Abstract
Loss due to cancer could predispose surviving spouses or partners to a variety of negative outcomes. Although a terminal prognosis may provide opportunities to prepare for the loss, existing evidence is inconclusive as to whether death expectedness buffers potentially negative bereavement outcomes. Using data from the Living After Loss study, we examined longitudinally outcomes of bereaved individuals whose spouses/partners died from cancer (n = 112) versus other causes (n = 213) while accounting for death expectedness. While most of the cancer deaths were expected, more than half of the non-cancer deaths were not. The lowest levels of depression, grief, and loneliness over time were among those whose spouses/partners died expectedly from causes other than cancer. Cancer-bereavement was as equally distressing as any unexpected death. Future efforts should focus on the mechanisms underlying these outcomes and develop effective and early interventions to those in greatest need.
The literature is replete with evidence that loss due to cancer can be particularly challenging for surviving spouses or partners because of difficult and unique end-of-life experiences such as an exhausting caregiving situations (Chentsova-Dutton et al., 2000; Holtslander, Bally, & Steeves, 2011; Lee & Carr, 2007), witnessing and managing distressing symptoms (Carr, 2003; Kim & Schulz, 2008; Prigerson et al., 2003; Stetz & Hanson, 1992), and being socially isolated while providing daily care to the dying person (Carr, House, Wortman, Nesse, & Kessler, 2001; Clark, Brethwaite, & Gnesdiloff, 2011). Consequently, persons bereaved from cancer, compared to those whose spouses died from other causes, could be more susceptible to a variety of negative outcomes including depression, anxiety, complicated grief, and loneliness (Holtslander & Duggleby, 2010; Holtslander et al., 2011; Holtslander & McMillan, 2011; Kim & Given, 2008; Kramer, Kavanaugh, Trentham-Dietz, Walsh, & Yonker, 2010; Winterling et al., 2010).
Cancer, particularly when the prognosis is terminal, is often characterized by a progressive period of deterioration for the patient that may provide the surviving family members with opportunities to begin preparing for the imminent loss and begin to engage in coping strategies prior to the death itself (Carr, Wortman, & Wolff, 2006). Existing empirical findings, however, are inconclusive as to whether death expectedness buffers potentially negative bereavement outcomes (see Carr et al., 2001; Carr et al., 2006; Schulz, Boerner, & Hebert, 2008) in part, because some family members of those dying from terminal illnesses report that they did not expect the death to occur (Teno et al., 2004). Some have suggested that cancer caregivers, in particular, are sometimes unwilling to accept a terminal diagnosis and experience denial of an impending death (Cagle & Kovacs, 2011; Kramer et al., 2010). This may be because some cancer patients and their families respond to the diagnosis with a desire to fight and battle in an effort to prevail over the prognosis and the disease.
To date, few studies have specifically compared bereavement adjustment outcomes over time of those whose spouses or partners succumbed to cancer versus other causes of death. Kelly et al (1996) compared AIDS and cancer-related bereavement at 3 months post-loss and found similar levels of psychological distress among the two groups. This study had a relatively small sample (N = 58), of which 25 (43%) were spouses. Another investigation in which spouses and partners comprised only 28% of the sample found that those bereaved due to cancer experienced lower grief levels compared to those bereaved due to deaths from HIV/AIDS and suicide. This was a cross-sectional study in which the participants were bereaved an average of 2 years (ranging from 3 months to 5 years) when the data collection took place (Houck, 2007). Finally, Burton et al (2008) reported that spouse caregivers of those with end-stage lung cancer had similar outcomes to dementia caregivers prior to the patient’s death and at an average of 4 months into bereavement. These investigators, however, acknowledged that their findings only revealed short-term effects and the study would have benefited from additional follow-up because bereavement is best understood as a process potentially lasting years.
The above investigations, which relied mostly on cross-sectional data, were unable to examine a long-term bereavement trajectory on a sample exclusively composed of bereaved spouses/partners. These past studies only compared cancer deaths to a set of unique and isolated causes of death that may, similar to cancer, require significant end-of-life caregiving experiences (i.e., dementia) or that may be associated with a greater likelihood of prolonged or heightened bereavement experiences (i.e., AIDS, suicide). Furthermore, these past studies lacked information regarding whether or not the death was actually expected by the surviving caregiver. While cancer-related bereavement potentially precipitates negative psychosocial outcomes because of its difficult end-of-life experiences, it is still unclear as to whether or not these difficulties exceed those associated with other causes of death, to what extent they persist over time, and if expecting the death further explains or moderates these potential differences.
Using data from the Living After Loss (LAL) study, we longitudinally examined outcomes of bereaved individuals whose spouses/partners succumbed to cancer compared to those whose spouses/partners died from other causes. We followed individuals from 2–6 months of bereavement up to 14–18 months post loss and accounted for whether or not the death was expected in the analyses. The research questions and analyses presented in this paper are also important because the knowledge we gain from examining the pre-death and pre-bereavement phase and how it might impact later adjustment outcomes may be useful in developing pre-bereavement interventions. There may be opportunities to teach current cancer caregivers skills unique to their situations and futures when we more fully understand how early coping impacts subsequent adjustments.
