Abstract
Current recommendations encourage the use of embolic stroke (ES) models and replication of results across laboratories in preclinical research. Since such endeavors employ different surgeons, we sought to ascertain the impact of injection technique on outcome and response to thrombolysis in an ES model. Embolic stroke was induced in Male Wistar Kyoto rats (n=166) by a fast or a slow clot injection (CI) technique. Saline or recombinant tissue plasminogen activator (rtPA) was given at 1 hour after stroke. Flow rate curves were assessed in 24 animals. Cerebral perfusion was assessed using laser Doppler flowmetry. Edema corrected infarct volume, hemispheric swelling, hemorrhagic transformation, and neurologic outcome were assessed at 24 hours after stroke. Clot burden was estimated in a subset of animals (n=40). Slow CI resulted in significantly smaller infarct volumes (P=0.024) and better neurologic outcomes (P=0.01) compared with fast CI at 24 hours. Unexpectedly, rtPA treatment attenuated infarct size in fast (P<0.001) but not in slow CI experiments (P=0.382), possibly related to reperfusion injury as indicated by greater hemorrhagic transformation (P<0.001) and hemispheric swelling (P<0.05). Outcome and response to thrombolysis after ES are operator dependent, which needs to be considered when comparing results obtained from different laboratories.
Keywords: animal model, embolic stroke, thrombolysis, tissue plasminogen activator
Introduction
Rat embolic stroke (ES) models are of great value in preclinical research because they closely mimic key aspects of human stroke pathophysiology. In addition to allowing for the study of reperfusion strategies,1, 2 they afford the unique possibility to explore phenomena that are not amenable to investigation with mechanical arterial occlusion approaches.3, 4, 5
However, depending on the model used, variability in infarct volume and mortality rates may be considerable.6 While it appears straight forward to standardize many factors potentially influencing model outcome (such as animal strain, gender, age, clot properties,7 surgical approach,8 and degree of blood flow reduction9) it may be challenging to control for operator-dependent factors. Arguably, this may be of little consequence for studies done in a blinded and randomized manner within a single laboratory by a single surgeon. Yet, if potential surgeon-related bias is not considered, then interpretation of results across different laboratories may be more complicated given the inherent variability of stroke models.10, 11, 12 If true, then this may have profound implications for the design of recommended multicenter preclinical phase III-type studies, which will involve many surgeons and thus potentially differing techniques.13, 14
Notably, we observed consistently differing infarct volumes and mortality rates among surgeons in our laboratory. Further investigation suggested the speed of clot injection (CI) as a critical variable; prompting us to adopt a slow CI technique (as opposed to a fast injection) in all subsequent experiments in an attempt to achieve smaller infarct volumes and greater animal survival. We now sought to formally investigate whether this protocol change resulted in different outcomes. To this end, we retrospectively compared data gained from all ES experiments conducted by a single surgeon using a fast or a slow CI technique in our laboratory.
Materials and methods
Animals in all original experiments were given ad libitum access to food and water and maintained on a 12-hour light/12-hour dark cycle. Our manuscript was written according to ARRIVE guidelines and experimental protocols were in accordance with the relevant guidelines and regulations of, and approved by, the Institutional Animal Care and Use Committee at the University of Massachusetts Medical School.
This study is a retrospective analysis of consecutive rats subjected to ES in our laboratory between January 2007 and June 2013. All animals were operated as part of experiments investigating the efficacy of recombinant tissue plasminogen activator (rtPA). In all studies, animals were randomly assigned to vehicle (saline) or rtPA treatment and all analyses were performed blindly. A fast CI technique was used from January 2007 to September 2010 and a slow CI technique thereafter.
This protocol change was prompted by our anecdotal observation that different surgeons appeared to achieve consistently different infarct volumes and survival rates. After excluding potential variation in experimental set-up, clot properties, surgery, and anesthesia we determined that the most likely confounding factor was the speed of manual CI (‘as fast as possible' versus ‘slowly over 2 seconds'). Because infarct volumes appeared to be smaller with slow CI and for consistency we asked all surgeons to exclusively use the slow CI paradigm with the goal to inject the clot over 2 seconds after September 2010. To minimize confounding, we only considered animals operated by a single, experienced surgeon (JB) for the purpose of the current analysis. Further, the first 16 animals operated using the slow CI technique for training purposes were excluded.
