Abstract
Congenital lobar emphysema (CLE) is an uncommon congenital malformation of the lung that can present with respiratory distress in early life. We report a full term female baby who presented with intermittent bluish discoloration of the lips and extremities during crying since birth. An initial diagnosis of left sided collapse-consolidation with right-sided compensatory emphysema was made from chest x-ray. When no improvement was noted after intravenous antibiotic therapy for 7 days, computerized tomographic scan of thorax was done which showed emphysema of the right middle lobe with transherniation and mediastinal shift to the left. Right middle lobectomy was done and postoperative period was uneventful. Histopathological examination of the specimen confirmed the diagnosis of CLE. CLE can mimic more common causes of respiratory distress in neonatal period and needs a high index of suspicion for diagnosis. Early diagnosis and effective surgical treatment is curative.
Key words: congenital lobar emphysema, cyanosis, newborn, respiratory distress.
Introduction
Congenital lobar emphysema (CLE) is a rare congenital malformation of the lung that can cause acute respiratory distress in early life.1 It is characterized by overinflation of a pulmonary lobe with resultant compression of the remaining ipsilateral lung.2 A mediastinal shift away from the increased-volume lung can also compress the contralateral lung. The abnormality is related to intrinsic bronchial narrowing. In these cases, weakened or absent bronchial cartilage leads to inspiratory air entry but collapse of the narrow bronchial lumen during expiration resulting in lobar air trapping. A single lobe is usually involved; however, patients can present with multiple lobar involvements. Males are more affected than females.3 Presence of a hyperlucent, hyperexpanded lobe with midline substernal herniation and compression of the remaining lung in computerized tomographic (CT) scan of thorax is usually diagnostic. The condition can mimic more common causes of respiratory distress in neonatal period and needs a high index of suspicion for diagnosis. Clinical awareness of this condition is therefore important for early diagnosis as effective surgical treatment is curative for this condition. We report a full term female baby in whom CLE mimicked as collapse-consolidation of the opposite lung. Final diagnosis could be established by CT scan of thorax. Right middle lobectomy was curative for the patient.
Case Report
A 22-day-old full term female baby, weighing 3800 g, presented with complains of intermittent bluish discoloration of the lips and extremities during crying since birth. These episodes used to be associated with rapid respiration and subsided spontaneously over a period of 10–15 min without any intervention. The baby remained active otherwise and accepted feeds well. On day 20 of life, the baby had a similar episode from which she did not recover spontaneously and became limp. She was taken to a local medical practitioner who referred her to us.
On examination, the baby was active without any clinical cyanosis, vitals were stable with a heart rate of 134/min, respiratory rate of 68/min and capillary refill time < 3 s; temperature was normal. Pulse oximetry showed oxygen saturation of 82% without oxygen which increased to 92% after giving oxygen by hood at a flow rate of 5 L/min. On auscultation of chest breath sounds were slightly diminished over the infraclavicular area on the left side. All the peripheral pulses were equally palpable and the heart sounds were normal. No congenital anomaly was present. Laboratory examinations showed hemoglobin of 14.6 g/dL, TLC of 12,400/mm3 with a differential count of N60 L38 E2 M0 and ESR of 20 mm in first hour. General blood picture was normal, blood biochemistry and arterial blood gases with oxygen were normal. Sepsis screening for both congenital and acquired infections were negative. Echocardiography with color Doppler excluded any congenital cardiac malformation.
Chest X-ray showed atelectasis of left upper and middle lobes with hyperinflation of the right lung (Figure 1). A diagnosis of left sided collapse-consolidation with right-sided compensatory emphysema was made and the baby was put on intravenous antibiotic therapy (cloxacillin and gentamicin). Her condition remained same and repeat chest X-ray after 7 days did not show any improvement. A CT scan of thorax was planned which showed hyperinflation of right middle lobe with transherniation and mediastinal shift to the left (Figure 2). A diagnosis of CLE was made and surgical consultation was taken. She was advised for right middle lobectomy. The child was operated upon under general anesthesia. The operative specimen measured 10×5×3 cm, no bulla could be identified. No evidence of bronchial atresia, cartilaginous malformation, anomalous artery or a mucus plug was found during operation, which could have been attributed for the emphysema. Histopathological examination of the specimen showed dilated alveoli and alveolar duct with disruption of alveolar septa at places suggesting emphysematous changes confirming the diagnosis of CLE (Figure 3). Inter-coastal drain was removed on 5th postoperative day. Postoperative X ray chest showed resolution of the emphysema with adequate expansion of the left lung. The child is now 3 months old, breast feeding well and gaining weight regularly, no further cyanotic episode was documented.
Figure 1.

