Multiple myeloma (MM) has the highest incidence of bone involvement amongst malignant diseases (1). Myeloma bone disease (MMBD) is characterized by osteoclast (OCL) activation with suppressed or absent osteoblast (OBL) function resulting in local bone destruction without new bone formation (2). IL-3 is a bifunctional cytokine that is upregulated in MM patients, increases myeloma cell and OCL proliferation, and indirectly suppresses osteoblastogenesis via CD14+ BM monocytes (BMM)(3, 4). However, the monocyte / macrophage-derived mediators of IL-3’s effects in MMBD are unknown.
To identify mediators of IL-3’s bone remodeling effects in MM we performed gene expression profiling of IL-3 treated MM patient CD14+ peripheral blood cells, as previously described (5). The INHBA gene, which codes for Activin A (6), was upregulated 184-fold. The data in this publication has been deposited in NCBI’s Gene Expression Omnibus and are accessible through GEO Series accession number GSE41992. ActA is a pluripotent TGF-β cytokine that stimulates osteoclastogenesis, inhibits OBLs, and is overproduced in MM. In MM patients, ActA levels correlate with advanced disease and bone involvement (7, 8), thus we hypothesized that ActA mediates IL-3’s bone effects in MM.
We confirmed our gene expression profiling findings by quantifying protein levels of IL-3 induced ActA production from healthy subject, MGUS patient, and MM patient CD14+ BMMs by ELISA (Quantikine® human/mouse/rat Activin A ELISA kit, R&D Systems, Minneapolis, MN). BM aspirates and peripheral blood samples were collected from healthy donors and MM or MGUS patients as previously described (3). Studies were approved by each institution’s Institutional Review Boards. IL-3 induced a 70-fold increase in ActA production by MM patient derived cells and a 10-fold increase in healthy donor samples.
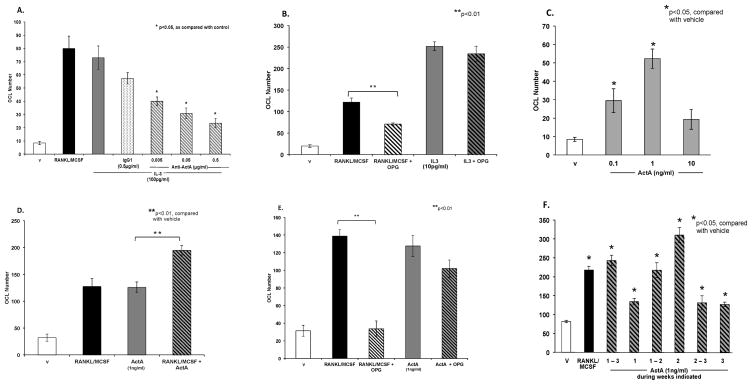
As CD14+ BMM are OCL precursors and IL-3 is a potent inducer of OCL formation (3), we evaluated the role of ActA in IL-3 mediated OCL formation. Nonadherent BM cells from healthy subjects were cultured in the presence or absence of varying concentrations of cytokines or an ActA neutralizing antibody (Anti-ActA) (R&D Systems, Minneapolis, MN) for 3 weeks, as previously described (3). An isotype-specific mouse IgG was used as control for anti-ActA antibody treatment. IL-3 treatment of OCL precursors in the presence of anti-ActA dose-dependently inhibited the osteoclastogenic effect of IL-3 on OCL formation (Figure 1A). Consistent with these findings ActA dose-dependently increased OCL formation with doses of 0.1 and 1 ng/ml (Figure 1B).
Figure 1.
Figure 1A: Anti-Activin A decreases IL-3 induced osteoclastogenesis. Human non-adherent BM cells (OCL precursors) were cultured in the presence of vehicle, rhRANKL (50ng/ml) with rhMCSF (10ng/ml), IL-3 (100pg/ml) , IL-3 with IgG1 isotype control (0.5μg/ml), and varying concentrations of a neutralizing antibody to ActA (anti-ActA) in combination with IL-3. Following 21days of culture, cells were fixed and stained. 23c6+ multinucleated cells were counted. The osteoclastogenic effects of IL-3 were significantly inhibited by anti-ActA in a dose-dependent manner.