Clot properties as well as animal set-up and surgery were identical in all experiments. Animals were excluded if they had incomplete middle cerebral artery occlusion as defined by a reduction in relative regional cerebral blood flow (rrCBF) by <55% from baseline.9 Animals with incomplete blood gasses and electrolytes, dying prematurely within 16 hours from ES, or with a final infarct volume of <50 mm3 were excluded from all analyses as previously described.9 Animals dying between 16 and 24 hours after stroke onset were included in all data analyses and 2,3,5-triphenyl-tetrazolium chloride staining was performed within a few hours after the animal was last observed to be alive.15
Study Design
Male Wistar Kyoto rats weighing 306±25 g (Charles River, Wilmington, MA, USA) underwent ES, which was induced using either a fast or a slow CI technique. In 166 animals, infarct volume and neurologic outcomes were assessed at 24 hours after receiving saline (n=50 fast CI and n=49 slow CI) or rtPA (n=37 fast CI and n=30 slow CI, 10 mg/kg) at 60 minutes after ES over 60 minutes, respectively. After a 0.1-mL bolus administration, an infusion pump was used to continuously deliver saline or rtPA at a rate of 1 mL/h for all experiments.9 In 10 rats per subgroup clot burden was assessed at 24 hours. In 24 animals (n=11 fast and n=13 slow) flow rate curve analysis was performed in a randomized manner to ascertain reproducibility of the CI technique.
To alleviate pain, animals received 0.05 mg/kg subcutaneous buprenorphine (Patterson Veterinary, Devens, MA, USA) 30 minutes before the end of anesthesia and every 6 hours afterwards for 12 hours. Additionally, each animal received 5 mg/kg subcutaneous carprofen (Patterson Veterinary) at the end of the anesthesia. Given the severity of the used stroke model, which renders long-term survival studies unfeasible, animals underwent neurologic assessment followed by euthanasia and brain removal at 24 hours after ES.
Embolus Preparation
Embolus preparation was performed as previously described in detail.16 In brief, whole blood (200 μL) was withdrawn from the rat 24 hours prior surgery into an Eppendorf tube, promptly mixed with 1.0 NIH unit (10 μL) of bovine thrombin, and 4.5 μL of 1 mol/L CaCl2 for a final CaCl2 concentration of 20 mmol/L. Within 5 seconds, a small portion of this mixture was drawn into an ∼30.0-cm length of PE-50 and allowed to clot at 37 °C for 2 hours. At the end of this period, the clot was extruded from the catheter into a saline-filled petri dish and stored at 4 °C for 22 hours. Before ES, the clot was placed into distilled water for 5 minutes at room temperature, then transferred into isotonic saline and dissected into a single 20-mm section. This section (clot) was collected into a PE-10 catheter, in a volume of 50 μL of saline and trimmed to a total length of 18 mm as measured inside the PE-10 catheter. To assess ex-vivo clot burden in a subset of animals (n=40), clots were dyed with Evans Blue as previously described.17
Embolic Stroke
Rats were anesthetized with isoflurane (5% for induction, 2% for surgery, and 1.5% for maintenance) in room air. PE-50 polyethylene tubing was inserted into the left femoral artery for continuous monitoring of mean arterial blood pressure and for obtaining blood samples to measure blood gases (pH, PaO2, and PaCO2), electrolytes (Na+, K+, and Ca2+ ) and plasma glucose at baseline, middle cerebral artery occlusion, and every 1 hour for 2 hours after ES. A second PE-50 tube was placed into the left femoral vein to allow intravenous vehicle or rtPA infusion. Body temperature was maintained at 37.0±0.5°C with a thermostatically controlled heating lamp.
For ES, PE-50 tubing with a PE-10 catheter tip was inserted via the external carotid artery into the internal carotid artery to the skull base and a single red blood clot was injected manually using 50 μL saline.16 After 7 minutes, the catheter was removed.
Clot Injection Measurements
To determine the intraoperator consistency of the CI speed as well as to characterize fast CI, real-time flow during the CIs was measured using a data acquisition system (Dewetron, Charlestown, RI, USA) connected to a flow probe (Transonic Systems, Ithaca, NY, USA), which was calibrated before the start of each experiment (Harvard Apparatus, Hollistone, MA, USA).18
Laser Doppler Flowmetry
Cerebral blood flow was measured in all animals using a PR407-1 straight needle LDF-probe (Perimed, Järfälla, Stockholm, Sweden) connected to a standard laser Doppler monitor (PF5010 LDPM Unit and PF5001 main unit; Perimed). The probe was placed over the ischemic hemisphere (4 mm posterior, 6.5 mm lateral, and 3 mm ventral to the Bregma) on the intact lateral aspect of the skull to assess CBF in the penumbral area.9 A stable baseline was established and recorded for 1 minute, ES was induced and rrCBF continuously assessed for 2 hours after occlusion. Values were averaged across 1 minute epochs at the designated time points (at baseline as well as at 1, 30, 60, 90, and 120 minutes).
