Abstract
Background & Aims
The increasing incidence of microscopic colitis has been partly attributed to diagnostic detection bias. We aimed to ascertain recent incidence trends and the overall prevalence of microscopic colitis in a population-based study.
Methods
Using data from the Rochester Epidemiology Project, we identified residents of Olmsted County, Minnesota who were diagnosed with collagenous colitis or lymphocytic colitis from January 1, 2002 through December 31, 2010 based on biopsy results and the presence of diarrhea (n=182; mean age at diagnosis, 65.8 y; 76.4% female). Poisson regression analyses were performed to evaluate associations between incidence and age, sex, and calendar period.
Results
The age- and sex-adjusted incidence of microscopic colitis was 21.0 cases per 100,000 person-years (95% confidence interval [CI], 18.0–24.1 cases per 100,000 person-years). The incidence of lymphocytic colitis was 12.0 per 100,000 person-years (95% CI, 9.6–14.3 per 100,000 person-years) and collagenous colitis was 9.1 per 100,000 person-years (95% CI, 7.0–11.1 per 100,000 person-years). The incidence of microscopic colitis and its subtypes remained stable over the study period (p=.63). Increasing age (p<.001) and female sex (p<.001) were associated with increasing incidence. On December 31, 2010, the prevalence of microscopic colitis was 219 cases per 100,000 persons (90.4 per 100,000 persons for collagenous colitis and 128.6 per 100,000 persons for lymphocytic colitis).
Conclusion
The incidence of microscopic colitis in Olmsted County residents has stabilized and remains associated with female sex and increasing age.
Keywords: Microscopic Colitis, Epidemiology
INTRODUCTION
Microscopic colitis (MC) is a common cause of chronic diarrhea, especially in the elderly, and has two main subtypes, lymphocytic colitis (LC) and collagenous colitis (CC).1,2 In prior epidemiological studies from Europe and North America, the incidence of CC ranged from <1 – 7 cases per 100,000 person-years, and the incidence of LC ranged from 3–16 per 100,000.2–8 In a North American study of Olmsted County residents between 1985 and 2001, there was a significant increase in the incidence of MC and both subtypes over the study period, as well as a higher prevalence than had been reported previously, 103.0 per 100,000 persons overall for MC (39.3 for collagenous colitis and 63.7 for lymphocytic colitis).2 Other studies have shown variable temporal trends, with some demonstrating an increase in the incidence of CC 3 or LC 4 over time, while another demonstrated stability in the incidence of CC.9
We performed an epidemiological study of microscopic colitis and its subtypes in a population-based cohort of Olmsted County residents from 2002 to 2010 to assess temporal trends in incidence and determine overall prevalence of microscopic colitis.
METHODS
Study Setting
Olmsted County, located in southeastern Minnesota, had a population of 144,248 at the time of the 2010 census. This figure represents an increase of 16.1% from the 2000 population (124,000) reported in our prior study.1,2 At the time of the 2010 census, 12.6% of county residents were over 65 years of age and 51.1% were female, which is comparable to the US population.10 The city of Rochester is the main urban center of Olmsted County. While residents of Olmsted County are socioeconomically similar to the general US population, there are some differences, including ethnic diversity (86% of the county population is Caucasian compared to 72% of the US population) and education (39% have completed a bachelor’s degree or higher compared to 28% of the US population).10 Moreover, 25% of Olmsted County residents are employed in health care versus 8% nationwide.10
Rochester Epidemiology Project
The Rochester Epidemiology Project (REP) is a valuable data resource that exploits the fact that the vast majority of health care for the residents of Olmsted County is provided by Mayo Medical Center and Olmsted Medical Center.11–13 The REP serves as a centralized diagnostic index that links records from all outpatient and emergency room visits, hospitalizations, nursing home stays, surgical procedures, autopsy examinations, and death certificates for all county residents since 1908.11,12 All medical records, from all sources of care available to Olmsted County residents, are linked and accessible through the REP, including drug prescriptions. The REP therefore allows investigators to follow subjects through their outpatient and hospitalization contacts across all local medical facilities, regardless of where the care was delivered and of insurance status, and to conduct long-term population-based studies of disease incidence, prevalence, and outcomes.12–14
Ascertainment of Microscopic colitis cases
The Institutional Review Boards of both Olmsted Medical Center and Mayo Clinic approved this study. All Olmsted County residents diagnosed with MC (CC or LC) from January 1, 2002 to December 31, 2010 were identified by either the diagnostic index of the Rochester Epidemiology Project or the Department of Pathology database, using ICD-9 code 558.9, and HICDA-8 (Hospital International Classification of Diseases Adapted) codes 561 and 563.9, similar to the search strategy used for our prior epidemiological study.2
All participants in this study were Olmsted County residents, 18 years old or older, with a biopsy consistent with microscopic colitis and diarrhea at the time of investigation. Patients were excluded if they had a history of inflammatory bowel disease, an alternative explanation for their diarrhea, such as infectious etiologies or ischemic colitis, no diarrhea at the time of investigation, or if their colon biopsies did not meet the criteria for LC or CC.
