SUMMARY
In recent years the incidence of fungal sinusitis has increased considerably, due both to increased survival of patients at risk and to improved diagnostic equipment. The pathogen responsible in most cases is the Aspergillus in its forms Fumigatus, Flavus and Niger.
The diagnosis is often delayed because the symptoms, characterized by headache, cough, and facial algia, are generally similar to that of chronic bacterial rhinosinusitis. It can be divided into invasive and non-invasive forms based on the clinical evolution and extent of the lesion. We report a case of non-invasive fungal rhinosinusitis in a patient with recurrent sinusitis and pain in the left maxillary region, resistant to antibiotic therapy.
Keywords: mycetoma, aspergillosis, sinuses, fungal sinusitis, aspergillus, odontogenic origins
Introduction
Aspergillus is a fungus belonging to the species of Ascomycetes. Its presence is ubiquitous, generally involving immunocompromised patients but rarely can also affect healthy subjects.
Transmission is primarily through inhalation but in the maxillary sinus can also occur through a iatrogenic communication oro-sinus secondary to a dental procedure, particularly after root canal treatments. In addition to the rhinosinusitis Aspergillus can cause lung infections, heart disease, liver-spleen or meningeal disease. The most common species pathogenic to humans are Aspergillus Fumigatus followed by Aspergillus Niger and Aspergillus Flavus. Hypoxic conditions, as occurs in the paranasal sinuses, promotes pathogenicity (1).
In base to the clinic and the extension can be classified into invasive and non-invasive forms.
We describe the diagnosis and treatment of a case of non-invasive fungal rhinosinusitis in a patient with symptoms of recurrent sinusitis.
Case report
A woman, 54 year old, has come to our attention at the Department of Dentistry of our clinic for a routine visit. In the last 2 years the patient reported a history of recurrent sinusitis and in particular by a week a pain in the left maxillary region, which appeared hyperemic, and associated with difficulty breathing, rhinorrhea and hyposmia. For such motive she had undertaken a treatment with amoxicillina and acid clavulanico for 5 days without resolution of the symptoms.
The evaluation of the oral cavity showed macroscopically nothing of pathological. The ortopantomography (Fig. 1) showed an area of ipodiafania at the level of the left maxillary sinus in the absence of significant erosion of the walls of the maxillary sinus.
Figure 1.
The pre-operative radiography, orthopanoramic, shows the opacification of the left maxillary sinus.
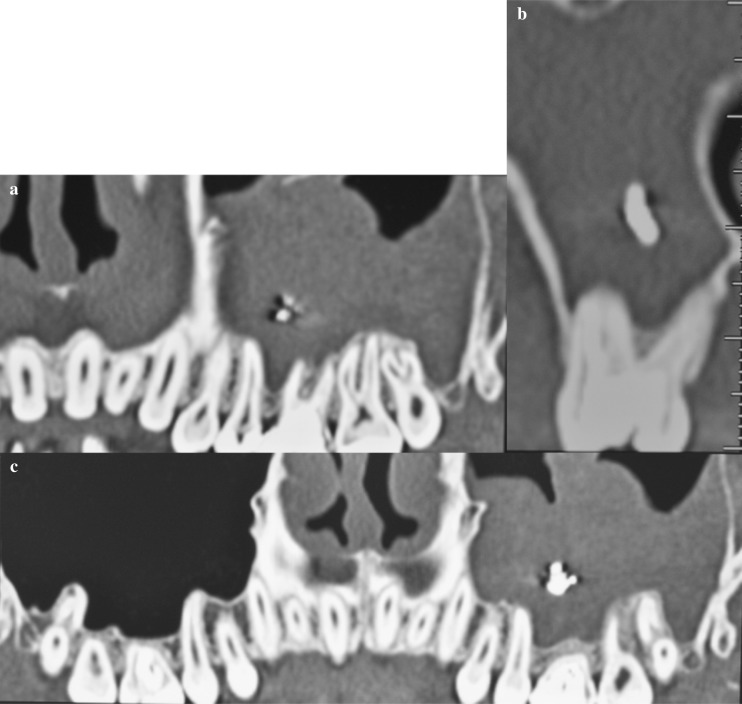
The Dentascan revealed the presence of a hypodense tissue that obliterated almost totally the left maxillary sinus, with hyperdense spots probably of calcic nature (Fig. 2a) and an endodontic treatment of the element 2.6 performed about a month before the occurence of symptoms (Fig. 2b).
Figure 2 a, b, c.
(a) Image TC Dentascan shows a tissue with the density of the soft tissues located at the level of the left maxillary sinus, with formations likely calcic nature. (b) Paraxial image in correspondence of 2.6 in which it is possible to appreciate the root canal and calcification in the context of the maxillary sinus that appears obliterated at that level. (c) Image TC Dentascan shows the normal pneumatization of the right maxillary sinus.
The controlateral maxillary sinus appeared free from pathological changes (Fig. 2c).