Methods
LAL was a longitudinal study of older bereaved spouses/partners conducted in two metropolitan areas in the western United States (Caserta, Utz, Lund, & de Vries, 2010; Lund, Caserta, Utz, & de Vries, 2010). Participants completed questionnaires at the following time points: at 2–6 months of bereavement (O1), 5–9 months post loss (O2), 8–12 months post loss (O3), and a final data point (O4) occurring at 14–18 months post-loss. In between O1 and O2, participants completed one of two interventions, each consisting of a 14-week facilitator-led support group. The first was a traditional support group focusing exclusively on the emotional needs of the bereaved persons. The second was theoretically based on the “dual process model of coping” (DPM - Stroebe & Schut, 1999, 2010), which holds that bereaved persons adapt more effectively if they oscillate between loss-oriented and restoration-oriented forms of coping; this support group included traditional facilitator-led discussions about loss and grief (loss-orientation), as well as guest speakers who provided information and training that might help the bereaved readjust their daily life (for instance, household repairs, nutrition, finances, home safety – typically restoration-oriented issues). Participants were randomly assigned to one of the two intervention conditions. Given the overall aim of this particular investigation, the two groups were combined for the majority of the analyses but as described later, we added study condition to the statistical models to determine if this altered the findings.
Sample
In order to be eligible for the LAL study, participants must have met the following criteria: (1) their spouses or co-residing partners must have died within the past 2–6 months, (2) they were 50 years of age or older at baseline, (3) they intended to reside in the local area for the duration of their participation in the study, (4) they were English-speaking, and (5) they were cognitively and physically able to participate and complete questionnaires. Deaths from homicides, suicides, and those still under investigation were excluded given the unique bereavement experiences that often follow them. After sending 3,104 letters of invitation to potential participants and being able to contact 1,474 of them, 42% of those we determined to be eligible agreed to participate in the study, yielding a final sample size of 328.
Sixty-one percent (n = 200) of those enrolled in the study were women and 39% (n = 128) were men. The average age of the sample at the beginning of the study was 69.6 years (SD = 10.6), with a range of 50 to 93 years. Participants had been married or partnered for an average of 39.8 years (SD = 16.9) at the time of the death. The sample was quite educated: only 15% of the sample had a high school education or less, 41% had some college, and 44% were college graduates. The majority were Caucasian (85%), with 7% Asian, 5% African American, 2%, Latino and 1% other.
Measures
In addition to demographic information, the baseline questionnaire asked the participants to report the cause of their spouses’/partners’ deaths. These were content analyzed whereby responses that mentioned cancers (independent of site) were coded as “cancer death,” while all other causes of death were coded as “other causes.” Expectedness was measured by a dichotomous item in which the participants were asked to indicate if their spouses’/partners’ deaths were perceived to be “expected” or “unexpected.” These two variables were cross-tabulated to form 4 subcategories of participants: 1) spouses’/partners’ cause of death was cancer and expected, 2) spouses’/partners’ cause of death was cancer but not expected, 3) spouses/partners died from other causes and were expected, and 4) spouses/partners died from other causes and were not expected.
The bereavement adjustment outcomes examined in this report were grief, depression, and loneliness. Grief and depression are commonly measured outcomes in bereavement research (Carr, 2006; Neimeyer, Hogan, & Laurie, 2008). Loneliness, as well, is one of the most pervasive outcomes of spousal loss (Hansson & Stroebe, 2007) and has been reported as the single greatest problem experienced by many widows and widowers ( Lund, Caserta, & Dimond, 1993). Past research has confirmed that each of these three outcomes are particularly salient in bereavement due to cancer (Holtslander & Duggleby, 2010; Holtslander & McMillan, 2011; Kim & Given, 2008).
Grief
The Texas Revised Inventory of Grief - Present Feelings (TRIG - Faschingbauer, 1981) consists of 13 Likert-type items that are summed to provide a score ranging from 13 (low) to 65 (high). The TRIG has been among the most widely used grief measure in bereavement studies (Neimeyer et al., 2008). The alpha coefficient for the TRIG was equal to .90 for the LAL sample.
Depression
The Geriatric Depression Scale -Short Form (Sheikh & Yesavage, 1986) consists of 15 yes/no items, yielding a total score ranging from 0 (none) to 15 (severe depression). This scale was adapted from a 30-item version using those items with the greatest item-total correlations (Sheikh & Yesavage, 1986). The LAL sample generated an alpha coefficient equal to .84 for this scale.
Loneliness was assessed by the UCLA Loneliness Scale - Short Form (Russell, 1996), consisting of 13 Likert items each describing facets of loneliness. The total score ranges from 13 (low) to 52 (high). This scale was internally consistent as well (alpha = .89).
Analytic Plan
Comparisons were made between groups using t-tests, one-way analyses of variance, and chi-square analyses. We first compared cancer versus non-cancer deaths; then compared the four subgroups accounting for cause of death (cancer, non-cancer) and death expectedness (expected, not-expected). We employed repeated measures analyses of variance (RM-ANOVA) to assess group differences as well as changes over time for the three outcome variables (grief, depression, and loneliness). When warranted, pertinent demographic variables as well as study condition were added to the RM-ANOVA models to determine if these altered the findings.