Once participants were identified, permission for research access to their medical records was verified and both inpatient and outpatient medical records were reviewed. Six cases whose biopsies were perceived as questionable were reviewed by an expert gastrointestinal pathologist (TCS) to confirm the diagnosis according to standard criteria: CC had preserved crypt architecture, increased intraepithelial lymphocytes (>20 lymphocytes per 100 epithelial cells) with a mixed lamina propria inflammatory infiltrate and a subepithelial collagen band at least 10 um thick, while patients with LC had similar inflammatory changes without a thickened collagen band.2 Of these 6 cases, one initially was read as suggestive of MC but on repeat was deemed normal. The remaining 5 were confirmed as being consistent with MC.
Statistical analysis
For the purpose of calculating incidence rates, it was assumed that the entire county population over the age of 18 was at risk. Confirmed cases of microscopic colitis were included in the numerator, and denominator age- and gender-adjusted person-years were estimated from decennial census data with interpolation between census years. Standard errors and 95% confidence intervals (95% CI) were calculated for the incidence rates assuming a Poisson distribution. Prevalence was calculated using all patients with a diagnosis of microscopic colitis residing in Olmsted County on December 31, 2010 as the numerator and the estimated county population on this date as the denominator. Prevalent cases residing in Olmsted County who were diagnosed before becoming county residents (i.e., non-incident prevalent cases), and those who were diagnosed in Olmsted County prior to 2001, were included in the prevalence calculation but not the incidence calculation. Incidence and prevalence rates were directly age- or age- and gender-adjusted to the population structure of white persons in the US in 2010.
Poisson regression was used to assess the association of age, gender and calendar period with the incidence rates categorizing calendar period as 2002–2004, 2005–2007, and 2008–2010. Both age and calendar period were considered continuous predictors in this analysis. These analyses were repeated separately for lymphocytic colitis and collagenous colitis. All analyses were carried out using SAS® software version 9.2 (SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
Initially, 228 potential cases were identified based on diagnostic codes; 46 were subsequently excluded: 5 were diagnosed prior to the defined study period, 4 had no diarrhea at diagnosis, 24 had biopsy reports that stated no evidence for microscopic colitis, 3 had a history of inflammatory bowel disease, and 10 had an alternate etiology for their diarrhea (3 C. difficile infection, 2 small intestinal bacterial overgrowth, 1 spirochetosis, 1 ischemic colitis, 1 with diarrhea secondary to chemotherapy, 1 melanosis coli from laxative abuse, and 1 radiation colitis).
Of the 182 patients included, the median age at diagnosis was 65.8 years (range, 22.8–92.1) and 139 (76.4%) were female. By colitis subtype, 104 had LC and 78 had CC. Smoking history was similar between colitis subtypes (18.3% of LC and 20.5% of CC were current smokers; 30.8% of LC and 35.9% of CC were former smokers, and 51.0% of LC and 43.6% of CC were never smokers). A personal history of colorectal cancer following the diagnosis of MC was reported in 2 patients, one with CC approximately 5 years following CC diagnosis and one with LC approximately 6 years after diagnosis with LC (1.1%). A history of colon cancer in a first degree relative was present in 26/182 (14.3%).
