Abstract
IMPORTANCE
Patients undergoing hemodialysis have an annual mortality rate exceeding 20%, comparable to many types of cancer. Past research has shown that patients with cancer overestimate their likelihood of survival relative to their physicians, but this relationship has not been examined in patients with noncancer diagnoses. Perceptions of prognosis and transplant candidacy may influence goals of care.
OBJECTIVES
To compare the perceptions of hemodialysis patients and their nephrologists concerning prognosis and the likelihood of transplant; to follow actual survival; and to explore the relationship between patients’ expectations and their goals of care.
DESIGN
We completed a medical record abstraction to estimate 1-year mortality risk among patients who underwent dialysis at any time from November 1, 2010, through September 1, 2011. We then conducted in-person interviews with eligible patients whose predicted 1-year mortality, based on validated prognostic tools, was at least 20%. We also interviewed their nephrologists. We compared patients’ and physicians’ expectations about 1- and 5-year survival and transplant candidacy and measured the association between patients’ expectations and goals of care. We then followed actual survival using Kaplan-Meier methods.
SETTING AND PARTICIPANTS
Two dialysis units in Boston. Two hundred seven patients undergoing hemodialysis included in the medical record review, with 62 eligible patients interviewed.
MAIN OUTCOMES AND MEASURES
Predicted 1-year mortality risk using validated prognostic tools; actual survival; patients’ and physicians’ expectations about 1-year survival and likelihood of transplant; and patients’ goals of care.
RESULTS
Of the 207 hemodialysis patients, 72.5% had a predicted 1-year mortality of at least 20%. Of the 80 patients eligible for interview, 62 participated (response rate, 78%). Patients were significantly more optimistic than their nephrologists about 1- and 5-year survival (P < .001 for both) and were more likely to think they were transplant candidates (37 [66%] vs 22 [39%] [P = .008]). Of the 81% of patients reporting a 90% chance or greater of being alive at 1 year, 18 (44%) preferred care focused on extending life, even if it meant more discomfort, compared with 1 (9%) among patients reporting a lower chance of survival (P = .045). Actual survival was 93% at 1 year but decreased to 79% by 17 months and 56% by 23 months.
CONCLUSIONS AND RELEVANCE
Hemodialysis patients are more optimistic about prognosis and transplant candidacy than their nephrologists. In our sample, patients’ expectations about 1-year survival were more accurate than those of their nephrologists, but their longer-term survival expectations dramatically overestimated even their 2-year survival rates. Patients’ prognostic expectations are associated with their treatment preferences. Our findings suggest the need for interventions to help providers communicate effectively with patients about prognosis.
End-stage renal disease is a significant cause of morbidity and mortality in the United States. Approximately 400 000 Americans currently undergo long-term dialysis,1 and the 1-year mortality rate for these patients ranges from 20% to 25%,2 comparable to that of many types of cancer. An accurate estimate of prognosis enables patients and families to plan for the future and make informed decisions about goals of care.3 We therefore believe that physicians should offer to discuss prognosis with patients, particularly those who are seriously ill.4
Several studies5-8 have documented that patients with cancer commonly overestimate their likelihood of survival relative to their physicians. However, this occurrence has not been studied in patients with noncancer diagnoses. Therefore, whether these findings translate to patients with other end-stage conditions, such as end-stage renal disease, is unknown. Although prognostication can be more difficult for noncancer diagnoses,9 validated prognostic instruments exist to estimate mortality risk for a number of patient populations, including those undergoing hemodialysis.10-17 In 2000, the Renal Physicians Association and the American Society of Nephrology issued a joint practice guideline18 recommending that providers communicate the likelihood of survival to all hemodialysis patients. An updated guideline19 was issued in 2010. To assist physicians in calculating survival estimates for individual hemodialysis patients, the guideline cites validated prognostic tools.19 However, the extent to which nephrologists have conversations with hemodialysis patients about prognosis is unknown.
One factor that may affect prognosis in end-stage renal disease and dialysis-related decision making is the possibility of kidney transplant. Transplant recipients have a 68% lower mortality rate than patients eligible for transplant who continue to receive hemodialysis.20 The degree to which patients and nephrologists agree about the likelihood of transplant remains unknown. Finally, we do not know whether the expectations that seriously ill hemodialysis patients have about prognosis and transplant candidacy influence their goals of care.
We sought to compare the perceptions of prognosis and likelihood of transplant among hemodialysis patients and their nephrologists, to follow actual patient survival, and to explore the relationship between patients’ expectations and their goals of care.
Methods
Design Overview
We conducted a 2-part study of patients receiving maintenance hemodialysis. Part 1 consisted of a medical record abstraction and a physician screening question to estimate the risk of 1-year mortality for all patients. Part 2 consisted of in-person interviews with seriously ill hemodialysis patients (defined as having a ≥20% risk of dying in the next year) and their nephrologists. Our cut point of 20% or greater is supported by the nephrology societies’ practice guideline,18,19 which recommends discussing temporally specific prognostic estimates with all hemodialysis patients. Human subjects committees at both hospitals and dialysis units approved the study.