Chest X-ray showing atelectasis of left upper and middle lobes with hyperinflation of the right lung.
Figure 2.
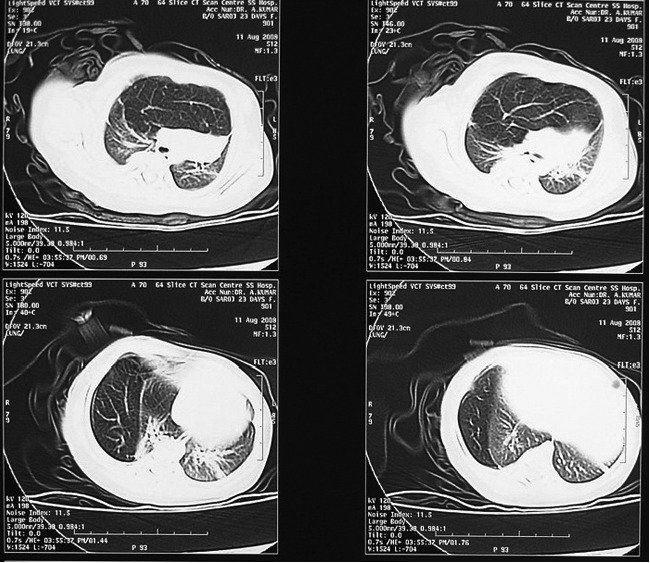
Computerized tomographic scan of thorax showing hyperinflation of right middle lobe with transherniation and mediastinal shift to the left.
Figure 3.
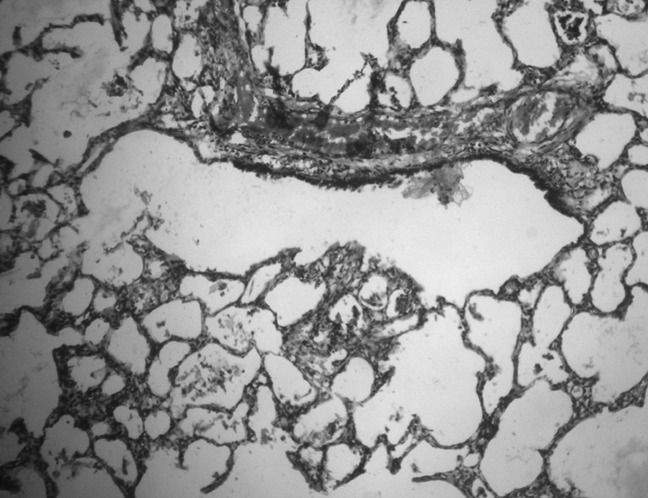
Histopathological examination of the specimen showing dilated alveoli and alveolar duct with disruption of alveolar septa at places suggesting emphysematous changes.
Discussion
CLE is an uncommon but potentially life-threatening cause of respiratory distress. Most of the cases are detected during newborn period but some may reach adulthood. Left upper lobe of the lung is found to be affected most commonly with CLE, followed by the right middle and right upper lobes and in most cases it is unilateral.4 Involvement of multiple lobes and involvement of lower lobe are rare.
CLE has no uniform etiology. It can be caused by intrinsic or extrinsic factors. Intrinsic factors include cartilaginous deficiency, bronchial stenosis, redundant bronchial mucosa or mucus plugs. Extrinsic causes include compression of the bronchus from outside by vascular rings or lymph nodes.3,5 Bronchial atresia and defective bronchial cartilage in the affected lobe are the common causes.4,6,7 The exact cause of CLE is difficult to determine in many cases and no apparent cause is found in 50%.8
The symptomatology of CLE is a manifold one. Common presenting symptoms are recurrent respiratory infection, dyspnea and cyanosis. Infants usually present with rapid respiration, wheezing or bluish discoloration of extremities, which may become generalized. Almost all cases of CLE are usually diagnosed within the first 6 months of life irrespective of any associated lesions. The age at the time of diagnosis is inversely related to the severity of the underlying lung problem, patients with lesser amount of functional lung tissue will present with respiratory distress earlier.5 Omerctahić-Dizdarević et al.2 reported three male infants, aged 16 days to 1 year who were diagnosed as CLE. Presenting symptoms were dyspnea, cyanosis, wheezing and recurrent respiratory tract infection.