Celiac disease was present in 5 patients (2.7%). Other noted autoimmune conditions include 1 patient with psoriasis, 2 with sarcoidosis, 2 with Grave’s disease, 4 with lymphocytic thyroiditis, 6 with multiple sclerosis, and 15 with rheumatoid arthritis.
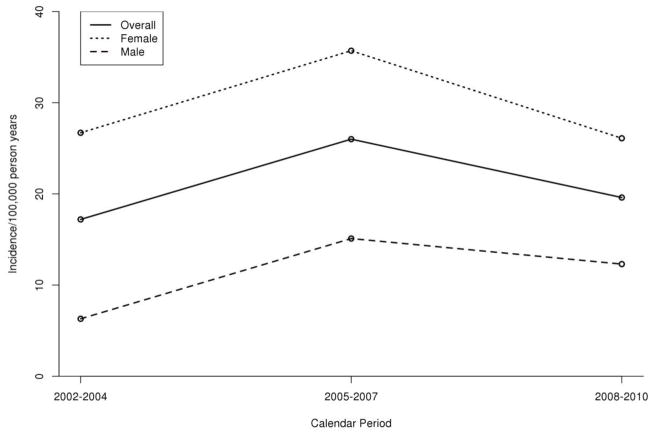
The age- and gender-adjusted incidence of MC overall was 21.0 cases per 100,000 person-years (95% CI, 18.0 – 24.1). Incidence was associated with increasing age (p<0.001) and female gender (p<0.001) but not study period (2002–2004, 17.2 cases per 100,000 person-years; 2005–2007, 26.0 per 100,000; 2008–2010, 19.6 per 100,000; p = 0.63) (Figure 1).
Figure 1.
Incidence of Microscopic colitis over time in residents of Olmsted County, Minnesota, 2002–2010
Changes in incidence over time were not significant (P=0.63)
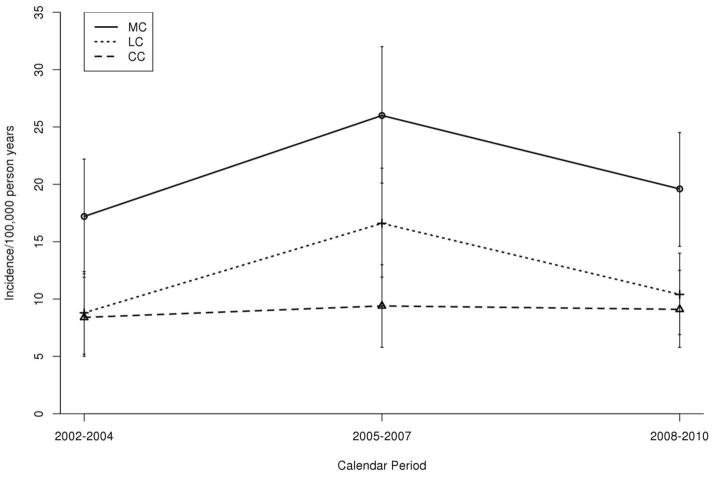
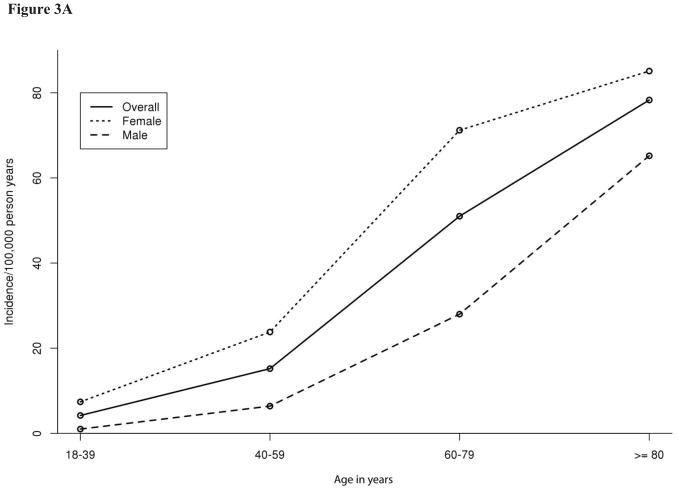
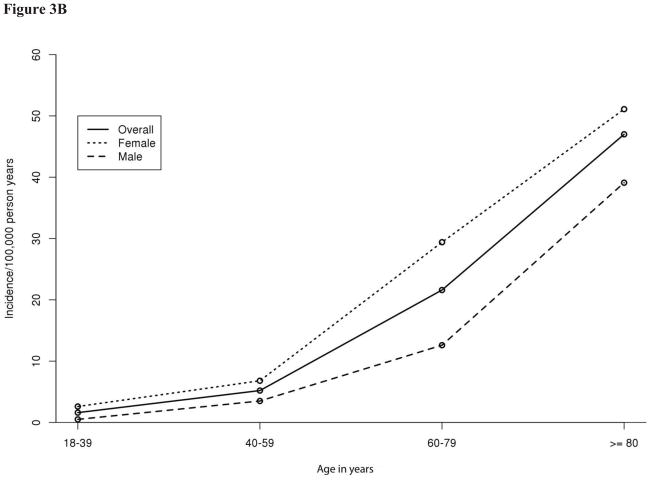
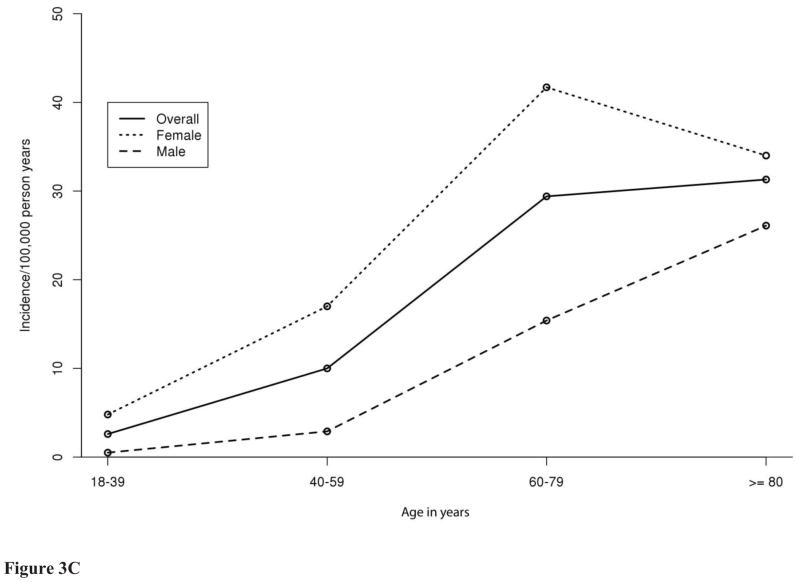
The overall age- and gender-adjusted incidence of each colitis subtype was similar: 12.0 per 100,000 person-years (95% CI, 9.6 – 14.3) for LC and 9.1 per 100,000 person-years (95% CI, 7.0–11.1) for CC (Figure 2). The incidence of LC (p<0.001) and CC (p=0.006) was associated with female gender and with increasing age (both p<0.001). The incidence of MC overall and its subtypes increased with age (Figure 3).
Figure 2.
Age- and gender-adjusted incidence of Microscopic colitis and subtypes over time in residents of Olmsted County, Minnesota, 2002–2010
Figure 3.
Age and gender specific incidence of Microscopic colitis (A), collagenous colitis (B), and lymphocytic colitis (C) among Olmsted County, Minnesota
On December 31, 2010, 234 residents of Olmsted County were alive with a diagnosis of MC. The prevalence of MC was 219.0 cases per 100,000 residents (95% CI, 190.0–247.1) with an overall prevalence in men of 103.4 (95% CI, 74.9–132.0) and an overall prevalence in women of 322.0 (95% CI, 275.2–368.8). The prevalence of LC was 90.4 per 100,000 (95% CI, 72.3–108.5), and of CC was 128.6 per 100,000 (95% CI, 107.1–150.1).