Setting and Participants
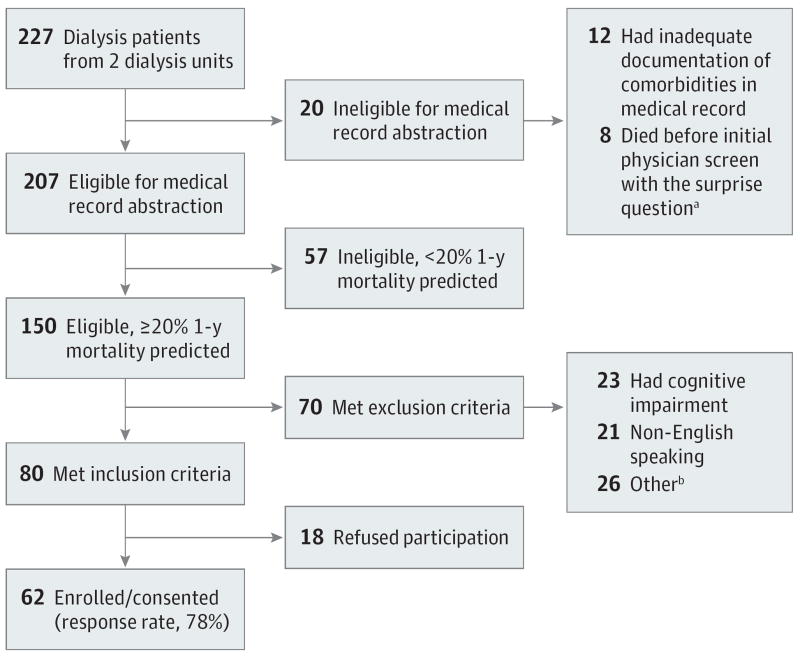
We included patients from 2 community-based hemodialysis units affiliated with tertiary care medical centers in Boston from November 1, 2010, through September 1, 2011. The Figure shows the construction of our sample. We began with all 227 patients on the hemodialysis centers’ rosters, of whom 207 had adequate documentation in their medical record to estimate 1-year mortality risk using 2 prognostic indices (described below). Among these 207 patients, 150 (72.5%) had an estimated 1-year mortality risk that was 20% or greater on at least 1 index, which we defined as seriously ill. We then applied exclusion criteria to these 150 patients to identify those eligible for our interview. Seventy of these patients (46.7%) were excluded owing to cognitive impairment (n = 23), inability to speak English (n = 21), or other factors (n = 26) (Figure). Of the remaining 80 eligible patients, 62 provided informed consent and were interviewed (response rate, 78%).
Figure. Study Flow Diagram.
aThe surprise question asks, “Would you be surprised if this patient died in the next 6 months?”
bIncludes transplant, transition to peritoneal dialysis, or death before being approached to participate in the interview; refusal of the physician to allow participation; and failure to interview the patient despite 3 attempts to approach him or her (typically owing to hospitalization or consistently sleeping during dialysis).
Medical Record Abstraction and Physician Screening Question
We collected information from the patients’ medical records on sociodemographic characteristics, medical comorbidities, use of health care resources, and albumin concentrations. We used the following 2 validated prognostic models11,13 to estimate hemodialysis patients’ risk of dying in the next year: (1) the modification by Beddhu et al11 of the Charlson Comorbidity Index21 and (2) the prognostic model of Cohen et al,13 which includes age, albumin concentration, presence of dementia, peripheral vascular disease, and the question asked of each patient’s nephrologist, “Would you be surprised if this patient died in the next 6 months?” (ie, the surprise question).22 A response of no is a strong predictor of mortality among dialysis patients.22 (Additional details regarding the 2 prognostic models are given in the eMethods in the Supplement.) Patients with a predicted risk of dying in the next year of at least 20% in either prognostic model underwent assessment for eligibility to participate in the interview.
Interviews With Patients and Nephrologists
We conducted in-person interviews with 62 eligible, seriously ill dialysis patients. This interview involved 77 items covering predictions about 1- and 5-year survival and the likelihood of transplant, preferences for care, and communication with family and physicians. We then interviewed each patient’s nephrologist (n = 14) to ascertain the nephrologist’s perspective on these domains for each specific patient.
The interview was adapted from previous studies, including the SUPPORT (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment) trial,23,24 the Coping with Cancer Study,25 and the Framingham Heart Study.26 We assessed patients’ prognostic expectations by asking what they thought their chances were of being alive in 1 and 5 years, respectively (≥90%, about 75%, about 50%, about 25%, ≤10%, or don’t know). Nephrologists were asked to estimate each patient’s likelihood of being alive at 1 and 5 years on a continuous scale from 0 to 100%.
We also asked patients and nephrologists whether they thought kidney transplant was a possibility and what they thought their likelihood of receiving a transplant was (using the same multiple-choice options as for estimates of prognosis). We defined “optimistic transplant discordance” as present when patients reported a greater likelihood than their nephrologists that they would receive a transplant. Patients’ goals of care were assessed by using the item, “If you were seriously ill, would you prefer care to (a) extend life, even if it meant more pain and discomfort, or (b) relieve pain and discomfort, even it if meant not living as long?” For each patient, nephrologists were asked to estimate life expectancy and to report whether they had provided an estimate to the patient. If not, they were asked whether they would communicate a specific estimate if the patient insisted on receiving one.
Abstraction of Survival Data
We obtained survival data through December 20, 2012, from the hemodialysis units. One unit recorded the date of death, whereas the other recorded only the month of death, in which case we set the date as the 15th of the month. We also obtained the last date of hemodialysis for any patient who was no longer receiving hemodialysis at the unit.
