Abstract
Objectives
To explore the effect of aging on cardiac toxicity specifically the interaction of age and antipsychotic drugs to alter the QT interval.
Methods
The Medline databases were searched using the OvidSP platforms with the search strategy: “QT interval” or “QT” and “age” or “aging”. The entry criteria were: over 10,000 apparently healthy individuals with data on both sexes; QT interval corrected for heart rate (QTc) and an expression of its variance for multiple age decades extending into the older ages.
Results
QTc increased in duration with increasing age. Considering a modest one SD increment in QTc in the normal population, the addition of Chlorpromazine produced a QTc on average greater than 450 ms for ages 70 years and older. Risperidone, that did not on average alter QTc, would be expected to produce a QTc of 450 ms in persons in their mid 70 years under some circumstances. QTc prolongation > 500 ms with antipsychotic drugs is more likely for persons with QTc initially at the 99th percentile. It may occur with Haloperidol which does not on average alter QTc.
Conclusions
The range of values for the QT interval in apparently normal older men or women, when combined with the range of expected QT interval changes induced by antipsychotic drugs, can readily be associated with prolonged QTc. Individuals with QTc at the 99th percentile may have serious QTc prolongation with antipsychotic drugs even those that are not usually associated with QTc prolongation.
Keywords: Cardiac safety, Antipsychotic drugs, Psychotropic drugs, QT interval, Aging
1. Introduction
Cardiac safety has attracted considerable attention because of the imperative to minimize or avoid drug-induced adverse effects on the heart at a drug's therapeutic dosages. The use of any drug needs to take into account its safety along with the expected benefit of treatment weighed against the alternatives. The potential of cardiac toxicity is unacceptable in healthy individuals using medication for a benign transient condition. On the other side of the spectrum is the situation in which the risk of a cardiac toxicity can be offset by the risk of not treating a patient with a serious condition which has a significantly increased risk of death or is associated with serious morbidity. A degree of cardiac toxicity may be tolerable when it restores a person with a debilitating psychiatric illness to normal functioning and reduces suicide risk. This concept underlies the use of antipsychotic drugs some of which have the potential to induce serious cardiac arrhythmias.[1]
Research efforts have focused on identifying drugs with a high probability of producing cardiac toxicity and identifying factors that predict or modulate the development of cardiac toxicity. Findings on the 12 lead ECG have been useful for sudden death prediction.[2] One frequently used identifier of an increased risk of a fatal cardiac arrhythmia is an increase in the QT interval on the standard ECG.[3]–[5] Although there are differences of opinion on the extent to which alterations in the QT interval can predict the development of potentially fatal cardiac arrhythmias, there is a compelling argument that the greater the drug-induced prolongation of QT duration, the more likely is the occurrence of serious ventricular arrhythmias such as torsade de pointes.[6]–[9]
The complexity of integrating the multiple factors that influence cardiac safety into the development of drug-induced cardiac toxicity risk prediction models,[10] has perhaps lead to less consideration of the role of aging or considerations of person's age in cardiac toxicity. Aging has well known and documented effects on drug pharmacokinetics and drug metabolism.[11] The question of the impact of aging on the QT interval and cardiac safety, however, has not been the subject of a much discussion. The objective of this study is to explore the effect of aging on the QT interval and specifically to illustrate the potential of antipsychotic drugs to compound the risks for alteration of the QT interval.
2. Methods
2.1. Search strategy
A systematic search was conducted to identify studies that examined the relationship between QT interval and aging. The Medline databases were searched using the OvidSP platforms. The full electronic search strategy was “QT interval” or” QT” and “age” or “aging”. The search was limited to humans and English language. The last date of search was January 30, 2014.
The inclusion criteria were (1) an original study, (2) over 5,000 persons in the study, (3) data on both sexes, (4) presentation of the measured QT interval corrected for heart rate, (5) presentation of mean data for measured QT interval plus an expression of its variance for multiple age decades extending into the older age groups, (6) apparently healthy individuals, and (7) at least 200 individuals over the age of 65 years.
A second search was conducted to identify a study from randomized control trials in adults that reported the effect of antipsychotic drugs on the QT interval and included an estimate of variance. The objective was to utilize the data from this study in conjunction with the age related QT data to assess the potential for age to impact the effect of antipsychotic drugs.
2.2. Data analysis
In order to combine data, the means of different groups were summed. In order to combine standard deviations, the square root of the sum of the standard deviations squared was used. The mean data for each calculation are displayed.
