Abstract
AIMS
The purpose of this study was to evaluate whether yoga training in addition to standard medical therapy can improve cardiac function and reduce N terminal pro B-type natriuretic peptide (NT pro BNP) in heart failure (HF).
METHODS
130 patients were recruited and randomized into two groups: Control Group (CG) (n = 65), Yoga Group (YG). In YG, 44 patients and in CG, 48 patients completed the study. Cardiac function using left ventricular ejection fraction (LVEF), myocardial performance index (Tei index), and NT pro BNP, a biomarker of HF, was assessed at baseline and after 12 weeks.
RESULT
Improvement in LVEF, Tei index, and NT pro BNP were statistically significant in both the groups. Furthermore, when the changes in before and after 12 weeks were in percentage, LVEF increased 36.88% in the YG and 16.9% in the CG, Tei index was reduced 27.87% in the YG and 2.79% in the CG, NT pro BNP was reduced 63.75% in the YG and 10.77% in the CG. The between group comparisons from pre to post 12 weeks were significant for YG improvements (LVEF, P < 0.01, Tei index, P < 0.01, NT pro BNP, P < 0.01).
CONCLUSION
These results indicate that the addition of yoga therapy to standard medical therapy for HF patients has a markedly better effect on cardiac function and reduced myocardial stress measured using NT pro BNP in patients with stable HF.
Keywords: yoga therapy, heart failure, ejection fraction, Tei index, NT pro BNP
Introduction
Heart failure (HF) is one among the most prevalent chronic illnesses with a profound clinical and economic impact on society.1,2 Previously, researchers have concentrated on the systolic dysfunction to explain the clinical features of HF.3 Consequently, treatment strategies such as preload and afterload reduction or the use of diuretic agents have been established for patients with reduced systolic left ventricular function. More recently, it has been determined that systolic and diastolic dysfunctions coexist in the majority of patients with congestive HF.4 N Terminal pro BNP (NT pro BNP) is a cardiac neuro hormone that is secreted from the myocardium in response to increased intracardiac pressure or volume.5 Measurement of NT pro BNP can help in earlier identification, better risk stratification,6 and better correlation with the severity of HF.7
Earlier reports have supported the interventions aimed to treat the symptoms of HF and to improve quality of life.8 Asana (postures) and pranayama (breathing exercises) in the form of yoga may be beneficial in the rehabilitation of cardio vascular diseases.9 Despite the widespread appeal of yoga, data on whether the practice of yoga improves cardiac function in patients with HF are limited.10
Yoga is the combination of structured physical and breathing techniques and meditation that helps to stimulate a sense of well-being. The relaxation, breathing, and meditation components may lead to decreased sympathetic activation, increased parasympathetic activity and improved baroreflex sensitivity causing a reduction in hypertension, which significantly impacts HF and other cardiovascular diseases. Studies have demonstrated the effect of yoga on improvement of lipid profiles,11 blood pressure,12 psychological well-being, regression of atherosclerosis when combined with dietary and other lifestyle modifications,13,14 and left ventricular ejection fraction (LVEF) in coronary heart patients.15 To our knowledge, there is little evidence regarding the effectiveness of yoga therapy on cardiac function and NT pro BNP in HF. Moreover, the clinical utility of the previous studies were limited by varied intensity, lack of control groups, and the duration of the yoga interventions.
The objective of this research was to study the effect of yoga therapy in addition to standard medical therapy on cardiac function and NT pro BNP in stable HF patients.
Materials and Methods
Study design
This study was a randomized parallel group controlled trial where the outcome assessor was blinded to the type of therapy. HF patients were assigned prospectively by randomization in a 1:1 ratio into the Yoga Group (YG) or the Control Group (CG) of the study. The randomization was done by referring to a computer generated randomization list. The details of the allocation sequence were contained in a set of sealed opaque envelopes and were not known to the investigators who enrolled the participants.