Neurologic Scoring
Neurologic deficits were graded using a modified neuroscore according to Menzies et al19 at 24 hours as follows: 0=no deficit, 1=failure to extend the left forepaw, 2=circling to paretic side by pulling the tail, 3=spontaneous contralateral circling, 4=depressed level of consciousness, and 5=dead.
Postmortem Analysis
Brains were sectioned coronally into eight 1.5-mm-thick slices and stained with 2,3,5-triphenyl-tetrazolium chloride for infarct volume calculation with edema correction.16
Brain swelling was expressed as the volume increase in the affected hemisphere (%HSE) and calculated as follows: HSE=100 × (HVi−HVc)/HVc where HVi and HVc are the volumes of the ipsilesional and contralesional hemispheres, respectively.20
The volume of hemorrhagic infarct transformation (HT) was estimated by summation of the areas in all brain slices showing HT21 and integrated by slice thickness (Supplementary Figure 1A).
Ex-vivo clot burden was assessed in animals injected with Evans Blue dyed clots by summing the area of all clot fragments visualized within the middle cerebral artery of the intact brain (Supplementary Figure 1C and D) using ImageJ (NIH, USA, http://imagej.nih.gov).17 In addition, the pattern of clot distribution within the Circle of Willis and its dependent branches was documented.
Statistical Analysis
Data are presented as mean±s.d. unless otherwise stated. For parametric tests, statistical comparisons were performed using analysis of variance with post hoc Fisher LSD Method for multiple comparisons, or Student's t-test, as appropriate. For nonparametric tests, Kruskal–Wallis analysis of variance on ranks with post hoc Dunn's method or Mann–Whitney U test were used. Because respective fast and slow CI experiments were not done concurrently (and unmeasured variables could have influenced the results across years) we employed Spearman correlation analyses to ascertain whether there was an association between final infarct volume as well as neurologic outcome with the time of surgery.
Interrater agreement of the HT measurement was determined by a Bland-Altman analysis performed on 80 slices of 10 randomly selected brains. To assess the correlation of HT measurements between raters, we computed the Pearson correlation coefficient (r). Secondary analyses were performed excluding all animals that had died between 16 and 24 hours after ES. Power calculations to determine group sizes were performed for the original experiments. Data analysis was performed using SPSS (Version 20.0, SPSS Inc., Chicago, IL, USA).
Results
Supplementary Figure 2 shows the flow chart of animal exclusion. Among the 622 animals in the database, 166 were included in the final analysis. Temperature, blood pressure, blood gases, glucose, and electrolytes were within the physiologic range in all groups and across time points. Weight before stroke did not differ significantly among experimental groups (data not shown).
In-Vivo Clot Injection
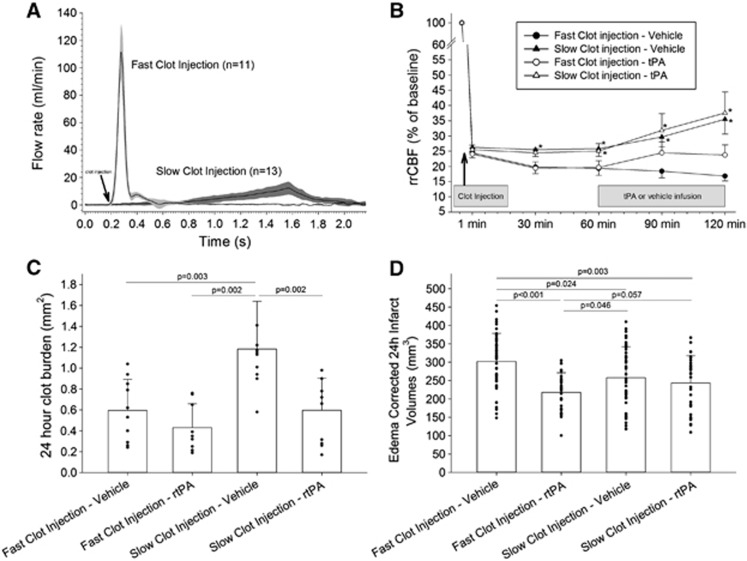
Figure 1A shows the superimposed flow rate curves during fast and slow CI. Respective peak flow rate (112±26 mL/min and 12±5 mL/min) was reached within 0.28 and 1.57 seconds in fast versus slow CI animals. Overall, flow curves were very similar between respective fast and slow CI experiments.
Figure 1.
(A) Flow rate curves in slow versus fast clot injection (CI). Arrow denotes start of CI. (B) Relative regional cerebral blood flow (rrCBF) as assessed by laser Doppler flowmetry in animals subjected to fast versus slow CI. *P<0.05 versus fast CI vehicle group. (C) At 24 hours after CI, significantly less clot material was visualized in the circle of Willis and dependent arteries of vehicle animals subjected to fast versus slow CI. Treatment with recombinant tissue plasminogen activator (rtPA) significantly reduced clot burden in slow CI but not in fast CI animals (P=0.195). (D) Comparison of final infarct volumes between experimental groups.
