Abstract
We report a case of congenital tuberculosis, a rare entity itself; complicated by pulmonary interstitial emphysema, thus leading to air entrapment in lungs and prolonged oxygen dependence. The diagnosis of congenital tuberculosis is often missed and under-reported due to low index of suspicion and less sensitivity of diagnostic tools.
Keywords: Anti-tuberculosis treatment, congenital tuberculosis, pulmonary interstitial emphysema
INTRODUCTION
Congenital tuberculosis is a rare clinical presentation of tuberculosis infection. Even in areas endemic for the disease, congenital tuberculosis has rarely been reported.[1,2,3] We report a 6-week-old female infant who presented with difficulty in breathing since birth. The diagnosis was made based on X-ray chest, which showed milliary mottling of lungs and demonstration of mycobacterium tuberculosis in endometrial biopsy of mother. The case was further complicated by pulmonary interstitial emphysema (PIE), thus causing prolonged oxygen dependence and suspicion in correctness of diagnosis. However, the patient showed clinical improvement and clearing of the pulmonary and splenic tuberculous lesions after anti-tuberculosis treatment. Thus, the case is being reported to increase awareness and index of suspicion of the medical practitioners in endemic areas about congenital tuberculosis. The disease should be considered as a differential diagnosis in infant and neonatal pneumonias and there should be ante-natal screening of high risk mothers.
CASE REPORT
The present case report is about a 6-week-old female child who presented to the Department of Pediatric with difficulty in breathing since birth and progressively worsening cough since 15 days. The child was a preterm baby born at 34 weeks by normal vaginal delivery. There was a history of previous still birth. Prior to being hospitalized, and had received multiple antibiotics.
On further examination, the child was pale and malnourished. She had hepatosplenomegaly. She was tachypneic (Respiratory rate = 98/min), with severe subcostal and intercostal recessions. Respiratory system examination revealed decreased air entry and wide spread coarse crepitations. Her SpO2 was 86% with 100% oxygen inhalation by mask. Thus, she was put on ventilator. Investigations revealed: Hb 7.4 g%, total leukocyte count 10,500. Bacterial cultures of blood, cerebrospinal fluid and urine were negative. Her chest radiograph showed milliary mottling of both lungs. [Figure 1] Ultrasonography showed hepatosplenomegaly with tiny hypoechoic nodules in spleen suggestive of granulomatous pathology. Montaux test was negative. Bronchial washings and gastric washings were negative for acid fast bacilli (AFB).
Figure 1.

Chest radiograph showing milliary mottling
The child's mother was counseled and investigated for tuberculosis. There was no abnormality detected on chest radiograph of mother and her sputum was negative for AFB. However, the diagnosis of genital tuberculosis was confirmed by endometrial biopsy which was positive for AFB. Thus, the child and the mother both were put on anti-tuberculosis treatment.
The child remained on ventilatory support for 6 days and was put on bubble continuous positive airway pressure for the next 10 days. Thereafter, she showed respiratory distress whenever weaned from oxygen. Thus, she was put on oxygen inhalation by nasal prongs and remained oxygen dependent for 2 months. Computed tomography scan report showed multiple diffuse consolidations and thin walled cystic lesions in upper and middle lobes. [Figure 2] The multiple cystic lesions were reported by the radiology department as interstitial pulmonary emphysema/tuberculous bullae; and were the explanation for air entrapment and prolonged oxygen dependence. Thus, the case was a unique case in which congenital tuberculosis, a rare entity itself was complicated by PIE, resulting in prolonged oxygen dependence. The child recovered slowly and was put off the oxygen inhalation by nasal prongs after 2 months. He was thus discharged in a satisfactory condition from the hospital after 2.5 months. On follow-up visit to the outpatient department after 2 weeks, there was marked clinical improvement. Repeat chest radiograph and ultrasonography showed clearing of tuberculous lesions.
Figure 2.