Statistical Analysis
Using the prognostic calculators,11,13 we compared characteristics between patients with at least a 20% and those with less than a 20% projected 1-year mortality. Next, we examined the 150 patients with a 1-year mortality risk of 20% or greater, comparing those who participated in the interview (n = 62), who met exclusion criteria (n = 70), and who refused participation (n = 18).
Our subsequent analyses focused on the 62 patients we interviewed. We examined how often patients and nephrologists reported that prognostic discussions occurred, and we assessed nephrologists’ willingness to formulate and communicate prognostic estimates to their patients. Consistent with previous research,8 we grouped physicians’ 1- and 5-year survival estimates into 5 categories to facilitate comparisons with patients’ estimates. We assessed agreement between patients’ and their nephrologists’ prognostic estimates with the weighted κ statistic and the Spearman correlation coefficient (rs) and between their beliefs about transplant candidacy with the κ statistic. We used the McNemar test to assess whether the disagreement between patients’ and nephrologists’ estimates was in a particular direction. We counted the number of patients with more optimistic estimates than their physicians and the number with more pessimistic estimates. As a sensitivity analysis, we repeated the analysis but required disagreement by at least 2 categories (ie, ≥90%, 61%-89%, 40%-60%, 11%-39%, and ≤10%). Next, we dichotomized patients’ survival estimates as 90% or greater or less than 90% and used Fisher exact tests to explore whether patients’ prognostic expectations and the presence of optimistic transplant discordance were associated with their goals of care. We excluded patients with item nonresponse from those analyses for which data were missing (ranging from 3 to 10). Finally, we estimated actual survival with the Kaplan-Meier product-limit method. We conducted all data analyses with commercially available software (SAS, version 9.2; SAS Institute, Inc).
Results
Table 1 shows characteristics of the 207 patients in our medical record review, comparing patients with a predicted 1-year mortality risk of at least 20% and those with a risk of less than 20%. Patients with a higher mortality risk were older (mean ages, 70.2 vs 48.4 years) and had a greater comorbid disease burden. Their nephrologists were also less likely to report that they would be surprised if the patient died in the next 6 months (53.4% vs 96.3%).
Table 1.
Characteristics of 207 Patients Undergoing Hemodialysis by Estimated Risk of 1-Year Mortalitya
| Characteristic | Estimated Risk of 1-y Mortality | P Value | |
|---|---|---|---|
| ≥20% (n = 150) | <20% (n = 57) | ||
| Sexb | |||
| Male | 71 (47.3) | 27 (47.4) | >.99 |
| Female | 79 (52.7) | 30 (52.6) | |
| Raceb | |||
| White | 50 (33.3) | 16 (28.1) | .38 |
| Black | 69 (46.0) | 34 (59.6) | |
| Asian | 7 (4.7) | 2 (3.5) | |
| Other | 2 (1.3) | 1 (1.8) | |
| Not documented | 22 (14.7) | 4 (7.0) | |
| Ethnicityb | |||
| Hispanic | 25 (16.7) | 8 (14.0) | .68 |
| Non-Hispanic | 68 (45.3) | 30 (52.6) | |
| Not documented | 57 (38.0) | 19 (33.3) | |
| Marital statusb | |||
| Married or living with a partner | 66 (44.0) | 20 (35.1) | .35 |
| Unmarried | 69 (46.0) | 33 (57.9) | |
| Not documented | 15 (10.0) | 4 (7.0) | |
| Age, yb | |||
| Mean (SD) | 70.2 (12.0) | 48.4 (11.9) | |
| ≤50 | 8 (5.3) | 33 (57.9) | <.001 |
| 51-60 | 23 (15.3) | 14 (24.6) | |
| 61-70 | 43 (28.7) | 9 (15.8) | |
| 71-80 | 43 (28.7) | 1 (1.8) | |
| >80 | 33 (22.0) | 0 | |
| Charlson Comorbidity Index scorec,d | |||
| Mean (SD) | 5.9 (1.7) | 3.2 (1.0) | |
| 0-4 | 31 (20.8) | 48 (84.2) | <.001 |
| 5-6 | 65 (43.6) | 9 (15.8) | |
| ≥7 | 53 (35.6) | 0 | |
| Nephrologist surprised if patient died in next 6 moc,e | |||
| Surprised | 79 (53.4) | 52 (96.3) | <.001 |
| Not surprised | 69 (46.6) | 2 (3.7) | |
| Presence of diabetes mellitusb | 106 (70.7) | 11 (19.3) | <.001 |
| Presence of dementiab | 23 (15.3) | 1 (1.8) | .006 |
| Use of health care resources in previous yearb | |||
| No. of hospitalizations, mean (SD) | 2.6 (2.8) | 2.2 (2.7) | .29 |
| No. of emergency department visits, mean (SD) | 3.2 (3.7) | 2.3 (2.8) | .10 |
Data are expressed as the number (percentage) of patients unless otherwise specified. Percentages have been rounded and might not total 100.
Obtained from the medical record abstraction.
Of the 207 patients in the analytic sample, 5 had missing data for the surprise question and 1 had missing data for the comorbidity score.
Calculated from comorbidity information obtained from the medical record abstraction.
Obtained from interview with the patient’s nephrologist.