Study population
Patients were recruited from the Cardiology Outpatient Department of the Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. Initially 942 HF patients were interviewed regarding their participation in this study. 748 patients did not meet the inclusion criteria, 64 patients declined to participate. The inclusion criteria consisted of systolic and/or diastolic dysfunction, ejection fraction of 30–50%, satisfaction of the New York Heart Association (NYHA) Class I–II classification, ability to walk without assistance, and use of stable medical therapy. Patients who had chronic obstructive pulmonary disease (COPD), were unable to attend yoga sessions, had orthopedic impediments to yoga, had undergone hospitalization within the last three months, and were suffering from myocardial infarction or recurrent angina within the last six months were excluded from the study. The study was approved by the Institute Ethics Committee of JIPMER, Puducherry. A total of 130 patients were recruited and randomized into two groups, CG (n = 65) receiving standard medical therapy and YG receiving standard medical therapy plus yoga therapy. The study was completed by 44 patients in YG and 48 patients in CG. Patients gave their written, informed consent to participate in the study.
Demographic data
Demographic data of the current study, such as gender, NYHA classification, hypertensive, coronary artery disease, diabetics, drugs, and other parameters were comparable (Table 1).
Table 1.
Patients demographic and baseline clinical characteristics.
| SL.NO | TOTAL NO OF PATIENTS N = (92) | YOGA GROUP (YG) N = (44) | CONTROL GROUP (CG) N = (48) |
|---|---|---|---|
| 1 | Age (Years) | 49.34 ± 5.70 | 50.14 ± 4.54 |
|
| |||
| 2 | Men/Women, n (%) | 32/12, (72.72%)/(27.27%) | 32/16, (66.66%)/(33.33%) |
|
| |||
| 3 | Height (cm) | 162.74 ± 8.03 | 163.24 ± 6.88 |
|
| |||
| 4 | Weight (kg) | 70.16 ± 8.24 | 70.46 ± 6.71 |
|
| |||
| 3 | Systolic dysfunction | 28 (63.63%) | 30 (62.5%) |
| Diastolic dysfunction | 16 (36.36%) | 18 (37.5%) | |
|
| |||
| 4 | NYHA class, n (%) | ||
| I | 13 (29.55%) | 14 (29.17%) | |
| II | 31 (70.45%) | 34 (70.83%) | |
|
| |||
| 5 | Medical History, n (%) | ||
| CAD | 19 (43.18%) | 26 (54.17%) | |
| HTN | 37 (84.09%) | 36 (75%) | |
| DM | 14 (31.82%) | 20 (41.66%) | |
| β-blockers | 34 (77%) | 38(79%) | |
| Statins | 30 (68%) | 32(67%) | |
| ACE inhibitor/Angiotensin II receptor blocker | 08 (18%) | 04(8%) | |
| Diuretics | 04 (9%) | 03(6%) | |
| Oral antiplatelet agents | 13 (30%) | 15(31%) | |
| Antidiabetics | 10(23%) | 12(25%) | |
Yoga therapy
Yoga sessions were conducted at the Advanced Centre for Yoga Therapy Education and Research (ACYTER), JIPMER, in the vicinity of the Department of Cardiology. Yoga therapy was designed in consultation with a cardiologist who was experienced in this form of therapy and research in conjunction with a yoga therapist having expertise in cardiac rehabilitation. Each session lasted around 60 minutes. After two weeks of participation in monitored sessions, they practiced the same for three days under our direct supervision, and three days at their homes for a total duration of 12 weeks.
