Abstract
Objectives
We estimated race/ethnicity-specific incident AIDS diagnosis rates (IARs) among people who inject drugs (PWID) in U.S. metropolitan statistical areas (MSAs) over time to assess the change in disparities after highly active antiretroviral therapy (HAART) dissemination.
Methods
We compared IARs and 95% confidence intervals (CIs) for black/African American and Hispanic/Latino PWID with those of white PWID in 93 of the most populous MSAs. We selected two three-year periods from the years immediately preceding HAART (1993–1995) and the years with the most recent available data (2005–2007). To maximize stability, we aggregated data across three-year periods, and we aggregated data for black/African American and Hispanic/Latino PWID for most comparisons with data for white PWID. We assessed disparities by comparing IAR 95% CIs for overlap.
Results
IARs were significantly higher for black/African American and Hispanic/Latino PWID than for white PWID in 81% of MSAs in 1993–1995 and 77% of MSAs in 2005–2007. MSAs where disparities became non-significant over time were concentrated in the West. Significant differences were more frequent in comparisons between black/African American and white PWID (85% of MSAs in 1993–1995, 79% of MSAs in 2005–2007) than in comparisons between Hispanic/Latino and white PWID (53% of MSAs in 1993–1995, 56% of MSAs in 2005–2007). IARs declined modestly across racial/ethnic groups in most MSAs.
Conclusions
AIDS diagnosis rates continue to be substantially higher for black/African American and Hispanic/Latino PWID than for white PWID in most large MSAs. This finding suggests a need for increased targeting of prevention and treatment programs, as well as research on MSA-level conditions that may serve to maintain the disparities.
Together, non-Hispanic black people/African Americans (hereafter, black people) and Hispanic or Latino people (hereafter, Hispanic people) are estimated to comprise about half of the population of people who inject drugs (PWID) in the U.S.,1 but they comprise about three-quarters of PWID who have been diagnosed with acquired immunodeficiency syndrome (AIDS).2 Harm-reduction programs are believed to have been partly responsible for reducing human immunodeficiency virus (HIV) transmission among PWID since the 1980s,3 and highly active antiretroviral therapy (HAART) has greatly reduced rates of progression to AIDS.4 These benefits, however, may not have spread evenly across racial/ethnic groups and localities. Racial/ethnic disparities in AIDS diagnosis rates may reflect disparities in HIV incidence, progression to AIDS among people who are HIV-positive, and time to diagnosis among people living with AIDS.5
From a fundamental cause perspective, racial/ethnic AIDS incidence disparities reflect underlying differences in social conditions and access to resources, including HIV prevention and treatment.6 These disparities can include proximal factors, such as access to harm-reduction programs and high-quality health care, and more distal factors, such as risk of incarceration and potential exposure to HIV from living in neighborhoods with high HIV prevalence.7 The social conditions that link race/ethnicity to HIV/AIDS risk act through multiple mechanisms, so that attempts to reduce disparities by eliminating one mechanism may fail because other mechanisms remain. The fundamental cause perspective suggests that improvements in treatment and prevention are likely to benefit white people more than black or Hispanic people, potentially maintaining or amplifying disparities over time.6,8,9
Nationally, there is evidence of decline in racial/ethnic disparities in HIV or AIDS diagnosis in the U.S. across risk groups. The magnitude of black-white and Hispanic-white AIDS diagnosis disparities declined significantly from 2000 to 2009, except for adolescent and young adult males (aged 13–24 years).5 From 2001 to 2004, the rate of HIV diagnosis declined by 6.8% annually among black people and by 4.7% among Hispanic people, but increased by 1.4% annually among white people.10 In an analysis of 2007 HIV surveillance data, black-white and Hispanic-white disparities in large urban areas were greatest in the Northeast, South, and Midwest.11 Results of that study suggest that changing HIV disparities may be related to changing trends in HIV incidence by risk category regardless of race/ethnicity, and contacts among risk groups and racial/ethnic groups over time.
Assessing disparities in AIDS diagnoses in specific geographic areas can help us study the fundamental causes of the disparities. Some of the mechanisms linking race/ethnicity to AIDS act outside of the direct control of individuals. For example, living in an area where HIV treatment is unavailable or is of poor quality can impact everyone in the area who is HIV-positive and is difficult to contend with individually, short of moving to an area with better treatment options. Area-specific AIDS prevalence rates reflect the accumulation of individual risk behaviors, the concentration of HIV in sex and injection networks, the social conditions in the area that affect risk behaviors, and HIV and drug use treatment and prevention programs.11,12 By comparing racial/ethnic differences in area-specific AIDS incidence rates across time, we can indirectly assess the system of mechanisms linking race/ethnicity and AIDS risk and identify where conditions are improving or worsening. Concurrently, data on changes in area-level racial/ethnic disparities can be used to more completely identify and understand those mechanisms.
To assess changes in racial/ethnic disparities, we compared new (incident) AIDS diagnosis rates (IARs) for black and Hispanic PWID with those of non-Hispanic white (hereafter, white) PWID in U.S. metropolitan areas over time.
METHODS
To calculate IARs, we obtained yearly data on the number of incident AIDS diagnoses and the number of PWID living with AIDS stratified by racial/ethnic group from 1993–2007 for 94 of the most populous U.S. MSAs. We used the MSA as the unit of analysis because MSAs are likely to reflect social and economic integration among resident injection drug users (IDUs).13 MSAs represent socially and economically integrated entities comprising contiguous counties that contain a central city of ≥50,000 people.14
The AIDS data were drawn from a complete count of new AIDS diagnoses reported to the Centers for Disease Control and Prevention (CDC). They were not subject to sampling error but were subject to random variation and may contain nonsampling error related to incomplete reporting and misclassification of transmission risk or of race/ethnicity. This error can have a greater impact where the data are sparse. Some MSAs in our study reported few AIDS diagnoses among PWID in some years, particularly when stratified by race/ethnicity. To minimize the potential impact of nonsampling error, we compared aggregated data from 1993–1995 (the three years immediately preceding HAART dissemination) with aggregated data from 2005–2007 (the three years with the most recent data). For each three-year period in each MSA, we calculated diagnosis rates by dividing the number of PWID AIDS diagnoses by the estimated number of PWID at risk for AIDS.
