Abstract
The rate of re-rupture of Achilles tendon after surgical treatment were reported to 1.7–5.6% previously. Re-rupture of Achilles tendon generally occurs subcutaneously. We experienced two rare cases of the open re-ruptures of Achilles tendon with a transverse wound perpendicular to the primary surgical incision. Re-rupture occurred 4 and 13 weeks after surgical treatment. We suggest that open re-rupture correlates more closely with skin scaring and shortening. Another factor may be adhesion between the subcutaneous scar and the suture of the paratenon and Achilles tendon with post-operative immobilization.
Key words: Achilles tendon, open re-rupture, surgical treatment.
Introduction
Achilles tendon rupture commonly happens to athletes and people doing leisure activities. Of the complications accompanying Achilles tendon ruptures, re-rupture is the most significant complication following treatment. The rate of re-rupture of the Achilles tendon after surgical treatment has been reported to be in the order of 1.7–5.6%.1–7 Wound detachment and infection are the other common complications after surgical treatment.6 Though conservative treatment can avoid wound detachment and infection, it has a higher risk of re-rupture than operative treatment.1,3–4 Re-rupture of the Achilles tendon generally occurs subcutaneously. In this present report, we report 2 cases of open re-ruptures of the Achilles tendon after operative treatment with a transverse wound perpendicular to the primary surgical incision. To our knowledge, there is only one previous report similar to our cases.8 The treatment and rehabilitation of our 2 cases will also be discussed.
Case Reports
Case #1
The patient was a 51-year old woman with no previous disease history. She had a non-contact injury to her left ankle while playing volleyball, which was her main leisure activity. She was admitted to our hospital and diagnosed with an Achilles tendon rupture by visual confirmation of a hollow over the Achilles tendon and positive Thompson test; she opted for surgical treatment. She was positioned prone on the operating table with tourniquet control. First, a posterior middle incision was made longitudinally. The Paratenon was dissected and the Achilles tendon was exposed. Then a one-bundle Bunnel suture with a size-2 non-absorbable braided suture was used for the distal site of the rupture and two-bundle Bunnel sutures were used for the proximal site. In addition, 3-0 absorbable sutures were used for the circumferential suture. The Paratenon was repaired almost completely. Post-operative immobilization in a below-knee cast with the ankle in the rest position was maintained for three weeks. The cast was then removed and weight bearing was allowed. She received rehabilitation and was walking with full-weight bearing without complication after four weeks post surgery. However, 13 weeks after the operation, she fell over and experienced an open re-rupture of the Achilles tendon (Figure 1). The open wound was transverse and perpendicular to the middle of the initial surgical incision. A second operation was performed and it was found that the Achilles tendon had ruptured completely at the same level of the initial suture. The scars at both ends of the Achilles tendon rupture were removed and one-bundle Bunnel sutures with a size-2 non-absorbable braided suture was used for the distal site of the rupture and a one-bundle baseball suture were used for the proximal site. As there was a 5 mm gap between the proximal and distal ends of rupture, we used the plantaris tendon to augment the Achilles tendon (Figure 2). Post-operative immobilization in a below-knee cast with the ankle in the rest position was once more maintained for three weeks. After the cast was removed and weight bearing was allowed, we used a brace to limit dorsal flexion of the ankle. The brace was removed ten weeks after the second operation. Two weeks later the patient had almost a full range of ankle motion and no pain when walking. Subsequent magnetic resonance imaging (MRI) showed the Achilles tendon had healed without defect (Figure 3).
Figure 1.

The open re-rupture of the Achilles tendon in case 1. The open wound was transverse and perpendicular to the middle of the initial surgical incision.
Figure 2.

Second surgical intervention in case 1. Augmentation of the gap of the Achilles tendon re-rupture using the plantaris in the second surgery.
