Abstract
Prehospital airway management is a key component of emergency responders and remains an important task of Emergency Medical Service (EMS) systems worldwide. The most advanced airway management techniques involving placement of oropharyngeal airways such as the Laryngeal Mask Airway or endotracheal tube. Endotracheal tube placement success is a common measure of out-of-hospital airway management quality. Regional variation in regard to training, education, and procedural exposure may be the major contributor to the findings in success and patient outcome. In studies demonstrating poor outcomes related to prehospital-attempted endotracheal intubation (ETI), both training and skill level of the provider are usually often low. Research supports a relationship between the number of intubation experiences and ETI success. National standards for certification of emergency medicine provider are in general too low to guarantee good success rate in emergency airway management by paramedics and physicians. Some paramedic training programs require more intense airway training above the national standard and some EMS systems in Europe staff their system with anesthesia providers instead. ETI remains the cornerstone of definitive prehospital airway management, However, ETI is not without risk and outcomes data remains controversial. Many systems may benefit from more input and guidance by the anesthesia department, which have higher volumes of airway management procedures and extensive training and experience not just with training of airway management but also with different airway management techniques and adjuncts.
Keywords: Airway, anesthesiology, emergency, management, prehospital
INTRODUCTION
Prehospital airway management is a key component of provider training and remains an important task of Emergency Medical Service (EMS) systems worldwide. The development of different prehospital airway management techniques and equipment mirrors the evolution of prehospital triage and emergency care. Basic airway skills included in Basic Life Support (BLS) training such as mouth-to-mouth-ventilation, mouth-to-nose-ventilation or the use of simple face mask devices have been taught to the general population for decades.
More intermediate airway management techniques including bag-mask ventilation (BMV) and placement of oral or nasal airway devices are utilized by Emergency Medical Technicians (EMTs). The most advanced airway management techniques involving placement of oropharyngeal airways such as the Laryngeal Mask Airway (LMA), Combitube®, King LT® tube, and others tend to be reserved for the more advanced level of prehospital provider such as paramedics or physicians. Similarly, endotracheal intubation (ETI), airway rescue device placement, capnography, and cricothyroidotomy remain the responsibility of either paramedics with advanced airway training or physicians. In recent years, advances in video-assisted laryngoscopy (VAL) and the refinement of oropharyngeal airways have shown the potential to change or add to the traditional approach of prehospital airway management.
Many European countries operate with a physician staffed EMS in which a physician is sent to life-threatening emergencies. The majority of EMS systems in the United States utilize nonphysician providers to manage the prehospital airway. One important distinction between the two EMS models is that EMT scope of practice within the Franco–German model is significantly limited in comparison to the American model of prehospital care. Most procedures are only performed by physicians unless there is an extraordinary circumstance where no physician is readily available to treat the patient at the scene. Within the European model, physician EMS providers perform the required procedures. Both system approaches rely on good education, high quality of training, and recertification standards to ensure advanced EMS providers are equipped with the skills necessary to avoid life-threatening complications from loss of airway or respiratory problems.
Airway management by first responder (lay person)
Lay people, with or without BLS training, are often the initial care providers at the scene of an emergency. The often encountered reluctance of performing mouth-to-mouth ventilation and the potential infection risk have been viewed as barriers to the initial care of nonbreathing patients. Observational studies have shown that “panic” was stated by lay people as the most common barrier to providing cardiopulmonary resuscitation (CPR) to a patient.[1] A simpler model employing “hands-only” (chest compression without conventional rescue breaths) was thought to potentially decrease some barriers to first responder care.[2] In addition, in an earlier study by Berg et al., assisted ventilation with CPR in a swine animal model did not improve outcome over hands-only CPR.[3] Observational studies in adults undergoing bystander CPR demonstrated similar survival rates among individuals receiving hands-only versus conventional CPR with rescue breaths.[4,5,6] Rationale for these observations include delay in hypoxemia due to adequate oxygenation at time of cardiovascular collapse, passive gas exchange with chest compressions, and agonal breathing patterns that may be present in a patient undergoing CPR after cardiac arrest. However, an acceptable length of time for hands-only CPR has not yet been established and most patients undergoing CPR will eventually receive advanced airway management, such as endotracheal tube (ETT) placement, by a medical provider during the process.