3. Results
Two studies were identified that fulfilled the entry criteria for QT studies.[12],[13] Several large studies were not included because they did not present an estimate of QT interval variance for age decades,[14] corrected QT for heart rate,[15] or did not include data extending into older ages.[16],[17]
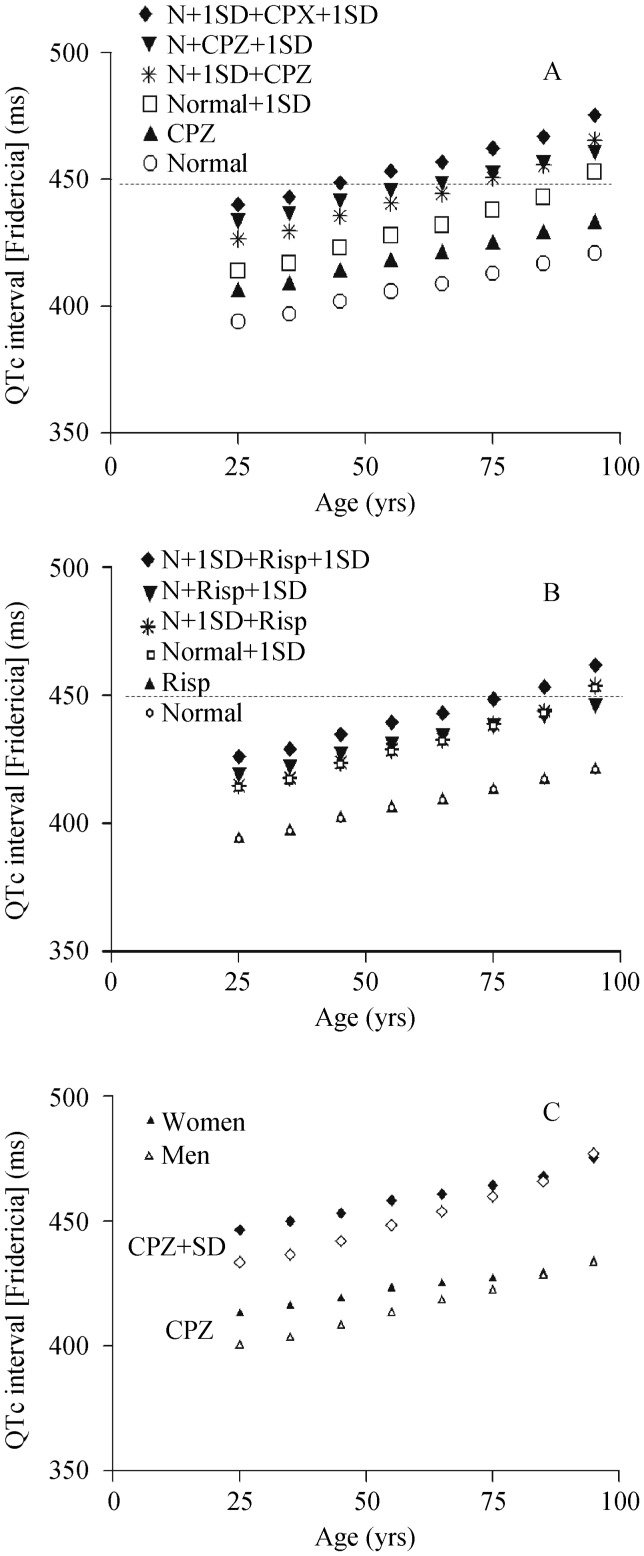
QTc shows a gradual increase in duration with increasing age in the largest data base, about 45,000 apparently healthy persons, of ECG intervals in apparently healthy individuals (Figure 1A).[12] The addition of data on the effect of Chlorpromazine (CPZ),[18] by combination of the means, showed a meaningful increase in QTc. Considering a modest one SD increment in QTc in the normal population, the addition of Chlorpromazine results in a QTc on average greater than 450 ms in persons mid 70 years of age and older. The 450 ms value is highlighted because it is the mid point between the recommended definition of an abnormal QTc for men and women.[19] Similar results are evident for individuals with normal QTc who respond to CPZ at a modestly greater QTc prolongation of one SD more. Individuals with slightly longer QTc (one SD greater than the mean), who respond to CPZ-induced QTc prolongation of 1SD greater than the mean, show a QTc of 450 ms before age 50 years and the QTc is more prolonged at older ages.