According to individual medical or orthopedic limitations, the asana were modified. “Pranayama consisted of deep inhalation and exhalation in a 1:1 ratio, without breath retention. Inhalation was taught to commence with sequential involvement of the abdomen, lower chest, and then, the upper chest, and the same sequence was performed in reverse, during exhalation. Meditation and relaxation practice were performed in a supine or seated position according to the participant’s comfort level and preference”.10
Assessment of cardiac function: each participant underwent an initial resting echocardiogram in multi views before the yoga program was initiated. Another echocardiogram was taken upon completion of the three-month cardiac rehabilitation yoga program. Images were taken with patients in the left lateral decubitus position with a 3.75 MHz sector probe using a commercially available Philips CX50, a Power Vision machine. An electrocardiogram was simultaneously recorded for each patient. Echocardiographic examinations were done using standard views and techniques according to the guidelines of the American Society of Echocardiography.16 LVEF was measured as previously described by Quinones and co-workers.17 For recordings of the mitral inflow velocity pattern, the sample volume (size 2 mm) of the pulsed Doppler was placed between the tips of the mitral leaflets in the apical four-chamber view. Accordingly, the left ventricular outflow velocity was recorded from the apical long-axis view with the sample volume of the pulsed Doppler positioned just below the aortic annulus. Two-dimensional and Doppler tracings were recorded over five cardiac cycles at a sweep speed of 50 or 100 mm s−1. Three consecutive beats were measured and averaged for each parameter. Doppler time intervals were measured from mitral inflow and left ventricular outflow Doppler tracings, as described by Tei and coworkers18 (Fig. 1). The interval “a” from cessation to onset of mitral inflow is equal to the sum of isovolumic contraction time, ejection time, and isovolumic relaxation time. Ejection time “b” is derived from the duration of the left ventricular outflow Doppler velocity profile. The sum of isovolumetric contraction time and isovolumic relaxation time was obtained by subtracting b from a. The Tei index was calculated as shown in Figure 1: (a − b)/b. Isovolumic relaxation time was measured by subtracting the interval d between the R wave and cessation of left ventricular outflow from the interval c between the R wave and the onset of mitral inflow.19 Isovolumic contraction time was calculated by subtracting isovolumic relaxation time from a − b (Fig. 1). Peak velocities of early (E) and late (A) filling were derived from the mitral inflow velocity curve.4
Figure 1.
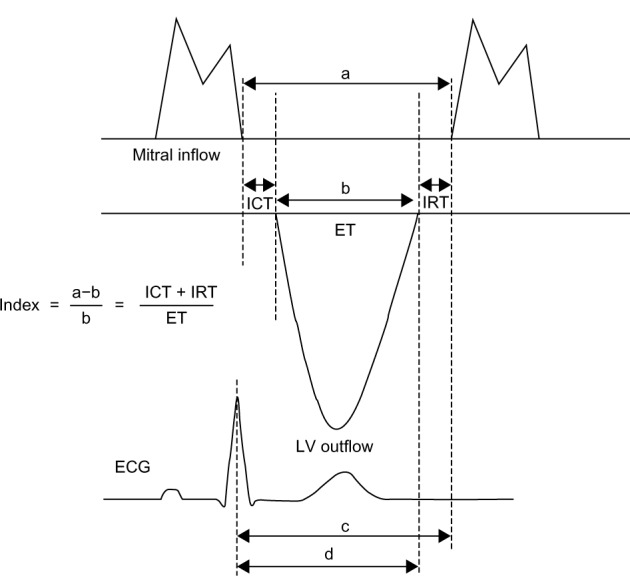
Schema for measurements of Doppler time intervals (according to Tei et al.18). The index (ICT + IRT/ET) is derived as (a − b/b), where a is the interval between cessation and onset of the mitral inflow, and b is the ejection time (ET) of left ventricular (LV) outflow. Isovolumetric relaxation time (IRT) is measured by subtracting the interval c between the R wave (ECG) and the cessation of LV outflow from the interval d between the R wave and the onset of mitral inflow (according to Kleinet al.19) Isovolumetric contraction time (ICT) is derived by subtracting IRT from a − b. ECG: electrocardiogram.
