Abstract
Several studies have shown that coronary artery bypass graft surgery (CABG) is superior to percutaneous coronary intervention (PCI) in patients with diabetes and multi-vessel disease. Whether this advantage of CABG over PCI is confined to diabetics who require insulin is unknown. We review the published literature comparing CABG with PCI in diabetics including 8 cohorts and 4,786 patients. There was a lower rate for all-cause mortality (Relative risk (RR): 0.78, 95% confidence interval (CI): 0.62–0.99), and for major adverse cardiac and cerebrovascular events (MACCE, RR: 0.59, 95% CI: 0.47–0.75) for CABG compared to PCI. Composite outcome of mortality, myocardial infarction and stoke was similar between CABG and PCI (RR: 0.87, 95% CI: 0.54–1.42). Visual inspection of the forest plots showed that in most analyses, the point estimates of the RR are similar between the insulin requiring group and non-insulin requiring group. On meta-regression, there was no interaction between status of insulin requirement and revascularization strategies (P > 0.05 for all). The presented data on the still unpublished analysis of the FREEDOM trial showed similar results. Thus, in the current era, CABG is superior to PCI with lower mortality and MACCE rates, but the state of insulin requirement had no effect on the outcomes from the two revascularization strategies.
Keywords: Percutaneous coronary intervention, Coronary artery bypass graft surgery, Diabetes mellitus, Insulin, Multivessel disease
1. Introduction
Coronary artery disease (CAD) is a leading cause of mortality and morbidity in diabetics, accounting for 70%–80% of deaths.[1],[2] Diabetes makes up to 20%–35% of all patients undergoing coronary revascularization.[3],[4] In diabetics, CAD tends to be diffuse having more complex lesions involving multiple vessels.[5] This makes effective revascularization difficult.
Several randomized trials have shown that coronary artery bypass graft surgery (CABG) is superior to percutaneous coronary intervention (PCI) in patients with diabetes and multi-vessel disease (MVD) mainly due to lower repeat revascularization rates.[6]–[11] However, whether the advantage of CABG over PCI is confined to diabetics who require insulin is not known. Patients who require insulin often have more long-standing diabetes with failed oral hypoglycemic therapies.[12] They have more cardiovascular risk factors with more complex end-organ macro- and micro-vascular complications.[13],[14] If the protective effect of CABG over PCI is limited to diabetics who require insulin, then there will be a huge impact, as the majority of diabetics are not insulin dependent and many are not insulin requiring.
We report a recent review of the literature comparing outcomes with CABG versus PCI in diabetics with MVD stratified by insulin requirement.
We included both randomized, controlled trials and prospective observational studies published before August 2013, involving adults (> 18 years old) with stable or unstable angina or non ST-segment Elevation Myocardial Infarction (STEMI), and had reported outcome stratified by insulin requirement. We specifically excluded studies involving patients with STEMI. Study end-points were (1) all-cause mortality, (2) major adverse cardiac and cerebrovascular events (MACCE), defined as all-cause mortality, cerebrovascular accidents (CVA), non-fatal myocardial infarction (MI), and repeat revascularization of any type, (3) composite of all-cause mortality, MI and CVA and (4) cardiac mortality.
From each of the included studies, data were extracted for the number and frequency of events at the final, or latest time-point reported. This was done separately for patients requiring insulin and for patients not requiring insulin. These data were analyzed by a random effects meta-analysis of relative risks using the user supplied METAN routine in Stata v13. In cases where exact patient number with events were not provided, we used the event rate read from the Kaplan –Meier (K-M) curve at the longest follow-up period.
To discern if the insulin requirement status alters the outcome, the comparing of CABG vs. PCI bymeta-regression is applied. This is a random effects regression weighted by the inverse of the variance of the effect size. This approach allows evaluation of outcomes to include some baseline variables that are different in the studies being analyzed.[15]–[17] Meta-regression was performed using the METAREG function of Stata, which performs random-effects meta-regression using aggregate-level data weighted by the inverse of the variance of the effect size. This function uses an iterative method to produce estimates of regression parameters, their asymptotic variances, and the residual heterogeneity variance.