Cerebral Blood Flow
Figure 1B depicts the temporal evolution of rrCBF after ES. In all groups, rrCBF declined to ∼25% of baseline (P=0.821 for between group differences). In animals subjected to fast CI, a further decline of rrCBF was observed from 30 to 120 minutes (P<0.05). Conversely, rrCBF remained unchanged up to 60 minutes after embolism in slow CI animals (P>0.05). After the start of rtPA at 60 minutes, there was a tendency toward increasing rrCBF in fast injected animals but this was not statistically significant (P=0.817). Similarly, in slow injected animals, rrCBF tended to increase at 90 to 120 minutes in vehicle (P=0.389) and rtPA-treated (P=0.954) animals to a similar degree but this was not statistically significant.
Clot Burden
There was a similar pattern of clot distribution within the Circle of Willis and its dependent branches after fast versus slow CI (not shown). However, after fast CI less clot material was visible as compared with slow CI (0.60±0.30 versus 1.18±0.46 mm2, P=0.003; Figure 1C). While thrombolysis was associated with decreased 24 hours clot burden as compared with vehicle treatment, this only reached significance in slow CI animals (P=0.002) but not in fast CI experiments (P=0.195).
Of note, in vitro clot extrusion (i.e., ejection of the clot from the catheter into a saline-filled petri dish) did not show clot fragmentation or a difference in clot size when using a fast (1.239±0.122 mm2, n=10) versus slow (1.184±0.076 mm2, n=10) CI approach (P=0.240; Supplementary Figure 1E).
Mortality
In vehicle animals, mortality between 16 and 24 hours after ES was significantly greater in fast (n=27 (54%)) versus slow (n=15 (31%)) CI animals (P=0.025). In animals randomized to rtPA, mortality did not differ between fast (n=17 (46%)) and slow (n=11 (37%)) CI animals (P=0.467).
Infarct Volume
Since all fast CI experiments were conducted before the slow CI experiments, we first correlated the date of surgery with infarct volumes in each subgroup to assess whether inadvertent changes in operative technique or other unmeasured factors may have contributed to differing lesion volumes over time (‘drift'). These analyses showed no significant association between the date of surgery and infarct volume within each subgroup: fast CI vehicle r=0.015, P=0.992; slow CI vehicle r=0.025, P=0.862; fast CI rtPA r=0.270, P=0.116; and slow CI rtPA r=0.331, P=0.074.
Figure 1D depicts the 24-hour edema corrected infarct volumes. In vehicle animals, infarct volumes were significantly smaller in animals subjected to slow CI compared with those subjected to fast CI (258±84 versus 298±75 mm3, P=0.024). Interestingly, while rtPA treatment significantly attenuated infarct size in fast CI animals (P<0.001) it did not affect lesion volume in slow injected animals (P=0.382).
Of note, exclusion of animals that died between 16 and 24 hours did not meaningfully change these results: slow CI animals receiving vehicle had smaller infarct volumes than fast CI animals (P=0.029) and rtPA reduced infarct volume in fast CI animals (202±72 versus 276±71 mm3, P=0.002) but not in slow CI animals (214±66 versus 231±84 mm3, P=0.426).