The diagnosis of CLE can be established by a combination of clinical, radiological, and histopathological features. The diagnosis can often be confirmed by a simple chest radiograph as an area of hyperlucency involving the affected lobe with collapse of the adjacent lung tissue, widening of the rib spaces, flattening of the ipsilateral diaphragm, and a mediastinal shift to the contralateral site. In cases where the emphysematous lobe is large, lung hemiation to the contralateral hemitborax and atelectasis of the contralateral lung can be seen. CT scan is usually diagnostic in doubtful situations. In the present case, the collapseconsolidation of left upper and middle lobes were initially thought to be the primary pathology and hyperinflation of the right lung was thought to be due to compensatory emphysema. Failure to respond to antibiotic therapy only led to the use of CT scan. Other investigations, which can be done, to confirm CLE are radionuclide ventilation-perfusion scan which show diminished ventilation and absent perfusion of the affected lobe. Bronchoscopy can be useful in the evaluation of airway patency, dynamic changes in the airway, and in excluding obstruction by a mucus plug.5
CLE has been reported secondary to congenital cardiac malformations. Common cardiac anomalies associated with CLE were found to be left-to-right shunts, pulmonary hypertension, tetralogy of Fallot and patent ductus arteriosus.5,9,10
Treatment of CLE is mainly surgical.1,2 Surgical excision of the affected lobe is the appropriate treatment in all infants under 2 months of age and in infants older than 2 months presenting with severe respiratory symptoms. Infants older than 2 months presenting with mild to moderate respiratory symptoms associated with normal bronchoscopic findings can be treated conservatively. The children should be kept under close follow-up while under conservative management, and the families should be properly counseled about the disease.11,12
Though the diagnosis was established by histopathological examination, no definite intrinsic or extrinsic cause of CLE could be found in the present case. Since, CLE can mimic as common neonatal respiratory conditions, like collapse-consolidation of opposite lung in this case, it is necessary to suspect this uncommon anomaly in neonates presenting with respiratory distress not amenable to common therapies. The diagnosis can easily be confirmed by CT scan. Early diagnosis is rewarding as lobectomy of the emphysematous lung leads to complete cure.
References
- 1.Al-Salem AH. Congenital lobar emphysema. Saudi Med J. 2002;23:335–335. [PubMed] [Google Scholar]
- 2.Omerctahić-Dizdarević A, Saracević E, Jonuzi F, et al. [Congenital lobar emphysema] Med Arh. 2005;59:113–4. [Article in Bosnian] [PubMed] [Google Scholar]
- 3.Karapurkar SA, Borkar JD, Birmole BJ. Malformation of lung in neonates (lobectomy for congenital lobar emphysema and lung cyst) J Postgrad Med. 1993;39:224–224. [PubMed] [Google Scholar]
- 4.Seo T, Ando H, Kaneko K, et al. Two cases of prenatally diagnosed congenital lobar emphysema caused by lobar bronchial atresia. J Pediatr Surg. 2006;41:e17–20. doi: 10.1016/j.jpedsurg.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 5.Moideen I, Nair SG, Cherian A, Rao SG. Congenital lobar emphysema associated with congenital heart disease. J Cardiothorac Vasc Anesth. 2006;20:239–41. doi: 10.1053/j.jvca.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Weingärtner L. [The congenital lobar emphysema (author's transl)]. Padiatr Padol. 1977;12:33–47. [Article in German] [PubMed] [Google Scholar]
- 7.Warner JO, Rubin S, Heard BE. Congenital lobar emphysema: a case with bronchial atresia and abnormal bronchial cartilages. Br J Dis Chest. 1982;76:177–84. [PubMed] [Google Scholar]
- 8.Kravitz RM. Congenital malformations of the lung. Pediatr Clin North Am. 1994;41:453–72. doi: 10.1016/s0031-3955(16)38765-x. [DOI] [PubMed] [Google Scholar]
- 9.Hishitani T, Ogawa K, Hoshino K, et al. Lobar emphysema due to ductus arteriosus compressing right upper bronchus in an infant with congenital heart disease. Ann Thorac Surg. 2003;75:1308–10. doi: 10.1016/s0003-4975(02)04623-4. [DOI] [PubMed] [Google Scholar]
- 10.Isojima A, Yuasa H, Kusagawa M, et al. Surgical treatment of infantile lobar emphysema in cardiovascular disease with left-to-right shunts. Jpn J Surg. 1978;8:57–65. doi: 10.1007/BF02469336. [DOI] [PubMed] [Google Scholar]
- 11.Karnak I, Senocak ME, Ciftci AO, Büyükpamukçu N. Congenital lobar emphysema: diagnostic and therapeutic considerations. J Pediatr Surg. 1999;34:1347–51. doi: 10.1016/s0022-3468(99)90009-x. [DOI] [PubMed] [Google Scholar]
- 12.Eigen H, Lemen RJ, Waring WW. Congenital lobar emphysema: long-term evaluation of surgically and conservatively treated children. Am Rev Respir Dis. 1976;113:823–31. doi: 10.1164/arrd.1976.113.6.823. [DOI] [PubMed] [Google Scholar]