Table 2 presents characteristics of the 150 patients with a 1-year mortality risk of 20% or greater, comparing eligible patients who were interviewed, eligible patients who refused participation, and ineligible patients. Ineligible patients were more frequently Hispanic. Interviewees were younger and less likely to have dementia than those who were ineligible or refused. Nephrologists of ineligible patients were the least likely to be surprised if the patient died in the next 6 months (40%). The groups were otherwise similar.
Table 2.
Characteristics of 150 Hemodialysis Patients With a 20% or Greater Risk of 1-Year Mortality by Eligibility Status for Interviewa
| Characteristic | Eligible Patients (n = 80) | Ineligible Patients (n = 70) | P Value | |
|---|---|---|---|---|
| Interviewed (n = 62) | Refused (n = 18) | |||
| Sexb | ||||
| Male | 26 (42) | 10 (56) | 35 (50) | .53 |
| Female | 36 (58) | 8 (44) | 35 (50) | |
| Raceb | ||||
| White | 19 (31) | 8 (44) | 23 (33) | .15 |
| Black | 32 (52) | 8 (44) | 29 (41) | |
| Asian | 5 (8) | 1 (6) | 1 (1) | |
| Other | 1 (2) | 0 | 1 (1) | |
| Not documented | 5 (8) | 1 (6) | 16 (23) | |
| Ethnicityb | ||||
| Hispanic | 5 (8) | 0 | 28 (40) | .003 |
| Non-Hispanic | 33 (53) | 7 (39) | 20 (29) | |
| Not documented | 24 (39) | 11 (61) | 22 (31) | |
| Marital statusb | ||||
| Married or living with a partner | 25 (40) | 9 (50) | 32 (46) | .67 |
| Unmarried | 31 (50) | 6 (33) | 32 (46) | |
| Not documented | 6 (10) | 3 (17) | 6 (9) | |
| Age, yb | ||||
| Age, mean (SD), y | 68.2 (10.3) | 69.4 (10.6) | 72.1 (13.5) | |
| ≤50 | 1 (2) | 1 (6) | 6 (9) | .03 |
| 51-60 | 13 (21) | 3 (17) | 7 (10) | |
| 61-70 | 24 (39) | 4 (22) | 15 (21) | |
| 71-80 | 15 (24) | 8 (44) | 20 (29) | |
| >80 | 9 (15) | 2 (11) | 22 (31) | |
| Length of time receiving hemodialysisc | ||||
| <6 mo | 1 (2) | NA | NA | NA |
| 6-12 mo | 11 (18) | NA | NA | |
| 13 mo to 5 y | 34 (55) | NA | NA | |
| >5y | 16 (26) | NA | NA | |
| Highest level of educationc | ||||
| Did not graduate high school | 13 (22) | NA | NA | NA |
| Graduated high school or completed GED | 21 (36) | NA | NA | |
| Some college | 9 (16) | NA | NA | |
| Graduated college | 15 (26) | NA | NA | |
| Charlson Comorbidity Index scored,e | ||||
| Mean (SD) | 5.8 (1.6) | 5.8 (2.1) | 6.0 (1.8) | |
| 0-4 | 13 (21) | 5 (28) | 13 (19) | .54 |
| 5-6 | 29 (47) | 9 (50) | 27 (39) | |
| ≥7 | 20 (32) | 4 (22) | 29 (42) | |
| Nephrologist surprised if patient died in next 6 moe,f | ||||
| Surprised | 38 (61) | 14 (78) | 27 (40) | .005 |
| Not surprised | 24 (39) | 4 (22) | 41 (60) | |
| Presence of diabetes mellitusb | 44 (71) | 12 (67) | 50 (71) | .94 |
| Presence of dementiab | 4 (6) | 4 (22) | 15 (21) | .03 |
| Use of health care resources in previous yearb | ||||
| No. of hospitalizations, mean (SD) | 2.7 (3.1) | 1.6 (1.7) | 2.8 (2.8) | .26 |
| No. of emergency department visits, mean (SD) | 3.0 (3.1) | 1.7 (1.6) | 3.8 (4.4) | .08 |
Abbreviations: GED, General Educational Development test; NA, not available.
Data are expressed as number (percentage) of patients unless otherwise specified. Percentages have been rounded and might not total 100.
Obtained from the medical record abstraction.
Obtained from interview with the patient. Therefore, data were not available for patients who were ineligible for interview or who refused to participate in the interview. Of the 62 interviewees, 4 had missing data for highest level of education.
Calculated from comorbidity information obtained from the medical record abstraction.
Of the 150 patients in the analytic sample, 2 had missing data for the surprise question and 1 had missing data for the comorbidity score.
Obtained from interview with the patient’s nephrologist.
Among the 62 interviewed patients, no patients reported that their nephrologist had discussed an estimate of life expectancy with them, and the nephrologists reported that they had done so for only 2 interviewed patients (3%). Nephrologists provided us with estimates of life expectancy for 55 of the interviewed patients (89%) but reported that, if the patient insisted on an estimate, they would refuse to provide any estimate for 33 of these (60%).