Blood collection and storage and NT pro BNP measurement
Blood was collected through venipuncture, allowed to clot, and centrifuged at 3,000 RPM at 4 °C for 10 minutes (Remi-refrigerated centrifuge) and the serum was separated and stored in a frozen state at −80 °C for analysis. NT pro BNP was measured using a commercially available ELISA kit (Uscn Life Science Inc).
Sample size and statistical analysis
A sample size of 40 in each group has a 90% power to detect a difference between means of LVEF of 4.16 with a significance level (alpha) of 0.05 (two-tailed). With 20% expected dropout, sample size was adjusted to 48 patients in each group.
Statistical analyses were done using the Statistical Package for Social Sciences 19 (IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp.). Data were expressed as mean ± SD with 95% confidence interval (CI). Two-tailed paired t-test was performed for within group differences. For between group comparisons, ANCOVA was used with baseline as a covariate. A two-tailed P-value <0.05 was considered statistically significant.
Results
Cardiac function: statistically significant improvement was found within group. LVEF and Tei index: LVEF was increased from 38.93 ± 5.1 to 52.96 ± 6.01 (P < 0.01) in YG, 39.65 ± 5.25 to 45.83 ± 5.68 (P < 0.01) in CG, Tei index was reduced from 0.53 ± 0.08 to 0.50 ± 0.07 (P < 0.01) in CG, 0.54 ± 0.85 to 0.38 ± 0.03 (P < 0.01) in YG. However, when the changes in before and after 12 weeks were in percentage, LVEF was increased 36.88% in YG and 16.9% in CG, Tei index was reduced 27.87% in YG and 2.79% in CG. However, between group comparisons from pre to post 12 weeks were significant for YG improvements (LVEF, P < 0.01, Tei index, P < 0.01; Table 2).
Table 2.
Between group, within group, mean% changes of NT pro BNP, EF%, Tei index.
| SL.NO | PARAMETER | TIME= 0 MONTHS | TIME= 3 MONTHS | % CHANGE FROM BASELINE (MEAN) |
|---|---|---|---|---|
| 1 | NT pro BNP | |||
| Control | 5495.47 ± 1382.50 | 4722.62 ± 1924.70* | 10.77 | |
| Yoga | 3965.48 ± 1365.08 | 1395 ± 997.08**$$ | 63.75 | |
|
| ||||
| 1 | EF (%) | |||
| Control | 39.65 ± 5.25 | 45.83 ± 5.68** | −16.09 | |
| Yoga | 38.93 ± 5.1 | 52.96 ± 6.01**$$ | −36.88 | |
|
| ||||
| 2 | Tei index | |||
| Control | 0.53 ± 0.08 | 0.50 ± 0.07** | 2.79 | |
| Yoga | 0.54 ± 0.85 | 0.38 ± 0.03**$$ | 27.87 | |
Notes:
Indicates within group
indicates between group.
P < 0.05
P < 0.01.
P < 0.001.
NT pro BNP level
12 weeks of yoga therapy resulted in significant decrease in YG (pre: 3965.48 ± 1365.08, post: 1395 ± 997.08, P < 0.01) and in CG (pre: 5495.47 ± 1382.50, post: 4722.62 ± 1924.70, P < 0.05). However, when the changes in before and after 12 weeks were expressed in percentage, NT pro BNP was reduced 63.75% in YG and 10.77% in CG. Between group difference was statistically significant (P < 0.01) (Table 2). The reduction in NT pro BNP, a biomarker of myocardial stress was negatively correlated with increased LVEF (r = −0.407) (Fig. 2) and positively correlated with reduced Tei index in YG (r = 0.132) (Fig. 3).
Figure 2.

Scatter graph showing the correlation between change in LVEF and NT pro BNP in YG (r = −0.407).
Figure 3.
Scatter graph showing the correlation between change in Tei index and NT pro BNP in YG (r = 0.132).