The 2010 American Heart Association (AHA) guidelines for CPR in adult patients now emphasize in the following order circulation, airway, and breathing with a much higher emphasis on chest compressions, rather than ventilation. This is in contrast to the pediatric population where conventional CPR with assisted ventilation demonstrates improved outcomes versus hands-only CPR.[7]
Airway management by EMR/EMT
At the federal level, the National Highway Traffic Safety Administration developed a minimum content and hour requirement for Emergency Medical Responder (EMR)/EMT training (National Standard Curriculum) that all states must meet.[8] Additionally, the National Highway Traffic Safety Administration developed a National EMS Scope of Practice Model which details the minimum psychomotor skill set that each care provider is expected to possess.[9]
However, current scope of practice is regulated at the state level and can vary significantly between states or even within varying regions of the same state. The National Registry of Emergency Medical Technicians (NREMT) developed certification tests for each emergency responder level, and most states currently use the NREMT guidelines as part of their licensure procedure. A recertification process exists including requirement for continuing education hours and courses.
The EMR works alongside other EMSs and healthcare professionals as part of the emergency care team. Functioning as part of a tiered response system, EMRs perform noninvasive interventions to reduce morbidity and mortality associated with out-of-hospital medical and trauma emergencies. The minimum psychomotor skills provided by EMRs includes insertion of airway adjuncts intended to go into the oropharynx, use of bag-valve-mask, suctioning of upper airway, and use of supplemental oxygen.
EMTs are subdivided into several classes including EMT-B (Basic), EMT-I (Intermediate), and AEMT (Advanced). The intermediate class of EMT is further subdivided into the 1985 and 1999 grouping. As a rule, minimum psychomotor skills and typical procedures in respect to airway management include all those provided by an EMR as well as insertion of airway adjuncts into the nasopharynx and use of additional positive pressure ventilation devices.
The Advanced EMT or AEMT is capable of providing all interventions that an EMR, EMT-B, and EMT-I can provide with additional minimum psychomotor airway skills including insertion of airways that are not intended to be placed into the trachea and tracheobronchial suctioning of an already intubated patient.[9]
Airway management by paramedics/physicians
According to the NREMT guidelines posted on NREMT.org, qualifications to become a paramedic includes age 18 years or older, current national or state certification at the EMT-B level or above, successful completion of a state approved EMT-paramedic/paramedic course or refresher course that meets or exceeds the U.S. Department of Transportation Paramedic National Standard Curriculum within the past 2 years, and verification of current CPR credentialing.
The U.S. Department of Transportation (DOT) pilot testing of the curriculum demonstrated that an average program with average students will achieve average results after somewhere between 1000 and 1200 hours of instruction.[8] Paramedic credentialing through the NREMT requires successful passage of both a cognitive and psychomotor examination. The cognitive examination is a computer-based examination encompassing airway management, ventilation, oxygenation, trauma, cardiology, medical, and EMS operations. The examination content involves both adult and pediatric patients. Psychomotor testing includes patient assessment in a trauma situation, ventilatory management, cardiac management skills, IV and medication skills, an oral case examination portion, pediatric skills, and other skills including spine immobilization. Airway and ventilatory assessment includes use of bag-valve-mask, supraglottic airway (SGA) placement, and ETI.
The physician-staffed European EMS system (Franco–German model) utilizes a multi-tier system composed of basic EMS providers with similar training to an EMT as well as intermediate providers with skills and training similar to that of an AEMT or paramedic. The last tier is physician staffed ground vehicles or helicopters. The physician is activated either by a dispatch center or one of the first arriving care providers at the scene. These physicians need to fulfill regional and national requirements to be qualified to participate in the EMS system. These requirements are not standardized but usually include a minimum of 2 years of completed residency training and procedural experience with intubation, central line placement, and chest tube placement.
Techniques for airway management prior to hospital arrival
The decision about whether an airway intervention is required is critical to patient care and survival. Depending on the responder's level of training, a quick assessment and decision is made regarding what if any intervention is required. Airway management is of course limited by scope of practice, education of the practitioner, and available resources.
Spontaneous breathing
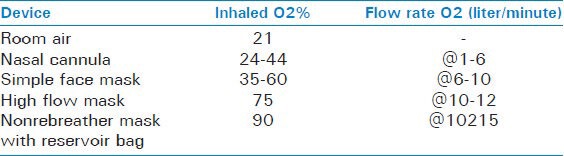
Spontaneous breathing remains a viable option for airway management when a provider is confronted with an awake patient possessing a patent airway. Assistance for spontaneous ventilation can be performed through the placement of a nasal or oral airway. Oxygenation can be improved with the supplementation of oxygen via nasal cannula, simple face mask, or nonrebreather face mask [Table 1]. Unfortunately, the maximally achieved FiO2 is often over estimated by care providers and hypoventilation resulting in hypercapnia cannot be normalized with increase oxygen supply.
Table 1.