Table 3 summarizes patients’ and nephrologists’ expectations about survival. We found almost no agreement between patients’ and nephrologists’ estimates of 1-year survival (weighted κ = 0.08; rs = 0.09),27 with patients significantly more optimistic than their nephrologists (P < .001). Patients’ estimates were more optimistic in 38 of 59 patient-nephrologist pairs (64%), whereas nephrologists were more optimistic in 6 of 59 pairs (10%). Overall, 81% of patients thought they had at least a 90% chance of being alive in 1 year, whereas nephrologists were this optimistic for only 25% of patients. The lack of patient-nephrologist agreement (weighted κ = 0.13; rs = 0.16) and the finding that patients were significantly more optimistic (P < .001) were similar for 5-year estimates. Patients’ estimates were more optimistic in 36 of 52 patient-nephrologist pairs (69%), whereas nephrologists were more optimistic in 1 of 52 pairs (2%). Only 6% of patients thought they had less than a 50% chance of being alive in 5 years, whereas nephrologists estimated that 56% of the patients had a chance of 5-year survival at less than 40%. For 1- and 5-year survival, sensitivity analyses requiring 2 categories of disagreement showed the same pattern (P < .001 for both).
Table 3.
Comparison of Patients’ and Nephrologists’ Estimates of 1- and 5-Year Survivala
| Patient Estimate of Survival, % | Nephrologist Estimate of Survival, %b | |||||
|---|---|---|---|---|---|---|
| ≥90 | 61-89 | 40-60 | 11-39 | ≤10 | Total, No. (%) | |
| At 1 yc | ||||||
| ≥90 | 13 (27) | 23 (48) | 12 (25) | 0 | 0 | 48 (81) |
| 75 | 2 (33) | 2 (33) | 2 (33) | 0 | 0 | 6 (10) |
| 50 | 0 | 4 (100) | 0 | 0 | 0 | 4 (7) |
| 25 | 0 | 0 | 0 | 0 | 1 (100) | 1 (2) |
| ≤10 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 15 (25) | 29 (49) | 14 (24) | 0 | 1 (2) | 59 (100) |
| At 5 yd | ||||||
| ≥90 | 3 (14) | 1 (5) | 5 (23) | 10 (45) | 3 (14) | 22 (42) |
| 75 | 1 (9) | 2 (18) | 4 (36) | 1 (9) | 3 (27) | 11 (21) |
| 50 | 0 | 0 | 7 (44) | 5 (31) | 4 (25) | 16 (31) |
| 25 | 0 | 0 | 0 | 2 (100) | 0 | 2 (4) |
| ≤10 | 0 | 0 | 0 | 0 | 1 (100) | 1 (2) |
| Total | 4 (8) | 3 (6) | 16 (31) | 18 (35) | 11 (21) | 52 (100) |
Data are expressed as the number (percentage) of patient-nephrologist pairs.
Assessed as response to the question, “What do you think the chances are that [patient] will be alive in 1 year and 5 years?” Nephrologists provided a specific estimate for each of their patients.
Assessed as response to the question, “What do you think the chances are that you will be alive in 1 year?” Overall, 59 pairs underwent analysis, excluding 3 pairs for whom data were missing for the patient’s estimate (of whom 2 were also missing data for the nephrologist’s estimate) (weighted κ for patient-nephrologist agreement, 0.08; rs = 0.09 [P < .001, McNemar test for primary and sensitivity analyses]).
Assessed as response to the question, “What do you think the chances are that you will be alive in 5 years?” Overall, 52 pairs underwent analysis, excluding 6 pairs for whom data were missing for the patient’s response, 2 pairs for whom data were missing for the nephrologist’s response, and 2 pairs for whom data were missing for both (weighted κ for patient-nephrologist agreement, 0.13; rs = 0.16[P < .001, McNemar test for primary and sensitivity analyses]).
Table 4 indicates that the degree of agreement between patients’ and nephrologists’ beliefs about transplant candidacy was only fair (κ = 0.35).27 Patients were significantly more likely than their nephrologists to report that they were transplant candidates (66% vs 39% [P = .008]), and 12 of 29 patients (41%) whose nephrologists said were not transplant candidates believed they were. Overall, optimistic transplant discordance was present in 24 of 57 patient-nephrologist pairs (42%).
Table 4.
Transplant Candidacya
| Patient Responseb | Nephrologist Responsec | |||
|---|---|---|---|---|
| Yes | No | Don’t Know | Total | |
| Yes | 20 (54) | 12 (32) | 5 (14) | 37 (66) |
| No | 2 (12) | 15 (88) | 0 | 17 (30) |
| Don’t know | 0 | 2 (100) | 0 | 2 (4) |
| Total | 22 (39) | 29 (52) | 5 (9) | 56 (100) |
Data are expressed as the number (percentage) of patient-nephrologist pairs. Overall, 56 pairs underwent analysis, excluding 6 pairs for whom data were missing for the patient’s response (of whom 2 were also missing data for the nephrologist’s response (κ = 0.35 for patient-nephrologist agreement [P = .008, McNemar test]).
Assessed as response to the question, “Do you think getting a kidney transplant is a possibility for you?”
Nephrologists were asked to report their belief about transplant candidacy for each of their patients individually.
Table 5 presents results for patients’ goals of care. Overall, 54% reported that, if they were seriously ill, they would want care focused on relieving pain and discomfort rather than extending life. Patients who thought they had a 90% chance or greater of being alive in 1 year were significantly more likely to prefer life-extending care than were those who reported a less than 90% chance (44% vs 9% [P = .045]). Patients who were more optimistic than their nephrologist about transplant likelihood were also more likely to report a preference for life-extending care (55% vs 23% [P = .054]).