Discussion
Current medical therapy for HF is based on after load reduction by agents such as angiotensin converting enzyme (ACE) inhibitors, reduction of fluid retention by diuretics, drugs to enhance myocardial contractility, and use of beta-blockers. With the existing therapy, the mortality rate remains high and the quality of life and morbidity are significantly impaired.20 Though these agents have improved the symptoms of congestive HF, prognosis is still poor and there is a need for alternative or further treatment strategies. This study is unique in that there is deficiency of data on the effect of yoga, a mind body technique that involves meditation, and a set of physical exercises performed in the sync with breathing exercises, on cardiac function measured by LVEF, Tei index, and NT pro BNP in stable HF. To our knowledge, this is the first study that explores the effect of yoga therapy in addition to standard medical therapy on cardiac function and NT pro BNP. The central findings of our study were that a 12 week yoga therapy, when added to the standard medical therapy for patients with stable HF, leads to reduced NT pro BNP and improved LVEF and Tei index.
In this study, we assessed cardiac function using measurements of systolic function using LVEF and Tei index. This is defined as the sum of isovolumic contraction and relaxation time divided by the ejection time, was reported to be simple, reproducible, and independent of heart rate and blood pressure,18 and is a sensitive indicator of overall cardiac dysfunction in patients with mild-to-moderate HF.4
Results of this study demonstrated that the addition of two weeks of yoga therapy to standard medical therapy improves cardiac function measured by LVEF and Tei index, and reduces myocardial stress measured by NT pro BNP. Mechanisms by which yoga may improve cardiac function and reduce myocardial stress are speculated at this time. Combination of yoga asana with breathing exercises and meditation reduces the sympathetic activity and could lead to a decrease in ventricular filling pressures.22 “In addition to allowing for a predominance of the parasympathetic state, yoga may also promote effective extraction of oxygen by peripheral tissues. When muscle is stretched, the O2 consumption increases. Studies that examined the health-related aspects of yoga found that 8 week yoga training increased muscular strength by 31%, increased muscular endurance by 57%, increased flexibility by 88%, increased oxygen uptake by 7% and reduced cardiovascular risk in healthy adults”.23 This reduces load and stress on the myocardium. It seems to support the current study’s reduction in NT pro BNP by 63.75% in YG compared to 10.77% in CG; Tei index was 27.87% in YG, 2.79% in CG; and LVEF increase in YG was 36.88%, whereas in CG, it was 10.77% only. The reduction in NT pro BNP, a biomarker of myocardial stress, was negatively correlated with increased LVEF (r = −0.407) (Fig. 2) and positively correlated with reduced Tei index in YG (r = 0.132) (Fig. 3). However, the weak correlation with Tei index may be because of medium sample size and short duration of yoga therapy. This may be addressed in future studies with larger sample size.
To assess the safety of the subjects during the yoga training, blood pressure and vital signs were checked before and after each yoga therapy session. In addition, the subjects were asked about soreness of the muscle before and after the yoga practice as well as any emergency department visits or hospitalization since the last yoga session. We found that there were no cardiac symptoms (shortness of breath, light-headedness), cardiac problems, or orthopedic injuries, during or in relation to the yoga sessions.
Conclusion
Results of this study demonstrate that a 12 week yoga therapy in addition to standard medical therapy improves cardiac function and myocardial stress in patients with stable HF. The improvement in cardiac function and myocardial stress seems to translate into a lower mortality rate. The clinical implication is that moderate physical activity in the form yoga asana, pranayama, and relaxation may be recommended in conjunction with standard medical therapy in stable HF patients.
Limitations
Effect of yoga on HF because of specific etiology was not assessed in the present study. Besides, we could not recruit more patients because of the high cost of NT pro BNP measurement. Finally, the short term follow up of our patients, confined to 12 weeks is another limitation.
Figure 4.
Flow chart of study recruitment.