Results
Descriptive Findings
One hundred and twelve (34%) of the participants in the sample reported their spouses’/partners’ cause of death as cancer, whereas 213 (65%) died from other causes. (Three individuals did not report cause of death so they were excluded from the analyses.) Ninety-eight percent of the deaths were due to natural causes, the remainder (n = 5) being the result of accidents. Over one-quarter (27%) of the sample experienced a loss due to cancer in which the death was expected and 7% were cancer-bereaved but reported the death was not expected. The greatest proportion of participants (36%) reported that their spouses or partners died unexpectedly from causes other than cancer, while 29% reported a non-cancer cause of death that was expected. More than half (n = 118; 55%) of the non-cancer deaths occurred without forewarning, 22% (n = 26) of which were reported as a heart attack or cardiac arrest. Conversely, most of the deaths due to cancer were expected (n = 89; 79%) but 23 individuals whose spouses or partners succumbed to cancer reported that they did not expect the death to occur.
In 32% (n = 36) of the cases in which the cause of death was cancer, the site of the tumor was not reported - that is, the respondents merely wrote “cancer” on the questionnaires. When a specific form of cancer was mentioned, the most common responses were lung or brain cancer (each 13%). Otherwise, there was a great deal of diversity in types of cancer from which the spouses/partners died. This held true independent of whether or not the death was expected by the bereaved spouse or partner. Small sample sizes did not permit us to do comparisons by type of cancer.
Demographic Comparisons Between Groups
Prior to addressing the overall aim of this investigation, we were interested in determining if there were demographic differences between those whose spouses or partners died from cancer versus other causes, and if these differences persisted when death expectedness was considered together with cause. As seen in Table 1, there were differences between cancer-bereaved and others according to gender, age and how long one was married/partnered at the time of the death. Women accounted for almost two-thirds (65%) of those whose spouses/partners died from non cancer causes, whereas among those who were cancer-bereaved, women only accounted for about half (52%) of the sample (p < .05). Furthermore, those bereaved due to cancer were younger (p < .001) and married or partnered for a shorter time (p < .05) than others in the sample. As expected, age was highly correlated with how long one was married or in a partnered relationship (r = .74, p < .001). There were no group differences with respect to education and race.
Table 1.
Sample Characteristics by Cause of Death and Death Expectedness, Living After Loss Study (n=325)
| Cause of Death
|
Death Expectedness
|
|||||
|---|---|---|---|---|---|---|
| Cancer n=112 | Non Cancer n=213 | Expected, Cancer n=89 | Not Expected, Cancer n=23 | Expected, Non Cancer n=95 | Not Expected, Non Cancer n=118 | |
| % Female | 52% | 65% * | 55% | 39% | 63% | 67% * |
| % White | 82% | 87% | 81% | 87% | 86% | 87% |
| % College Degree | 50% | 41% | 46% | 65% | 40% | 42% |
| Mean Age (Std Dev) range 50–93 | 66.88 (10.03) | 71.13 (10.57) *** | 66.99 (9.42) | 66.48 (12.34) | 73.96 a (9.43) | 68.86 (10.92) *** |
| Mean Years Married (Std Dev) range 1–70 | 37.06 (16.39) | 41.39 (17.11) * | 37.77 (15.85) | 34.33 (18.44) | 46.13 a (15.27) | 37.58 (17.61) *** |
Notes:
p< .05,
p<.01,
p<.001 Statistically significant differences were assessed with independent samples t-tests for the two-group cause of death comparison and with Chi-Square (sex, race, education) and One-Way ANOVA (age, years married) for the four-group death expectedness comparisons.
Scheffe post-hoc pairwise comparison tests revealed that the expected, non-cancer group was different from the other three groups.
Gender, age, and how long one was married or partnered also accounted for group differences among the 4 subsamples based on cause of death and death expectedness (p < .05 for gender; p < .001 for age and years married/partnered). The majority (61%) of those whose spouse or partner died unexpectedly from cancer were men, whereas women represented the majority of those in the remaining three categories. Scheffe post hoc pairwise comparisons revealed that participants whose spouses’/partners’ deaths were expected and due to something other than cancer were, on average, older and married longer than those in the other three groups. Again, there were no statistically significant group differences for education and race.