Table 5.
Association Between Patients’ Goals of Care and Estimates of Prognosis and Optimistic Transplant Discordancea
| Patient’s Goals of Care, No. (%)b | ||||
|---|---|---|---|---|
| Prefer Care Focused on Life Extension | Prefer Care Focused on Relieving Pain and Discomfort | Don’t Know | Total | |
| Patient estimate of chances for 1-year survivalc | ||||
| ≥90% | 18 (44) | 20 (49) | 3 (7) | 41 (79) |
| <90% | 1 (9) | 8 (73) | 2 (18) | 11 (21) |
| Total | 19 (37) | 28 (54) | 5 (10) | 52 (100) |
| Optimistic transplant discordanced | ||||
| Yes | 12 (55) | 8 (36) | 2 (9) | 22 (42) |
| No | 7 (23) | 20 (67) | 3 (10) | 30 (58) |
| Total | 19 (37) | 28 (54) | 5 (10) | 52 (100) |
Percentages have been rounded and might not total 100. Data were missing for at least 1 of the questions below for 10 patients.
Assessed as patient response to the question, “If you were seriously ill, would you prefer care to (a) extend life, even if it meant more pain and discomfort, or (b) relieve pain and discomfort, even if it meant not living as long?”
Assessed as patient response to the question, “What do you think the chances are that you will be alive in 12 months?” (P = .045, Fisher exact test).
Defined as optimistic when patients reported a greater likelihood than their nephrologists that they would receive a transplant. Numbers represent patient-nephrologist pairs (P = .054, Fisher exact test).
The Kaplan-Meier survival curve for the 62 interviewed patients is shown in the eFigure in the Supplement. Survival was 93% at 1 year but decreased to 79% by 17 months and 56% by 23 months.
Discussion
In our study using interviews with 62 patients and their nephrologists, we found that seriously ill hemodialysis patients were significantly more optimistic than their nephrologists about their prognosis and transplant candidacy. In our sample, patients’ expectations about 1-year survival were more accurate than those of their nephrologists, whereas patients’ longer-term survival expectations dramatically overestimated even their 2-year survival rates. Only 6% of patients thought they had less than a 50% chance of being alive in 5 years, whereas actual survival at just less than 2 years of follow-up was only 56%. Meanwhile, nephrologists estimated that more than half the patients had a likelihood of 5-year survival below 40%, supporting the assertion that nephrologists were more accurate than patients about longer-term survival. Furthermore, more than one-third of patients whose nephrologists said they were not transplant candidates believed they were. Our finding that seriously ill hemodialysis patients overestimate their chances of survival compared with their physicians has been observed in patients with cancer5-8 and in surrogate decision makers for patients in intensive care units28-34 but has never been studied in patients with noncancer diagnoses. That hemodialysis patients and their nephrologists had discordant views about prognosis is not surprising because we found that not a single patient reported receiving an estimate of life expectancy from a nephrologist and that nephrologists reported having given such estimates to only 2 patients. Our findings are consistent with a Canadian study in which fewer than 10% of hemodialysis patients reported that their nephrologist had discussed prognosis.35 That study also found that more than 90% of patients with advanced kidney disease wanted prognostic information. However, although many patients want their physician to discuss prognosis with them, another study found that 25% of elderly patients did not.36 Therefore, clinicians should always elucidate a patient’s preferences before sharing prognostic estimates.
Perhaps of greater concern is our finding that nephrologists reported that, for 60% of patients, they would not provide any estimate of prognosis even if their patient insisted. This percentage of nondisclosure is higher than the percentage documented in the cancer literature37 and suggests that nephrologists maybe even more reluctant to discuss prognosis with their hemodialysis patients than physicians caring for patients with cancer. Recent qualitative work38 found that lack of confidence in predictions and concern about upsetting patients were barriers to nephrologists’ discussing prognosis; this issue deserves further research to design effective interventions to improve communication.
Our finding that patients are more optimistic than their nephrologists about the likelihood of transplant is a novel contribution to the literature and has important implications. Previous research comparing patients’ and physicians’ expectations about prognosis has focused on patients with cancer, for whom solid-organ transplant is not a treatment option. In contrast, for some seriously ill hemodialysis patients, a kidney transplant maybe possible, and kidney transplant has been shown to improve their prognosis.20 Patients should have an accurate understanding of their likelihood of transplant, so they can make informed medical decisions. Our findings raise the possibility that patients maybe making medical decisions based on an inaccurate assumption that they are likely to receive a kidney transplant.
More than half of patients interviewed stated that if they were seriously ill they would choose care focused on relieving pain and discomfort, even if it meant not living as long. Among those who thought their chance of being alive in 1 year was at least 90%, about half indicated a preference for comfort-focused care compared with nearly all patients who thought their chance was less than 90%. Previous work35,39,40 exploring treatment preferences for end-of-life care among patients with advanced kidney disease did not examine the association between prognostic expectations and goals of care. Our findings therefore have additional implications. First, because patients’ beliefs about prognosis were associated with their goals of care, sharing prognostic information with patients may affect medical decision making. Second, because more than half the interviewed patients indicated a preference for comfort-focused care if they were seriously ill, hemodialysis patients generally may receive more aggressive care at the end of life than they desire.