Figure 1. The QT interval adjusted for heart rate by Fridericia method, according to age [12].
The mid point of each decade was used for graphical presentation. (A): The QTc that would be anticipated if the average QTc prolongation with CPZ treatment is added to the mean, mean plus one SD of normal group, or mean plus CPZ plus one SD of CPZ group or the normal group one SD plus CPZ group plus one SD; (B): The QTc that would be anticipated if the average QTc prolongation with Risp treatment is added to the mean, mean plus one SD of normal group, or mean plus Risp plus one SD of Risp group or the normal group one SD plus Risp group plus one SD; (C): The QTc that would be anticipated if the average QTc prolongation with CPZ treatment is added to the mean or mean plus CPZ plus one SD of CPZ group for men and women. CPZ: Chlorpromazine; Risp: Risperidone.
For comparison, an agent, such as Risperidone, that did not alter QTc in a study of almost 400 individuals,[18] produced little effect in this kind of analysis (Figure 1B). However, the trend of increasing QTc with age produced QTc of 450 ms in persons in their mid 70 years when they began with a QTc only 1 SD greater than the mean and had a response to Risperidone which was 1 SD greater than the average response to Risperidone.
Women in general have a longer QTc than men.[12] Women who receive CPZ have a longer QTc than men (Figure 1C). QTc increases with age more in men than women so the differentially larger QTc in women decreases with increasing age.
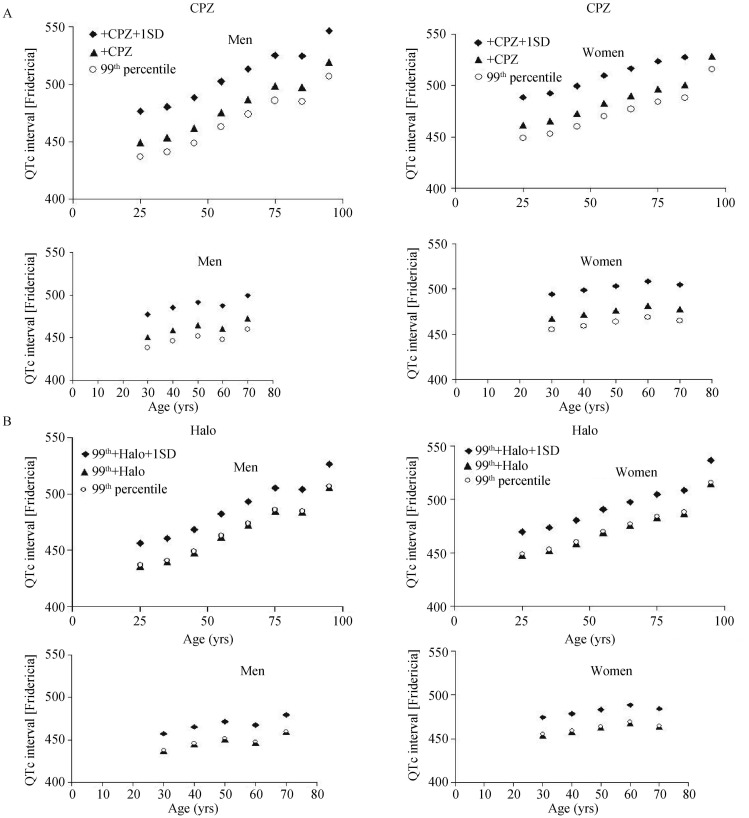
Prolonged QTc has been considered to be a relative contraindication to the use of antipsychotic agents. To explore the implications of this concept, the 99th percentile for QTc at different ages was compared in the two data bases. The 99th percentile for QTc increases with age in both data sets.[12],[13] CPZ produces an incremental increase in QTc which becomes more prominent with increasing age (Figure 2A). The absolute magnitude of the QTc approaches 500 ms in men in their late 60s for those whose response to CPZ is one SD greater than the mean response. Men over, 70 years of age show a persistent increase in QTc with age. Women who receive CPZ and whose pretreatment QTc is in the 99th percentile attained a QTc of 500 ms by age 50 years if response to CPZ is one SD greater than the mean response. Women over 50 years of age show a persistent increase in QTc with increasing age.
Figure 2. The 99th percentile of the QT interval for men and women adjusted for heart rate by Fridericia method, according to age using the mid point of each decade, was used for graphical presentation according to the data of Mason et al.[12] upper panel and Dmitrienko et al.[13] lower panel.