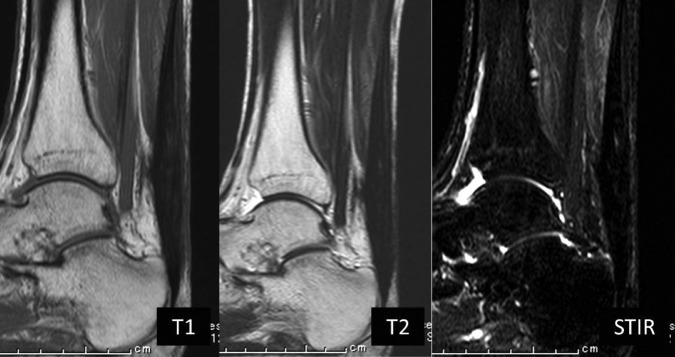
Figure 3.

Magnetic resonance (MR) images post-operative 12 weeks after the second surgery in case 1. The Achilles tendon had healed without defect on T1-weighted, T2-weighted, and STIR of MRI.
Case #2
The patient was a 29-year old man with no previous disease history. He had a non-contact injury to his left ankle during competitive basketball. The same primary operation and postoperative rehabilitation protocol as described in case 1 was performed. Four weeks after his initial operation, he fell over and was injured with an open re-rupture of the Achilles tendon. The open wound was transverse and perpendicular to the distal one-fourth of the initial incision. A second surgical intervention found the Achilles tendon was ruptured completely at the same level of the initial suture. The scars at both ends of the Achilles tendon rupture were removed and the correct apposition of both ends could be simply sutured end to end (Figure 4). A one-bundle suture by the Marti method with a size-2 non-absorbable braided suture was used for the distal site of the rupture and two-bundle sutures were used for the proximal site. The post-operative rehabilitation protocol was the same as described in case 1. Twelve weeks after the second operation, the patient had almost a full range of ankle motion and no pain when walking. Subsequent MRI showed the Achilles tendon had healed without defect (Figure 5).
Figure 4.

Second surgical intervention in case 2. Simple end-to-end suture of the Achilles tendon re-rupture was performed.
Figure 5.
Post-operative magnetic resonance (MR) images 12 weeks after the second surgical intervention in case 2. The Achilles tendon had healed without defect on T1-weighted, T2-weighted, and STIR of MRI.
Discussion
Re-rupture of the Achilles tendon is a significant complication when considering either surgical or conservative treatment. The rate of re-rupture after operative treatment has been previously reported to be 1.7–5.6%,1–7 while the rate of re-rupture during conservative treatment is reported to be 11.7–20.8%.1,3–5 Wound detachment and re-rupture are well known complications after open surgical treatment of Achilles tendon ruptures. However, open re-rupture after surgical treatment of the Achilles tendon occurs much less frequently. To our knowledge, there is only one publication describing the case of an open wound that was transverse and perpendicular to the initial incision after surgical treatment of an Achilles tendon rupture. García-Germán et al. reported on 2 cases that were similar to our 2 patients.8 They hypothesized that open re-rupture may have been related to incomplete closure of the paratenon. As they used the Christiensen or Lindholm technique to augment the Achilles tendon during initial surgery, the bulk up and adhesion led to incomplete healing of the rupture. Mellor et al. reported that when special care was taken to perform a correct separate repair of the paratenon, the rates of wound break down, infection and re-rupture after surgical repair were lower than in previous reviews.9 Though we performed a complete suture of the paratenon, open re-rupture occurred. Kuwada et al. reported that the long-term non-weight bearing and immobilization increased the risk of recurrent rupture.10 García-Germán et al. also suggested that an extended casting protocol was related to recurrent rupture, involving an above-knee cast for the first two weeks after surgery and a below-knee cast for following six weeks. Our 2 cases, however, underwent similar immobilization with a below-knee cast for only three weeks. Pneumaticos et al. reported that in biomechanical tests on rabbits whose ankles were immobilized by pinning for 35 days after surgical repair of an Achilles tendon rupture had more stiffness of the Achilles tendon than did rabbits that were immobilized for only 14 days.11 Several studies have examined what role the paratenon plays; Graf et al. found that the role of a