Our study has important limitations. First, our sample was limited to patients from 2 hemodialysis units affiliated with academic medical centers, which may limit generalizability. Second, our sample was relatively small, in large part because almost half the patients with a predicted 1-year mortality of 20% or greater met exclusion criteria, most commonly owing to cognitive impairment. Conversations about prognosis are arguably even more important with cognitively impaired patients and their health care proxies, who often face difficult treatment decisions toward the end of life. Therefore, future research exploring expectations and beliefs among the proxies of such patients would be valuable. Hispanic patients also made up a disproportionate share of excluded patients, and it is unclear whether our findings would be similar among Spanish-speaking patients. Nonetheless, our interview participation rate was 78%, which is quite high for a study involving in-depth interviews with seriously ill patients.41
Another limitation is that prognostic indices may be inaccurate for individual patients. Also of note, our survival data are based on hemodialysis unit-recorded deaths. These data could bias our survival estimates upward because deaths of patients who were no longer receiving hemodialysis at the units are not reflected in our data.
In addition, patients were asked about their goals of care if they were seriously ill, and hypothetical preferences may not reflect actual future preferences or use of aggressive care. Finally, although perceived prognosis was associated with goals of care, this association cannot be interpreted as causal. Certain types of patients may be predisposed to be more optimistic about prognosis and to prefer life-extending care independent of their prognostic optimism, in which case discussions about prognosis may not modify their decision making.
Conclusions
Our study suggests that seriously ill hemodialysis patients are more optimistic than their nephrologists about their prognosis and the likelihood of transplant and that nephrologists rarely disclose prognostic estimates to patients. In our sample, patients’ optimistic survival expectations were not inconsistent with actual survival at 1 year. However, between 1 and 2 years, actual survival rapidly declined, and patients’ expectations became markedly overoptimistic. The ability to accurately estimate prognosis in patients with noncancer diagnoses is increasingly being recognized as critical to patient-centered decision making,4 and a number of prognostic indices with good predictive properties exist for end-stage renal disease.13,16,17 As our ability to accurately prognosticate for seriously ill patients continues to advance, developing interventions to help providers communicate effectively with patients about prognosis will become increasingly important.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by grants from the National Institute of Nursing Research and the US Department of Health and Human Services Health Resources and Services Administration (Dr Wachterman) and by award UL1 RR 025758 from the National Institutes of Health (Harvard Catalyst and the Harvard Clinical and Translational Science Center).
Footnotes
Author Contributions: Dr Wachterman had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Wachterman, Marcantonio, Cohen, Phillips, and McCarthy.
Acquisition of data: Wachterman and McCarthy.
Analysis and interpretation of data: All authors.
Drafting of the manuscript: Wachterman.
Critical revision of the manuscript for important intellectual content: Marcantonio, Davis, Cohen, Waikar, Phillips, and McCarthy.
Statistical analysis: Wachterman, Davis, and McCarthy.
Obtained funding: Marcantonio, Phillips, and McCarthy.
Administrative, technical, and material support: Cohen, Waikar, Phillips, and McCarthy.
Study supervision: Marcantonio, Cohen, and McCarthy.
Additional Contributions: Mary Ersek, PhD, RN, University of Pennsylvania School of Nursing, and Benjamin Sommers, MD, PhD, Harvard School of Public Health, provided helpful feedback on earlier versions of this manuscript. They received no financial compensation for their contributions.
Disclaimer: The sponsors had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Conflict of Interest Disclosure: None reported.
Previous Presentations: This study was presented at the national meetings of the Society of General Internal Medicine; May 9, 2012; Orlando, Florida; and the American Society of Nephrology; November 2, 2012; San Diego, California.
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases. Kidney disease statistics for the United States. [October 26, 2012];2012 Jul 2; http://kidney.niddk.nih.gov/kudiseases/pubs/kustats/#23.