(A): The data are presented for the 99th percentile plus the mean change in QTc for CPZ as well as the change in QTc plus 1 SD with CPZ; (B): The data are presented for the 99th percentile plus the mean change in QTc for Halo as well as the change in QTc plus 1 SD with Halo. CPZ: Chlorpromazine; Halo: Haloperidol.
The impact of age is evident for agents that do not on average increase QTc such as Haloperidol, which was evaluated in over 1,000 individuals.[18] QTc approaches 500 ms in men in their late 60s for those whose response to Haloperidol is one SD greater than the mean response (Figure 2B). This effect is somewhat more apparent in one data base[12] than the other.[13] The impact of Haloperidol on QTc was evident in women as well as men (Figure 2B).
4. Discussion
The important contribution of this study is the illustration that the range of values for the QT interval in apparently normal older individuals, when combined with the range of expected QT interval changes induced by antipsychotic drugs, can readily be associated with prolonged QT intervals in the range that can be considered serious. Furthermore, QTc in the range that may be seriously abnormal may be produced by agents that are not usually associated with QTc prolongation because of the pretreatment longer QTc in apparently healthy older persons. These findings were noted in both men and women.
The large studies examined herein, consisting of about 56,000 individuals, and both demonstrated an increased QT interval with increasing age.[12],[13] The relationship between age and QT interval appears to have a steeper slope at older ages. This translates into a much longer QT with increasing age especially at 70 years of age and older. The increase in QTc with age evaluated in the present study is supported by a number of small studies,[16],[20],[21] although there are some exceptions.[22],[23]
Cardiac safety of various drugs is compromised in older individuals. This represents a complex interaction of factors including altered drug pharmacokinetics and metabolism in aging, the development of clinical or occult cardiovascular disease, and probably the molecular biology of aging as it related to cardiac toxicity.[11],[24] The present study provides illustrative evidence that the increased QT interval with aging is another factor to consider in explaining the reduction in cardiac safety with drugs that prolong the QTc in older individuals.
Several QTc cutoff points were used to illustrate the effect of age and anti-psychotic drugs. A QTc of 450 ms was selected to illustrate the effects of aging and antipsychotic drugs on QTc. This value was selected because it is the mid point between the recommended definition of an abnormal QTc for men and women.[19] A QTc of 500 ms has frequently been used as a cutoff because these longer QTc interval measurements are associated with substantially higher risk especially with the use of anti-psychotic drugs.[8] Although other factors can also influence the risk, the greater the QT duration, the greater is the likelihood of potentially fatal arrhythmias such as torsade de pointes.[6]–[9]
Sex differences in the QT interval may explain in part the greater incidence of fatal cardiac arrhythmias in women on antipsychotic drugs compared to men.[25] QTc is usually greater in most women than men. QTc is not likely the only factor as the difference between men and women is reduced in the older age groups. This observation has been noted previously.[19]
Several limitations of this study should be kept in mind. First, this study was not designed to be a detailed evaluation of the effect of antipsychotic drugs on QT interval. Rather the study focused on QT interval and used the effect of anti-psychotic drugs as an example of how agents might interact with the QT interval at different person's ages. Second the study is conceptual in format and should not necessarily be used as an indicator of the action of all antipsychotic drugs. Third, one data source with antipsychotic drugs was used.[18] These data included studies with same kinds of protocols and ECG analysis. The effect of the antipsychotic drugs on QT interval summarized in that study,[18] was similar to randomized evaluation of six different agents in the same patient population.[26] Fourth, the measurement of QT is not without its technical challenges and the QT interval is not simply a reflection only of repolarization. Both of the issues with measurement and interpretation of the QT interval have been addressed in reviews and discussions.[8],[15],[27] Fifth, mechanisms responsible for each of the components of the QT interval[28] might be affected by the processes involved with aging and drugs that reduce cardiac safety. Sixth, the method used for the QT correction for heart rate was the Fridericia formula. While concerns have been raised about the accuracy of this formula for QT correction,[29] comparison of 10 mathematically different QT prediction formulae in 881 middle-aged men found that the Fridericia's formula fit the data better than most other formulae.[30] In a large data sets of over 10,000 normal ECGs the Fridericia was similar to Framingham, and Hodges formulae.[31] Thus, the Fridericia adjustment for the effect of heart rate on QT interval is an acceptable approach to QT interval correction for heart rate.