Maximum oxygen FiO2 with different oxygen delivery devices
Some EMS systems recently introduced continuous positive airway pressure (CPAP) as an assist modality for spontaneous breathing patients. To apply CPAP the provider fixes a tight fitting mask to the patient allowing CPAP during spontaneous ventilation. One study examined the effectiveness of prehospital CPAP in the management of acute pulmonary edema and found decreased intubation rates and a mortality benefit in this particular patient population.[10] However, this modality requires the cooperation of the patient and can only be performed in patients with intact mental status who are able to follow instructions. Another disadvantage is the amount of time required to apply and initiate this form of assisted ventilation. As a temporizing measure, CPAP and BiPAP may prove beneficial, however, it is crucial for the prehospital care provider to recognize why inadequate ventilation may be occurring and definitively secure a patient's airway if respiratory collapse appears imminent.
Emergency conditions can greatly limit the safety of allowing a patient to continue spontaneous ventilation. This is especially true in the trauma situation where impending airway or cardiovascular collapse may necessitate early and aggressive airway management.
Mouth-to-Mouth ventilation
Mouth-to-mouth or mouth-to-nose ventilation is still a recognized management technique for prehospital airway management. However, this modality has fallen out of favor recently with the increasing support of “hands-only” CPR. Proper face masks should be utilized if they are available.
Bag-mask-ventilation
BMV remains a standard initial approach to airway management in the prehospital and hospital settings. Proper preoxygenation prior to intubation provides patients with improved oxygenation and increases time to hypoxemia. BMV can be applied as a sole practitioner or in conjunction with a second care provider. BMV can also occur during spontaneous respirations as a pressure support method for patients with depressed tidal volumes and inadequate ventilation. This is similar to the use of CPAP or BiPAP to assist patients who are spontaneously breathing but are not adequately oxygenating or ventilating.
Oropharyngeal and nasopharyngeal airways
Used as an adjunct device for spontaneous or assisted ventilation, oropharyngeal and nasopharyngeal airways are frequently utilized by prehospital care providers to improve oxygenation and ventilation. These devices are frequently used to temporize until a more definitive airway is obtained, and there are several circumstances that prohibit their placement (severe head or facial injuries).
Supraglottic airway devices
Supraglottic airway (SGA) device placement requires less training than ETI.[11] As a procedure, it is certainly less invasive than ETI. For care providers not sufficiently trained in ETI these devices can offer better ventilation during transport than BMV alone. In addition, SGAs can be used as a backup tool for failed intubation in accordance with the difficult airway algorithm by the American Society of Anesthesiology (ASA).[12]
Some of the more common SGAs include the LMA, laryngeal tube, and Combitube. Initial evaluations of SGA devices as an alternative to ETI for the prehospital provider were promising.[13] Unfortunately, unexpected complications such as aspiration, soft tissue injury, airway injury, hypoxemia, hypercarbia, and vocal cord injury have been associated with these devices.
Endotracheal intubation
The gold standard for definitive airway management in the prehospital setting remains ETI. A cuffed tube in the trachea allows for positive pressure ventilation, positive end-expiratory pressure (PEEP), positive pressure recruitment maneuvers, and protection from aspiration. Multiple studies support the model that proficient ETI requires rigorous training and higher numbers of ETI experience.[14]
Providers must know how to detect proper tube placement using physical examination and capnography and also be equipped to handle failed intubations. Proficiency with the gum elastic bougie or intubating LMAs can help providers rescue difficult airways. Additionally, prehospital airway specialists must be capable of performing a cricothyroidotomy when other methods of ventilation are either unsafe or impossible.
Rapid sequence intubation versus no-medication intubation
Pharmacologic muscle paralysis relaxes the pharyngeal and facial musculature and results in improved intubation conditions. Rapid sequence intubation (RSI) techniques incorporate pharmacologic muscle relaxation and are utilized by anesthesiologists and emergency medicine physicians. However, one drawback to these techniques is the elimination of a patient's ability to breathe spontaneously if the intubation fails. Yet many providers conversely argue that optimal intubating conditions should be achieved prior to attempted intubation in the prehospital setting. The reason for this is that prehospital airway intervention is frequently time sensitive due to trauma, cardiac arrest, hypoxemia, or aspiration risk.