- 2.Collins AJ, Foley R, Herzog C, et al. Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis. 2008;51(1 suppl 1):S1–S320. doi: 10.1053/j.ajkd.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Gill TM. The central role of prognosis in clinical decision making. JAMA. 2012;307(2):199–200. doi: 10.1001/jama.2011.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith AK, Williams BA, Lo B. Discussing overall prognosis with the very elderly. N Engl J Med. 2011;365(23):2149–2151. doi: 10.1056/NEJMp1109990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siminoff LA, Fetting JH, Abeloff MD. Doctor-patient communication about breast cancer adjuvant therapy. J Clin Oncol. 1989;7(9):1192–1200. doi: 10.1200/JCO.1989.7.9.1192. [DOI] [PubMed] [Google Scholar]
- 6.Pronzato P, Bertelli G, Losardo P, Landucci M. What do advanced cancer patients know of their disease? a report from Italy. Support Care Cancer. 1994;2(4):242–244. doi: 10.1007/BF00365729. [DOI] [PubMed] [Google Scholar]
- 7.Eidinger RN, Schapira DV. Cancer patients’ insight into their treatment, prognosis, and unconventional therapies. Cancer. 1984;53(12):2736–2740. doi: 10.1002/1097-0142(19840615)53:12<2736::aid-cncr2820531233>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 9.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 10.Miskulin DC, Martin AA, Brown R, et al. Medical Directors, Dialysis Clinic, Inc. Predicting 1 year mortality in an outpatient haemodialysis population: a comparison of comorbidity instruments. Nephrol Dial Transplant. 2004;19(2):413–420. doi: 10.1093/ndt/gfg571. [DOI] [PubMed] [Google Scholar]
- 11.Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000;108(8):609–613. doi: 10.1016/s0002-9343(00)00371-5. [DOI] [PubMed] [Google Scholar]
- 12.Hemmelgarn BR, Manns BJ, Quan H, Ghali WA. Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis. 2003;42(1):125–132. doi: 10.1016/s0272-6386(03)00415-3. [DOI] [PubMed] [Google Scholar]
- 13.Cohen LM, Ruthazer R, Moss AH, Germain MJ. Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin J Am Soc Nephrol. 2010;5(1):72–79. doi: 10.2215/CJN.03860609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Couchoud C, Labeeuw M, Moranne O, et al. French Renal Epidemiology and Information Network (REIN) registry. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24(5):1553–1561. doi: 10.1093/ndt/gfn698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barrett BJ, Parfrey PS, Morgan J, et al. Prediction of early death in end-stage renal disease patients starting dialysis. Am J Kidney Dis. 1997;29(2):214–222. doi: 10.1016/s0272-6386(97)90032-9. [DOI] [PubMed] [Google Scholar]
- 16.Peralta CA, Shlipak MG, Judd S, et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305(15):1545–1552. doi: 10.1001/jama.2011.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tangri N, Stevens LA, Griffith J, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305(15):1553–1559. doi: 10.1001/jama.2011.451. [DOI] [PubMed] [Google Scholar]
- 18.Galla JH Renal Physicians Association; American Society of Nephrology. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol. 2000;11(7):1340–1342. doi: 10.1681/ASN.V1171340. [DOI] [PubMed] [Google Scholar]
- 19.Moss AH. Revised dialysis clinical practice guideline promotes more informed decision-making. Clin J Am Soc Nephrol. 2010;5(12):2380–2383. doi: 10.2215/CJN.07170810. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3(5):1379–1384. doi: 10.2215/CJN.00940208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knaus WA, Harrell FE, Jr, Lynn J, et al. The SUPPORT prognostic model: objective estimates of survival for seriously ill hospitalized adults. Ann Intern Med. 1995;122(3):191–203. doi: 10.7326/0003-4819-122-3-199502010-00007. [DOI] [PubMed] [Google Scholar]
- 24.SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (SUPPORT) JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 25.Kadan-Lottick NS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG. Psychiatric disorders and mental health service use in patients with advanced cancer: a report from the Coping With Cancer Study. Cancer. 2005;104(12):2872–2881. doi: 10.1002/cncr.21532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCarthy EP, Pencina MJ, Kelly-Hayes M, et al. Advance care planning and health care preferences of community-dwelling elders: the Framingham Heart Study. J Gerontol A Biol Sci Med Sci. 2008;63(9):951–959. doi: 10.1093/gerona/63.9.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Altman D. Practical Statistics for Medical Research. London, England: Chapman & Hall; 1991. [Google Scholar]
- 28.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers’ interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156(5):360–366. doi: 10.1059/0003-4819-156-5-201203060-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azoulay E, Chevret S, Leleu G, et al. et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28(8):3044–3049. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 30.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. The language of prognostication in intensive care units. Med Decis Making. 2010;30(1):76–83. doi: 10.1177/0272989X08317012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyd EA, Lo B, Evans LR, et al. “It’s not just what the doctor tells me”: factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38(5):1270–1275. doi: 10.1097/CCM.0b013e3181d8a217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182(7):905–909. doi: 10.1164/rccm.201002-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zier LS, Burack JH, Micco G, et al. Doubt and belief in physicians’ ability to prognosticate during critical illness: the perspective of surrogate decision makers. Crit Care Med. 2008;36(8):2341–2347. doi: 10.1097/CCM.0b013e318180ddf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meadow W, Pohlman A, Frain L, et al. Power and limitations of daily prognostications of death in the medical intensive care unit. Crit Care Med. 2011;39(3):474–479. doi: 10.1097/CCM.0b013e318205df9b. [DOI] [PubMed] [Google Scholar]
- 35.Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5(2):195–204. doi: 10.2215/CJN.05960809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahalt C, Walter LC, Yourman L, Eng C, Perez-Stable EJ, Smith AK. “Knowing is better”: preferences of diverse older adults for discussing prognosis. J Gen Intern Med. 2012;27(5):568–575. doi: 10.1007/s11606-011-1933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med. 2001;134(12):1096–1105. doi: 10.7326/0003-4819-134-12-200106190-00009. [DOI] [PubMed] [Google Scholar]
- 38.Schell JO, Patel UD, Steinhauser KE, Ammarell N, Tulsky JA. Discussions of the kidney disease trajectory by elderly patients and nephrologists: a qualitative study. Am J Kidney Dis. 2012;59(4):495–503. doi: 10.1053/j.ajkd.2011.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morton RL, Tong A, Howard K, Snelling P, Webster AC. The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. BMJ. 2010;340:c112. doi: 10.1136/bmj.c112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davison SN, Simpson C. Hope and advance care planning in patients with end stage renal disease: qualitative interview study. BMJ. 2006;333(7574):886. doi: 10.1136/bmj.38965.626250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Casarett D. Ethical considerations in end-of-life care and research. J Palliat Med. 2005;8(suppl 1):S148–S160. doi: 10.1089/jpm.2005.8.s-148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.