Hemispheric Swelling
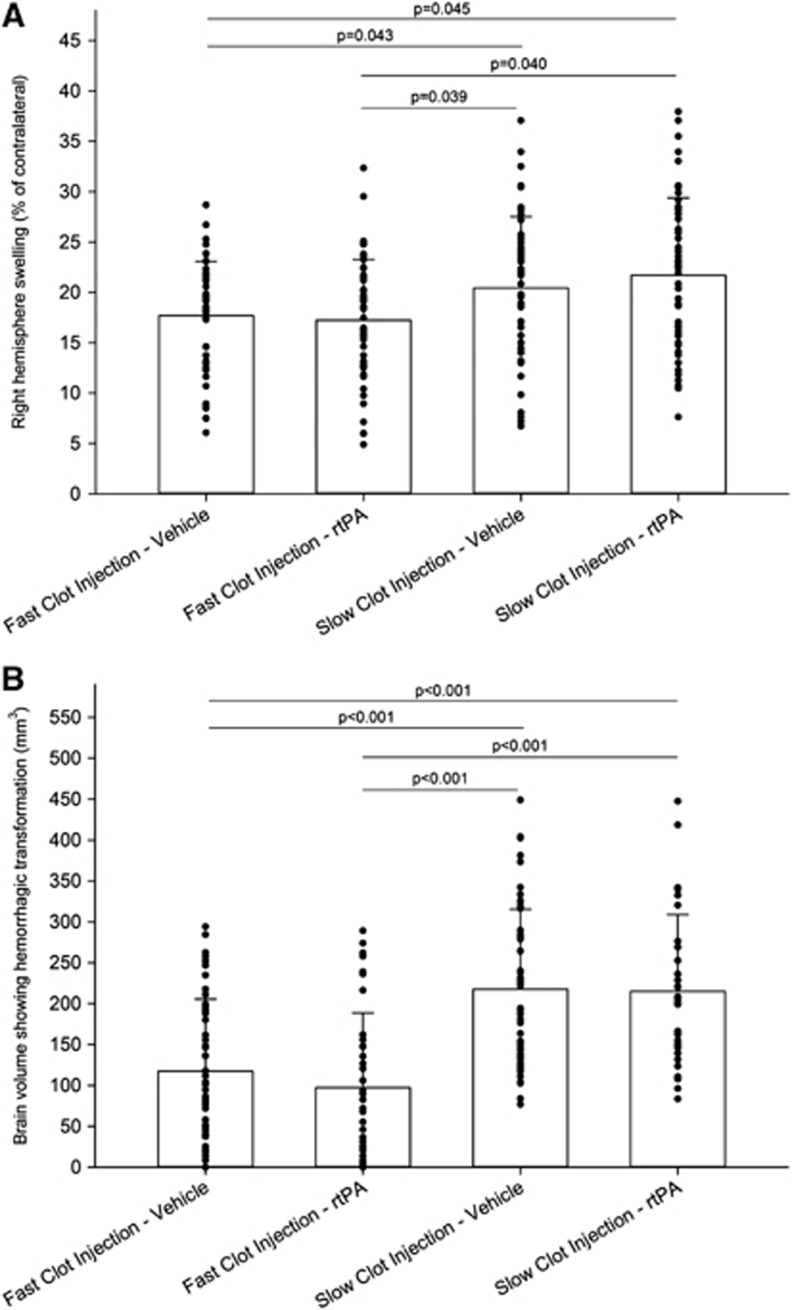
Ipsilesional hemisphere swelling at 24 hours after ES is depicted in Figure 2A. Animals subjected to slow CI had significantly greater swelling than those subjected to fast CI (P<0.05). There was no significant difference in ipsilesional hemisphere swelling in rtPA versus saline-treated animals subjected to slow and fast CI, respectively (P>0.05).
Figure 2.
(A) Comparison of right hemispheric swelling between all experimental groups. At 24 hours after embolic stroke, animals subjected to slow clot injection (CI) had a significantly greater swelling than animals subjected to fast CI. (B) At 24 hours after embolic stroke, animals subjected to slow CI had a significantly greater brain volume with hemorrhagic transformation (not corrected for edema) than animals subjected to fast CI (one-way analysis of variance (ANOVA) with post hoc Fisher LSD testing). rtPA, recombinant tissue plasminogen activator.
After exclusion of animals that died between 16 and 24 hours there was no significant between-group difference (P=0.054, not shown), consistent with the notion that death in these animals is caused by malignant infarction.
Hemorrhagic Transformation
There was excellent interrater agreement in HT assessment as indicated by a significant correlation of HT measurements (Pearson r=0.981, P<0.0001), small rater bias (rater 2: −0.54 mm2; 95% CI=−1.43 to 0.34 mm2), and narrow limits (−8.28 to 7.19 mm2; Supplementary Figure 1B).
Hemorrhagic infarct transformation was significantly greater in slow versus fast CI vehicle (P<0.001) as well as slow versus fast CI rtPA (P<0.001) animals (Figure 2B). Within each injection approach, HT was similar in animals treated with saline versus rtPA (P=0.320 for fast CI and P=0.909 for slow CI).
Excluding animals that died between 16 and 24 hours did not meaningfully change these associations (not shown).