On December 31, 2010, in the age group 18–44, there were 27 cases of MC (24 female, 3 male) with a prevalence of 50.3 per 100,000 (90.1/100,000 female and 11.1/100,000 male). In the age group 45–65, there were 62 cases (47 female, 15 male) with a prevalence of 156.7 per 100,000 (232.5/100,000 female and 77.5/100,000 male). In the age group 65 and older, there were 76 cases of MC (55 female, 21 male) with a prevalence of 440.1 per 100,000 (557.4/100,000 female and 283.7/100,000 male).
DISCUSSION
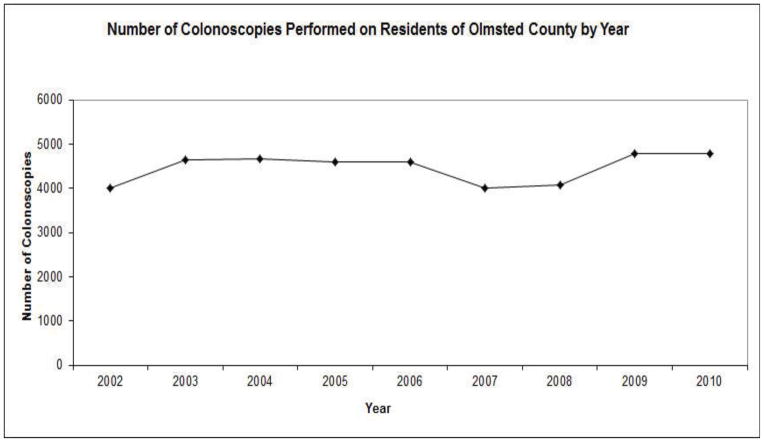
Although the incidence of MC and its subtypes increased significantly in Olmsted County residents from 1985–20012, it stabilized between 2002 and 2010. The prevalence of MC on December 31, 2010 was higher than we reported in our prior study (219.0 vs. 103.0 cases per 100,000 residents).2 This prevalence is higher compared to another study from Spain from April 2008 to December 2010, which reported the prevalence to be 48/100,000.8 The previously noted increase in incidence was partly attributed to increasing utilization of colonoscopy and biopsy, leading to diagnostic detection bias.2 It is likely that, over the latter part of that study and continuing into the current study, physician awareness of MC as a relatively common cause of chronic watery diarrhea stabilized, thus eliminating detection bias that may have contributed to the prior increase in incidence. Indeed, the average numbers of colonoscopy procedures performed in Olmsted County residents was relatively stable over the study period from 2002–2004 (Figure 4).
Figure 4.