Outcomes and discussion
While there is little debate regarding the importance of airway management, continued debate exists over prehospital ETI. Many existing publications to date support the notion that prehospital ETI correlates with higher incidence of mortality.[15]
One prospective study by Cobas et al. showed a 31% incidence of failed prehospital intubation (PHI), but found no difference in mortality between patients who were properly intubated and those who were not.[16] This study suggested the use of bag-valve-mask as an adequate alternative method of airway management for critically ill trauma patients. When compared with BMV, one recent study demonstrated advanced airway management to be independently associated with decreased odds of neurologically favorable survival.[17]
Still other studies would suggest that ETI in the field is a vital component to patient survival. Miraflor et al. demonstrated that the timing of intubation of initially stable, moderately injured trauma patients affects mortality. Early intubation was associated with an 85% mortality risk reduction in this particular patient population.[18]
An unrelated outcomes analysis from a major trauma registry demonstrated an association between intubation and mortality among individual trauma patients with a Glasgow Coma Scale (GCS) of 8 or less. However, the sub-analysis suggested that sites with increased intubation attempts had instead a decreased mortality rate. The EMS system (Medic One) in King County, WA utilizes prehospital ETI extensively and shows improved survival rates when compared with systems participating in this study with fewer PHIs.[19]
A clinical outcomes paper from Resuscitation combined data from 16 U.S. states and examined out of hospital airway management and outcomes. The data was pooled from the 2008 National Emergency Medical Services Information System (NEMSIS) Public Release Data Set. With 4,383,768 EMS activations, 10,356 ETIs were performed, 2246 alternate airways were placed, and 88 cricothyroidotomies were performed. Overall ETI success rate was 77%. Regional variability demonstrated the highest ETI failure rate to exist in the southern USA.[20]
A physician staffed EMS system in Germany demonstrated a significantly higher number of patients being discharged after suffering cardiac arrest (17.1%) than a paramedic staffed system (3.9%).[21] Some attribute this difference in outcome to the fact that physicians in the German EMS system possess superior airway management skills.[22] In contrast to that study, a study by Nichol et al. demonstrated that Seattle, WA paramedic treated out-of-hospital cardiac arrest (OHCA) patients survived to discharge 16.3% of the time and therefore better than the other participating systems.[23] However, it is important to note that there was great regional variability in survival to discharge data between the systems. The King County EMS system (Medic One) does maintain a rigorous airway training program with intubation success rates of over 98%.[24] These studies support the notion that superior airway management has a strong correlation with training efforts and ultimately with patient outcome. In regard to performance and outcome, these studies also suggest that systems with well trained paramedics can compete in performance and outcome with physician staffed EMS models.
While data surrounding out-of-hospital ETI and survival outcome remains conflicting, what is clear is that the current level of training of U.S. paramedics and European EMS physicians is not sufficient to guarantee a universally acceptable intubation success rate. In Europe, many procedure requirements are decreased locally to ensure recruitment of an adequate number of physicians. For example, some German states require only a minimum of 25 intubations to qualify as an EMS physician provider.[25] This is far less than the approximate 200 intubations that Bernhard et al. demonstrated to be necessary to increase intubation success from 82% to 92%.[26] At present, U.S. paramedic trainees require just five ETI attempts for the national paramedic certification. Poor training and lack of experience may explain why many paramedic or physician staffed systems demonstrate poor patient outcomes, low success rates, or high numbers of complications with ETI.
Some have suggested that SGA devices should replace ETI in the prehospital setting. Sunde et al. performed a retrospective analysis of 347 adult OHCA patients in Norway. The success rate of laryngeal tube insertion was 85.3% with a first pass success rate of 74.4%. Air leakage (17.6%) and aspiration (12.7%) were reported complications.[27] A cadaveric study by Scmidbauer et al. demonstrated that inspiratory pressures of 40 and 60 mbar led to esophageal insufflation in all studied devices (LMA-Supreme™, LMA-Proseal™, laryngeal tubes LTS-D and LTS II, Combitube®, and i-gel®).[28] Insufflation pressures during out-of-hospital ventilation are difficult to monitor, and unintended gastric and esophageal insufflation may lead to aspiration. Additionally, there are case reports of Combitube® use contributing to aspiration, injury, and vocal cord damage.[29] A swine cardiac arrest model demonstrated compression of the internal and external carotid vessels with SGA device placement (King LTS-D®, LMA Flexible®, Combitube®).[30] A secondary analysis of data obtained from a multicenter study of patients suffering from OHCA showed that ETI was associated with improved outcomes over SGA device insertion.[31] However, confounding variables in this analysis may impact the applicability of these findings. Additionally, other studies have shown no difference in neurologically favorable outcomes between patients treated with SGA devices and ETI in OHCA.[32] While SGA devices will continue to remain a key component of prehospital airway management, at present they have not replaced ETI.