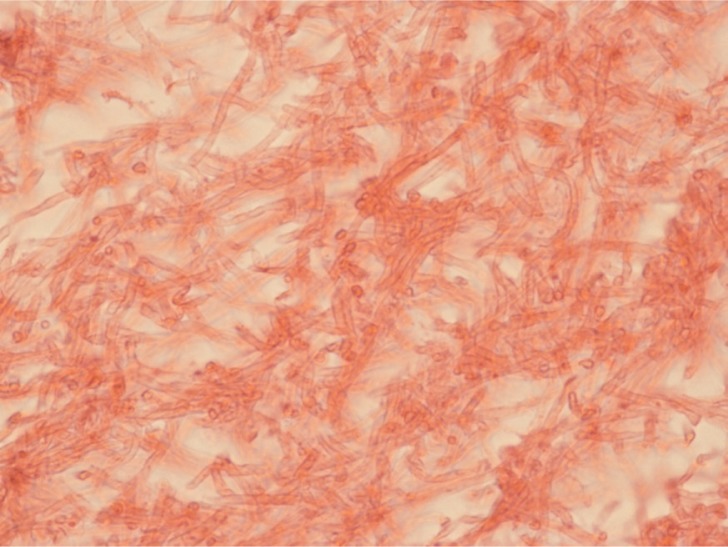
According to the tecnique Caldwell-Luc has been planned and executed surgery. Before surgery were performed blood tests and a chest xray. The postoperative histological examination revealed a polypoid formation composed by an agglomerate of hyphae mycetes (Fig. 3). The next control with instrumental examination Dentascan (Fig. 4) showed complete excision of the lesion described and the restoration of normal pneumatization of the maxillary sinus with a simultaneous resolution of the symptoms.
Figure 3.
The microscopic evaluation shows the presence of hyphae of mycetes.
Figure 4.
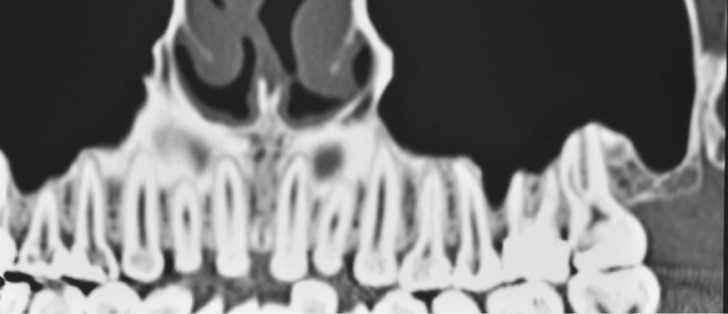
Image TC Dentascan post surgery shows the restoration of normal pneumatization of the left maxillary sinus.
Discussion
In recent years the incidence of fungal rhinosinusitis has grown due to the diffusion of different pathogenic organisms (2), but also of diseases such as diabetes, long-term treatment with steroids and immunosuppressive treatments. Loidolt et al. (3) have reported that approximately 10% of all patients treated surgically for chronic sinusitis are suffering from fungal rhinosinusitis.
Thanks imaging and diagnostic endoscopy was possible to better define the classification, diagnosis and management of these diseases (4). The fungal rhinosinusitis are generally classified into invasive and non-invasive.
The invasive form occurs more frequently in immune-compromised patients and it’s can be classified into granulomatous, invasive chronic and fulminant acute (5), is a very serious condition, which leads to death in 90% of cases because its intracranial complications (6).
The non-invasive form, in turn, it’s subdivided into allergic fungal sinusitis and mycetoma.
The first to describe a case of non-invasive fungal sinusitis was probably Mackenzie in 1894 (7).
The mycetoma can be described as accumulation of non-invasive fungal dense concretions at the level of the paranasal cavities (8), is more often unilateral although rarely can affect more sinus cavities (9), generally occurs in adult subjects, with a mean age of 64 years (10), and has a predominance for the female sex. It differs from allergic fungal sinusitis that affects generally more sinuses. The mycetoma is most often localized at the level of the maxillary sinus, followed by frequency from the sphenoid sinus. However the opacification of the sphenoid sinus is very rare, it is indeed found in 5% of patients with diseases of the paranasal sinuses, of which only 5% is suffering from mycetoma (11).
Patients with mycetoma are almost all immuno-competent, without significant alterations in the levels of immunoglobulin or IgG subclasses (12). Because of its slow evolution, few symptoms, and non-invasiveness, the diagnosis of mycetoma is often late, in fact, only 29% of patients are diagnosed before one year from symptom onset (13). Generally the symptoms includes headache, cough and facial algia and are often similar to symptoms of bacterial chronic rhinosinusitis.
Have been described many risk factors associated with the onset of mycetoma (diabetes mellitus, Wegener’s granulomatosis, asthma, lymphoproliferative diseases, and anatomical variants like the deviation of the nasal septum, etc.), but only the previous root canal treatments have a strong correlation with its development; has been demonstrated that 84% of patients suffering from mycetoma have received previously a endodontic treatment (14).
The examination of the first level for the diagnosis of mycetoma is orthopanoramic radiography (OPT), where you can usually view unilaterally the maxillary sinus opacification. The presence of some focal areas of radiopacity or a single focus radiopaque are respectively present in 50% or 25% of the cases (15) and are strongly suggestive of mycetoma.