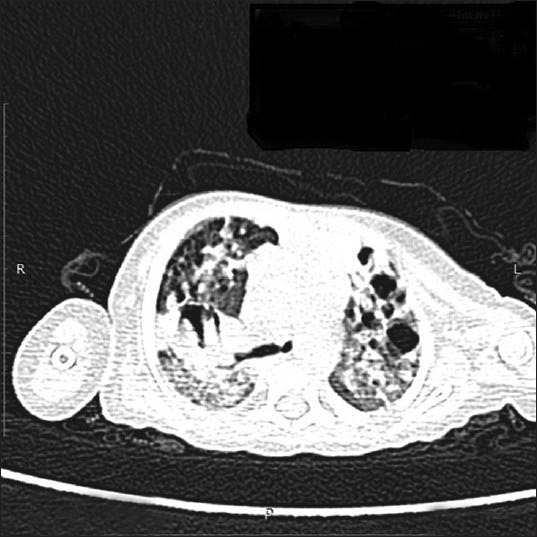
Computed tomography-scan showing pulmonary interstitial emphysema
DISCUSSION
Congenital tuberculosis is defined as tuberculosis occurring in infants caused by infection during the intrauterine life or before complete passage through the birth canal.[1] In spite of high incidence of tuberculosis and its sub-clinical forms in women of reproductive age group in developing countries, congenital tuberculosis is a rare disease with mortality rate of 22%. The probable reason for the rarity may be under-reporting of the disease and lack of good diagnostic tools.[2,3]
Diagnostic criteria for congenital tuberculosis were proposed in 1935 by Beitzke: (i) Tuberculosis firmly established in 1st few days of life, (ii) primary complex in the liver, (iii) lesions presenting in 1st few days of life, when extrauterine infection has been excluded with certainty.[4,5] Cantwell later made a modification in the criteria in 1995 according to which there should be proven tuberculosis lesion in the infant plus one of the following: lesions occurring in the 1st week of life, a primary hepatic complex, maternal genital tract or placental tuberculosis and exclusion of postnatal transmission by thorough investigation of contacts.[3] In this age group, the criteria used to differentiate congenital from post-natally acquired tuberculosis is the mode of acquiring the disease. For a diagnosis of congenital tuberculosis to be established there should be a proof of antenatal transmission while the disease may either be acquired in early postnatal period. Some experts suggest that distinguishing congenital from early post-natally acquired tuberculosis is clinically irrelevant as presenting clinical features, treatment and immediate prognosis are similar.[6,7,8]
Our case qualifies the diagnosis of congenital tuberculosis as she had milliary tuberculosis lesions in lungs with evidence of endometrial biopsy being positive for AFB in the mother. However, the case was unique due to prolonged oxygen requirement for 2.5 months due to PIE in spite of starting anti-tuberculosis treatment within first 3 days of admission. PIE is a serious complication of mechanical ventilation, associated with prematurity and respiratory distress syndrome. Progression of PIE is a life-threatening condition.[9] Barotrauma of mechanical ventilation, causes rupture of the alveolar space at its junction with less expandable fluid-rich perivascular connective tissue. The air leaks into the perivascular sheath and dissects it, giving rise to PIE, pneumothorax and pneumo-mediastinum.[10] In most of the cases, treatment for PIE is conservative including high frequency oscillation ventilation, lateral decubitus positioning. In our case, the bullous tuberculous lung tissue was complicated by further air trapping due to PIE, thus leading to prolonged oxygen dependence.
CONCLUSION
Based on the above case study, it can be concluded that congenital tuberculosis should be considered as a differential diagnosis in neonatal and infant pneumonias. The medical practitioners should have high index of suspicion for the disease especially in neonates born to high risk mothers in endemic areas. Prolonged oxygen requirement in such cases may be due to ventilation inflicted interstitial emphysema worsened by bullous disruption of tuberculosis. The case report also signifies the need for maternal screening for tuberculosis in endemic areas.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hudson FP. Clinical aspects of congenital tuberculosis. Arch Dis Child. 1956;31:136–9. doi: 10.1136/adc.31.156.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abalain ML, Petsaris O, Héry-Arnaud G, Marcorelles P, Couturaud F, Dobrzynski M, et al. Fatal congenital tuberculosis due to a Beijing strain in a premature neonate. J Med Microbiol. 2010;59:733–5. doi: 10.1099/jmm.0.016881-0. [DOI] [PubMed] [Google Scholar]
- 3.Cantwell MF, Shehab ZM, Costello AM, Sands L, Green WF, Ewing EP, Jr, et al. Brief report: Congenital tuberculosis. N Engl J Med. 1994;330:1051–4. doi: 10.1056/NEJM199404143301505. [DOI] [PubMed] [Google Scholar]
- 4.Balasubramanian S, Shivram R, Padmasani LN, Nagaraju Congenital tuberculosis. Indian J Pediatr. 1999;66:148–50. doi: 10.1007/BF02752376. [DOI] [PubMed] [Google Scholar]
- 5.Sri SS. Child Textbook of Pulmonary and Extra Pulmonary Tuberculosis. 2nd ed. New Delhi: Mehta Publishers; 1995. Congenital tuberculosis; p. 205. [Google Scholar]
- 6.Armstrong L, Garay SM. Tuberculosis and pregnancy and tuberculous mastitis. In: Rom WN, Garay SM, editors. Boston: Little Brown and Company; 1996. pp. 689–98. [Google Scholar]
- 7.Hageman J, Shulman S, Schreiber M, Luck S, Yogev R. Congenital tuberculosis: Critical reappraisal of clinical findings and diagnostic procedures. Pediatrics. 1980;66:980–4. [PubMed] [Google Scholar]
- 8.Raghu MB, Patel YS, Mangrola UG, Bhat GJ. Tuberculosis in early infancy. Cent Afr J Med. 1986;32:60–4. [PubMed] [Google Scholar]
- 9.Dördelmann M, Schirg E, Poets CF, Ure B, Glüer S, Bohnhorst B. Therapeutic lung puncture for diffuse unilateral pulmonary interstitial emphysema in preterm infants. Eur J Pediatr Surg. 2008;18:233–6. doi: 10.1055/s-2008-1038498. [DOI] [PubMed] [Google Scholar]
- 10.Oh MH, Kim MY, Shim WS, Oh SS, Shin BK, Cho SJ, et al. A case of localized persistent interstitial pulmonary emphysema. J Korean Med Sci. 2001;16:225–8. doi: 10.3346/jkms.2001.16.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]