Special considerations
Trauma victims are an interesting subgroup of the prehospital patient. These individuals are frequently hypovolemic from the traumatic insult. For example, bilateral femur fractures can result in blood loss of three liters or more, and pelvic fractures can result in life-threatening hemorrhage within minutes of the injury. Prehospital ETI in trauma patients has been associated with hypotension and decreased survival.[15] However, securing the airway of a patient in the face of impending hemodynamic collapse is critical. Induction agents and positive pressure ventilation may further worsen hypotension that the trauma victim is already experiencing from hemorrhage. Positive pressure ventilation causes a reduction in venous return to the heart and can contribute to cardiovascular collapse. Volume replacement (preferably with blood and clotting factors) should be performed in conjunction with positive pressure ventilation.
Proficient and reliable pediatric airway management skills are difficult to acquire and maintain. One study from Pediatrics concluded that LMA placement led to more rapid establishment of an airway with fewer demonstrated complications.[33] Despite airway insertion times not being statistically different, paramedics in a simulated pediatric respiratory arrest scenario preferred the King Laryngeal Tube airway over conventional ETI.[34] Other studies have suggested that LMA use is safe and effective when compared with BMV during neonatal resuscitation.[35] This patient population will likely continue to remain a challenge to prehospital providers until better education and maintenance standards exist.
Time to hospital arrival must be taken into consideration and long distance travel prior to hospitalization may necessitate ETI for airway management. For example, fluid shifts from bleeding and restorative IV therapy during resuscitation can lead to respiratory failure from pulmonary edema. In this situation it is wise to preemptively secure a patient's airway prior to transport.
Airway management protocols for use in combat situations have not yet been defined.[36] A study of prehospital airway management from Operation Iraqi Freedom demonstrated an ETI success rate of 95.7%.[37] This is in contrast to one recent study that suggested that airway and chest lifesaving interventions were most frequently missed in combat situations.[38] No matter what current outcomes data may imply, it is reasonable to expect that improved protocols and rigorous training standards should improve prehospital airway management in combat situations.
Future developments
Video airway management devices will likely become a component of prehospital airway management education in the future. At present, several portable laryngoscopes including the Glidescope®, Pentax®, Storz® (DCI and CMAC), Airtraq®, and McGrath® are utilized by anesthesiology and emergency medicine physicians. VAL is often used as a primary intubation technique for patients with a presumed difficult airway or cervical spine injury. Additionally, these video devices are frequently utilized as a rescue technique for failed intubation. However, wide spread acceptance of VAL in the prehospital setting has yet to gain universal support.
To date, several studies have compared VAL with conventional direct laryngoscopy (DL). Aziz et al. demonstrated an overall success rate for Glidescope® intubation of 97% with a 94% success rate of Glidescope® intubation after failed DL.[39] Studies have demonstrated that VAL led to improved glottic visualization, however, intubation times varied between different VAL devices and were not globally superior to DL.[40] Additionally, studies have demonstrated great variability in ETI success rates between different types of VAL devices.[41] This makes it impossible to extrapolate data from one study and apply it to all VAL devices.
One review article highlighted increased first-attempt success and decreased time to intubation in studies of nonexperts with the Glidescope® compared with DL. However, these authors suggested the need for further investigation into this correlation.[42]
One paramedic study again supported the conclusion that glottic visualization was improved with VAL.[43] However, the same study found similar ETI success rates between VAL and DL. Despite conflicting data, it is reasonable to expect that VAL will become an important technique for prehospital airway providers. Improved access to these devices during provider training will increase familiarity and comfort with VAL.
Additional future considerations include the implementation of capnography in the prehospital setting. This modality offers noninvasive confirmation of ETT placement, provides a real-time measure of a patient's ventilatory status, and can assist in advanced airway placement.[44,45] Increasing use of capnography within the field of emergency medicine will likely translate to future use in the prehospital setting as well.
CONCLUSION
ETI success is a common measure of out-of-hospital airway management quality. Some studies suggest that prehospital ETI success ranges from 69% to 98.4%.[46,47,48,49,50,51] Regional variation in regard to training, education, and procedural exposure may be the major contributor to these findings. In studies demonstrating poor outcomes related to prehospital-attempted ETI, both training and skill level of the provider are usually is often low.
Research supports a relationship between the number of intubation experiences and ETI success.[26] National standards for paramedics currently require a minimum of five intubations for certification. The minimum requirement for physicians participating German EMS systems is anywhere from 25 to 50 intubations. The ACGME mandates that 35 intubations are required for emergency medicine residents during training.[52] When compared with the greater than 1000 experiences that anesthesiology residents are exposed to during their training these minimum requirements appear inadequate. One survey of paramedic training programs reported that the median number of ETIs per student was 7 and suggested that 20-25 ETIs were required to achieve an overall success rate of 90%.[53]
Some training programs, such as King County, WA offer paramedic students early access to airway management skills through hands-on skill labs, lectures, and involvement in the operating room setting. Paramedic students learn the basics of airway management in a controlled environment under the close supervision of anesthesiologists, anesthesiology residents, and CRNAs. Following this thorough introduction, senior level paramedics assume the role of educators and further instruct paramedic trainees on how to properly manage the prehospital airway. More rigorous paramedic training programs (such as King County, WA) report significantly higher success rates with prehospital ETI.[24] In regard to ETI, development of more rigorous and universally accepted training standards would likely lead to improved success rates and outcomes, in paramedic and physician staffed systems.