In summary, the values for the QT interval in apparently normal older men and women when combined with the range of expected QT interval changes induced by antipsychotic drugs can be associated with prolonged QT intervals in the range that can be considered serious. Furthermore, QTc in the range that may be seriously abnormal may be produced by agents that are not usually associated with QTc prolongation because of the pretreatment longer QTc in apparently healthy older persons. Antipsychotic medications are disproportionately used among elderly persons especially in persons over age 80 years and among subjects living in institutions.[32] This study highlights the potential problems with the use of antipsychotic medications and other drugs which prolong QT interval when used in older individuals.
References
- 1.Ray WA, Chung CP, Murray KT, et al. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360:225–235. doi: 10.1056/NEJMoa0806994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rabkin SW. Electrocardiographic abnormalities in apparently healthy men and the risk of sudden death. Drugs. 1984;28:28–45. doi: 10.2165/00003495-198400281-00004. [DOI] [PubMed] [Google Scholar]
- 3.Elming H, Holm E, Jun L, et al. The prognostic value of the QT interval and QT interval dispersion in all-cause and cardiac mortality and morbidity in a population of Danish citizens. Eur Heart J. 1998;19:1391–1400. doi: 10.1053/euhj.1998.1094. [DOI] [PubMed] [Google Scholar]
- 4.Noseworthy PA, Peloso GM, Hwang SJ, et al. QT interval and long-term mortality risk in the Framingham Heart Study. Ann Noninvasive Electrocardiol. 2012;17:340–348. doi: 10.1111/j.1542-474X.2012.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okin PM, Devereux RB, Howard B V, et al. Assessment of QT interval and QT dispersion for prediction of all-cause and cardiovascular mortality in American Indians: The Strong Heart Study. Circulation. 2000;101:61–66. doi: 10.1161/01.cir.101.1.61. [DOI] [PubMed] [Google Scholar]
- 6.Moss AJ. Measurement of the QT interval and the risk associated with QTc interval prolongation: a review. Am J Cardiol. 1993;72:23B–25B. doi: 10.1016/0002-9149(93)90036-c. [DOI] [PubMed] [Google Scholar]
- 7.Joy JP, Coulter C V, Duffull SB, et al. Prediction of torsade de pointes from the QT interval: analysis of a case series of amisulpride overdoses. Clin Pharmacol Ther. 2011;90:243–245. doi: 10.1038/clpt.2011.107. [DOI] [PubMed] [Google Scholar]
- 8.Glassman AH, Bigger JT., Jr Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry. 2001;158:1774–1782. doi: 10.1176/appi.ajp.158.11.1774. [DOI] [PubMed] [Google Scholar]
- 9.Roden DM. Keep the QT interval: it is a reliable predictor of ventricular arrhythmias. Hear Rhythm. 2008;5:1213–1215. doi: 10.1016/j.hrthm.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bai JP, Fontana RJ, Price ND, et al. Systems pharmacology modeling: an approach to improving drug safety. Biopharm Drug Dispos. 2014;35:1–14. doi: 10.1002/bdd.1871. [DOI] [PubMed] [Google Scholar]
- 11.Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57:6–14. doi: 10.1046/j.1365-2125.2003.02007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mason JW, Ramseth DJ, Chanter DO, et al. Electrocardiographic reference ranges derived from 79,743 ambulatory subjects. J Electrocardiol. 2007;40:228–234. doi: 10.1016/j.jelectrocard.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Dmitrienko AA, Sides GD, Winters KJ, et al. Electrocardiogram reference ranges derived from a standardized clinical trial population. Drug Inf J. 2005;39:395–405. [Google Scholar]
- 14.Bachman S, Sparrow D, Smith LK. Effect of aging on the electrocardiogram. Am J Cardiol. 1981;48:513–516. doi: 10.1016/0002-9149(81)90081-3. [DOI] [PubMed] [Google Scholar]
- 15.Rautaharju PM, Zhou SH, Wong S, et al. Sex differences in the evolution of the electrocardiographic QT interval with age. Can J Cardiol. 1992;8:690–695. [PubMed] [Google Scholar]