Number of colonoscopies performed on residents of Olmsted County by year
An epidemiologic study from southern Sweden also demonstrated stabilization in the incidence of CC between 2001 and 2010, which was attributed to high physician awareness of MC for many years, and regular use of colonoscopy and biopsy to evaluate patients with chronic diarrhea.9 Another population based study conducted in Örebro, Sweden from 1999–2008 also demonstrated the stabilization of incidence in both CC and LC, with an overall prevalence of MC of 123 per 100,000 on December 31, 2008.15
In residents of Olmsted County, the incidence of MC is approaching that of inflammatory bowel disease (IBD). From 2001–2004, the incidence of Crohn’s disease was 12.9/100,000 person years (95% CI 9.7–16.1) and for ulcerative colitis it was 12.5/100,000 person years (95% CI 9.4–15.6). On January 1, 2005 the prevalence of Crohn’s disease was 222 per 100,000 (95% CI, 197–247) and for ulcerative colitis, it was 273 per 100,000 (95% CI, 245–300).16
The incidence of MC continues to be associated with female gender. Although the prior Olmsted County study demonstrated an association of CC but not LC with female gender2, in the present study both types were associated with gender. Some prior studies also demonstrated an association with female gender and the incidence of both LC and CC6, while others demonstrated an association only in CC.2,4,5 This is in contrast to other studies that found either no gender association8 or that the female association is decreasing.9 The explanation for the association with female gender reported in most studies is likely multifactorial, including possible hormonal contributions, the increased likelihood of women developing autoimmune processes, and greater likelihood of females presenting to a physician to investigate chronic diarrhea.3,6
The incidence of MC also continues to be associated with older age, as demonstrated in multiple prior studies.2–4,17,18 Although the elderly population takes more medications and is therefore more susceptible to developing drug-induced MC,19 and clinicians may be more likely to perform a colonoscopy on an elderly individual with diarrhea,6 the striking association between age and incidence suggests a true underlying biologic phenomenon. For example, a recent analysis of nearly 800,000 colon pathology reports, which included over 8,000 patients with MC, demonstrated that the prevalence of MC was significantly higher in patients between the ages of 60–80 compared to those younger than 60 (p<0.0001).20
Similar to some prior studies, we demonstrated that the incidence of LC is higher than that of CC,2,5,6 although other studies have demonstrated a higher incidence of CC3 or no significant difference in incidence by subtype.4,6,7 The explanation for differences in incidence by subtype, or for the disparate findings in these various studies, is not clear and warrants further investigation.
In conclusion, this population-based cohort study demonstrates that the incidence of microscopic colitis in Olmsted County residents stabilized from 2002–2010, after a significant rise from 1985–2001.
Footnotes
Nicole M. Gentile: No conflict of interest to disclose.
Sahil Khanna: No conflict of interest to disclose
Edward V. Loftus, Jr: No conflict of interest to disclose
Thomas C. Smyrk: No conflict of interest to disclose
William J. Tremaine: No conflict of interest to disclose
W. Scott Harmsen: No conflict of interest to disclose
Alan R. Zinsmeister: No conflict of interest to disclose
Patricia P. Kammer: No conflict of interest to disclose
Darrell S. Pardi: No conflict of interest to disclose
Prior presentation:
Presented in part at Digestive Disease Week 2012 in San Diego, CA, and published in abstract form (Gastroenterology 2012;142(5) (Suppl 1):S-571).
Disclosures: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01 AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contributions:
Nicole M. Gentile: Study concept, design, data collection, data interpretation, manuscript drafting, and revision, review of final manuscript
Sahil Khanna: Study concept, design, data collection, data interpretation, manuscript drafting, and revision, review of final manuscript
Edward V. Loftus, Jr: Study concept, design, data interpretation, manuscript revision, review of final manuscript
Thomas C. Smyrk: Study concept, design, review of pathology slides, data interpretation, manuscript revision, review of final manuscript
William J. Tremaine: Study concept, design, data interpretation, manuscript revision, review of final manuscript
W. Scott Harmsen: Study concept, design, statistical analysis, data interpretation, manuscript revision, review of final manuscript
Alan R. Zinsmeister: Study concept, design, statistical analysis, data interpretation, manuscript revision, review of final manuscript