ETI remains the cornerstone of definitive prehospital airway management. However, ETI is not without risk and outcomes data remains controversial. At present, ETI has not been replaced by SGA devices in the prehospital setting. However, these devices continue to gain favor in certain patient populations.[33,34,35] As technology and provider experience improves, it is reasonable to believe that VAL will likely become a widely accepted prehospital airway modality. Additionally, capnography will most likely become a component of prehospital provider education and daily practice. Many systems may benefit from more input and guidance by the anesthesia department, which have higher volumes in regard to airway management and extensive training and experience not just with training of airway management but also with different airway management techniques and adjuncts.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Swor R, Khan L, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: Do CPR-trained bystanders perform CPR? Acad Emerg Med. 2011;6:509–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 2.Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Adult Basic Life Support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S685–705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 3.Berg RA, Kern KB, Hilwig RW, Ewy GA. Assisted ventilation during ‘Bystander’ CPR in a swine acute myocardial infarction model does not improve outcome. Circulation. 1997;96:1635–41. doi: 10.1161/01.cir.96.12.4364. [DOI] [PubMed] [Google Scholar]
- 4.Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD American Heart Association Emergency Cardiovascular Care Committee. Hands-only (compression-only) cardiopulmonary resuscitation: A call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: A science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–7. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 5.Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116:2908–12. doi: 10.1161/CIRCULATIONAHA.107.710194. [DOI] [PubMed] [Google Scholar]
- 6.Dumas F, Rea TD, Fahrenbruch C, Rosenqvist M, Faxen J, Svensson L, et al. Chest compression alone cardiopulmonary resuscitation is associated with better long-term survival compared with standard cardiopulmonary resuscitation. Circulation. 2013;127:435–41. doi: 10.1161/CIRCULATIONAHA.112.124115. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: A prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347–54. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- 8.Stoy WE, editor. US Department of Transportation. National Traffic Highway Safety Administration. EMT-Paramedic: National Standard Curriculum. 1998 [Google Scholar]
- 9.Armstrong E, Corning D, Gainor D, Kalinowski E, King M, Manz D, et al. National Highway Traffic Safety Administration; 2007. National EMS Scope of Practice Model; pp. 2–37. [Google Scholar]
- 10.Hubble MW, Richards ME, Jarvis R, Millikan T, Young D. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care. 2006;10:430–9. doi: 10.1080/10903120600884848. [DOI] [PubMed] [Google Scholar]
- 11.Frascone RJ, Russi C, Lick C, Conterato M, Wewerka SS, Griffith KR, et al. Comparison of prehospital insertion success rates and time to insertion between standard endotracheal intubation and a supraglottic airway. Resuscitation. 2011;82:1529–36. doi: 10.1016/j.resuscitation.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Practice guidelines for management of the difficult airway. Anesthesiology. 2003;98:1269–77. doi: 10.1097/00000542-200305000-00032. [DOI] [PubMed] [Google Scholar]
- 13.Pennant JH, Walker MB. Comparison of the endotracheal tube and laryngeal mask in airway management by paramedical personnel. Anesth Analg. 1992;74:531–4. doi: 10.1213/00000539-199204000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Garza AG, Gratton MC, Coontz D, Noble E, Ma OJ. Effect of paramedic experience on orotracheal intubation success rates. J Emerg Med. 2003;25:251–6. doi: 10.1016/s0736-4679(03)00198-7. [DOI] [PubMed] [Google Scholar]
- 15.Shafi S, Gentilello Pre-Hospital endotracheal intubation and positive pressure ventilation is associated with hypotension and decreased survival in hypovolemic trauma patients: An analysis of the national trauma Data Bank. J Trauma. 2005;59:1140–5. doi: 10.1097/01.ta.0000196434.88182.77. [DOI] [PubMed] [Google Scholar]