2. Major findings
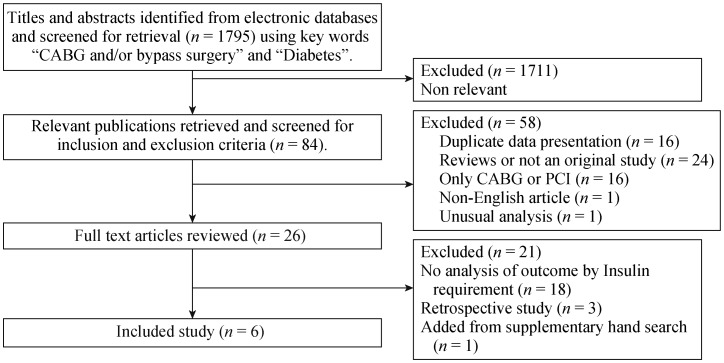
Figure 1 shows the stepwise results from the literature search. From the included final 6 publications (4,786 patients), we performed our analysis. Table 1 summarizes their characteristics. These 6 publications described 8 cohorts: 4 randomized controlled trials (RCTs) cohorts and 4 prospective observational cohorts. One of the included publications[18] reported outcomes from the Bypass Angioplasty Revascularization Investigation (BARI) randomized trial and the BARI non-randomized registry. Another described results from both Arterial Revascularization Therapy I and II trials (ARTS).[19] Also, the paper which described EMORY registry (EMORY) data[20] reported outcomes for the insulin requiring group,but not for the non-insulin requiring group.
Figure 1. Summary of study selection process.
CABG: coronary artery bypass graft; PCI: percutaneous coronary intervention.
Table 1. Baseline characteristics of included studies.
| Study [Reference] | Number of subjects | Duration, yrs | Definition of diabetes | Type of PCI | Coronary lesions | Outcome reported |
| Randomised Trials | (PCI vs. CABG) | |||||
| BARI [18] | 170 vs. 173 | 5 | Hypoglycemics or Insulin | PTCA | MVD | All-cause mortality, cardiac-mortality |
| SYNTAX [21] | 227 vs. 204 | 1 | Hypoglycemics or Insulin | DES | MVD/LMD | All-cause mortality, MACCE*, cardiac mortality, composite of death, MI and CVA |
| CARDIA [22] | 253 vs. 248 | 1 | Diet, Hypoglycemics or Insulin | DES + BMS | MVD | MACCE*, composite of death, MI and CVA |
| ARTS-I [19] | 112 vs. 96 | 3 | Diet, Hypoglycemics or Insulin | BMS | MVD | MACCE* |
| Prospective cohorts | (PCI vs. CABG) | |||||
| BARI [18] | 182 vs. 117 | 5 years | Hypoglycemics or Insulin | PTCA | MVD | All-cause mortality, cardiac-mortality |
| ARTS-II#[19] | 159 vs. 96 | 3 years | Diet, Hypoglycemics or Insulin | DES | MVD | MACCE* |
| EMORY [20] | 810 vs. 1731 | 10 years | Diet, Hypoglycemics or Insulin | PTCA | MVD | All-cause mortality |
| Japanese Registry [23] | 92 vs. 116 | 3 years | Diet, Hypoglycemics or Insulin | DES | MVD | All-cause mortality |
*MACCE: Defined as all-cause mortality, non-fatal MI, CVA and repeat revascularisation; #Comparison made between a prospective cohort (PCI) vs. historical control group (CABG). ARTS: arterial revascularisation therapy study; BARI: bypass angioplasty revascularization investigation; BMS: bare metal stent; CABG: coronary artery bypass graft; CARDIA: coronary artery revascularization in diabetes; CVA: cerebrovascular accident; DES: drug eluting stent; LMD: left main disease; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction; MVD: multi-vessel disease; PCI: percutaneous coronary intervention; PTCA: percutaneous transluminal coronary angioplasty; SYNTAX: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
Six of the 8 included cohorts defined diabetes as those requiring dietary modifications, oral hypoglycaemics or insulin. BARI[18] and SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX)[21] trials defined diabetes as those requiring oral hypoglycaemics or insulin. Diabetes was a predefined subgroup in all studies except BARI.[18]
Of the 4,786 included patients, 1,602 were insulin requiring 3,184 non- insulin requiring; 2,005 were treated with PCI and 2,781 with CABG. As for the method of PCI, the BARI trial, BARI registry,[18] and EMORY[20] used percutaneous transluminal coronary angioplasty (PTCA) while ARTS I used bare metal stent (BMS) and Coronary Artery Revascularization in Diabetes (CARDIA) trial[22] used a mixture of BMS and drug eluting stent (DES). The remaining studies, including SYNTAX, used DES. The average follow- up duration was 6.6 years, ranging from 1 to 10 years (Table 1).