well vascularized paratenon was of paramount importance in the surgical treatment of a rupture and correct closure could help vascularization and avoid adhesion to superficial layers.12 García-Germán et al. could not completely close the paratenon because of augmented repair of the Achilles tendon rupture. They concluded that incomplete closure of the paratenon correlated with open re-rupture of the Achilles tendon. Though augmented repair of Achilles tendon ruptures has been commonly used on chronic ruptures, there remains little literature on open re-rupture of the Achilles tendon after surgical treatment. We think that the reasons for open re-rupture of the Achilles tendon had little to do with incomplete closure of the paratenon; rather we suggest that open re-rupture correlates more closely with skin scaring and shortening, though to our knowledge there are no reports in literature about skin scaring and shortening after surgical treatment of Achilles tendon ruptures. Another factor may be adhesion between the subcutaneous scar and the suture of the paratenon and Achilles tendon with post-operative immobilization for only three weeks. We suggest that to avoid an open re-rupture of the Achilles tendon, the surgical incision must be made transverse to the Achilles tendon or in a zigzag. In addition, the post-operative term for the ankle cast should be shortened and rehabilitation should be started as early as possible to obtain the best results.
References
- 1.Cetti R, Christensen SE, Ejsted R, et al. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–9. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 2.Kellam JF, Hunter GA, McElwain JP. Review of the operative treatment of Achilles tendon rupture. Clin Orthop Relat Res. 1985;201:80–3. [PubMed] [Google Scholar]
- 3.Kocher MS, Bishop J, Marshall R, et al. Operative versus nonoperative management of acute Achilles tendon rupture: expected-value decision analysis. Am J Sports Med. 2002;30:783–90. doi: 10.1177/03635465020300060501. [DOI] [PubMed] [Google Scholar]
- 4.Lo IK, Kirkley A, Nonweiler B, Kumbhare DA. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a quantitative review. Clin J Sport Med. 1997;7:207–11. doi: 10.1097/00042752-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Möller M, Lind K, Movin T, Karlsson J. Calf muscle function after Achilles tendon rupture. A prospective, randomized study comparing surgical and non-surgical treatment. Scand J Med Sci Sports. 2002;12:9–16. doi: 10.1034/j.1600-0838.2002.120103.x. [DOI] [PubMed] [Google Scholar]
- 6.Pajala A, Kangas J, Ohtonen P, Leppilahti J. Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am. 2002;84-A:2016–21. doi: 10.2106/00004623-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Strauss EJ, Ishak C, Jazrawi L, et al. Operative treatment of acute Achilles tendon ruptures: an institutional review of clinical outcomes. Injury. 2007;38:832–8. doi: 10.1016/j.injury.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 8.García-Germán D, Rubio-Quevedo R, Lopez-Goenaga J, Martin-Guinea J. Achilles tendon recurrent rupture following surgical repair: report on two cases. Foot Ankle Surg. 2009;15:152–4. doi: 10.1016/j.fas.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Mellor SJ, Patterson MH. Tendo Achillis rupture; surgical repair is a safe option. Injury. 2000;31:489–91. doi: 10.1016/s0020-1383(00)00028-0. [DOI] [PubMed] [Google Scholar]
- 10.Kuwada GT, Schuberth J. Evaluation of Achilles tendon rerupture. J Foot Surg. 1984;23:340–3. [PubMed] [Google Scholar]
- 11.Pneumaticos SG, Phd PCN, McGarvey WC, et al. The effects of early mobilization in the healing of achilles tendon repair. Foot Ankle Int. 2000;21:551–7. doi: 10.1177/107110070002100704. [DOI] [PubMed] [Google Scholar]
- 12.Graf J, Schneider U, Niethard FU. Microcirculation of the Achilles tendon and significance of the paratenon. A study with the plastination method. Handchir Mikrochir Plast Chir. 1990;22:163–6. [PubMed] [Google Scholar]