- 16.Cobas MA, De la Peña MA, Manning R, Candiotti K, Varon AJ. Prehospital intubations and mortality: A level 1 trauma center perspective. Anesth Analg. 2009;109:489–93. doi: 10.1213/ane.0b013e3181aa3063. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa K, Hiraide A, Chang Y, Brown D. Association of prehospital airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309:257–66. doi: 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
- 18.Miraflor E, Chuang K, Miranda MA. Timing is everything: Delayed intubation is associated with increased mortality in initially stable trauma patients. J Surg Res. 2011;170:286–90. doi: 10.1016/j.jss.2011.03.044. [DOI] [PubMed] [Google Scholar]
- 19.Davis DP, Koprowicz KM, Newgard CD, Daya M, Bulger EM, Stiell I, et al. The relationship between out-of-hospital airway management and outcome among trauma patients with glasgow coma scale scores of 8 or less. Prehosp Emerg Care. 2011;15:184–92. doi: 10.3109/10903127.2010.545473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang HE, Mann NC, Mears G, Jacobson K, Yealy D. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–85. doi: 10.1016/j.resuscitation.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Fischer M, Krep H, Wierich D, Heister U, Hoeft A, Edwards S, et al. Comparison of the emergency medical services systems of Birmingham and Bonn: Process efficacy and cost effectiveness. Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:630–42. doi: 10.1055/s-2003-42507. [DOI] [PubMed] [Google Scholar]
- 22.Timmermann A, Russo SG, Hollman MW. Paramedic versus emergency physician emergency medical service: Role of the anaesthesiologist and the European versus the Anglo-American concept. Curr Opin Anesth. 2008;21:222–7. doi: 10.1097/ACO.0b013e3282f5f4f7. [DOI] [PubMed] [Google Scholar]
- 23.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional Variation in Out-of-Hospital Cardiac Arrest Incidence and Outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warner KJ, Sharar SR, Copass MK, Bulger EM. Prehospital management of the difficult airway: A prospective cohort study. J Emerg Med. 2009;36:257–65. doi: 10.1016/j.jemermed.2007.10.058. [DOI] [PubMed] [Google Scholar]
- 25.Genzwürker H, Hinkelbein J, Ellinger K. Emergency physician qualification in the different Federal states of Germany. Der Notarzt. 2003;19:186–92. [Google Scholar]
- 26.Bernhard M, Mor S, Weigand MA, Martin E, Walther A. Developing the skill of endotracheal intubation: Implication for emergency medicine. Acta Anaesthesiol Scand. 2012;56:164–71. doi: 10.1111/j.1399-6576.2011.02547.x. [DOI] [PubMed] [Google Scholar]
- 27.Sunde GA, Brattebø G, Odegården T, Kjernlie DF, Rødne E, Heltne JK. Laryngeal tube use in out-of-hospital cardiac arrest by paramedics in Norway. Scand J Trauma Resusc Emerg Med. 2012;20:84. doi: 10.1186/1757-7241-20-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidbauer W, Genzwürker H, Ahlers O, Proquitte H, Kerner T. Cadaver study of oesophageal insufflation with supraglottic airway devices during positive pressure ventilation in an obstructed airway. Br J Anaesth. 2012;109:454–8. doi: 10.1093/bja/aes142. [DOI] [PubMed] [Google Scholar]
- 29.Vézina MC, Trépanier CA, Nicole PC, Lessard MR. Complications associated with the Esophageal-Tracheal Combitube in the pre-hospital setting. Can J Anaesth. 2007;54:124–8. doi: 10.1007/BF03022008. [DOI] [PubMed] [Google Scholar]
- 30.Segal N, Yannopoulos D, Mahoney BD, Frascone RJ, Matsuura T, Cowles CG, et al. Impairment of carotid artery blood flow by supraglottic airway use in a swine model of cardiac arrest. Resuscitation. 2012;83:1025–30. doi: 10.1016/j.resuscitation.2012.03.025. [DOI] [PubMed] [Google Scholar]
- 31.Wang HE, Szydlo D, Stouffer JA, Lin S, Carlson JN, Vaillancourt C, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation. 2012;83:1061–6. doi: 10.1016/j.resuscitation.2012.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kajino K, Iwami T, Kitamura T, Daya M, Ong ME, Nishiuchi T, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care. 2011;15:R236. doi: 10.1186/cc10483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen L, Hsiao AL. Randomized trial of endotracheal tube versus laryngeal mask airway in simulated prehospital pediatric arrest. Pediatrics. 2008;122:e294–7. doi: 10.1542/peds.2008-0103. [DOI] [PubMed] [Google Scholar]