The estimated yearly numbers of PWID of each racial/ethnic group in each MSA have been developed in a series of studies, using multiple data sources to account for difficulties in assessing this hard-to-reach population.1,15–19 These sources included data from published national and MSA-specific research studies, and data on HIV counseling and testing, drug treatment, arrests for heroin and cocaine possession, and new AIDS diagnoses, adjusted for HIV prevalence. Although these PWID population estimates show strong consistency with external validators (i.e., deaths due to hepatitis C and drug poisoning), it is important to note that they contain error and may be biased to underrepresent PWID who did not interact with the health-care or criminal justice systems.1 PWID living with AIDS were excluded from the denominators to calculate IARs for the PWID populations at risk for AIDS. For the purposes of this study, PWID at risk for AIDS could be HIV-infected or HIV-uninfected. We combined black and Hispanic PWID data for most comparisons with white PWID to minimize the exclusion of MSAs with no AIDS diagnoses among black or Hispanic PWID in either time period from the analysis. Hispanic PWID could be of any race.
To facilitate comparisons, we calculated 95% confidence intervals (CIs) for each IAR. For analytic purposes, the number of AIDS diagnoses that actually occurred can be viewed as one of a large series of possible results that could have occurred under the same or similar conditions. As infrequent events, AIDS diagnoses can be considered as occurring in a Poisson-distributed function. Under this assumption, we calculated IAR 95% CIs using standard formulas when there were ≥100 diagnoses, and using tabled values when there were <100 diagnoses.20,21 The 95% CIs reflect the range of IARs that could have occurred under the same or similar conditions 95 times out of 100. These CIs are based on estimates that reflect only random variation in the numerator and not error in the denominator PWID population estimates.
We considered various methods for assessing change in IAR disparities, including comparing absolute and relative differences in IAR values and ratios.22,23 The choice of disparity measurement can affect the interpretation of results.23,24 Most absolute change measures (e.g., rate differences) were sensitive to high IARs in the early period so that disparities appeared to decrease simply because the overall rates declined. Conversely, relative measures (e.g., rate ratios [RRs]) were sensitive to small values, so that disparities appeared to vary greatly in MSAs with small but changing numbers of diagnoses.
One method for comparing area-level rates for important differences is to compare CIs for overlap. If the CIs do not overlap, the difference can be considered significant at the 95% level.21,25 Comparing IAR CIs for overlap is an absolute comparison that takes into account the precision of the IARs. We chose to focus on the CI overlap method because our main interest was in the frequency of important disparities.
We calculated IARs and their respective 95% CIs for each MSA, time period, and racial/ethnic group. IARs are scaled (multiplied by 10,000) for presentation. To provide information on the magnitude of the disparities, we calculated IAR ratios (relative risks) by dividing the combined black/Hispanic PWID IAR by the white PWID IAR. We compared the frequency of IAR disparities by region (Northeast, South, Midwest, and West) to summarize their geographic distribution.
Data from 93 MSAs were included in the analysis. One MSA (San Juan-Bayamon, Puerto Rico) was excluded because virtually all PWID diagnoses were among Hispanic people. In the 2005–2007 period, racial/ethnic comparisons were not made in two additional MSAs (Ann Arbor, Michigan, and Ventura, California) because no incident AIDS diagnoses were reported among white PWID. IARs for black PWID were not calculated for two MSAs in 2005–2007 because there were no diagnoses reported among them. IARs were not calculated for Hispanic PWID in five MSAs in 1993–1995 and in two MSAs in 2005–2007 for the same reason. IARs for PWID who reported Asian, American Indian/Alaska Native, and Native Hawaiian/other Pacific Islander race/ethnicity were not analyzed because the numbers of diagnoses were too small.
RESULTS
Racial/ethnic group-specific IARs, 95% CIs, and IAR ratios comparing the combined black/Hispanic PWID group with white PWID for both time periods in each MSA are presented in the Table. There were modest declines in IARs among all three racial/ethnic groups in most MSAs. IARs were significantly greater for black/Hispanic than for white PWID in 81% of MSAs (75 of 93) in 1993–1995 and 77% of MSAs (70 of 91) in 2005–2007. Of the 75 MSAs with significant disparities in 1993–1995, disparities remained significant in 65 MSAs in 2005–2007; there were no longer significant disparities in nine MSAs and disparities were not computed in one MSA (Ann Arbor). Of the nine MSAs where there were no longer significant disparities over time, the change reflected a reduction in IARs for black/Hispanic relative to white PWID in seven MSAs: Fresno, California; Honolulu, Hawaii; Sacramento, California; Salt Lake City-Ogden, Utah; San Diego, California; San Francisco, California; and Tacoma, Washington. The change in Akron, Ohio, reflected a greater increase in IARs for white PWID relative to the increase for black/Hispanic PWID, while the change in Indianapolis, Indiana, reflected a wider CI for black/Hispanic PWID in 2005–2007. Of the 18 MSAs where IARs were not significantly different between black/Hispanic and white PWID in 1993–1995, IARs were significantly different in five MSAs in 2005–2007 (an IAR was not computed for Ventura). These changes reflected an increase in IARs for black/Hispanic PWID in Columbus, Ohio, and Knoxville, Tennessee, and a greater decrease for white than for black/Hispanic PWID in Denver, Colorado; Grand Rapids/Muskegon/Holland, Michigan; and Tucson, Arizona.
Table.