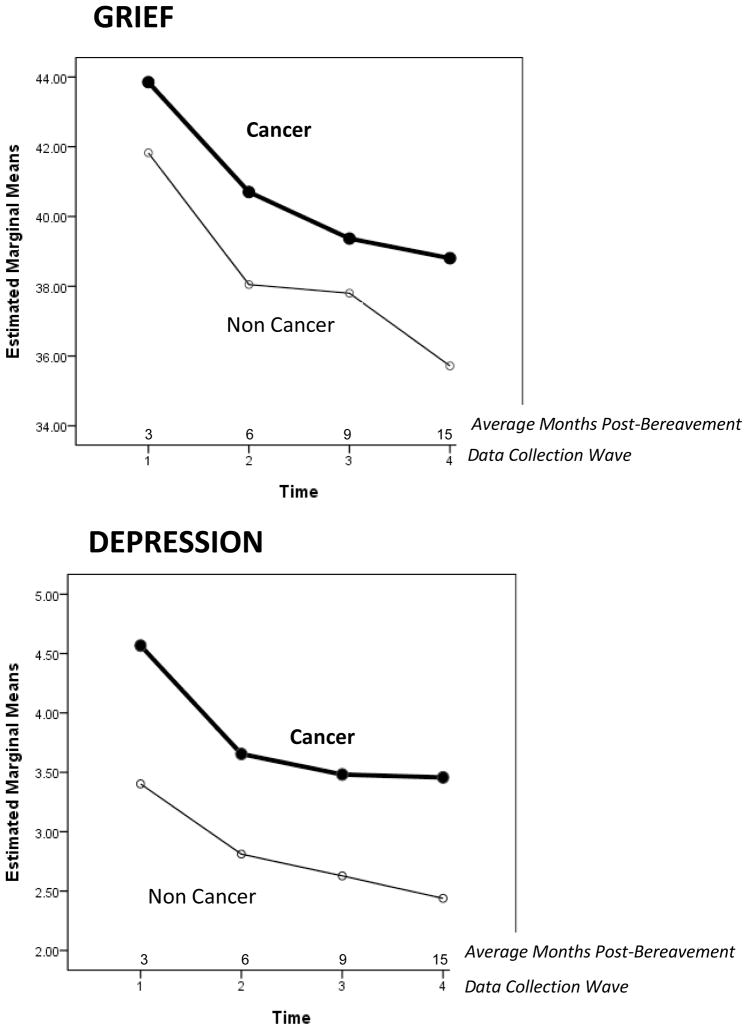
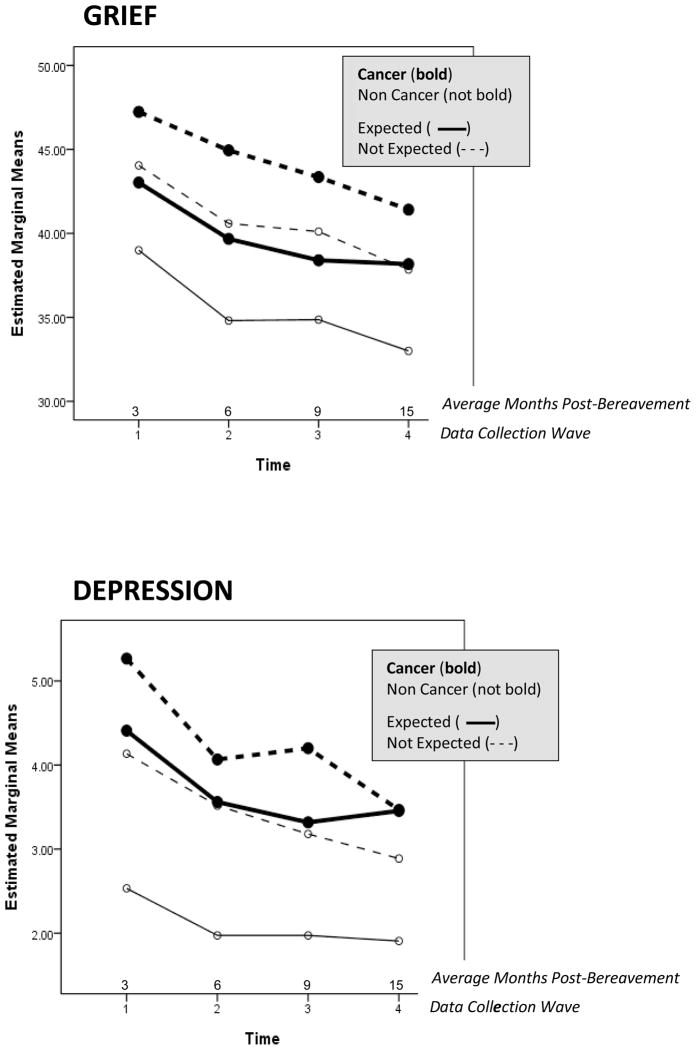
Bereavement By Cause of Death
Figure 1 graphically depicts the results of the RM-ANOVAs comparing grief, depression and loneliness over time for those bereaved due to cancer versus other causes of death. Those who lost their spouses/partners to cancer were more depressed (F = 6.46, p = .01) and tended to experience greater grief levels (F = 3.49, p = .06) than those whose spouse/partner died from other causes. There were no group differences pertaining to loneliness, however (F = 2.94, ns). The RM-ANOVAs also revealed that although there was overall improvement (decreasing levels of all outcomes) over time (all p < .001), the rate of change was similar for both groups, given the group x time interactions were not statistically significant.
Figure 1.
Repeated Measures of Grief, Depression, and Loneliness by Cause of Death
Because the two groups differed by gender, age and years married or partnered, we conducted RM-ANOVAs in which we entered each of these into the models to determine if this altered the findings. The results of these analyses were essentially unchanged except that the group differences for grief (which initially attained borderline statistical significance at the .06 level) dropped from significance when age was entered as a covariate. Age, however, was not related to grief.