3. All cause morality
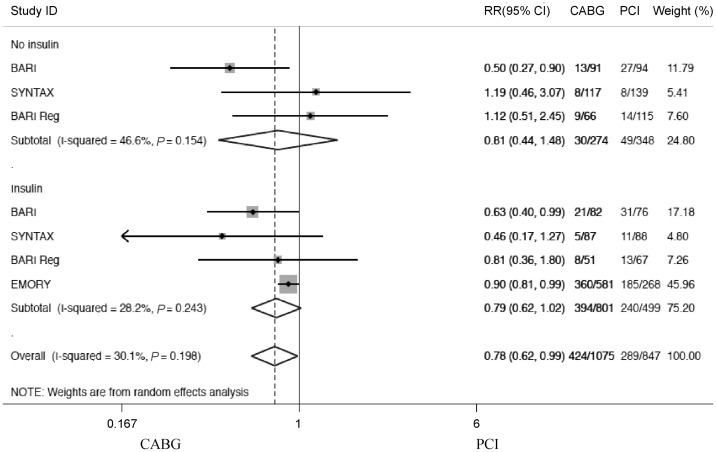
Overall the mortality rate was lower in diabetic patients treated with CABG compared to PCI (relative risk (RR): 0.78, 95% confidence interval (95%CI): 0.62–0.99, Figure 2). Visual inspection of the forest plot showed that the point estimates of the relative risk were very similar between the insulin requiring group (RR: 0.79, 95%CI: 0.62–1.02) and non-insulin requiring group (RR: 0.81, 95%CI: 0.44–1.48).
Figure 2. Forest plot showing all-cause mortality stratified by insulin requirement (CABG vs. PCI).
The EMORY registry reported K-M curves for the whole cohort and the insulin requiring group. It was considered that subtraction of the 2 K-M curves would involve too many assumptions so only results in the insulin requiring group were reported. BARI: bypass angioplasty revascularization investigation; CABG: coronary artery bypass graft; CI: confidence interval; PCI: percutaneous coronary intervention; Reg: registry data; RR: relative risk; SYNTAX: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
A separate analysis with the two RCTs showed that within the insulin requiring group, patients treated with CABG had approximately 40% lower risk of mortality compared to those treated with PCI (RR: 0.60, 95%CI: 0.39–0.90). The interaction term from meta-regression between insulin use and treatment method (PCI vs. CABG) was not significant (P = 0.952 for all studies, P = 0.778 for RCTs only, Table 2).
Table 2. P values from meta-regression of interaction term between insulin and study type and outcomes.
| Outcome | All studies | RCTs | Cohort |
| All cause mortality | 0.952 | 0.778 | 0.677 |
| MACCE | 0.883 | 0.947 | 0.563 |
| Composite of all-cause mortality, MI and CVA. | 0.182 | 0.182 | –* |
| Cardiac death | 0.307 | 0.470 | –# |
*No observational studies reported composite outcome of all-cause mortality, MI and CVA; #Only one observational study reported cardiac death and meta-regression was not performed. CVA: cerebrovascular accidents; MACCE: major adverse coronary and cerebrovascular events; MI: myocardial infarction; RCTs: randomised controlled trials.