Computed tomography (CT) scan is the examination of the second level and remains the test of choice because it can provide information both on characteristics and extent of the lesion both on the choice of the best surgical approach. CT findings associated with the presence of mycetoma are characterized by the presence of an inhomogeneous material at the level of the paranasal sinus involved, which often appears obliterated, with the presence of some material hyperdense spot or a single focus hyperdense. The sensitivity and specificity of CT, in the presence of these findings was calculated respectively in 62% and 99% (16). Although the CT has high sensitivity and specificity is always necessary to rule out other sinus disorders benign or malignant, like mucocele, inverted papilloma, B-cell lymphomas or T-cell, squamous cell carcinoma, adenoid cystic carcinomas, inflammatory myofibroblastic tumors.
The treatment of mycetoma can be both performed through the classic surgery of Caldwell-Luc, as in our case, both using endoscopic techniques. The result is excellent with both techniques and rarely requires a systemic antifungal therapy.
The case we have described emphasizes the importance of careful evaluation of patients presenting obliteration sinuses, especially unilateral, even when they appear asymptomatic.
In particular it is important to emphasize the specialists in dentistry that is critical make an accurate follow-up post-operatively after endodontic treatments, especially when materials such as zinc oxide, titanium, lead, calcium salts, barium and sulfur are used. These materials that allow fungal growth, in particular the Aspergillus, with the consequent formation of mycetoma.
References
- 1.Pasqualotto AC. Differences in pathogenicity and clinical syndromes due to Aspergillus fumigatus and Aspergillus flavus. Med Mycol. 2008:1–10. doi: 10.1080/13693780802247702. [DOI] [PubMed] [Google Scholar]
- 2.Dhong HJ, Lanza DC. Fungal rhinosinusitis. In: Kennedy DW, Bolger WE, Zinreich SJ, editors. Diseases of the sinuses:diagnosis and management. BC Decker Inc; Hamilton: 2001. pp. 179–195. [Google Scholar]
- 3.Loidolt D, Mangge H, Wilders-Trusching M, Beaufort F, Schauenstein K. In vivo and in vitro suppression of lympho-cytefunction in aspergillussinusitis. ArchOtorhinolaryngol. 1989;246:321–3. doi: 10.1007/BF00463585. [DOI] [PubMed] [Google Scholar]
- 4.Grosjean P, Weber R. Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol. 2007 May;264(5):461–70. doi: 10.1007/s00405-007-0281-5. Epub 2007 Mar 15. [DOI] [PubMed] [Google Scholar]
- 5.deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R. A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 1997 Nov;123(11):1181–8. doi: 10.1001/archotol.1997.01900110031005. [DOI] [PubMed] [Google Scholar]
- 6.Segal BH. Aspergillosis. N Engl J Med. 2009 Apr 30;360(18):1870–84. doi: 10.1056/NEJMra0808853. [DOI] [PubMed] [Google Scholar]
- 7.Mackenzie JJ. Preliminary report on aspergillusmycosis of the antrummaxillare. John Hopkins Hosp Bull. 1893;4:9–10. [Google Scholar]
- 8.Ferguson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am. 2000;33:389–398. doi: 10.1016/s0030-6665(00)80013-4. [DOI] [PubMed] [Google Scholar]
- 9.Mitsimponas KT, Walsh S, Collyer J. Bilateral maxillary sinus fungus ball: report of a case. Br J Oral Maxillofac Surg. 2009 Apr;47(3):242. doi: 10.1016/j.bjoms.2008.08.023. Epub 2008 Dec 18. [DOI] [PubMed] [Google Scholar]
- 10.Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Karkas A, Klossek JM. Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology. 2005 Mar;43(1):34–9. [PubMed] [Google Scholar]
- 11.Sethi DS. Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg. 1999 May;120(5):730–6. doi: 10.1053/hn.1999.v120.a89436. [DOI] [PubMed] [Google Scholar]
- 12.Jiang RS, Hsu CY. Serum immunoglobulins and IgG subclass levels in sinus mycetoma. Otolaryngol Head Neck Surg. 2004 May;130(5):563–6. doi: 10.1016/j.otohns.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Barry B, Topeza M, Géhanno P. Aspergillosis of the paranasal sinus and environmental factors. Ann Otolaryngol Chir Cervicofac. 2002;119(3):170–3. [PubMed] [Google Scholar]
- 14.Barry B, Topeza M, Gehanno P. Aspergillosis of the paranasal sinus and environmental factors. Ann Otolaryngol Chir Cervicofac. 2002;119:170–173. [PubMed] [Google Scholar]
- 15.Stammberger H, Jakse R, Beaufort F. Aspergillosis of the paranasal sinuses. X-ray diagnosis, histopathology, and clinical aspects. Ann Otol Rhinol Laryngol. 1984;93:251–256. doi: 10.1177/000348948409300313. [DOI] [PubMed] [Google Scholar]
- 16.Dhong HJ, Jung JY, Park JH. Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol. 2000;14:227–231. doi: 10.2500/105065800779954446. [DOI] [PubMed] [Google Scholar]