Abstract
Scrub typhus is endemic in large parts of India and can cause multi-organ failure and death. Acute pancreatitis as a complication is very rare and is potentially fatal. This case series describes seven adult patients who presented with an acute febrile illness and were diagnosed to have scrub typhus with acute pancreatitis. The mean age of the seven patients with acute pancreatitis was 49.4 years, and mean duration of fever prior to presentation was 7.7 days. All seven patients had abdominal pain, and three had a pathognomonic eschar. The mean serum lipase level was 1,509 U/L (normal value: <190 U/L) and the mean serum amylase level was 434 U/L (normal value: <200 U/L). Six patients had evidence of multi-organ dysfunction. Hematological and respiratory system dysfunction was seen in five patients, hepatic and renal dysfunction in four, and central nervous system dysfunction in three patients. Three patients who had ≥4 organs involved, died (mortality rate: 42.8%). Our case series shows that pancreatitis in scrub typhus is an extremely rare complication and when present, is associated with increased mortality (42.8%). Physicians may be familiar with the various complications of scrub typhus but less so with acute pancreatitis and hence may be underdiagnosed.
Keywords: Complication, Pancreatitis, Scrub typhus
INTRODUCTION
Scrub typhus is a mite-borne illness caused by a Gram-negative obligate intracellular bacterium called Orientia tsutsugamushi and is endemic in many areas in India, especially southern India. It usually presents as an acute undifferentiated febrile illness and may involve multiple organs. Severe complications include acute respiratory distress syndrome (ARDS), hepatitis, renal failure, meningoencephalitis, and myocarditis with shock in a varying proportion of patients. Involvement of the abdomen is well documented, with nausea, vomiting, and abdominal pain being common symptoms. Abdominal pain is seen in about 22% of the patients with scrub typhus and often requires surgical exploration.[1] Some unusual presentations of scrub typhus with abdominal pain include acute acalculous cholecystitis, duodenal ulcer perforation, peritonitis, and gastric ulceration.[2] Direct involvement of the pancreas with O. tsutsugamushi has been conclusively proven in autopsy studies, but clinical description of the same is scant.[3] We describe seven patients who were diagnosed to have scrub typhus with acute pancreatitis.
CASE REPORT
Seven patients admitted between 2007 and 2012 to the Christian Medical College, Vellore with a diagnosis of scrub typhus and acute pancreatitis are described. Scrub typhus was confirmed by scrub typhus immunoglobulin M enzyme-linked immunosorbent assay (IgMELISA)(InBios International, Inc., Seattle, USA) positivity. Other endemic infections like malaria, dengue fever, and leptospirosis were ruled out by appropriate serological testing. The diagnosis of acute pancreatitis was made on the basis of at least two of the following criteria: acute onset of persistent severe abdominal pain, elevation in serum lipase or amylase to three times greater than the upper limit of normal and characteristic findings of acute pancreatitis on radiographic imaging. Dysfunction of different organs was defined by the following criteria:[4]
Hematological dysfunction: Thrombocytopenia (platelets less than 100,000/cu mm), leukopenia (total white cell counts less than 4000/cumm), leukocytosis (white cell counts more 11,000/cumm) or evidence of coagulopathy (prothrombin time more than 12.5 seconds and activated partial thromboplastin time more than 36.7 seconds);
Respiratory dysfunction: ratio of partial pressure arterial oxygen and fraction of inspired oxygen (PaO2/FiO2 ratio)<200 or need for ventilator assistance;
Renal dysfunction: serum creatinine>2 mg/dL or need for dialysis;
Cardiovascular dysfunction: Hypotension or need for inotropic or vasopressor support;
Liver dysfunction: Serum bilirubin >2 mg/dL or threefold elevation of liver enzymes;
Neurologic dysfunction: Alteration in the level of consciousness.
RESULTS
This case series describes seven cases with proven scrub typhus complicated by acute pancreatitis. Patients’ profile is shown in Table 1. The mean age of the subjects was 49.4 years, and six of them were males. None of them had a history of significant alcohol consumption. Three subjects had a pathognomonic eschar. The mean duration of fever prior to presentation was 7.7 days. All subjects had a history of abdominal pain, which was central and did not improve with proton-pump inhibitors. Thrombocytopenia (platelet count <100 × 103/L) was seen in five subjects, but only one case [case7] had significant gastrointestinal bleeding. Pancreatic enzymes were significantly elevated to three times more than the upper limit of normal in all subjects. Ultrasonography evidence of acute pancreatitis (bulky pancreas) was seen in two subjects, whereas minimal left-sided pleural effusion was seen in five cases. Other causes of pancreatitis like gallstones and hypercalcemia were ruled out. Evidence of multiorgan dysfunction syndrome (MODS) with >2 organ involvement was seen in all cases except case one [Table 2]. Five subjects had both hematological and respiratory system dysfunction, whereas four had both hepatic and renal dysfunction. Central nervous system (CNS) dysfunction was observed only in three cases. Acute pancreatitis was managed conservatively with nil oral intake and opioid painkillers.