Figure 1B: IL-3 induced osteoclastogenesis is RANKL independent. OCL precursors were cultured in the presence of RANKL/MCSF or IL-3 (10pg/ml) in the presence or absence of osteoprotegerin (OPG), a decoy receptor for RANKL. OPG completely inhibited RANKL induced OCL formation, as expected. However, OPG only slightly decreased IL-3 induced OCL formation, demonstrating that IL-3 induced osteoclastogenesis occurs via a RANKL-independent mechanism.
Figure 1C: ActA increases OCL number. OCL precursors were cultured in the presence of varying doses of ActA for 21 days. At the end of the culture period cells were fixed and stained for α5β3 integrin with 23c6+ antibody. 23c6+ multinucleated cells were quantified. ActA enhances osteoclastogenesis significantly at doses of 0.1 and 1 ng/ml.
Figure 1D: RANKL enhances ActA induced osteoclastogenesis. OCL precursors were cultured in RANKL/MCSF, ActA alone (1ng/ml), or both for 21 days. At the conclusion of the culture period, cells were fixed and stained. 23c6+ cells were counted. ActA induced osteoclastogenesis was significantly increased in the presence of RANKL/MCSF.
Figure 1E: ActA induced osteoclastogenesis is also RANKL independent. OCL precursors were cultured in the presence of RANKL/MCSF or ActA in the presence or absence of OPG. OPG alone modestly reduced ActA induced OCL formation, demonstrating that ActA induced osteoclastogenesis, like IL-3 induced osteoclastogenesis, is RANKL-independent.
Figure 1F: Activin A acts early in osteoclastogenesis. OCL precursors were cultured in the presence of ActA during specified weeks of culture, then fixed and stained for 23c6+. While all cultures treated with ActA had significantly greater numbers of OCL than control culture (RANKL/MCSF), the most pronounced effect occurred during the first two weeks of culture.
We previously reported that the combination of RANKL and IL-3 enhances OCL formation over IL-3 induced osteoclastogenesis alone (3). Thus, we next tested if IL-3 enhances osteoclastogenesis via a RANKL-independent mechanism. OCL precursors were treated with IL-3 and osteoprotegrin (OPG), the RANKL decoy receptor. OPG did not significantly reduce IL-3 induced OCL formation (Figure 1B). Others have reported that ActA stimulates OCL differentiation in the presence of RANKL and MCSF (8, 9). We confirmed this and demonstrate that BMM treated with ActA alone (Figure 1C) and in combination with low concentrations of RANKL/MCSF increased OCL formation compared with RANKL/MCSF induced osteoclastogenesis (Figure 1D). Similar to IL-3, treatment of OCL-precursors with ActA and OPG did not block ActA-induced OCL, though RANKL-induced OCL was fully inhibited (Figure 1E). This suggests that both ActA and IL-3 induce OCL via a RANKL-independent mechanism.
We then examined the time-course of ActA’s effects on OCL formation. OCL precursors proliferate during the first week of marrow culture and differentiate and fuse during the second and third weeks of culture. ActA was added to BM cultures at set time points to determine if it affects OCL proliferation or differentiation. Analogous to our finding that IL-3 increases OCL formation early in the culture period (3), the most pronounced effect occurred with addition of ActA during weeks 1 and 2 or week 2 of culture (Figure 1F). As ActA’s primary effect on osteoclastogenesis occurs early, we evaluated whether IL-3 induced ActA expression decreases during OCL differentiation. CD14+ BMM were cultured with RANKL/MCSF to induce OCL, and at designated time points cells were treated with IL-3 for 24h. Conditioned media ActA levels were quantified by ELISA. IL-3 induced ActA secretion was significantly higher than basal ActA secretion at days 1 and 14 of OCL differentiation, with a 62-fold increase in IL-3 induced CM ActA levels at day 1, a 14-fold increase at day 14, and an 8-fold increase at day 28. As IL-3 signals through the IL-3 receptor (IL-3R, CD123), we next tested if OCL precursor expression of IL-3R changes during OCL maturation. CD123 is highly expressed on early OCL precursors, with 83% of CD14+ cells expressing CD123. Expression of CD123 steadily decreased during the course of OCL differentiation, with 66% of CD14+ derived cells expressing CD123 at day 7, 55% at day 14, and 25% at day 28.