AIDS diagnosis rates per 10,000 population and 95% CIs for people who inject drugs, by race/ethnicity, and RRs comparing non-Hispanic black/African American and Hispanic/Latino people who inject drugs with those of non-Hispanic white people who inject drugs: 93 U.S. metropolitan areas, 1993–1995 and 2005–2007
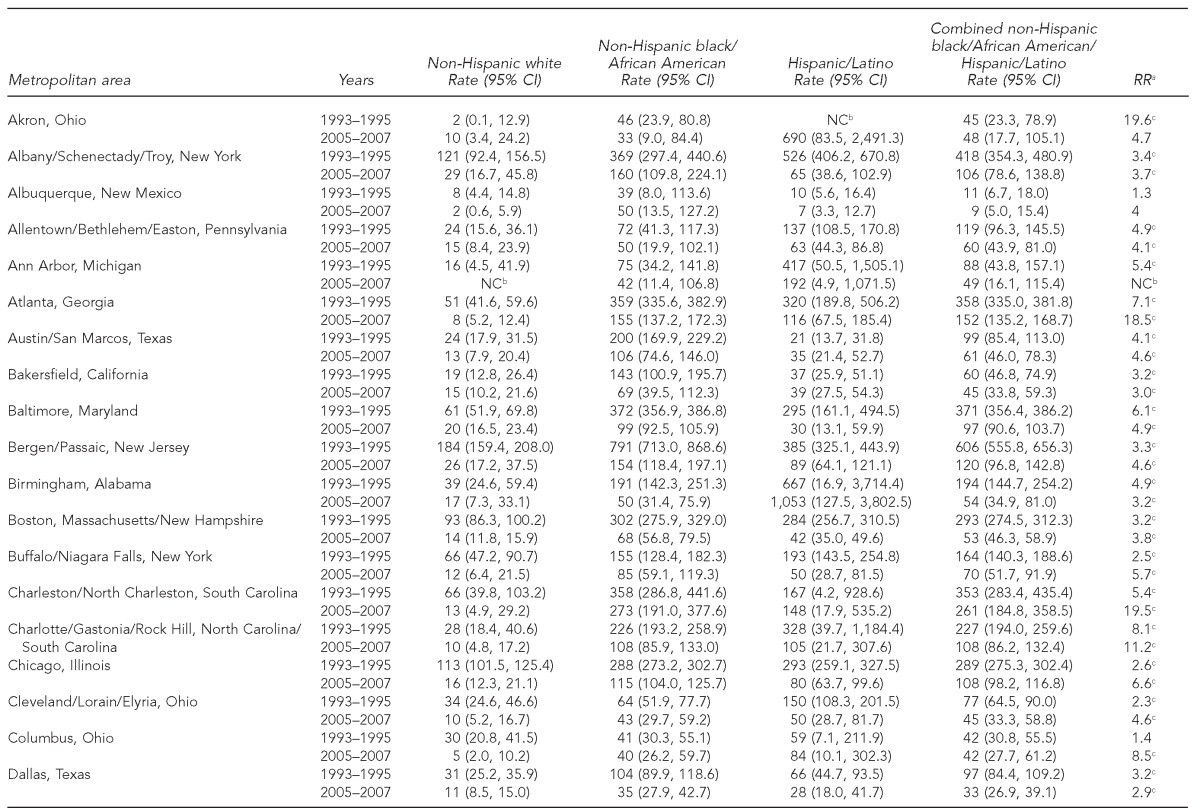
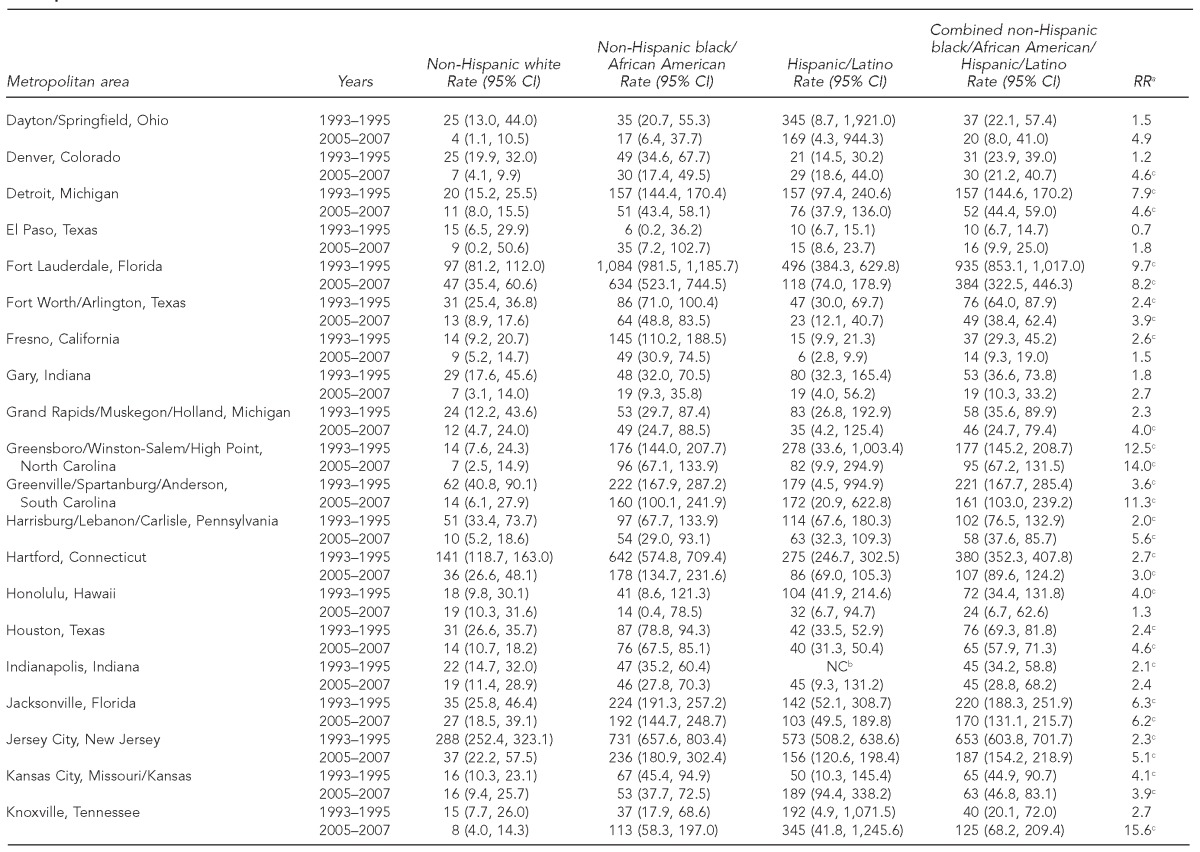
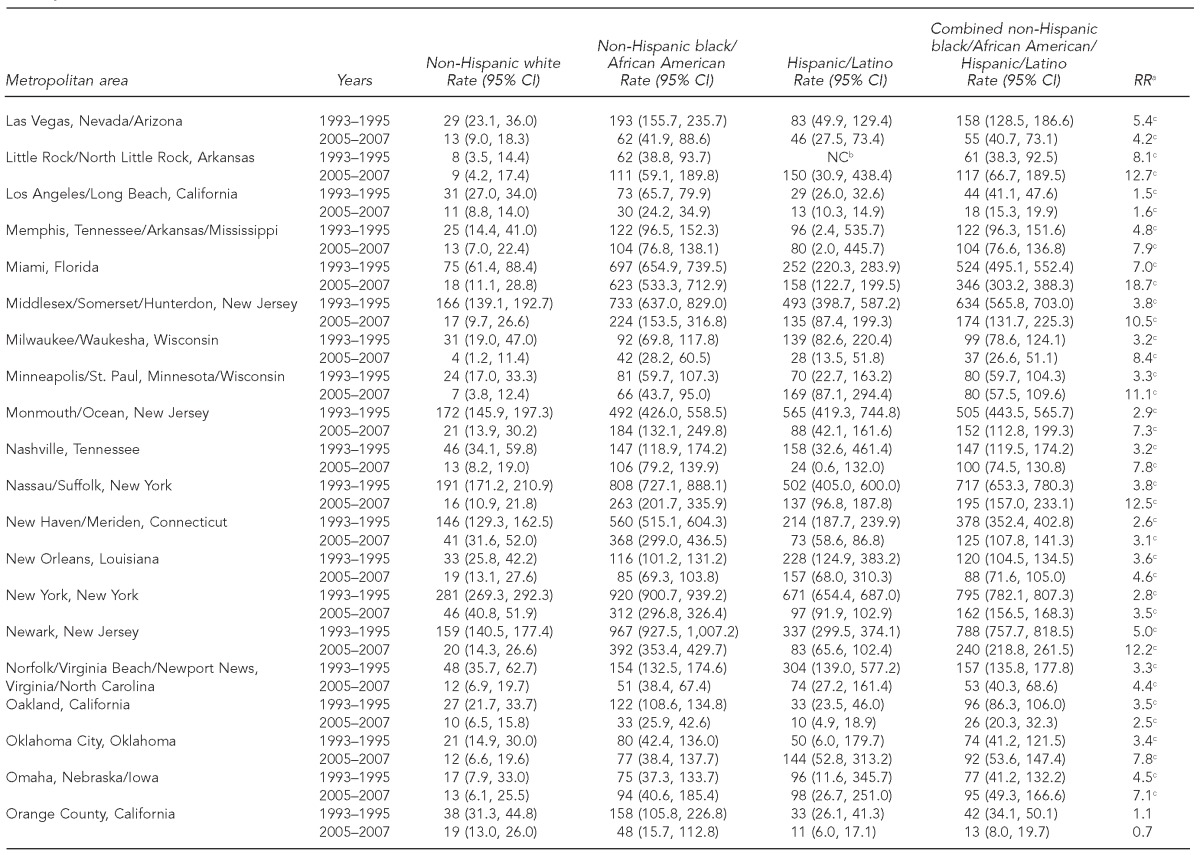
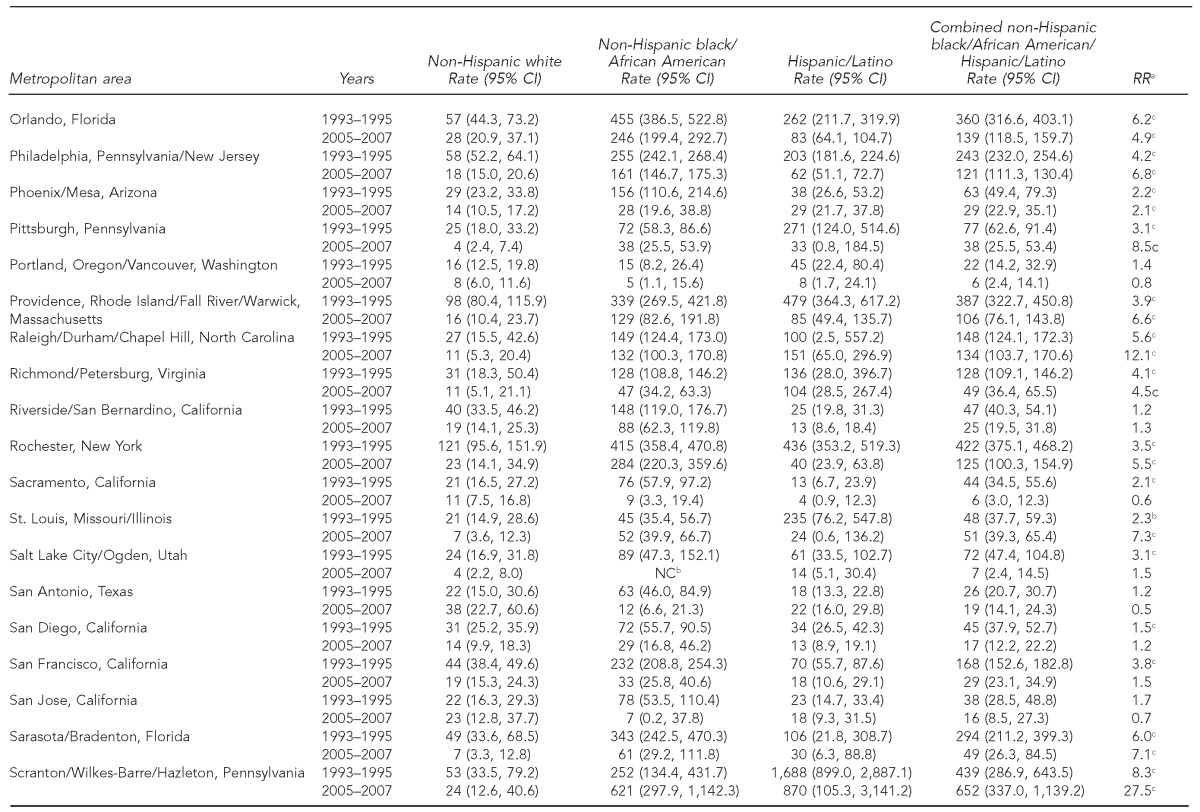
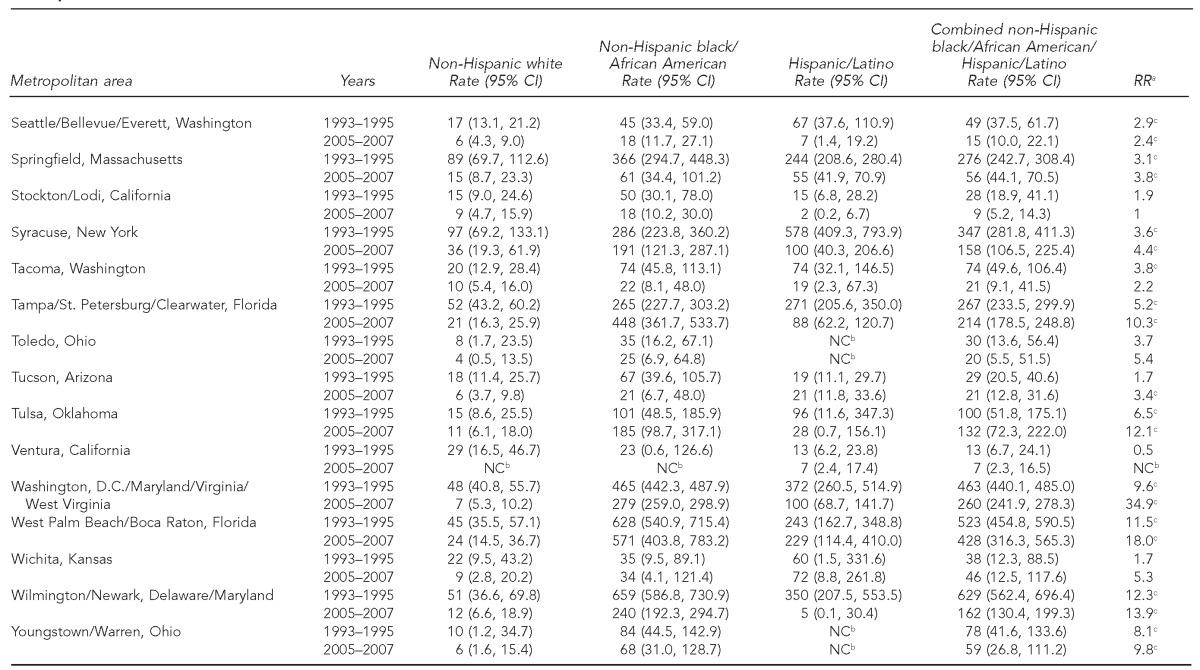
aRR comparing the AIDS diagnosis rate for non-Hispanic black/African American and Hispanic people who inject drugs combined with the rate for non-Hispanic white people who inject drugs
bCould not be computed because no diagnoses were reported in one or more groups or time periods