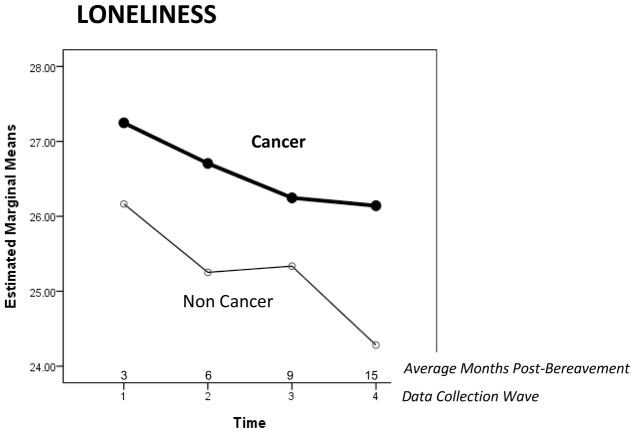
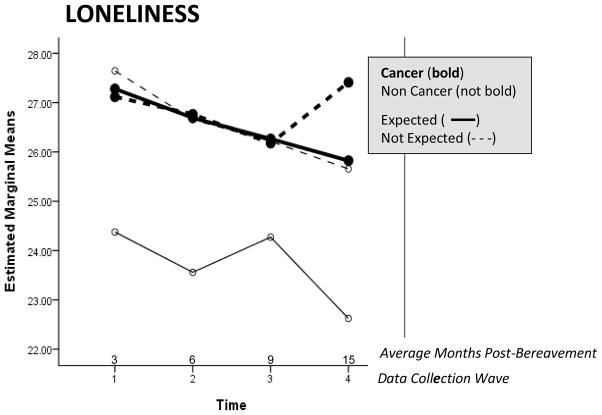
Bereavement by Cause of Death and Death Expectedness
RM-ANOVAs revealed statistically significant group differences for all three outcomes (FGrief = 6.72, p < .001; FDepression = 5.55, p = .001; FLoneliness = 4.47, p < .01), as well as significant changes over time indicating overall improvement (grief and depression, p ≤ .001; loneliness, p < .01). No statistically significant groups x time interactions were detected. These results are depicted graphically in Figure 2.
Figure 2.
Repeated Measures of Grief, Depression, and Loneliness by Cause of Death and Death Expectedness.
Scheffe post hoc pairwise comparisons specifically determined that those whose spouses’/partners’ deaths were expected and due to a cause other than cancer experienced lower grief (p < .05) and depression levels (p ≤ .05) than those in the other three groups. Those whose spouses or partners died unexpectedly (independent of cause) and those who expected the cancer death had similarly higher levels of grief and depression over time.
The findings were similar for the third outcome – loneliness. Like the results for grief and depression, the post hoc comparisons for loneliness revealed that those whose spouses’/partners’ deaths were expected and due to a cause other than cancer experienced the lowest levels of loneliness (p < .05). However, this group was only significantly different from those in the “cancer-expected” and “non cancer – not expected” categories. No significant pairwise differences were detected between the “non cancer, expected” and the “cancer, not expected” groups. A visual inspection of the trends, however, could suggest that this might be a function of reduced statistical power due to the small cell size for this category of participants.
As we did for RM-ANOVAs that compared cancer versus non cancer deaths, we added gender, age and length of marriage to the models to determine if the findings for these 4-category comparisons changed as each of these were controlled. In each case, the results were essentially unchanged for all three outcomes.
Finally, because the LAL study compared the effectiveness of two group-based interventions, we repeated all longitudinal analyses controlling for study condition (treatment versus control) to determine if the random assignment to one of two interventions altered the key findings that were initially detected pertaining to between-group differences and changes over time. In both the two-group comparison (cancer versus non cancer) and the four-group comparison (cause of death and death expectedness), the results remain largely unchanged when study condition was included in the model. This suggests that the study condition had little, if any, effect on the three bereavement outcomes associated with the four group categories we compared.
Discussion
The LAL study data enabled us to compare spousal loss due to cancer versus other causes of death, but unlike earlier reports by others, we were able to examine the course of bereavement over an approximate 12-month period of time beginning at 2 – 6 months post-loss. These data also provided an opportunity to account for death expectedness as a potentially moderating factor.
The results of this investigation confirm that when a spouse/partner dies from cancer, the surviving spouse/partner is likely to experience heightened bereavement outcomes, at least compared to those persons whose spouse/partner dies from other causes. Those who experienced a loss due to cancer were clearly more depressed than others in the sample. There also was a tendency for the cancer bereaved to report higher grief levels, although there was no difference in loneliness across the two groups.
The analyses comparing cancer versus non-cancer bereavement, however, only revealed part of the adjustment story. Once death expectedness was considered as well, a clearer picture emerged. The lowest levels of depression, grief, and loneliness were among those whose spouses/partners died from causes other than cancer who also had a sense of forewarning. Therefore, bereavement due to cancer, more so than that from other causes, was just as distressing as if the death happened unexpectedly. This difference in outcomes persisted over time even as overall improvement occurred across all subgroups compared.
Death expectedness potentially mitigates negative outcomes only among those whose spouses’ or partners’ deaths were due to something other than cancer. While there is the tendency for surviving spouses or partners to experience relief after a death that followed an extended illness (Burton, Haley, & Small, 2006), this is not the case when the death is due to cancer (Hudson, 2006). The period leading up to a cancer death - whether expected or not - and the time that follows could plausibly leave the surviving spouses or partners so emotionally and physically exhausted that they are depleted of resources needed to cope (Holtslander & Duggleby, 2010; Lunney, Lynn, Foley, Lipson, & Guralnik, 2003). When someone is diagnosed with cancer, the time during and following treatment is often described in terms of a “battle” - a description not typically used in reference to other potentially terminal diseases, such as chronic obstructive pulmonary disease, congestive heart failure, or even Alzheimer’s disease. Furthermore, this struggle or battle is rarely borne by the patient alone, but also by family members, particularly spouses (Clark et al., 2011). So by the time the “battle is lost” it has taken its toll on the survivors.