4. MACCE
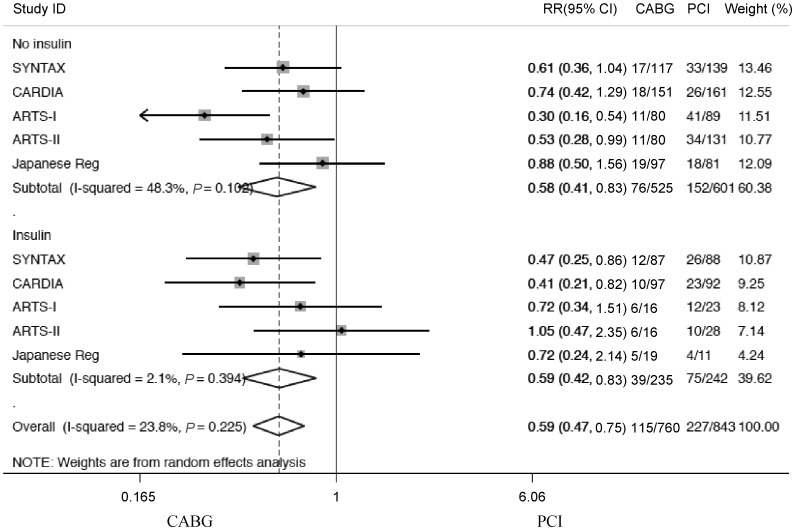
Figure 3 shows that the overall MACCE rate was lower in diabetic patients treated with CABG than those treated with PCI (RR: 0.59, 95%CI: 0.47–0.75). This was present for both insulin groups. Visual inspection of forest plots showed that the point estimates of the relative risk were very similar between the insulin requiring group (RR: 0.59, 95%CI: 0.42–0.83) and non-insulin requiring group (RR: 0.58, 95%CI: 0.41–0.83). An analysis of MACCE with just RCTs revealed a RR of 0.52 favoring CABG, which is no different from the overall analysis.
Figure 3. Forest plot showing MACCE stratified by insulin requirement (CABG vs. PCI).
ARTS: arterial revascularisation therapy study; CABG: coronary artery bypass graft; CARDIA: coronary artery revascularization in diabetes; CI: confidence interval; MACCE: major adverse cardiac and cerebrovascular events; PCI: percutaneous coronary intervention; Reg: registry data; RR: relative risk; SYNTAX: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
The interaction term from meta-regression of insulin use and treatment method was not significant for MACCE (P = 0.883 for all studies, and P = 0.947 for RCTs, Table 2).
5. Composite of all-cause mortality, MI and CVA
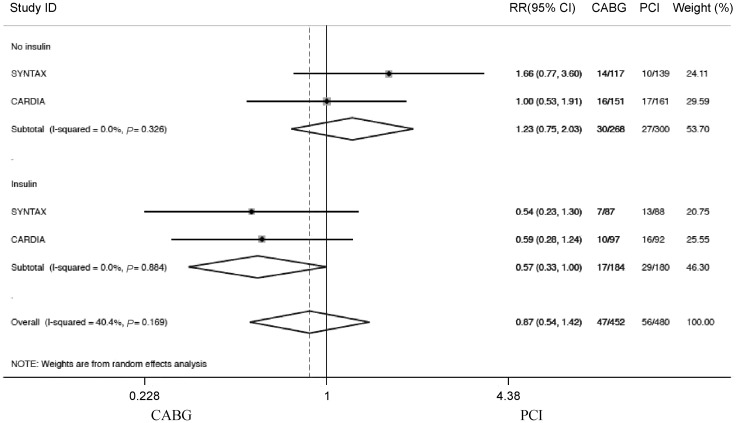
Of the eight included cohorts, only two RCTs (CARDIA and SYNTAX) reported the composite of all-cause mortality, MI, and CVA by insulin requirements (Figure 4). Among diabetics treated with insulin, this composite endpoint tended to be lower in those treated with CABG compared to those treated with PCI (RR: 0.57, 95%CI: 0.33– 1.00). Among the non-insulin requiring diabetics, there was no difference in outcome between CABG and PCI (RR: 1.23, 95%CI: 0.75–2.03). The interaction term from meta- regression of insulin use and treatment method was not significant (P = 0.182, Table 2.)
Figure 4. Forest plot showing composite of all-cause mortality, MI and CVA stratified by insulin requirement (CABG vs. PCI).