Behavioral Outcome
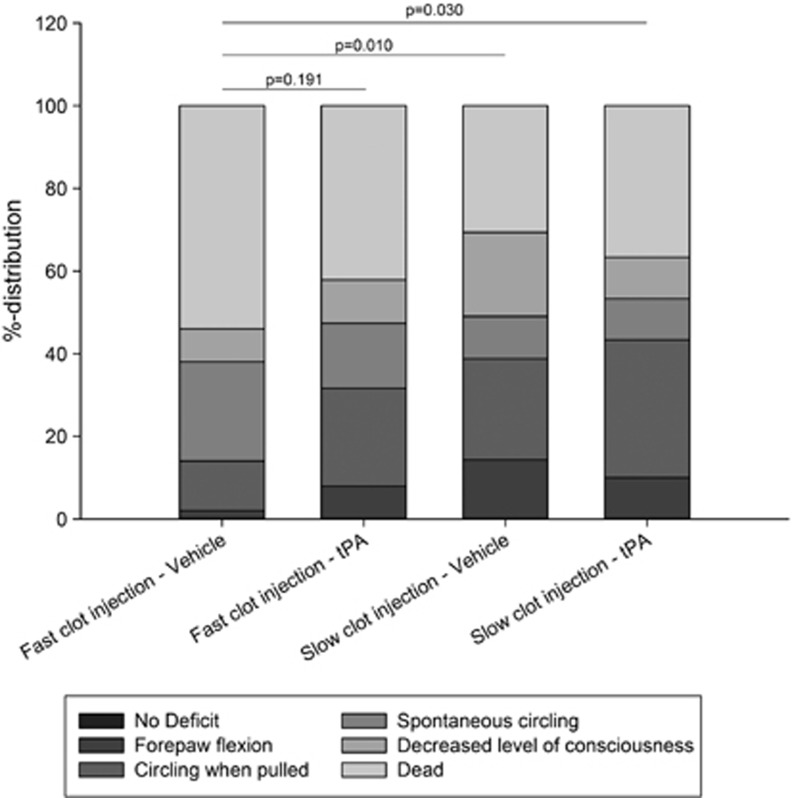
Figure 3 summarizes the distribution of 24 hours neurologic scores within each subgroup. Compared with slow CI, fast CI was associated with significantly worse neurologic outcomes at 24 hours (P=0.01). Treatment with rtPA tended to improve outcome in fast CI animals but this did not reach statistical significance (P=0.191). No overt benefit with rtPA was noted in slow CI animals (P=0.892).
Figure 3.
Distribution of 24 hours neuroscores in each subgroup. tPA, tissue plasminogen activator.
After exclusion of animals that were dead at 24 hours the moderate to strong association between infarct volume and neuroscore remained but this was only significant in fast CI animals (not shown). However, given the relatively low n, there was insufficient power to detect a significant association.
Discussion
The most important findings of this study are that outcome and response to rtPA after ES were highly dependent on the CI technique. Specifically, using a fast injection paradigm resulted in significantly greater infarct volumes and mortality as compared with slow CI. Consistent with prior observations thrombolysis with rtPA reduced lesion volumes in fast CI animals. However, contrary to our expectations, rtPA did not significantly reduce infarct volumes in slow CI experiments.
The reasons for the observed differential effect are not entirely clear. However, compared with slow CI animals fast CI animals had lower acute rrCBF values and less visible clot material at 24 hours. The in-vitro experiments showed no clot fragmentation with either fast or slow clot extraction indicating that clot integrity was maintained after ejection from the catheter. Thus, we hypothesize that fast CI caused greater clot compaction and more complete arterial occlusion resulting in less spontaneous recanalization and reperfusion and subsequently larger infarction. This notion is supported by the observation that rrCBF remained stable in fast CI animals whereas rrCBF increased from 60 to 120 minutes in slow CI animals. Though not statistically significant from baseline, the more than twofold rise of this spontaneous increase was similar to that observed after rtPA treatment, which is remarkable in light of our prior observation that laser Doppler flowmetry -based regional blood flow assessment underestimates reperfusion.9 Potentially, our observation period of 60 minutes after rtPA may have been too short to assess maximal reperfusion and future studies may therefore benefit from extended monitoring to address this issue. Additionally, slow CI animals had significantly greater brain swelling as well as infarct volumes showing hemorrhagic transformation, which are surrogate markers of reperfusion mediated injury.22 Yet, without analyzing markers of reperfusion-associated injury this remains speculative.22 Nevertheless, spontaneous reperfusion in slow CI animals could also explain the reduced efficacy of rtPA with this approach. First, attenuation of infarct extent after spontaneous reperfusion may result in a ceiling effect with subsequent thrombolysis having only little additional benefit. Second, hypothesized reperfusion-associated injury may partially offset the benefit derived from rtPA.