While the results pertaining to grief and depression were consistent with reports from others (Holtslander & McMillan, 2011; Kim & Given, 2008; Kramer et al., 2010), the findings regarding loneliness tend to depart from those reported in a qualitative study of 10 cancer-bereaved spouse caregivers by Holtslander and colleagues (2011). The participants in their study reported difficulties dealing with loneliness after their spouses’ deaths, which followed a period of time-consuming caregiving responsibilities – something that can be socially isolating. Reconnecting with others was an important way to regain balance in their lives. For the LAL sample, however, the relationship between cancer-related bereavement and loneliness only was revealed once analyses accounted for expectedness. In that instance, those whose spouses or partners died expectedly from causes other than cancer reported significantly less loneliness than the cancer-bereaved and those who otherwise lost a spouse or partner unexpectedly. One can speculate that a death that is expected but due to a cause other than cancer could be preceded by a longer-term illness, which may allow a spouse caregiver more time to (re)establish social relationships prior to the death. Although a cancer caregiving period is potentially shorter in duration than the caregiving required by other chronic illnesses, it could be more all-consuming (Kim & Schulz, 2008) that the caregiver could be more easily isolated from others. The potential impact of cancer-related loss on the loneliness of the surviving spouse or partner, however, clearly warrants further investigation.
Although the cancer-bereaved group was typically married/partnered for a shorter period of time, younger, and male (particularly if the death was also unexpected), the differences in bereavement outcomes over time were largely independent of gender, age, and how long the couple had been married or in a partnered relationship at the time of the death. There have been studies reporting that men and those who are younger tend to experience greater difficulty (see W. Stroebe & Schut, 2001 for a review), but others have argued that the influence of demographic factors on bereavement outcomes has at times been overemphasized (Lund et al., 1993). The findings reported here appear to be consistent with the latter argument, since the trajectories of grief, depression, and loneliness remained unchanged after accounting for demographic factors. Hence, the contrasting outcomes between cancer-related and other forms of loss probably transcend most demographic differences.
Not surprisingly, the majority of the cancer-bereaved group reported that they expected the death to occur. For a notable minority, however, their spouses’ or partners’ deaths apparently caught them unaware, which is consistent with Teno et al.’s (2004) population-based study. Although small sample sizes did not find this unique group to be statistically significant from other groups, the patterns displayed in the figures appear to suggest that this group (cancer-bereaved who did not expect the death) was experiencing the poorest outcomes - particularly grief and depression. It is plausible that these bereaved spouses or partners were unwilling to acknowledge a terminal diagnosis– perhaps due to their preoccupation with fighting the cancer “battle” (Kramer et al., 2010). Or conversely, they might be mired in uncertainty about the progression of the disease or a clear prognosis – perhaps due to inadequate or limited communication from health care providers and/or hospice staff regarding cancer (Cagle & Kovacs, 2011).
The bereavement trajectories observed in this study were independent of LAL study condition. In both group conditions, issues and problems (particularly those that were loss-oriented) were addressed more globally without substantial focus on mode of death. Individualized bereavement interventions tailored more specifically to contextual factors like cause of death (e.g., cancer) and expectedness should be designed and examined. Also, while early pre-bereavement interventions are restricted by a lack of knowledge and obvious limitations due to time constraints and stress associated with caregiving, it may be very worthwhile to be creative in finding strategies to enhance early coping skills among the caregivers. Early assessments of the caregivers could be used to determine whether or not and how extensive an intervention might be designed to meet their needs. The primary assumption is that early interventions, when possible, are likely to be the most effective, especially when targeted for those who are likely to have the greatest difficulty.
While this study addressed some of the methodological limitations of earlier reports comparing cancer-related bereavement to loss from other causes of death, caveats still exist that could potentially temper the findings. First, the cause of death was obtained from self-reports from the bereaved participants on the baseline questionnaire and not from official death records. This could call into question the accuracy of some of the responses. Furthermore, small sample sizes did not allow us to further explore specific causes of death (cancer or non-cancer). This would have enabled more direct comparisons between the findings of this study and those of Kelly et al. (1996), Houck (2007) and Burton et al. (2008).
The most notable limitations to this investigation are the lack of pre-death measures and the dichotomous nature of the expectedness item. Although bereavement following an extended illness presupposes a period of caregiving that precedes the death (Schulz et al., 2008), this can only be assumed and not confirmed without actual pre-death data describing the context of the illness and/or one’s caregiving responsibilities. Future studies should focus on expanding the measurement of pre-death circumstances such as the spouse/partner’s involvement in caregiving activities (e.g., duration, level of care provided), caregiver-related distress, perceived and actual levels of preparedness, and anticipatory grief – all of which might modify post-death bereavement outcomes. Cancer caregivers might be in a caregiving situation for shorter lengths of time than dementia caregivers, for example, but during that period devote a large portion of their day providing care to their spouse or partner (Kim & Schulz, 2008). Being a caregiver for a shorter period of time prior to one’s spouse’s or partner’s death could result in greater levels of grief and depression because there is less time to prepare for widowhood (Burton et al., 2008). This could be one potential reason those bereaved due to cancer, whether the death was expected or not, were experiencing similar levels of difficulty to those whose spouses or partners died unexpectedly from a non-cancer related cause. Future studies with better measurement of pre-death caregiving experiences may be able to better explain the causal mechanisms underlying the relationships between cause of death and bereavement outcomes.