CABG: coronary artery bypass graft; CARDIA: coronary artery revascularization in diabetes; CI: confidence interval; CVA: cerebrovascular accidents; MI: myocardial infarction; PCI: percutaneous coronary intervention; RR: relative risk; SYNTAX: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
6. Cardiac mortality
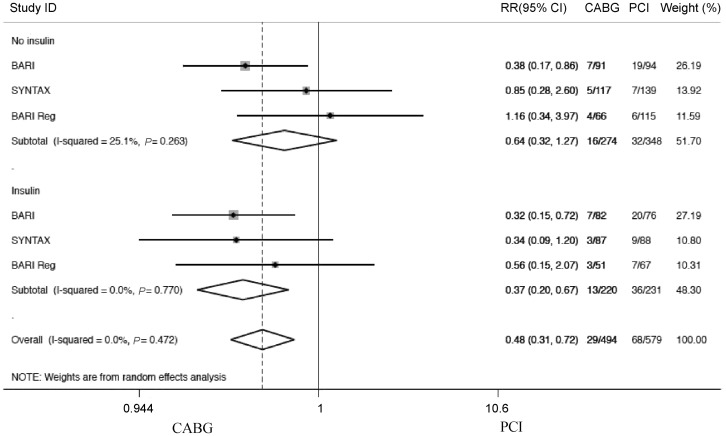
In all diabetics with MVD, the risk of cardiac mortality was 52% lower in patients treated with CABG compared to PCI (RR: 0.48, 95%CI: 0.31–0.72, Figure 5). Visual inspec- tion suggested that the point estimate of the relative risk was lower in the insulin requiring group (RR: 0.37, 95%CI: 0.20– 0.67) than in the non-insulin requiring group (RR: 0.64, 95%CI: 0.32–1.27). A separate analysis with only RCTs (BARI and SYNTAX) did not reveal much difference in treatment effect between the two diabetic groups. The interaction term from meta-regression of insulin use and treatment method was not significant (P = 0.307, Table 2).
Figure 5. Forest plot showing cardiac mortality stratified by insulin requirement (CABG vs. PCI).
BARI: bypass angioplasty revascularization investigation; CABG: coronary artery bypass graft; CI: confidence interval; PCI: percutaneous coronary intervention; Reg: registry data; RR: Relative risk; SYNTAX- SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
7. Discussion
In the current review including 4,786 diabetics with MVD, CABG provides statistically significant advantages over PCI, with lower rates of all-cause mortality, cardiac mortality and MACCE. The status on insulin requirement has no effect on the relative advantage of CABG over PCI.
The optimal revascularization method in diabetics with MVD has been investigated previously. Two separate meta-analyses by Hoffman, et al.[24] and by Daemen, et al.[25] found no difference in all-cause mortality between CABG and PCI. A separate patient level data meta-analysis of 10 RCTs by Hlatky et al.[26] found increased mortality in those treated with PCI. Another recent meta-analysis by Zhang et al.[27] including more recent trials such as SYNTAX and CARDIA also found increased mortality in those treated with PCI. These findings should be interpreted in the context that all avenues of patient management: medications, CABG, PCI have been continuously evolving over the period, so that earlier reviews may not be as applicable.
The finding from our analysis (21% lower all-cause mortality risk with CABG versus PCI) supporting the superiority of CABG over PCI adds to the literature. Of note, we only included studies that reported status of insulin requirement. Our neutral finding between the two revascularization methods on the composite endpoint of mortality, MI and CVA is likely because of the fact that the risks of CVA is generally higher with CABG.[28] Our overall findings are consistent with the patient level meta-analysis from Daemen et al.[25] published 5 years ago which included different studies than ours. Our current study, despite using stringent inclusion criteria requiring data on insulin status, has included the more recent trials of CARDIA and SYNTAX.