The strengths of our study relate to the standardized evaluation of a large number of animals in accordance with the STAIR recommendations (defining inclusion/exclusion criteria a priori, and reporting the reasons for excluding animals from the final data analysis, randomized and blinded experiments).13 Our study is limited due to its retrospective design. While animals were randomized to rtPA versus vehicle within each included study, they were not randomized to the injection technique. Yet, this approach and the exclusion of training animals increased reliability and reproducibility of the injection technique as indicated by highly consistent flow rate curves. Furthermore, absent correlation between the date of surgery and the infarct volume argues against the notion that unmeasured factors resulted in inadvertent model changes over time. Consistent with prior publication15 we included animals dying within 16 to 24 hours after ES, which are excluded from final analysis in other published studies.13 Nevertheless, the associations between injection technique and our key outcome parameters (final infarct volume, brain swelling, hemorrhagic transformation, and response to rtPA) remained when we reanalyzed our data excluding animals dying before the 24-hour time point. These results suggest that inclusion of animals dying within 8 hours of the study end point is appropriate. Clot burden assessment was performed in a subset of animals and at 24 hours after embolism. Thus, immediate rtPA-mediated effects could not be studied, which may also account for the apparent lack of benefit with rtPA on clot burden in light of significantly reduced infarct volumes. Finally, given the severity of the used model with relatively high 24 hours mortality long-term follow-up is not feasible.1 However, it is not expected that longer survival would change the major noted association between injection technique and acute cerebral perfusion and infarct volume.
Despite these limitations, our data clearly show that ES modeling is prone to a significant variation in outcome depending on the embolization approach utilized. More importantly this can result in a significantly different and unexpected response to therapy. As noted initially, this may be of little consequence for a given laboratory if the same approach is used consistently. However, in light of failed translation of bench-to-bedside research and the call for multicenter preclinical phase III-type studies, such potential bias deserves considerable consideration. Imagine the scenario in which Laboratory A uses the fast injection approach and accordingly reports a significant effect with rtPA. Laboratory B uses a slow injection approach and is unable to replicate the results. Yet, rtPA is the established acute stroke therapy with consistent efficacy in multiple stroke models and across laboratories as well as in multiple human trials. Thus, one ‘aberrant' result might be easily dismissed as a technical limitation or chance finding. Yet, if a novel drug had been tested this one negative result might lead to early discontinuation of research into an otherwise promising compound. Even worse, doubts as to the laboratories ability in stroke modeling or the model appropriateness itself might be raised.
For these reasons, cross-laboratory stroke research should include specific recommendations for uniform embolic modeling including considerations as to the approach to surgery, clot creation, and CI technique. For example, centralized surgical training and the use of automated (injection pump) clot delivery methods could help minimize interlaboratory variation. Conversely, reliance on a single clot model is inadvisable because it will not capture the many facets of human ES that are important to consider for achieving robust and broad compound efficacy.
Conclusion
In conclusion, we show that outcome and response to rtPA after ES are highly injection technique dependent, which has significant implications for the design and interpretation of data gained from multicenter preclinical phase III-type studies.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Journal of Cerebral Blood Flow & Metabolism website (http://www.nature.com/jcbfm)
This study was funded by institutional grants. Funding sources played no role in the writing of the manuscript or in the decision to submit the manuscript for publication. Recombinant tissue plasminogen activator was a kind gift of Genentech Inc.
Supplementary Material
References
- Zhu H, Fan X, Yu Z, Liu J, Murata Y, Lu J, et al. Annexin A2 combined with low-dose tPA improves thrombolytic therapy in a rat model of focal embolic stroke. J Cereb Blood Flow Metab. 2012;30:1137–1146. doi: 10.1038/jcbfm.2009.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan X, Lo EH, Wang X. Effects of minocycline plus tissue plasminogen activator combination therapy after focal embolic stroke in type 1 diabetic rats. Stroke. 2013;44:745–752. doi: 10.1161/STROKEAHA.111.000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henninger N, Sicard KM, Fisher M. Spectacular shrinking deficit: insights from multimodal magnetic resonance imaging after embolic middle cerebral artery occlusion in Sprague-Dawley rats. J Cereb Blood Flow Metab. 2007;27:1756–1763. doi: 10.1038/sj.jcbfm.9600477. [DOI] [PubMed] [Google Scholar]