- 16.Macfarlane PW, McLaughlin SC, Devine B, et al. Effects of age, sex, and race on ECG interval measurements. J Electrocardiol. 1994;27:14–19. doi: 10.1016/s0022-0736(94)80039-1. [DOI] [PubMed] [Google Scholar]
- 17.Simonson E, Cady LD, Jr, Woodbury M. The normal Q-T interval. Am Heart J. 1962;63:747–753. doi: 10.1016/0002-8703(62)90059-5. [DOI] [PubMed] [Google Scholar]
- 18.Camm AJ, Karayal ON, Meltzer H, et al. Ziprasidone and the corrected QT interval: a comprehensive summary of clinical data. CNS Drugs. 2012;26:351–365. doi: 10.2165/11599010-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Rautaharju PM, Surawicz B, Gettes LS. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part IV: The ST Segment, T and U Waves, and the QT Interval: A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias C. Circulation. 2009;119:e241–e250. doi: 10.1161/CIRCULATIONAHA.108.191096. [DOI] [PubMed] [Google Scholar]
- 20.Reardon M, Malik M. QT interval change with age in an overtly healthy older population. Clin Cardiol. 1996;19:949–952. doi: 10.1002/clc.4960191209. [DOI] [PubMed] [Google Scholar]
- 21.Taneja T, Mahnert BW, Passman R, et al. Effects of sex and age on electrocardiographic and cardiac electrophysiological properties in adults. Pacing Clin Electrophysiol. 2001;24:16–21. doi: 10.1046/j.1460-9592.2001.00016.x. [DOI] [PubMed] [Google Scholar]
- 22.Huang JH, Lin YQ, Pan NH, et al. Aging modulates dispersion of ventricular repolarization in the very old of the geriatric population. Hear Vessel. 2010;25:500–508. doi: 10.1007/s00380-010-0026-z. [DOI] [PubMed] [Google Scholar]
- 23.Boettger MK, Schulz S, Berger S, et al. Influence of age on linear and nonlinear measures of autonomic cardiovascular modulation. Ann Noninvasive Electrocardiol. 2010;15:165–174. doi: 10.1111/j.1542-474X.2010.00358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fleg JL. Ventricular arrhythmias in the elderly: prevalence, mechanisms, and therapeutic implications. Geriatrics. 1988;43:23–29. [PubMed] [Google Scholar]
- 25.Letsas KP, Efremidis M, Kounas SP, et al. Clinical characteristics of patients with drug-induced QT interval prolongation and torsade de pointes: Identification of risk factors. Clin Res Cardiol. 2009;98:208–212. doi: 10.1007/s00392-008-0741-y. [DOI] [PubMed] [Google Scholar]
- 26.Harrigan EP, Miceli JJ, Anziano R, et al. A randomized evaluation of the effects of six antipsychotic agents on QTc, in the absence and presence of metabolic inhibition. J Clin Psychopharmacol. 2004;24:62–69. doi: 10.1097/01.jcp.0000104913.75206.62. [DOI] [PubMed] [Google Scholar]
- 27.Benoit SR, Mendelsohn AB, Nourjah P, et al. Risk factors for prolonged QTc among US adults: Third National Health and Nutrition Examination Survey. Eur J Cardiovasc Prev Rehabil. 2005;12:363–368. doi: 10.1097/01.hjr.0000173110.21851.a9. [DOI] [PubMed] [Google Scholar]
- 28.Kolbe K, Schonherr R, Gessner G, et al. Cysteine 723 in the C-linker segment confers oxidative inhibition of hERG1 potassium channels. J Physiol. 2010;588:2999–3009. doi: 10.1113/jphysiol.2010.192468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Indik JH, Pearson EC, Fried K, et al. Bazett and Fridericia QT correction formulas interfere with measurement of drug-induced changes in QT interval. Hear Rhythm. 2006;3:1003–1007. doi: 10.1016/j.hrthm.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 30.Puddu PE, Jouve R, Mariotti S, et al. Evaluation of 10 QT prediction formulas in 881 middle-aged men from the seven countries study: emphasis on the cubic root Fridericia's equation. J Electrocardiol. 1988;21:219–229. doi: 10.1016/0022-0736(88)90096-9. [DOI] [PubMed] [Google Scholar]
- 31.Luo S, Michler K, Johnston P, et al. A comparison of commonly used QT correction formulae: the effect of heart rate on the QTc of normal ECGs. J Electrocardiol. 2004;37:81–90. doi: 10.1016/j.jelectrocard.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 32.Giron MS, Forsell Y, Bernsten C, et al. Psychotropic drug use in elderly people with and without dementia. Int J Geriatr Psychiatry. 2001;16:900–906. doi: 10.1002/gps.438. [DOI] [PubMed] [Google Scholar]