In the recent FREEDOM trial recruiting patients from 2005 to 2010, 1900 patients with diabetes and multivessel disease were randomized to undergo either PCI with DES, or CABG,[29] and were followed-up for a median of 3.8 years. Comparing the PCI group with the CABG group, the 5-year K-M rate was higher for all-cause mortality (16.3% vs. 10.9%, P = 0.049) but not different for cardiovascular mortality (10.9 vs. 6.8%, P = 0.12). The 5 year K-M rate was also higher for MI (13.9 vs. 6.0%, P < 0.001), but for CVA this was lower (2.4% vs. 5.2%, P = 0.03). For the primary endpoint in FREEDOM (combined rate of death, MI, or CVA) the 5-year K-M rate was 26.6% vs. 18.7%, P = 0.005; suggesting that CABG was of greater benefit than PCI.[29]
Theoretically, an advantage of CABG over PCI in one subset of diabetics may be offset by a disadvantage in the remainder so that the overall result is relatively neutral. In our meta-regression analysis, there is no interaction between the status of insulin requirement and outcome after the 2 different revascularization strategies. In diabetics, the advantage of having CABG over PCI as the revascularization strategies persists regardless of the status of insulin requirement. Recently, the FREEDOM investigators presented their yet unpublished analysis in the 2013 October Transcatheter Cardiovascular Therapeutics (TCT) meeting. Among non-insulin treated patients, 5-year K-M mortality rate was 14.5% in the PCI group and 9.3% in the CABG group (an advantage of 5.2% with CABG). Among insulin treated patients, 5-year K-M mortality rate was 19% in the PCI group and 14.1% in the CABG group (an advantage of 5.1% with CABG). Findings on the other endpoints of stroke, MI and MACCE are similar showing insulin use did not alter the relative outcome between the PCI group and the CABG group. The interaction P value is non-significant for all reported endpoints.
In conclusion, there is likely a significant survival (mortality) and event free (MAACE) advantage favoring CABG over PCI in diabetic patients with MVD. The status of insulin requirement does not influence the outcome after different modes of revascularization. This important finding is similar to the presented result of the insulin and non-insulin subsets analyses of the FREEDOM trial. In diabetics with MVD, insulin requirement should not be used to determine the revascularization strategy.
References
- 1.Harris MI. Diabetes in America: epidemiology and scope of the problem. Diabetes Care. 1998;21(Suppl 3):C11–C14. doi: 10.2337/diacare.21.3.c11. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- 3.Brooks MM, Jones RH, Bach RG, et al. Predictors of mortality and mortality from cardiac causes in the bypass angioplasty revascularization investigation (BARI) randomized trial and registry. For the BARI Investigators. Circulation. 2000;101:2682–2689. doi: 10.1161/01.cir.101.23.2682. [DOI] [PubMed] [Google Scholar]
- 4.Weintraub WS, Grau-Sepulveda MV, Weiss JM, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–1476. doi: 10.1056/NEJMoa1110717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicholls SJ, Tuzcu EM, Kalidindi S, et al. Effect of diabetes on progression of coronary atherosclerosis and arterial remodeling: a pooled analysis of 5 intravascular ultrasound trials. J Am Coll Cardiol. 2008;52:255–262. doi: 10.1016/j.jacc.2008.03.051. [DOI] [PubMed] [Google Scholar]
- 6.Influence of diabetes on 5-year mortality and morbidity in a randomized trial comparing CABG and PTCA in patients with multivessel disease: the Bypass Angioplasty Revascularization Investigation (BARI) Circulation. 1997;96:1761–1769. doi: 10.1161/01.cir.96.6.1761. [DOI] [PubMed] [Google Scholar]
- 7.King SB, III, Kosinski AS, Guyton RA, et al. Eight-year mortality in the Emory Angioplasty versus Surgery Trial (EAST) J Am Coll Cardiol. 2000;35:1116–1121. doi: 10.1016/s0735-1097(00)00546-5. [DOI] [PubMed] [Google Scholar]
- 8.Serruys PW, Ong AT, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575–581. doi: 10.1016/j.jacc.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez AE, Baldi J, Fernández Pereira C, et al. Five-year follow-up of the Argentine randomized trial of coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple vessel disease (ERACI II) J Am Coll Cardiol. 2005;46:582–588. doi: 10.1016/j.jacc.2004.12.081. [DOI] [PubMed] [Google Scholar]
- 10.Hueb W, Lopes NH, Gersh BJ, et al. Five-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2007;115:1082–1089. doi: 10.1161/CIRCULATIONAHA.106.625475. [DOI] [PubMed] [Google Scholar]