- Lam CK, Yoo T, Hiner B, Liu Z, Grutzendler J. Embolus extravasation is an alternative mechanism for cerebral microvascular recanalization. Nature. 2010;465:478–482. doi: 10.1038/nature09001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger M, Hartig W, Reichenbach A, Bechmann I, Michalski D. Blood-brain barrier breakdown after embolic stroke in rats occurs without ultrastructural evidence for disrupting tight junctions. PLoS ONE. 2013;8:e56419. doi: 10.1371/journal.pone.0056419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strom JO, Ingberg E, Theodorsson A, Theodorsson E. Method parameters' impact on mortality and variability in rat stroke experiments: a meta-analysis. BMC Neurosci. 2013;14:41. doi: 10.1186/1471-2202-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niessen F, Hilger T, Hoehn M, Hossmann KA. Differences in clot preparation determine outcome of recombinant tissue plasminogen activator treatment in experimental thromboembolic stroke. Stroke. 2003;34:2019–2024. doi: 10.1161/01.STR.0000080941.73934.30. [DOI] [PubMed] [Google Scholar]
- Overgaard K, Rasmussen RS, Johansen FF. The site of embolization related to infarct size, oedema and clinical outcome in a rat stroke model - further translational stroke research. Exp Transl Stroke Med. 2010;2:17. doi: 10.1186/2040-7378-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henninger N, Bouley J, Bratane BT, Bastan B, Shea M, Fisher M. Laser Doppler flowmetry predicts occlusion but not tPA-mediated reperfusion success after rat embolic stroke. Exp Neurol. 2009;215:290–297. doi: 10.1016/j.expneurol.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Asahi M, Asahi K, Wang X, Lo EH. Reduction of tissue plasminogen activator-induced hemorrhage and brain injury by free radical spin trapping after embolic focal cerebral ischemia in rats. J Cereb Blood Flow Metab. 2000;20:452–457. doi: 10.1097/00004647-200003000-00002. [DOI] [PubMed] [Google Scholar]
- Dijkhuizen RM, Asahi M, Wu O, Rosen BR, Lo EH. Delayed rt-PA treatment in a rat embolic stroke model: diagnosis and prognosis of ischemic injury and hemorrhagic transformation with magnetic resonance imaging. J Cereb Blood Flow Metab. 2001;21:964–971. doi: 10.1097/00004647-200108000-00009. [DOI] [PubMed] [Google Scholar]
- Tiebosch IA, Crielaard BJ, Bouts MJ, Zwartbol R, Salas-Perdomo A, Lammers T, et al. Combined treatment with recombinant tissue plasminogen activator and dexamethasone phosphate-containing liposomes improves neurological outcome and restricts lesion progression after embolic stroke in rats. J Neurochem. 2012;123 (Suppl 2:65–74. doi: 10.1111/j.1471-4159.2012.07945.x. [DOI] [PubMed] [Google Scholar]
- Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, et al. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke. 2009;40:2244–2250. doi: 10.1161/STROKEAHA.108.541128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirnagl U, Hakim A, Macleod M, Fisher M, Howells D, Alan SM, et al. A concerted appeal for international cooperation in preclinical stroke research. Stroke. 2013;44:1754–1760. doi: 10.1161/STROKEAHA.113.000734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Irie K, Anwer MS, Fisher M. Delayed triphenyltetrazolium chloride staining remains useful for evaluating cerebral infarct volume in a rat stroke model. J Cereb Blood Flow Metab. 1997;17:1132–1135. doi: 10.1097/00004647-199710000-00016. [DOI] [PubMed] [Google Scholar]
- Henninger N, Sicard KM, Schmidt KF, Bardutzky J, Fisher M. Comparison of ischemic lesion evolution in embolic versus mechanical middle cerebral artery occlusion in Sprague Dawley rats using diffusion and perfusion imaging. Stroke. 2006;37:1283–1287. doi: 10.1161/01.STR.0000217223.72193.98. [DOI] [PubMed] [Google Scholar]
- Walvick RP, Bratane BT, Henninger N, Sicard KM, Bouley J, Yu Z, et al. Visualization of clot lysis in a rat embolic stroke model: application to comparative lytic efficacy. Stroke. 2011;42:1110–1115. doi: 10.1161/STROKEAHA.110.602102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chueh JY, Kuhn AL, Puri AS, Wilson SD, Wakhloo AK, Gounis MJ. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: a quantitative in vitro study. Stroke. 2013;44:1396–1401. doi: 10.1161/STROKEAHA.111.670463. [DOI] [PubMed] [Google Scholar]
- Menzies SA, Hoff JT, Betz AL. Middle cerebral artery occlusion in rats: a neurological and pathological evaluation of a reproducible model. Neurosurgery. 1992;31:100–106. doi: 10.1227/00006123-199207000-00014. [DOI] [PubMed] [Google Scholar]
- Gerriets T, Stolz E, Walberer M, Muller C, Kluge A, Bachmann A, et al. Noninvasive quantification of brain edema and the space-occupying effect in rat stroke models using magnetic resonance imaging. Stroke. 2004;35:566–571. doi: 10.1161/01.STR.0000113692.38574.57. [DOI] [PubMed] [Google Scholar]
- Henninger N, Bratane BT, Bastan B, Bouley J, Fisher M. Normobaric hyperoxia and delayed tPA treatment in a rat embolic stroke model. J Cereb Blood Flow Metab. 2009;29:119–129. doi: 10.1038/jcbfm.2008.104. [DOI] [PubMed] [Google Scholar]
- Chen H, Yoshioka H, Kim GS, Jung JE, Okami N, Sakata H, et al. Oxidative stress in ischemic brain damage: mechanisms of cell death and potential molecular targets for neuroprotection. Antioxid Redox Signal. 2011;14:1505–1517. doi: 10.1089/ars.2010.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.