cStatistically significant difference between non-Hispanic black/African American and Hispanic people who inject drugs combined and non-Hispanic white people who inject drugs at the p≤0.05 level by non-overlap of CIs
AIDS = acquired immunodeficiency syndrome
CI = confidence interval
RR = rate ratio
NC = not calculable
IAR ratio values comparing the combined black/Hispanic PWID group with white PWID were mostly quite large across both time periods, although the highest values tended to be in MSAs with relatively fewer diagnoses. In MSAs where black/Hispanic IARs were significantly higher than those for white PWID in 1993–1995, IAR ratios were above 2.0 in 97% and above 10.0 in 5% of the MSAs. In MSAs where black/Hispanic IARs were significantly higher than those for white PWID in 2005–2007, IAR ratios were above 2.0 in 98% and above 10.0 in 28% of the MSAs.
We also compared black and Hispanic PWID IARs separately with white PWID IARs across time. IARs for black PWID were significantly greater than those for white PWID in 85% of MSAs (79 of 93) in 1993–1995 and in 79% of MSAs (71 of 90) in 2005–2007. IARs for Hispanic PWID were significantly greater than those for white PWID in 53% of MSAs (47 of 88) in 1993–1995 and in 56% of MSAs (50 of 89) in 2005–2007.
Comparisons can be made across groups, time, and/or MSAs. For example, it can be seen that in the Miami, Florida, MSA, the IAR ratio increased because IARs decreased for white PWID by 76% between time periods, but decreased for the combined black/Hispanic group by only 34%. By comparing their respective CIs, IARs were significantly lower in 2005–2007 compared with 1993–1995 for the combined black/Hispanic group, as well as for white and Hispanic PWID, but not for black PWID.