Similarly, more refined measurements of death expectedness could also help explain the relationships reported here between cause of death and bereavement outcomes. Many scholars and clinicians agree that death expectedness does not necessarily equate to preparedness (Barry, Kasl, & Prigerson, 2002; Hebert, Prigerson, Schulz, & Arnold, 2006), which is a limitation of the dichotomous measure for expectedness used in this study. Although expecting the death has been used as “an indicator of readiness to handle the bereavement process” (Barry et al., 2002, p. 454), it is clear that these findings would have been strengthened if we were able to obtain the participants’ own perceptions of how prepared they were for their spouses’ or partners’ deaths. Future investigations should include assessments of how prepared bereaved individuals are for their spouses’ or partners’ deaths -- both emotionally and in practical matters as well.
Even with the above limitations, however, the results of this investigation have provided some new insight into the bereavement experiences of those whose spouses and partners died from cancer versus other causes. Unlike previous studies, we were able to obtain a longitudinal profile of bereavement experiences and were able to model the moderating influence of death expectedness. Loss due to cancer – no matter if expected or not – is a distressing situation that could potentially predispose the surviving spouse or partner to greater risk for adverse consequences. Efforts should continue to further understand the mechanisms underlying these outcomes and develop effective ways to provide assistance to those who need it.
Acknowledgments
The Living After Loss study was funded by a grant from the National Institute on Aging (R01 AG023090). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
The authors wish to acknowledge the helpful contributions of three external consultants: Drs. Judith Hays, Duke University, Bert Hayslip, University of North Texas, and Marilyn Skaff, University of California, San Francisco. Also, Dr. Brian de Vries, San Francisco State University, was a major contributor to the study by serving as the Site PI at that location.
Contributor Information
Michael S. Caserta, University of Utah.
Rebecca L. Utz, University of Utah.
Dale A. Lund, California State University, San Bernardino.
References
- Barry LC, Kasl SV, Prigerson HG. Psychiatric disorders among bereaved persons: The role of perceived circumstances of death and preparedness for death. American Journal of Geriatric Psychiatry. 2002;10(4):447–457. [PubMed] [Google Scholar]
- Burton AM, Haley WE, Small BJ. Bereavement after caregiving or unexpected death: Effects on elderly spouses. Aging and Mental Health. 2006;10(3):319–326. doi: 10.1080/13607860500410045. LR5T383267124042. [DOI] [PubMed] [Google Scholar]
- Burton AM, Haley WE, Small BJ, Finley MR, Dillinger-Vasille M, Schonwetter R. Predictors of well-being in bereaved former hospice caregivers: The role of caregiving stressors, appraisals, and social resources. Palliative and Supportive Care. 2008;6(2):149–158. doi: 10.1017/S1478951508000230. [DOI] [PubMed] [Google Scholar]
- Cagle JG, Kovacs PJ. Informal caregivers of cancer patients: Perceptions about preparedness and support during hospice care. Journal of Gerontological Social Work. 2011;54(1):92–115. doi: 10.1080/01634372.2010.534547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D. A “good death” for whom? Quality of spouse’s death and psychological distress among older widowed persons. Journal of Health and Social Behavior. 2003;44(2):215–232. [PubMed] [Google Scholar]
- Carr D. Methodological issues in studying late life bereavement. In: Carr D, Nesse R, Wortman CB, editors. Spousal bereavement in late life. New York, NY: Springer; 2006. pp. 19–47. [Google Scholar]
- Carr D, House JS, Wortman CB, Nesse R, Kessler RC. Psychological adjustment to sudden and anticipated spousal death among the older widowed. Journal of Gerontology: Social Sciences. 2001;56B(4):S237–S248. doi: 10.1093/geronb/56.4.s237. [DOI] [PubMed] [Google Scholar]
- Carr D, Wortman CB, Wolff K. How older Americans die today: Implications for surviving spouses. In: Carr D, Nesse RM, Wortman CB, editors. Spousal bereavement in late life. New York: Springer Publishing Company; 2006. pp. 49–78. [Google Scholar]
- Caserta M, Utz R, Lund D, de Vries B. Sampling, recruitment, and retention in a bereavement intervention study: Experiences from the Living After Loss project. Omega (Westport) 2010;61(3):181–203. doi: 10.2190/OM.61.3.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chentsova-Dutton Y, Shuchter S, Hutchin S, Strause L, Burns K, Zisook S. The psychological and physical health of hospice caregivers. Annals of Clinical Psychiatry. 2000;12(1):19–27. doi: 10.1023/a:1009070826012. [DOI] [PubMed] [Google Scholar]
- Clark PG, Brethwaite DS, Gnesdiloff S. Providing support at time of death from cancer: Results of a 5-year post-bereavement group study. Journal of Social Work in End-of-Life & Palliative Care. 2011;7(2–3):195–215. doi: 10.1080/15524256.2011.593156. [DOI] [PubMed] [Google Scholar]
- Faschingbauer TR. Texas revised inventory of grief manual. Houston, TX: Honeycomb; 1981. [Google Scholar]
- Hansson RO, Stroebe MS. Bereavement in late life: Coping, adaptation, and developmental influences. Washington, DC: American Psychological Association; 2007. [Google Scholar]
- Hebert RS, Prigerson HG, Schulz R, Arnold RM. Preparing caregivers for the death of a loved one: A theoretical framework and suggestions for future research. Journal of Palliative Medicine. 2006;9(5):1164–1171. doi: 10.1089/jpm.2006.9.1164. [DOI] [PubMed] [Google Scholar]