Table 1.
Clinical features and laboratory investigations
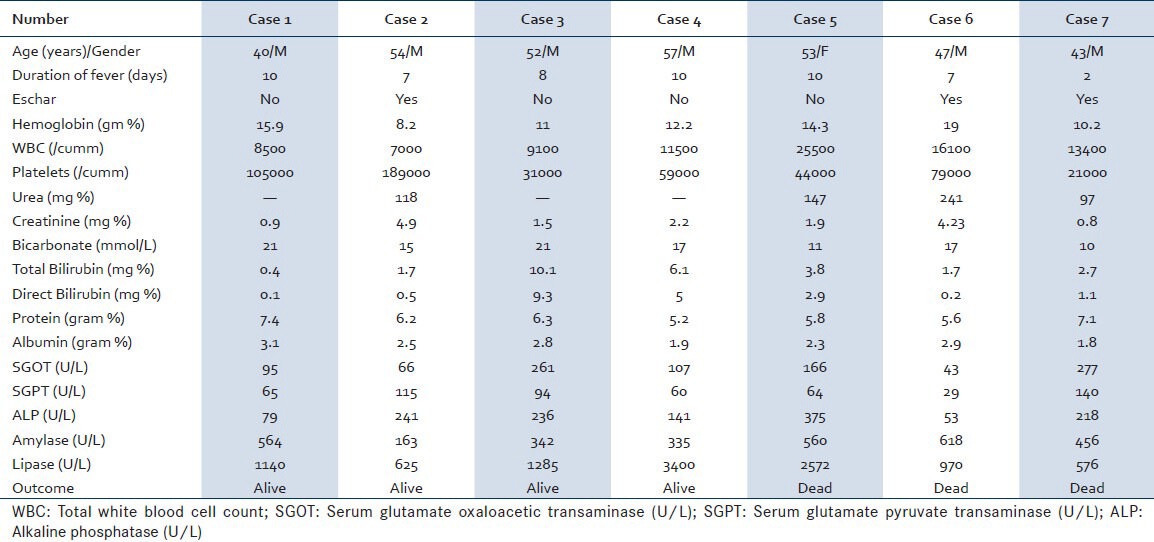
Table 2.
Organ dysfunction and outcome
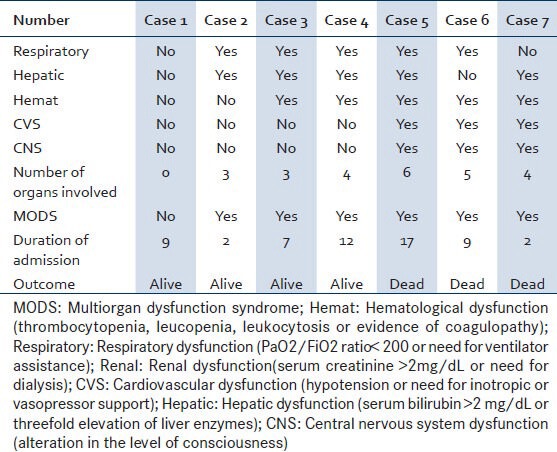
Three patients (cases 5, 6, and 7) who required vasoactive agents for hypotension also had involvement of ≥4 organs dysfunction and eventually died. Case 5 had severe scrub typhus with multiorgan failure. During the second week of illness, she developed secondary pulmonary infection with Acinetobacter baumannii and died of septic shock 17 days after hospitalization. Case 6 developed pancreatic ascites as was evidenced by high levels of ascitic fluid amylase (7,550 U/L) and lipase (3,300 U/L) that led to secondary infection with Candida tropicalis and his subsequent death on the ninth day of admission. Case 7 had severe scrub typhus with multiple-organ failure and succumbed to the illness within 48 hours of admission.