Yoga therapy schedule.
| SL.NO | NAME OF THE PRACTICE | REPETITION | DURATION (60MIN) APPROX |
|---|---|---|---|
| 1 | Loosening practices | 1 | 10 min |
| 2 | Makarasana | 1 | 2 min |
| 3 | Tadasana | 2 | 2 min |
| 4 | Trikonasana | 2 | 2 min |
| 5 | Veerasana | 2 | 2 min |
| 6 | Ardhakati Chakrasana | 2 | 2 min |
| 7 | Vakrasana | 2 | 2 min |
| 8 | Matsysana | 2 | 2 min |
| 9 | Makarasana | 1 | 2 min |
| 10 | Meditation | 1 | 10 min |
| 11 | Chandranadi Pranayama | 10 | 5 min |
| 12 | Bhramari Pranayama | 2 | 2 min |
| 13 | AUM chanting | 4 | 2 min |
| 14 | Shavasana | 1 | 15 min |
Acknowledgments
We extend our sincere thanks to the personnels of echocardiography lab, Department of Cardiology and ELISA lab, Department of Biochemistry, JIPMER, Puducherry, India, for their kind cooperation and Programme Director, ACYTER, JIPMER for providing laboratory facilities and Yoga therapy.
Footnotes
Author Contributions
BHK and JB conceived and designed the experiments. BHK and EJ analyzed the data. BHK and EJ wrote the first draft of the manuscript. PP, GKP, JB, YS, MGS, and GSG contributed to the writing of the manuscript. BHK, JB, PP, GKP, YS, MGS, GSG, and EJ agree with manuscript results and conclusions. BHK, JB, PP, GKP, YS, MGS, GSG, and EJ jointly developed the structure and arguments for the paper. BHK, JB, PP, GKP, YS, MGS, GSG, and EJ made critical revisions and approved the final version. All authors reviewed and approved the final manuscript.
ACADEMIC EDITOR: Steven Gurgevich, Editor in Chief
FUNDING: We gratefully acknowledge the Department of Science and Technology (DST) for giving Junior Research Fellowship under the AORC component of the INSPIRE fellowship, and the Director, JIPMER, for providing partial funding through an intramural research grant (PhD).
COMPETING INTERESTS: Author(s) disclose no potential conflicts of interest.
DISCLOSURES AND ETHICS
As a requirement of publication the authors have provided signed confirmation of their compliance with ethical and legal obligations including but not limited to compliance with ICMJE authorship and competing interests guidelines, that the article is neither under consideration for publication nor published elsewhere, of their compliance with legal and ethical guidelines concerning human and animal research participants (if applicable), and that permission has been obtained for reproduction of any copyrighted material. This article was subject to blind, independent, expert peer review. The reviewers reported no competing interests.
REFERENCES
- 1.Adams KF, Jr, Zannad F. Clinical definition and epidemiology of advanced heart failure. Am Heart J. 1998;135:S204–S215. doi: 10.1016/s0002-8703(98)70251-0. [DOI] [PubMed] [Google Scholar]
- 2.Masoudi FA, Baillie CA, Wang Y, et al. The complexity and cost of drug regimens of older patients hospitalized with heart failure in the United States, 1998–2001. Arch Intern Med. 2005;165:2069–76. doi: 10.1001/archinte.165.18.2069. [DOI] [PubMed] [Google Scholar]
- 3.Wilson JR, Ferraro N. Exercise intolerance in patients with chronic left heart failure: relation to oxygen transport and ventilatory abnormalities. Am J Cardiol. 1983;51:1358–63. doi: 10.1016/0002-9149(83)90312-0. [DOI] [PubMed] [Google Scholar]
- 4.Bruch C, Schmermund A, Marin D, et al. Tei-index in patients with mild-to-moderate congestive heart failure. Eur Heart J. 2000;21:1888–95. doi: 10.1053/euhj.2000.2246. [DOI] [PubMed] [Google Scholar]