- Holtslander L, Duggleby W. The psychosocial context of bereavement for older women who were caregivers for a spouse with advanced cancer. Journal of Women and Aging. 2010;22(2):109–124. doi: 10.1080/08952841003716147. 921468168. [DOI] [PubMed] [Google Scholar]
- Holtslander LF, Bally JM, Steeves ML. Walking a fine line: An exploration of the experience of finding balance for older persons bereaved after caregiving for a spouse with advanced cancer. European Journal of Oncology Nursing. 2011;15(3):254–259. doi: 10.1016/j.ejon.2010.12.004. [DOI] [PubMed] [Google Scholar]
- Holtslander LF, McMillan SC. Depressive symptoms, grief, and complicated grief among family caregivers of patients with advanced cancer three months into bereavement. Oncology Nursing Forum. 2011;38(1):60–65. doi: 10.1188/11.ONF.60-65. [DOI] [PubMed] [Google Scholar]
- Houck JA. A comparison of grief reactions in cancer, HIV/AIDS, and suicide bereavement. Journal of HIV/AIDS & Social Services. 2007;6(3):97–112. doi: 10.1300/J187v06n03_7. [DOI] [Google Scholar]
- Hudson PL. How well do family caregivers cope after caring for a relative with advanced disease and how can health professionals enhance their support? Journal of Palliative Medicine. 2006;9(3):694–703. doi: 10.1089/jpm.2006.9.694. [DOI] [PubMed] [Google Scholar]
- Kelly B, Raphael B, Statham D, Ross M, Eastwood H, McLean S, O’Loughlin B, Brittain K. A comparison of the psychosocial aspects of AIDS and cancer-related bereavement. International Journal of Psychiatry in Medicine. 1996;26(1):35–49. doi: 10.2190/PUWY-N3AL-KK3T-B89L. [DOI] [PubMed] [Google Scholar]
- Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: Across the trajectory of the illness. Cancer. 2008;112(11 Suppl):2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- Kim Y, Schulz R. Family caregivers’ strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2008;20(5):483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- Kramer BJ, Kavanaugh M, Trentham-Dietz A, Walsh M, Yonker JA. Complicated grief symptoms in caregivers of persons with lung cancer: The role of family conflict, intrapsychic strains, and hospice utilization. Omega (Westport) 2010;62(3):201–220. doi: 10.2190/om.62.3.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MA, Carr D. Does the context of spousal loss affect the physical functioning of older widowed persons? Research on Aging. 2007;29(5):457–487. [Google Scholar]
- Lund D, Caserta M, Dimond M. Handbook of bereavement: Theory, research and intervention. London: Cambridge University Press; 1993. The course of spousal bereavement in later life; pp. 240–254. [Google Scholar]
- Lund D, Caserta M, Utz R, de Vries B. A tale of two counties: Bereavement in socio-demographically diverse places. Illness, Crisis & Loss. 2010;18(4):301–321. doi: 10.2190/il.18.4.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. Journal of the American Medical Association. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- Neimeyer RA, Hogan NS, Laurie A. The measurement of grief: Psychometric considerations in the assessment of reactions to bereavement. In: Stroebe M, Hansson RO, Schut H, Stroebe W, editors. Handbook of bereavement research and practice: Advances in theory and intervention. Washington, DC: American Psychological Association; 2008. pp. 133–161. [Google Scholar]
- Prigerson HG, Cherlin E, Chen JH, Kasl SV, Hurzeler R, Bradley EH. The stressful caregiving adult reactions to experiences of dying (SCARED) scale: A measure for assessing caregiver exposure to distress in terminal care. American Journal of Geriatric Psychiatry. 2003;11(3):309–319. [PubMed] [Google Scholar]
- Russell DW. UCLA loneliness scale (version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Schulz R, Boerner K, Hebert RS. Caregiving and bereavement. In: Stroebe M, Hansson RO, Schut H, Stroebe W, editors. Handbook of bereavement research and practice: Advances in theory and intervention. Washington, DC: American Psychological Association; 2008. pp. 265–285. [Google Scholar]
- Sheikh JI, Yesavage JA. Clinical gerontology: A guide to assessment and intervention. New York, NY: Haworth Press; 1986. Geriatric depression scale (GDS): Recent evidence and development of a shorter version; pp. 165–173. [Google Scholar]
- Stetz KM, Hanson WK. Alterations in perceptions of caregiving demands in advanced cancer during and after the experience. Hospice Journal. 1992;8(3):21–34. doi: 10.1080/0742-969x.1992.11882728. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H. The dual process model of coping with bereavement: Rationale and description. Death Studies. 1999;23:197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H. The dual process model of coping with bereavement: A decade on. Omega (Westport) 2010;61(4):273–289. doi: 10.2190/OM.61.4.b. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Schut H. Risk factors in bereavement outcome: A methodological and empirical review. In: Stroebe M, Hansson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping, and care. Washington, DC: American Psychological Association; 2001. pp. 349–371. [Google Scholar]
- Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. Journal of the American Medical Association. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- Winterling J, Wasteson E, Arving C, Johansson B, Glimelius B, Nordin K. Factors associated with psychological distress and grief resolution in surviving spouses of patients with advanced gastrointestinal cancer. Support Care in Cancer. 2010;18(11):1377–1384. doi: 10.1007/s00520-009-0753-9. [DOI] [PubMed] [Google Scholar]