- 11.Javaid A, Steinberg DH, Buch AN, et al. Outcomes of coronary artery bypass grafting versus percutaneous coronary intervention with drugeluting stents for patients with multivessel coronary artery disease. Circulation. 2007;116:I200–I206. doi: 10.1161/CIRCULATIONAHA.106.681148. [DOI] [PubMed] [Google Scholar]
- 12.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 13.Akin I, Bufe A, Eckardt L, et al. Comparison of outcomes in patients with insulin-dependent versus non-insulin dependent diabetes mellitus receiving drug-eluting stents (from the first phase of the prospective multicenter German DES.DE registry) Am J Cardiol. 2010;106:1201–1207. doi: 10.1016/j.amjcard.2010.06.042. [DOI] [PubMed] [Google Scholar]
- 14.Bauer T, Möllmann H, Weidinger F, et al. Impact of diabetes mellitus status on coronary pathoanatomy and interventional treatment: insights from the Euro heart survey PCI registry. Catheter Cardiovasc Interv. 2011;78:702–709. doi: 10.1002/ccd.22939. [DOI] [PubMed] [Google Scholar]
- 15.Harris RJ, Bradburn MJ, Deeks JJ, et al. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. [Google Scholar]
- 16.Thompson S, Higgin JPT. How should meta-regression analyses be undertaken and interpreted? Statist Med. 2002;21:1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 17.van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Statist Med. 2002;21:589–624. doi: 10.1002/sim.1040. [DOI] [PubMed] [Google Scholar]
- 18.Detre KM, Guo P, Holubkov R, et al. Coronary revascularization in diabetic patients: a comparison of the randomized and observational components of the bypass Angioplasty Revascularization Investigation (BARI) Circulation. 1999;99:633–640. doi: 10.1161/01.cir.99.5.633. [DOI] [PubMed] [Google Scholar]
- 19.Daemen J, Kuck KH, Macaya C, et al. Multivessel coronary revascularization in patients with and without diabetes mellitus: 3-year follow-up of the ARTS-II (Arterial Revascularization Therapies Study-Part II) trial. J Am Coll Cardiol. 2008;52:1957–1967. doi: 10.1016/j.jacc.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 20.Weintraub WS, Stein B, Kosinski A, et al. Outcome of coronary bypass surgery versus coronary angioplasty in diabetic patients with multivessel coronary artery disease. J Am Coll Cardiol. 1998;31:10–19. doi: 10.1016/s0735-1097(97)00441-5. [DOI] [PubMed] [Google Scholar]
- 21.Banning AP, Westaby S, Morice MC, et al. Diabetic and nondiabetic patients with left main and/or 3-vessel coronary artery disease: comparison of outcomes with cardiac surgery and paclitaxel-eluting stents. J Am Coll Cardiol. 2010;55:1067–1075. doi: 10.1016/j.jacc.2009.09.057. [DOI] [PubMed] [Google Scholar]
- 22.Kapur A, Hall RJ, Malik IS, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial. J Am Coll Cardiol. 2010;55:432–440. doi: 10.1016/j.jacc.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Yamagata K, Kataoka Y, Kokubu N, et al. A 3-year clinical outcome after percutaneous coronary intervention using sirolimus-eluting stent and off-pump coronary artery bypass grafting for the treatment of diabetic patients with multivessel disease. Circ J. 2010;74:671–678. doi: 10.1253/circj.cj-09-0736. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman SN, TenBrook JA, Wolf MP, et al. A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: one- to eight-year outcomes. J Am Coll Cardiol. 2003;41:1293–1304. doi: 10.1016/s0735-1097(03)00157-8. [DOI] [PubMed] [Google Scholar]
- 25.Daemen J, Boersma E, Flather M, et al. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation. 2008;118:1146–1154. doi: 10.1161/CIRCULATIONAHA.107.752147. [DOI] [PubMed] [Google Scholar]
- 26.Hlatky MA, Boothroyd DB, Bravata DM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373:1190–1197. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 27.Zhang F, Yang Y, Hu D, et al. Percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) in the treatment of diabetic patients with multi-vessel coronary disease: a meta-analysis. Diabetes Res Clin Pract. 2012;97:178–184. doi: 10.1016/j.diabres.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 28.Gao F, Zhou YJ, Shen H, et al. Meta-analysis of percutaneous coronary intervention versus coronary artery bypass graft surgery in patients with diabetes and left main and/or multivessel coronary artery disease. Acta Diabetol. 2013;50:765–773. doi: 10.1007/s00592-012-0411-4. [DOI] [PubMed] [Google Scholar]
- 29.Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–2384. doi: 10.1056/NEJMoa1211585. [DOI] [PubMed] [Google Scholar]