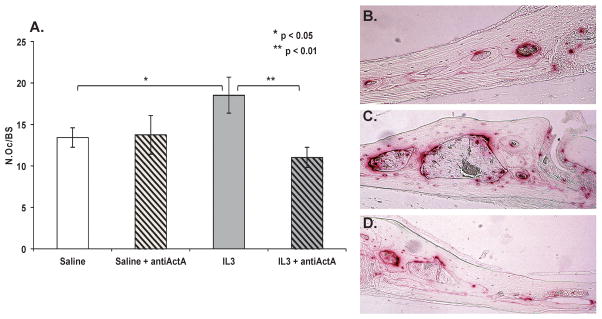
Finally, to determine if IL-3 enhances OCL in vivo, and if ActA mediates these effects, mice were injected intraperitoneally with saline (100μl) or anti-ActA (1μg in 100μl PBS) for 7 days. Beginning on day 3, mice were injected subcutaneously over the calvaria with m-IL-3 (1μg in 50μl PBS) or saline (50μl) daily for 5 days under anesthesia. Mice were sacrificed after 7 days. Animal protocols were approved by the Institutional Animal Care and Use Committee of Virginia Commonwealth University. TRAP+ OCL were counted on the endosteal bone surfaces of the calvaria and data were expressed as the number of OCL per endosteal bone surface, corrected for bone surface area (N.Oc/BS). All histomorphometry analyses were done on images captured using a Leica microscope with a Q-imaging camera using Bioquant Osteo software automated measuring system (Bioquant Imaging Corporation). TRAP+ OCL per field were quantified. OCL numbers on the endosteal bone surfaces, corrected for bone surface area (N.Oc/BS), were dramatically increased by IL-3 treatment compared to saline controls (Figure 2). Further, treatment of mice with intraperitoneal anti-ActA prior to and during supracalvarial IL-3 treatment significantly reduced IL-3 induced N.Oc/BS.
Figure 2.
Figure 2A: IL3 increases osteoclast numbers in vivo and AntiActA inhibits this effect in vivo. C57BL 9-week-old mice per group were injected intraperitoneally with saline (100 μl) or antiActA (1μg in 100μl PBS) for 7 days and injected subcutaneously over the calvaria with mIL-3 (1μg in 50μl PBS) or saline daily for 5 days under light isoflurane anesthesia. After 7 days, mice were sacrificed and calvaria fixed, decalcified, and sectioned in a coronal orientation posterior to the junction of the sagittal and coronal suture and stained for TRAP. TRAP+ osteoclasts were counted on the endosteal bone surfaces. IL-3 treatment resulted in significantly more TRAP+ cells on the endosteal surface of the calvaria as compared with saline treated controls (mean N.Oc/BS saline treated control 13.42, SD 1.18; supracalvarial IL-3 treatment 18.51, SD 2.14, p < 0.05). Animals treated with intraperitoneal anti-ActA in combination with IL-3 had a reduced number of TRAP+ cells as compared with IL-3 treated animals only, (mean N.Oc/BS supracalvarial IL-3 with intraperitoneal antiActA 11.01, SD 1.2, p<0.01).
Figure 2B - D: IL-3 increases TRAP+ OCL formation in vivo and intraperitoneal treatment with an ActA neutralizing antibody abrogates the osteoclastogenic effect of IL-3. Representative images of calvaria sections from mice treated with subcutaneous supracalvarial injections of saline (B) as compared with IL-3 (C) are shown. TRAP+ OCL stain red. Significantly more TRAP activity (red stained cells) is seen in calvarial sections from mice treated with IL-3 as compared with saline control. (D) Mice were treated with IL-3 in combination with intraperitonal antiActA, which significantly decreased the osteoclastogenic effect of IL-3. Images were captured at x20 magnification for four consecutive fields lateral to the sagittal suture. Reduced TRAP activity is seen in calvarial sections from mice treated with IL-3 in combination with anti-ActA as compared with IL-3 treatment alone.