Patricia P. Kammer: administrative support, study concept, design, manuscript drafting, review of final manuscript
Darrell S. Pardi: Study supervision, study concept, design, data analysis and, interpretation, manuscript drafting, and revision, review of final manuscript
Disclosures: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01 AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
All authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pardi DS, Kelly CP. Microscopic colitis. Gastroenterology. 2011;140:1155–1165. doi: 10.1053/j.gastro.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Pardi DS, Loftus EV, Jr, Smyrk TC, et al. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Gut. 2007;56:504–508. doi: 10.1136/gut.2006.105890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agnarsdottir M, Gunnlaugsson O, Orvar KB, et al. Collagenous and lymphocytic colitis in Iceland. Digestive diseases and sciences. 2002;47:1122–1128. doi: 10.1023/a:1015058611858. [DOI] [PubMed] [Google Scholar]
- 4.Olesen M, Eriksson S, Bohr J, Jarnerot G, Tysk C. Microscopic colitis: a common diarrhoeal disease. An epidemiological study in Orebro, Sweden, 1993–1998. Gut. 2004;53:346–350. doi: 10.1136/gut.2003.014431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez-Banares F, Salas A, Forne M, Esteve M, Espinos J, Viver JM. Incidence of collagenous and lymphocytic colitis: a 5-year population-based study. The American journal of gastroenterology. 1999;94:418–423. doi: 10.1111/j.1572-0241.1999.00870.x. [DOI] [PubMed] [Google Scholar]
- 6.Williams JJ, Kaplan GG, Makhija S, et al. Microscopic colitis-defining incidence rates and risk factors: a population-based study. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2008;6:35–40. doi: 10.1016/j.cgh.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Banares F, Salas A, Esteve M, et al. Evolution of the incidence of collagenous colitis and lymphocytic colitis in Terrassa, Spain: a population-based study. Inflammatory bowel diseases. 2011;17:1015–1020. doi: 10.1002/ibd.21438. [DOI] [PubMed] [Google Scholar]
- 8.Guagnozzi D, Lucendo AJ, Angueira-Lapena T, Gonzalez-Castillo S, Tenias Burillo JM. Prevalence and incidence of microscopic colitis in patients with diarrhoea of unknown aetiology in a region in central Spain. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. 2012;44:384–388. doi: 10.1016/j.dld.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Vigren L, Olesen M, Benoni C, Sjoberg K. An epidemiological study of collagenous colitis in southern Sweden from 2001–2010. World journal of gastroenterology : WJG. 2012;18:2821–2826. doi: 10.3748/wjg.v18.i22.2821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howden LMaJM. Commerce Do, editor. Age and Sex Composition: 2010 Census Briefs. Washington, DC: U.S. Department of Commerce Economics and Statistics Administraton US Census Bureau; May, 2011. [Google Scholar]
- 11.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. American journal of epidemiology. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clinic proceedings. Mayo Clinic. 2012;87:1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. International journal of epidemiology. 2012;41:1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clinic proceedings. Mayo Clinic. 2012;87:151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wickbom A, Bohr J, Eriksson S, Udumyan R, Nyhlin N, Tysk C. Stable Incidence of Collagenous Colitis and Lymphocytic Colitis in Orebro, Sweden, 1999–2008: A Continuous Epidemiologic Study. Inflamm Bow Dis. 2013 Aug 13; doi: 10.1097/MIB.0b013e31829ed8cd. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Ingle SB, Loftus EV, Tremaine WJ, Harmsen WS, Zinsmeister AR, Melton LJ, Sandborn WJ. Increasing incidence and prevalence of inflammatory bowel disease in Olmsted County, Minnesota, 2001–2004. Gastroenterology. 2007;132(4 Suppl 2):A19–20. [Google Scholar]
- 17.Wickbom A, Lindqvist M, Bohr J, et al. Colonic mucosal tears in collagenous colitis. Scandinavian journal of gastroenterology. 2006;41:726–729. doi: 10.1080/00365520500453473. [DOI] [PubMed] [Google Scholar]
- 18.Olesen M, Eriksson S, Bohr J, Jarnerot G, Tysk C. Lymphocytic colitis: a retrospective clinical study of 199 Swedish patients. Gut. 2004;53:536–541. doi: 10.1136/gut.2003.023440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beaugerie L, Pardi DS. Review article: drug-induced microscopic colitis - proposal for a scoring system and review of the literature. Aliment Pharmacol Ther. 2005;22:277–284. doi: 10.1111/j.1365-2036.2005.02561.x. [DOI] [PubMed] [Google Scholar]
- 20.Sonnenberg A, Genta RM. Lymphocytic and Collagenous Colitis: Epidemiologic Differences and Similarities. Dig Dis Sci. 2013 May 26; doi: 10.1007/s10620-013-2718-6. Epub ahead of print. [DOI] [PubMed] [Google Scholar]