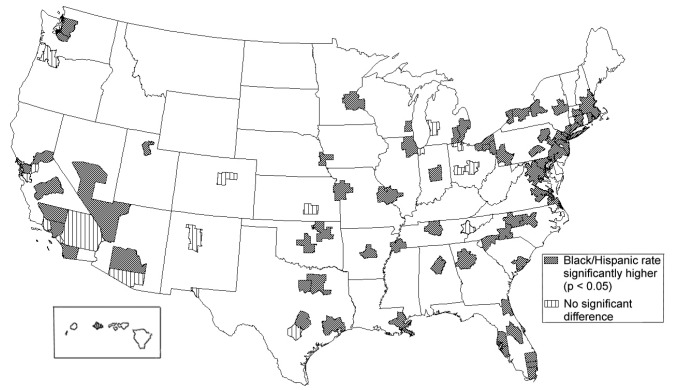
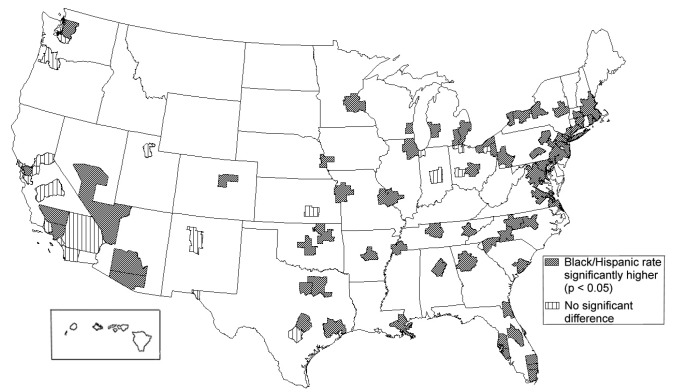
As shown in Figure 1, in 1993–1995, significant differences between black/Hispanic and white PWID IARs were more frequent in the Northeast (21 of 21 MSAs, 100%) and South (29 of 32 MSAs, 91%) than in the Midwest (12 of 18 MSAs, 67%) or West (13 of 22 MSAs, 59%). As shown in Figure 2, in 2005–2007, they were also more frequent in the Northeast (21 of 21 MSAs, 100%) and South (30 of 32 MSAs, 94%) than in the Midwest (11 of 17 MSAs, 65%) or West (eight of 21 MSAs, 38%). All seven of the MSAs in which significant IAR differences in the early time period became non-significant in the later time period, reflecting reduced black/Hispanic IARs relative to white IARs, were in the West. Of the five MSAs in which non-significant IAR differences in the early time period became significant in the later time period, reflecting increased black/Hispanic IARs relative to white IARs, two were in the South, two were in the West, and one was in the Midwest.
Figure 1.
Disparities in AIDS diagnosis rates comparing non-Hispanic black/African American and Hispanic/Latino people who inject drugs with non-Hispanic white people who inject drugs: 93 U.S. metropolitan areas, 1993–1995
AIDS = acquired immunodeficiency syndrome
Figure 2.
Disparities in AIDS diagnosis rates comparing non-Hispanic black/African American and Hispanic/Latino people who inject drugs with non-Hispanic white people who inject drugs: 91 U.S. metropolitan areas, 2005–2007
AIDS = acquired immunodeficiency syndrome
DISCUSSION
AIDS diagnosis rates continue to be substantially higher for black and Hispanic PWID than for white PWID in most large MSAs more than a decade after the introduction of HAART. In seven MSAs, IARs for the combined black/Hispanic PWID group declined more rapidly than for white PWID, resulting in IARs that were no longer significantly different. All seven were located in the West; five were in California and one each was in Hawaii and Utah. Research is needed to determine the extent to which the IAR ratio reductions in these MSAs reflected changes in trends in HIV incidence by risk category and mixing between risk groups and/or effects of interventions, such as harm-reduction services, other HIV prevention efforts, or HAART utilization. For the remaining 86 MSAs, there was little or no reduction in disparities relative to white PWID. National trends showing declining racial/ethnic disparities in AIDS or HIV diagnosis overall may provide limited information regarding the trends for PWID and may mask MSA-specific trends. The lower frequency of significant differences in Hispanic-white comparisons than in black-white comparisons in both time periods is partly a function of the wider CIs for Hispanic IARs, resulting from the smaller size of Hispanic PWID populations—and fewer concomitant diagnoses—in many MSAs.
Although we had no HAART data available for this study, we speculate based on studies of individuals that systematic differences in HAART use by race/ethnicity and/or by MSA may have influenced our results. For example, racial/ethnic IAR disparities may be related to lower access to and/or adherence to HAART among HIV-infected black and Hispanic people compared with white people.26 Black and Hispanic PWID have been found to progress to AIDS more rapidly following HIV diagnosis than white PWID,27 due in part to late HIV diagnosis,28 lower ART adherence, and poorer HIV care management.26 Studies have shown HAART to be about as effective among PWID as among non-PWID,29,30 so research on HIV treatment overall may be useful for understanding HIV treatment for PWID. Recent cohort data suggest that, of HIV-infected people overall, those who reside in the South and those who are nonwhite have more HIV-related medical events and later HAART initiation.31
Because our outcome represents both infection with HIV and progression to AIDS, other factors beyond HAART may also be important. Recent research has found overall AIDS diagnosis rates in localities to be correlated with the racial/ethnic composition of the population and potential social determinants of health, including the proportion of the population that is unmarried and the population density, possibly reflecting HIV transmission through sexual networks.32
Social determinants of health, believed to underlie racial/ethnic disparities, have received increasing attention by the U.S. Department of Health and Human Services since 1985,33–36 and eliminating HIV disparities has been an overarching goal of CDC since at least 2001.37–39 The National HIV/AIDS Strategy, released by the White House in 2010, includes reducing HIV-related disparities as one of its major goals.39 Efforts have included working with local health departments and community leaders to promote counseling and testing, increasing treatment for sexually transmitted diseases, publishing guidelines and recommendations, sponsoring scientific meetings and research, promoting the diffusion of effective behavioral prevention interventions, and establishing the Enhanced Comprehensive HIV Prevention Planning project in 12 jurisdictions with the greatest HIV burden.40–43 This critical work acknowledges the multiple mechanisms underlying the disparities and the need for comprehensive prevention and treatment strategies.41 The data from this study can be used to indirectly assess associations over time with the MSA-level presence of HIV prevention and treatment programs and policies for PWID, and targeting of prevention and treatment programs for black and Hispanic PWID.
Our results are consistent with fundamental cause theory in the sense that, despite these efforts, IARs remained substantially higher for black and Hispanic PWID than for white PWID in the vast majority of MSAs. Research is needed to determine the extent to which differences in previously identified mechanisms linking race/ethnicity to AIDS diagnosis among PWID can be addressed more effectively, or whether more basic differences in social conditions must be considered, such as those related to residential segregation and policing practices.7,44–46
Limitations
Because our data were aggregated at the MSA level, the potential mechanisms underlying the observed disparities should not be assumed to have operated in the same way at the individual level. The method of comparing CIs for overlap is a conservative test of significant difference. Some differences may have been statistically significant by other tests even when the CIs overlapped.21 At the same time, our error calculations did not account for error in the estimated numbers of PWID at risk for AIDS in the denominators; thus, they may have overestimated the number of significant differences. The overall results may underestimate racial/ethnic disparities in 2005–2007 because we excluded two MSAs that reported no new diagnoses among white PWID but did report new diagnoses among black and/or Hispanic PWID.