DISCUSSION
Scrub typhus affects almost a million people every year and mainly occurs in populations that encounter scrub vegetation as part of their occupation or daily life. It has been found to account for up to 50% of undifferentiated febrile illness that occur in some parts of India. It can range from a self-limiting disease, if not promptly diagnosed and appropriately treated, to a fatal illness due to multiorgan dysfunction.[1] Mortality in scrub typhus varies from 12% to 50%.[1] A large prospective study showed the following mortality rates with complications in scrub typhus: ARDS (29.7%), renal failure (29.7%), altered sensorium (24.4%), and shock (38.4%).[1] Our case series shows a much higher mortality rate (42.8%) among those with acute pancreatitis complicating scrub typhus. It is therefore important to watch out for this complication especially in those presenting with acute severe abdominal pain.
The diagnosis of pancreatitis is based on elevated pancreatic enzymes and imaging. Serum lipase has a higher sensitivity and specificity up to 82%-100%. In addition, lipase levels peak early and last longer, returning to normal only after about six to eight days. Delineation of the body and tail may be poor with ultrasound, as also the presence of bowel gas may preclude evaluation of pancreas and the bile duct. Despite these limitations, an ultrasound may still be performed as an initial imaging modality as it is a quick and easy-to-perform test on hemodynamically unstable patients in view of transportation issues. Computer tomography (CT) scanning, although better at delineating pathology of acute pancreatitis, may not be enough in itself, and hence patients may still require ultrasonography to rule out gallstone disease. Magnetic resonance imaging has higher sensitivity for diagnosing pancreatitis than CT scan and it can characterize the pancreatic and bile ducts and complications of pancreatitis better. However, it has a longer scanning time, which makes it difficult to use frequently in sick patients.
Five of our patients had minimal left-sided pleural effusion and one had bilateral pleural effusions. Pleural effusion, which is seen in 4%-17% of patients with acute pancreatitis is considered as a marker of severe pancreatitis and is associated with a mortality rate of 20%-30%. Pleural effusions are usually small, occasionally bloody, and are characterized by high amylase (>1000 U/L) and high protein levels (>3 g/dL).
Infectious causes of acute pancreatitis include mumps, Coxsackievirus, Cytomegalovirus, Mycoplasma, Legionella, Salmonella, and Aspergillus. Pancreatic involvement with scrub typhus is extremely rare, and only four such cases have been reported till date. Sun et al. reported a 75-year-old man with scrub typhus with acute pancreatitis and pancreatic abscess.[5] A 40-year-old lady with scrub typhus and dengue coinfection and a 41-year-old man with leptospirosis and scrub typhus coinfection also were reported to have pancreatitis. Nayyar et al. reported pancreatitis in a patient from South India who had scrub typhus and dengue coinfection.[6] The pathogenesis of acute pancreatitis in scrub typhus is not well known but is probably vasculitis and perivasculitis of the small blood vessels due to widespread endothelial cell invasion by the causative organism.
CONCLUSION
Our case series shows that pancreatitis in scrub typhus is an extremely rare complication and when present, is associated with increased mortality rates (42.8%). As this is not a well-known complication of scrub typhus, clinicians may not consider this possibility, thus leading to underdiagnosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Chrispal A, Boorugu H, Gopinath KG, Prakash JAJ, Chandy S, Abraham OC, et al. Scrub typhus: An unrecognized threat in South India-clinical profile and predictors of mortality. Trop Doct. 2010;40:129–33. doi: 10.1258/td.2010.090452. [DOI] [PubMed] [Google Scholar]
- 2.Yang CH, Young TG, Peng MY, Hsu GJ. Unusual presentation of acute abdomen in scrub typhus: A report of two cases. Zhonghua Yi XueZaZhi (Taipei) 1995;55:401–4. [PubMed] [Google Scholar]
- 3.Moron CG, Popov VL, Feng HM, Wear D, Walker DH. Identification of the Target Cells of Orientia tsutsugamushi in Human Cases of Scrub Typhus. Mod Pathol. 2001;14:752–9. doi: 10.1038/modpathol.3880385. [DOI] [PubMed] [Google Scholar]
- 4.Balk RA. Pathogenesis and management of mu ltiple organ dysfunction or failure in severe sepsis and septic shock. Crit Care Clin. 2000;16:337–52. doi: 10.1016/s0749-0704(05)70113-5. [DOI] [PubMed] [Google Scholar]
- 5.Yi SY, Tae JH. Pancreatic abscess following scrub typhus associated withmultiorgan failure. World J Gastroenterol. 2007;13:3523–5. doi: 10.3748/wjg.v13.i25.3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iqbal N, Viswanathan S, Remalayam B, Muthu V, George T. Pancreatitis and MODS due to scrub typhus and dengue co-infection. Trop Med Health. 2012;40:19–21. doi: 10.2149/tmh.2012-07. [DOI] [PMC free article] [PubMed] [Google Scholar]


