;43:1206–8. doi: 10.1016/j.jpedsurg.2008.01.075. [DOI] [PubMed] [Google Scholar]
- 16.Beahrs OM, Judd ES, Jr, Dockerty MB. Chylous cysts of the abdomen. Surg Clin North Am. 1950;30:1081–96. doi: 10.1016/s0039-6109(16)33090-0. [DOI] [PubMed] [Google Scholar]
- 17.Mennemmeyer MS. Multicystic peritoneal mesothelioma: a report with electron microscopy of a case mimicking intra-abdominal cystic hygroma (lymphangiona) Cancer. 2006;44:692–8. doi: 10.1002/1097-0142(197908)44:2<692::aid-cncr2820440242>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 18.Chung MA, Brandt ML, St-Vil D, Yazbeck S. Mesenteric cysts in children. J Pediatr Surg. 1991;26:1306–8. doi: 10.1016/0022-3468(91)90606-t. [DOI] [PubMed] [Google Scholar]
- 19.Ros PR, Olmsted WW, Moser RP, Jr, et al. Mesenteric and omental cysts: histological classification with imaging correlation. Radiology. 1987;164:327–32. doi: 10.1148/radiology.164.2.3299483. [DOI] [PubMed] [Google Scholar]
- 20.Mason JE, Soper NJ, Brunt LM. Laparoscopic excision of mesenteric cysts: A report of two cases. Surg Laparosc Endosc Percutan Tech. 2001;11:382–4. doi: 10.1097/00129689-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Curry CA, Horton B, Urban S, et al. CT of primary cystic pancreatic neoplasm; can CT be used for triage and treatment. AJM Am Roentgenol. 2001;177:469–70. [Google Scholar]
- 22.Falidas E, Mathioulakis S, Vlachos K, et al. Traumatic mesenteric cyst after blunt abdominal trauma. Int J Surg Case Reports. 2011;2:159–62. doi: 10.1016/j.ijscr.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shamiyeh A, Rieger R, Schrenk P, Wayand W. Role of laparoscopic surgery in treatment of mesenteric cysts. Eco Health. 1999;13:937–9. doi: 10.1007/s004649901140. [DOI] [PubMed] [Google Scholar]
- 24.Alwan MH, Eid AS, Alisharif IM. Retroperitoneal and mesenteric cysts. Singapore Med J. 1999;40:160–4. [PubMed] [Google Scholar]
- 25.O'Brien MF, Winter DC, Lee G, et al. Mesenteric cysts – a series of 6 cases with a review of the literature. Ir J Med Sci. 1999;168:233–6. doi: 10.1007/BF02944346. [DOI] [PubMed] [Google Scholar]
- 26.Wiesen A, Sideridis K, Stark B, Bank S. Mesenteric chylous cyst. Gastrointest Endosc. 2006;63:502–502. doi: 10.1016/j.gie.2005.06.064. [DOI] [PubMed] [Google Scholar]
- 27.Ho TP, Bhattachaya V, Wyatt MG. Chylous cyst of the small bowel mesentery presenting as a contained rupture of an abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2002;23:82–3. doi: 10.1053/ejvs.2001.1485. [DOI] [PubMed] [Google Scholar]
- 28.Tebala GD, Camperchioli MD, Valeria T, et al. Laparoscopic treatment of a huge mesenteric chylous cyst. J Soc Laparoendosc Surg. 2010;14:436–8. doi: 10.4293/108680810X12924466007205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vu JH, Thomas EL, Spencer DD. Laparoscopic management of mesenteric cyst. Am Surg. 1999;65:264–5. [PubMed] [Google Scholar]