- 34.Mitchell MS, Lee White M, King WD, Wang HE. Paramedic King Laryngeal Tube airway insertion versus endotracheal intubation in simulated pediatric respiratory arrest. Prehosp Emerg Care. 2012;16:284–8. doi: 10.3109/10903127.2011.640762. [DOI] [PubMed] [Google Scholar]
- 35.Zhu XY, Lin BC, Zhang QS, Ye HM, Yu RJ. A prospective evaluation of the efficacy of the laryngeal mask airway during neonatal resuscitation. Resuscitation. 2011;82:1405–9. doi: 10.1016/j.resuscitation.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 36.Mabry RL, Frankfurt A. Advanced airway management in combat casualties by medics at the point of injury: A sub-group analysis of the reach study. J Spec Oper Med. 2011;11:16–9. doi: 10.55460/W35F-54HG. [DOI] [PubMed] [Google Scholar]
- 37.Adams BD, Cuniowski PA, Muck A, De Lorenzo RA. Registry of emergency airways arriving at combat hospitals. J Trauma. 2008;64:1548–54. doi: 10.1097/TA.0b013e3181728c41. [DOI] [PubMed] [Google Scholar]
- 38.Lairet JR, Bebarta VS, Burns CJ, Lairet KF, Rasmussen TE, Renz EM, et al. Prehospital interventions performed in a combat zone: A prospective multicenter study of 1,003 combat wounded. J Trauma Acute Care Surg. 2012;73(2 Suppl 1):S38–42. doi: 10.1097/TA.0b013e3182606022. [DOI] [PubMed] [Google Scholar]
- 39.Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: An analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41. doi: 10.1097/ALN.0b013e3182023eb7. [DOI] [PubMed] [Google Scholar]
- 40.Healy DW, Picton P, Morris M, Turner C. Comparison of the glidescope, CMAC, storz DCI with the Macintosh laryngoscope during simulated difficult laryngoscopy: A manikin study. BMC Anesthesiol. 2012;12:11. doi: 10.1186/1471-2253-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maassen R, Lee R, Hermans B, Marcus M, van Zundert A. A comparison of three videolaryngoscopes: The Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009;109:1560–5. doi: 10.1213/ANE.0b013e3181b7303a. [DOI] [PubMed] [Google Scholar]
- 42.Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can J Anaesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piepho T, Weinert K, Heid FM, Werner C, Noppens RR. Comparison of the McGrath® Series 5 and GlideScope® Ranger with the Macintosh laryngoscope by paramedics. Scand J Trauma Resusc Emerg Med. 2011;19:4. doi: 10.1186/1757-7241-19-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nagler J, Krauss B. Capnography: A Valuable Tool for Airway Management. Emerg Med Clin North Am. 2008;26:881–97. doi: 10.1016/j.emc.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Mentzelopoulos SD, Augustatou CG, Papageorgiou EP. Capnography-guided nasotracheal intubation of a patient with a difficult airway and unwanted respiratory depression. Anesth Analg. 1998;87:734–6. doi: 10.1097/00000539-199809000-00049. [DOI] [PubMed] [Google Scholar]
- 46.Bulger EM, Copass MK, Maier RV, Larsen J, Knowles J, Jurkovich GJ. An analysis of advanced prehospital airway management. J Emerg Med. 2002;23:183–9. doi: 10.1016/s0736-4679(02)00490-0. [DOI] [PubMed] [Google Scholar]
- 47.Bulger EM, Nathens AB, Rivara FP, MacKenzie E, Sabath DR, Jurkovich GJ. National variability in out-of-hospital treatment after traumatic injury. Ann Emerg Med. 2007;49:293–301. doi: 10.1016/j.annemergmed.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 48.Warner KJ, Sharar SR, Copass MK, Bulger EM. Prehospital management of the difficult airway: A prospective cohort study. J Emerg Med. 2009;36:257–65. doi: 10.1016/j.jemermed.2007.10.058. [DOI] [PubMed] [Google Scholar]
- 49.Wang HE, Kupas DF, Paris PM, Bates RR, Yealy DM. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation. 2003;58:49–58. doi: 10.1016/s0300-9572(03)00058-3. [DOI] [PubMed] [Google Scholar]
- 50.Davis DP, Fisher R, Buono C, Brainard C, Smith S, Ochs G, et al. Predictors of intubation success and therapeutic value of paramedic airway management in a large, urban EMS system. Prehosp Emerg Care. 2006;10:356–62. doi: 10.1080/10903120600725751. [DOI] [PubMed] [Google Scholar]
- 51.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–7. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 52.ACGME Emergency Medicine Guidelines, guidelines for procedures and resuscitation. [Last accessed on 2013 Apr 2]. Available from: http:///www.acgme.org .
- 53.Wang HE, Seitz SR, Hostler D, Yealy DM. Defining the learning curve for paramedic student endotracheal intubation. Prehosp Emerg Care. 2005;9:156–62. doi: 10.1080/10903120590924645. [DOI] [PubMed] [Google Scholar]