MMBD continues to be a significant cause of patient morbidity and a major source of health care expenditures. We previously reported that IL-3 enhances MM cell proliferation, OCL formation, and indirectly suppresses OBL differentiation via BMM, and that IL-3 levels are increased in 75% of MM patients (3, 4). We confirmed that IL-3 levels are increased in MM patients by measuring bm plasma IL-3 levels in a large cohort of MM patients (n=130) and healthy individuals (n=36). Consistent with our previous findings, IL-3 levels were elevated in MM patients as compared with healthy individuals. (Mean IL-3 healthy: 62.98 pg/ml, minimum 0, maximum 1104.17; MM mean IL-3: 247.57 pg/ml, minimum 0, maximum 9527.28, p<0.05.) Mean IL-3 levels were also higher in MM patients with one or more skeletal lesions (mean with skeletal lesions: 304.23 pg/ml, n = 49, mean without skeletal lesions 87 pg/ml, n = 87), though results did not reach statistical significance due to the highly skewed distribution of IL-3 levels between populations. While these findings suggest that IL-3 could be an ideal therapeutic target for MM, IL-3 has widespread effects on multiple hematopoietic cell types. Thus, effective targeting of IL-3 requires an improved understanding of its mechanism of action in MMBD.
ActA is one of the most abundant TGF-β/BMP family members in bone (9) and is an important regulator of osteolysis in MM (8). A soluble activin receptor antagonist (9, 10) that inhibits MM growth and reverses osteoblast inhibition (8) is currently under investigation. Lenalidomide, an immunomodulator highly active in MM has recently been shown to increase ActA secretion from bone marrow stromal cells (11), however the mechanism for ActA upregulation in MM has not previously been identified. In this study we demonstrate that ActA is upregulated with IL-3 treatment, that IL-3 induces OCL in vivo, and that antiActA blocks the effects of IL-3 on OCL formation in vitro and in vivo. In addition ActA, like IL-3, directly stimulates early OCL differentiation, and each stimulates OCL via a RANKL-independent mechanism.
ActA synergizes with RANKL to enhance OCL fusion in murine systems (12, 13). It also enhances OCL formation by direct, local action on OCL precursors that promote OCL differentiation and activation of the IκBα/NFκB pathway (14). Our results demonstrate that ActA has a direct effect on osteoclastogenesis that is RANKL independent. In addition, ActA’s impact on OCL development is most significant during early osteoclastogenesis, similar to IL-3 (3), and consistent with our current data demonstrating that both IL-3 induced ActA production by CD14+ BMM and expression of the IL-3R on OCL precursors decrease during OCL differentiation. These results suggest that ActA may act as an autocrine or paracrine factor for OCL formation and that ActA is a rational target for reduction of the downstream, bone-specific effects of IL-3 on OCL stimulation in MMBD.
Acknowledgments
Dr. Giuliani has been funded by the Associazione Italiana per la Ricerca sul Cancro (A.I.R.C.) Special Program in Molecular Clinical Oncology.
The authors thank Dr. Khalid Mohammad for technical assistance with the BioQuant system, Dr. Keith Condon for histology services, and Dirce Gennari for technical support. This work was supported in part by grants from the N.I.H. and VA Merit Review Program (G.D.R.) as well as the Associazione Italiana per la Ricerca sul Cancro (A.I.R.C.) Special Program in Molecular Clinical Oncology (N.G.).
Footnotes
Authorship Contributions
Contribution: R.S. designed and performed most experiments and wrote the manuscript; M.B. performed cell culture experiments; P.S. performed gene expression profiling experiments and contributed to molecular biology procedures; D.G. performed ELISA assays; S.B. performed flow cytometry analysis; F.A. contributed to sample collections; D.Z. and J.L.A. assisted with tissue culture experiments and other in vitro studies; J.W. performed statistical analysis of the population data; J.J.W. provided mice and performed the in vivo studies; G.D.R. designed experiments and helped to write the manuscript; N.G. designed some of the in vitro and gene profiling experiments.
Conflict-of-Interest Statement: Dr. Roodman is a consultant for Amgen and receives research support from the NIH, the VA Merit Review Program, and Eli Lilly and Co
The other authors have no conflict-of-interest disclosures.