- 5.Belagavi AC, Rao M, Pillai AY, Srihari US. Correlation between NT proBNP and left ventricular ejection fraction in elderly patients presenting to emergency department with dyspnoea. Indian Heart J. 2012;64:302–4. doi: 10.1016/S0019-4832(12)60091-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palazzuoli A, Gallotta M, Quatrini I, Nuti R. Natriuretic peptides (BNP and NT-proBNP): measurement and relevance in heart failure. Vasc Health Risk Manag. 2010;6:411–8. doi: 10.2147/vhrm.s5789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SC, Stevens TL, Sandberg SM, et al. The potential of brain natriuretic peptide as a biomarker for New York Heart Association class during the outpatient treatment of heart failure. J Card Fail. 2002;8:149–54. doi: 10.1054/jcaf.2002.125368. [DOI] [PubMed] [Google Scholar]
- 8.Walke LM, Byers AL, Gallo WT, Endrass J, Fried TR. The association of symptoms with health outcomes in chronically ill adults. J Pain Symptom Manage. 2007;33:58–66. doi: 10.1016/j.jpainsymman.2006.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bulavin VV, Kliuzhev VM, Kliachkin LM, Lakshmankumar, Zuikhin ND, Vlasova TN, et al. Elements of yoga therapy in the combined rehabilitation of myocardial infarct patients in the functional recovery period. Vopr Kurortol Fizioter Lech Fiz Kult. 1993:7–9. [PubMed] [Google Scholar]
- 10.Pullen PR, Nagamia SH, Mehta PK, et al. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J Card Fail. 2008;14:407–13. doi: 10.1016/j.cardfail.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Mahajan AS, Reddy KS, Sachdeva U. Lipid profile of coronary risk subjects following yogic lifestyle intervention. Indian Heart J. 1999;51:37–40. [PubMed] [Google Scholar]
- 12.Selvamurthy W, Sridharan K, Ray US, et al. A new physiological approach to control essential hypertension. Indian J Physiol Pharmacol. 1998;42:205–13. [PubMed] [Google Scholar]
- 13.Ornish D. Can lifestyle changes reverse coronary heart disease? World Rev Nutr Diet. 1993;72:38–48. doi: 10.1159/000422326. [DOI] [PubMed] [Google Scholar]
- 14.Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. 2001;4:165–70. doi: 10.1111/j.1520-037x.2001.00542.x. [DOI] [PubMed] [Google Scholar]
- 15.Paul Biman Bihari. Effect of shavasan practices on coronary heart patients with special reference to shavasan and meditation. Int Sci Yoga J Sense. 2011;1:86–91. [Google Scholar]
- 16.Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American society of echocardiography committee on standards, subcommittee on quantitation of two-dimensional echocardiograms. J Am Soc Echocardiogr. 1989;2:358–67. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 17.Quinones MA, Waggoner AD, Reduto LA, et al. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981;64:744–53. doi: 10.1161/01.cir.64.4.744. [DOI] [PubMed] [Google Scholar]
- 18.Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function–a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26:357–66. [PubMed] [Google Scholar]
- 19.Klein AL, Burstow DJ, Tajik AJ, Zachariah PK, Bailey KR, Seward JB, et al. Effects of age on left ventricular dimensions and filling dynamics in 117 normal persons. Mayo Clin Proc. 1994;69:212–24. doi: 10.1016/s0025-6196(12)61059-3. [DOI] [PubMed] [Google Scholar]
- 20.Cohn JN. The management of chronic heart failure. N Engl J Med. 1996;335:490–8. doi: 10.1056/NEJM199608153350707. [DOI] [PubMed] [Google Scholar]
- 21.Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995;26:135–6. [PubMed] [Google Scholar]
- 22.Pullen PR, Thompson WR, Benardot D, et al. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. 2010;42:651–7. doi: 10.1249/MSS.0b013e3181bf24c4. [DOI] [PubMed] [Google Scholar]
- 23.Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. 2001;4:165–70. doi: 10.1111/j.1520-037x.2001.00542.x. [DOI] [PubMed] [Google Scholar]