CONCLUSIONS
Black and Hispanic PWID continue to be diagnosed with AIDS at significantly higher rates than white PWID in most large MSAs. Achieving equality in health outcomes among racial/ethnic subpopulations is an important goal of public health.33,36,47 Therefore, greater efforts are needed in more MSAs to eliminate IAR disparities. The limited decline in disparities suggests a need for increased targeting of PWID HIV prevention and treatment programs48–50 and a need for research on MSA-level conditions that may convey an increased risk of HIV infection and/or progression to AIDS for black or Hispanic PWID.44 These conditions may include economic conditions; policing practices; harm-reduction and other HIV education and prevention programs; health-care utilization, including HIV testing and HAART; as well as trends in population age structure, residence, immigration, HIV risk networks, and mixing.49,51–53
Footnotes
This study was supported by a grant from the U.S. National Institute on Drug Abuse (R01 DA013336). The National Development and Research Institutes, Inc., Institutional Review Board approved a waiver for this study because it was based on surveillance data, and no human subjects were involved. The authors acknowledge the National Institutes of Health-funded Center for Drug Use and HIV Research (P30 DA121041) for its support and assistance. Preliminary results from this study were presented at the XIX International AIDS Conference, July 22–27, 2012, in Washington, D.C.
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Tempalski B, Pouget ER, Cleland CM, Brady JE, Cooper HL, Hall HI, et al. Trends in the population prevalence of people who inject drugs in US metropolitan areas 1992–2007. PLoS One. 2013;8:e64789. doi: 10.1371/journal.pone.0064789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) Atlanta: CDC; 2009. HIV/AIDS surveillance supplemental report: cases of HIV infection and AIDS in the United States and dependent areas, by race/ethnicity, 2003–2007. [Google Scholar]
- 3.Wodak A, McLeod L. The role of harm reduction in controlling HIV among injecting drug users. AIDS. 2008;22(Suppl 2):S81–92. doi: 10.1097/01.aids.0000327439.20914.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vlahov D, Galai N, Safaeian M, Galea S, Kirk GD, Lucas GM, et al. Effectiveness of highly active antiretroviral therapy among injection drug users with late-stage human immunodeficiency virus infection. Am J Epidemiol. 2005;161:999–1012. doi: 10.1093/aje/kwi133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.An Q, Prejean J, Hall HI. Racial disparity in U.S. diagnoses of acquired immune deficiency syndrome, 2000–2009. Am J Prev Med. 2012;43:461–6. doi: 10.1016/j.amepre.2012.07.040. [DOI] [PubMed] [Google Scholar]
- 6.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No:80-94. [PubMed] [Google Scholar]
- 7.Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35(12 Suppl):S13–8. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 8.Rubin MS, Colen CG, Link BG. Examination of inequalities in HIV/AIDS mortality in the United States from a fundamental cause perspective. Am J Public Health. 2010;100:1053–9. doi: 10.2105/AJPH.2009.170241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC health disparities and inequalities report—United States, 2011. MMWR Morb Mortal Wkly Rep. 2011;60(Suppl):1–124. [PubMed] [Google Scholar]
- 10.Racial/ethnic disparities in diagnoses of HIV/AIDS—33 states, 2001–2004. MMWR Morb Mortal Wkly Rep. 2006;55(5):121–5. [PubMed] [Google Scholar]
- 11.Hall HI, Espinoza L, Benbow N, Hu YW. Epidemiology of HIV infection in large urban areas in the United States. PLoS One. 2010;5:e12756. doi: 10.1371/journal.pone.0012756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.An Q, Prejean J, McDavid Harrison K, Fang X. Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. Am J Public Health. 2013;103:120–6. doi: 10.2105/AJPH.2012.300853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pierce TG. Gen-X junkie: ethnographic research with young white heroin users in Washington, DC. Subst Use Misuse. 1999;34:2095–114. doi: 10.3109/10826089909039440. [DOI] [PubMed] [Google Scholar]
- 14.Office of Management and Budget (US) Standards for defining metropolitan and micropolitan statistical areas. Fed Reg. 2000;65:8228–38. [Google Scholar]
- 15.Brady JE, Friedman SR, Cooper HL, Flom PL, Tempalski B, Gostnell K. Estimating the prevalence of injection drug users in the U.S. and in large U.S. metropolitan areas from 1992 to 2002. J Urban Health. 2008;85:323–51. doi: 10.1007/s11524-007-9248-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pouget ER, Friedman SR, Cleland CM, Tempalski B, Cooper HL. Estimates of the population prevalence of injection drug users among Hispanic residents of large U.S. metropolitan areas. J Urban Health. 2012;89:527–64. doi: 10.1007/s11524-012-9670-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper HL, Brady JE, Friedman SR, Tempalski B, Gostnell K, Flom PL. Estimating the prevalence of injection drug use among black and white adults in large U.S. metropolitan areas over time (1992–2002): estimation methods and prevalence trends. J Urban Health. 2008;85:826–56. doi: 10.1007/s11524-008-9304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmberg SD. The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. Am J Public Health. 1996;86:642–54. doi: 10.2105/ajph.86.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedman SR, Tempalski B, Cooper H, Perlis G, Keem M, Friedman R, et al. Estimating numbers of injecting drug users in metropolitan areas for structural analyses of community vulnerability and for assessing relative degrees of service provision for injecting drug users. J Urban Health. 2004;81:377–400. doi: 10.1093/jurban/jth125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM, Sutton PD. Births: final data for 2001. Natl Vital Stat Rep. 2002 Dec 18;51:1–103. [PubMed] [Google Scholar]
- 21.Kleinman JC, Kiely JL. Infant mortality. Healthy People 2000 Stat Notes. 1991;1:1–10. [PubMed] [Google Scholar]
- 22.Hoover K, Bohm M, Keppel K. Measuring disparities in the incidence of sexually transmitted diseases. Sex Transm Dis. 2008;35(12 Suppl):S40–4. doi: 10.1097/OLQ.0b013e3181886750. [DOI] [PubMed] [Google Scholar]