References
- 1.Roodman GD. Mechanisms of bone metastasis. The New England journal of medicine. 2004 Apr 15;350(16):1655–1664. doi: 10.1056/NEJMra030831. [DOI] [PubMed] [Google Scholar]
- 2.Giuliani N, Rizzoli V, Roodman GD. Multiple myeloma bone disease: Pathophysiology of osteoblast inhibition. Blood. 2006 Dec 15;108(13):3992–3996. doi: 10.1182/blood-2006-05-026112. [DOI] [PubMed] [Google Scholar]
- 3.Lee JW, Chung HY, Ehrlich LA, Jelinek DF, Callander NS, Roodman GD, et al. IL-3 expression by myeloma cells increases both osteoclast formation and growth of myeloma cells. Blood. 2004 Mar 15;103(6):2308–2315. doi: 10.1182/blood-2003-06-1992. [DOI] [PubMed] [Google Scholar]
- 4.Ehrlich LA, Chung HY, Ghobrial I, Choi SJ, Morandi F, Colla S, et al. IL-3 is a potential inhibitor of osteoblast differentiation in multiple myeloma. Blood. 2005 Aug 15;106(4):1407–1414. doi: 10.1182/blood-2005-03-1080. [DOI] [PubMed] [Google Scholar]
- 5.Storti P, Bolzoni M, Donofrio G, Airoldi I, Guasco D, Toscani D, et al. Hypoxia-inducible factor (HIF)-1alpha suppression in myeloma cells blocks tumoral growth in vivo inhibiting angiogenesis and bone destruction. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK. 2013 Aug;27(8):1697–1706. doi: 10.1038/leu.2013.24. [DOI] [PubMed] [Google Scholar]
- 6.Nicks KM, Perrien DS, Akel NS, Suva LJ, Gaddy D. Regulation of osteoblastogenesis and osteoclastogenesis by the other reproductive hormones, Activin and Inhibin. Molecular and cellular endocrinology. 2009 Oct 30;310(1–2):11–20. doi: 10.1016/j.mce.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terpos E, Kastritis E, Christoulas D, Gkotzamanidou M, Eleutherakis-Papaiakovou E, Kanellias N, et al. Circulating activin-A is elevated in patients with advanced multiple myeloma and correlates with extensive bone involvement and inferior survival; no alterations post-lenalidomide and dexamethasone therapy. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2012 Apr 6; doi: 10.1093/annonc/mds068. [DOI] [PubMed] [Google Scholar]
- 8.Vallet S, Mukherjee S, Vaghela N, Hideshima T, Fulciniti M, Pozzi S, et al. Activin A promotes multiple myeloma-induced osteolysis and is a promising target for myeloma bone disease. Proceedings of the National Academy of Sciences of the United States of America. 2010 Mar 16;107(11):5124–5129. doi: 10.1073/pnas.0911929107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearsall RS, Canalis E, Cornwall-Brady M, Underwood KW, Haigis B, Ucran J, et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proceedings of the National Academy of Sciences of the United States of America. 2008 May 13;105(19):7082–7087. doi: 10.1073/pnas.0711263105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lotinun S, Pearsall RS, Davies MV, Marvell TH, Monnell TE, Ucran J, et al. A soluble activin receptor Type IIA fusion protein (ACE-011) increases bone mass via a dual anabolic-antiresorptive effect in Cynomolgus monkeys. Bone. 2010 Apr;46(4):1082–1088. doi: 10.1016/j.bone.2010.01.370. [DOI] [PubMed] [Google Scholar]
- 11.Scullen T, Santo L, Vallet S, Fulciniti M, Eda H, Cirstea D, et al. Lenalidomide in combination with an activin A-neutralizing antibody: preclinical rationale for a novel anti-myeloma strategy. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK. 2013 Aug;27(8):1715–1721. doi: 10.1038/leu.2013.50. [DOI] [PubMed] [Google Scholar]
- 12.Fuller K, Bayley KE, Chambers TJ. Activin A is an essential cofactor for osteoclast induction. Biochemical and biophysical research communications. 2000 Feb 5;268(1):2–7. doi: 10.1006/bbrc.2000.2075. [DOI] [PubMed] [Google Scholar]
- 13.Gaddy-Kurten D, Coker JK, Abe E, Jilka RL, Manolagas SC. Inhibin suppresses and activin stimulates osteoblastogenesis and osteoclastogenesis in murine bone marrow cultures. Endocrinology. 2002 Jan;143(1):74–83. doi: 10.1210/endo.143.1.8580. [DOI] [PubMed] [Google Scholar]
- 14.Sakai R, Eto Y, Ohtsuka M, Hirafuji M, Shinoda H. Activin enhances osteoclast-like cell formation in vitro. Biochemical and biophysical research communications. 1993 Aug 31;195(1):39–46. doi: 10.1006/bbrc.1993.2006. [DOI] [PubMed] [Google Scholar]