- 23.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim I, Mays V, et al. Methodological issues in measuring health disparities. Vital Health Stat 2. 2005;(141) [PMC free article] [PubMed] [Google Scholar]
- 24.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 25.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: final data for 2006. Natl Vital Stat Rep. 2009 Jan 7;57:1–104. [PubMed] [Google Scholar]
- 26.Simoni JM, Huh D, Wilson IB, Shen J, Goggin K, Reynolds NR, et al. Racial/ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60:466–72. doi: 10.1097/QAI.0b013e31825db0bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grigoryan A, Hall HI, Durant T, Wei X. Late HIV diagnosis and determinants of progression to AIDS or death after HIV diagnosis among injection drug users, 33 US states, 1996–2004. PLoS One. 2009;4:e4445. doi: 10.1371/journal.pone.0004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2011;14:65–81. doi: 10.1007/s10903-011-9497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lima VD, Nosyk B, Wood E, Kozai T, Zhang W, Chan K, et al. Assessing the effectiveness of antiretroviral regimens in cohort studies involving HIV-positive injection drug users. AIDS. 2012;26:1491–500. doi: 10.1097/QAD.0b013e3283550b68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werb D, Mills EJ, Montaner JS, Wood E. Risk of resistance to highly active antiretroviral therapy among HIV-positive injecting drug users: a meta-analysis. Lancet Infect Dis. 2010;10:464–9. doi: 10.1016/S1473-3099(10)70097-9. [DOI] [PubMed] [Google Scholar]
- 31.Meditz AL, MaWhinney S, Allshouse A, Feser W, Markowitz M, Little S, et al. Sex, race, and geographic region influence clinical outcomes following primary HIV-1 infection. J Infect Dis. 2011;203:442–51. doi: 10.1093/infdis/jiq085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song R, Hall HI, Harrison KM, Sharpe TT, Lin LS, Dean HD. Identifying the impact of social determinants of health on disease rates using correlation analysis of area-based summary information. Public Health Rep. 2011;126(Suppl 3):70–80. doi: 10.1177/00333549111260S312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Department of Health and Human Services (US) Washington: Government Printing Office (US); 1985. Report of the Secretary's Task Force on black and minority health. [Google Scholar]
- 34.Department of Health and Human Services (US) DHHS Publication No. (PHS) 91-50212. Washington: HHS; 1991. Healthy people 2000: national health promotion and disease prevention objectives—full report. [Google Scholar]
- 35.Department of Health and Human Services (US) 2nd ed. Washington: Government Printing Office (US); 2000. Healthy people 2010: understanding and improving health. [Google Scholar]
- 36.Department of Health and Human Services (US) Healthy people 2020: final review. Hyattsville (MD): HHS. 2011. [cited 2013 Aug 6]. Also available from: URL: http://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf.
- 37.Centers for Disease Control and Prevention (US) Atlanta: CDC; 2001. HIV prevention strategic plan through 2005. [Google Scholar]
- 38.Sharpe TT, McDavid Harrison K, Dean HD. Summary of CDC consultation to address social determinants of health for prevention of disparities in HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis. Public Health Rep. 2010;125(Suppl 4):11–5. doi: 10.1177/00333549101250S404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Office of National AIDS Policy (US) National HIV/AIDS strategy for the United States. 2010. [cited 2013 Aug 6]. Available from: URL: http://www.whitehouse.gov/administration/eop/onap/nhas.
- 40.Centers for Disease Control and Prevention (US) Rockville (MD): Department of Health and Human Services (US); 2011. HIV strategic plan 2011 through 2015. [Google Scholar]
- 41.Belani H, Chorba H, Fletcher F, Kroeger K, Lansky A, Leichliter J, et al. Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. MMWR Recomm Rep. 2012;61(RR-5):1–40. [PubMed] [Google Scholar]
- 42.Dolcini MM, Gandelman AA, Vogan SA, Kong C, Leak TN, King AJ, et al. Translating HIV interventions into practice: community-based organizations' experiences with the diffusion of effective behavioral interventions (DEBIs) Soc Sci Med. 2010;71:1839–46. doi: 10.1016/j.socscimed.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–32. [PubMed] [Google Scholar]
- 44.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl 1):S30–5. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thomas JC, Thomas KK. Things ain't what they ought to be: social forces underlying racial disparities in rates of sexually transmitted diseases in a rural North Carolina county. Soc Sci Med. 1999;49:1075–84. doi: 10.1016/s0277-9536(99)00197-5. [DOI] [PubMed] [Google Scholar]
- 46.Freudenberg N. Jails, prisons, and health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78:214–35. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (US) Office of Minority Health and Health Equity. MHHE's guiding principle. [cited 2013 Aug 6]. Available from: URL: http://www.cdc.gov/minorityhealth/about/OMHHE.pdf.
- 48.Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. 2012;27:1047–67. doi: 10.1007/s11606-012-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hall HI, McDavid K, Ling Q, Sloggett A. Determinants of progression to AIDS or death after HIV diagnosis, United States, 1996 to 2001. Ann Epidemiol. 2006;16:824–33. doi: 10.1016/j.annepidem.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 50.Lasry A, Sansom SL, Hicks KA, Uzunangelov V. Allocating HIV prevention funds in the United States: recommendations from an optimization model. PLoS One. 2012;7:e37545. doi: 10.1371/journal.pone.0037545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Estrada AL. Health disparities among African-American and Hispanic drug injectors—HIV, AIDS, hepatitis B virus and hepatitis C virus: a review. AIDS. 2005;19(Suppl 3):S47–52. doi: 10.1097/01.aids.0000192070.95819.7c. [DOI] [PubMed] [Google Scholar]
- 52.Broz D, Ouellet LJ. Racial and ethnic changes in heroin injection in the United States: implications for the HIV/AIDS epidemic. Drug Alcohol Depend. 2008;94:221–33. doi: 10.1016/j.drugalcdep.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Friedman SR, Cooper HL, Osborne AH. Structural and social contexts of HIV risk among African Americans. Am J Public Health. 2009;99:1002–8. doi: 10.2105/AJPH.2008.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]