Abstract
The development of efficacious theory-based, culturally relevant interventions to promote cervical cancer prevention among underserved populations is crucial to the elimination of cancer disparities. The purpose of this article is to describe the development of a theory-based, culturally relevant intervention focusing on primary (sexual risk reduction) and secondary (Pap smear) prevention of cervical cancer among Latina immigrants using intervention mapping (IM). The PEN-3 and Health Belief Model provided theoretical guidance for the intervention development and implementation. IM provides a logical five-step framework in intervention development: delineating proximal program objectives, selecting theory-based intervention methods and strategies, developing a program plan, planning for adoption in implementation, and creating evaluation plans and instruments. We first conducted an extensive literature review and qualitatively examined the socio-cultural factors associated with primary and secondary prevention of cervical cancer. We then proceeded to quantitatively validate the qualitative findings, which led to development matrices linking the theoretical constructs with intervention objectives and strategies as well as evaluation. IM was a helpful tool in the development of a theory-based, culturally relevant intervention addressing primary and secondary prevention among Latina immigrants.
Keywords: intervention development, intervention mapping, cervical cancer prevention, Latina immigrants
The cervix is the fourth leading site of new cancer cases among Latinas in the United States, with an incidence rate of 13.2/100,000 as compared to 8.2/100,000 among White women (American Cancer Society, 2009), and the mortality rate is 40% higher among Latinas as compared to Whites (American Cancer Society, 2009). Given the increased Latino immigration to this country, cervical cancer incidence and mortality rates in Latin America need to be seriously considered as they have direct implications for cervical cancer control in the United States. The incidence of cervical cancer in Central and South America are 40.3/100,000 and 30.9/100,000, respectively (Pan American Health Organization, 2001), with cervical cancer being the leading cause of cancer mortality among women in Latin America (Pisani, Parkin, Bray, & Ferlay, 1999).
In terms of primary prevention, human papillomavirus (HPV) infection has been shown to be the most important contributing factor for cervical cancer (Rock, Michael, Reynolds, & Ruffin, 2000). Latinas are 2 times more likely than African American women and 5 times more likely than White women to display an association between HPV infection and squamous intraepithelial lesions (Tortolero-Luna et al., 1998). With regard to secondary prevention, Latinas are less likely to get a Pap smear than Whites (Hubbell, Chavez, Mishra, & Valdez, 1996) and African American women (Bazargan, Bazargan, Farooq, & Baker, 2004), with screening rates being even lower among Latina immigrants (Hubbell et al., 1996; Scarinci, Beech, Kovach, & Bailey, 2003).
Several studies have found that there are a number of factors associated with cervical cancer screening among Latinas, such as income (Swan, Breen, Coates, Rimer, & Lee, 2003), education (Chavez, Hubbell, McMullin, Martinez, & Mishra, 1995; Scarinci et al., 2003), health insurance (Chavez et al., 1995), having a regular source of health care (Zambrana, Breen, Fox, Gutierrez-Mohamed, 1999), prior history of cancer screening (Zambrana et al., 1999), embarrassment (Byrd, Chavez, & Wilson, 2007), fear of results (Byrd et al., 2007), and self-efficacy (Fernández et al., 2009a). Studies have also shown that Latinas tend to be less knowledgeable (Scarinci et al., 2003) about cancer signs, causes, and treatment effectiveness and tend to display more fatalistic beliefs regarding cancer and cancer screening than White women (Chavez, Hubbell, Mishra, & Valdez, 1997; Scarinci et al., 2003).
One successful approach to improving health behaviors and cervical cancer screening among Latinas has been the development of interventions based on a sociologic approach that takes into account their cultural beliefs, attitudes, and behaviors (Fernández et al., 2009b; Navarro et al., 1998; Navarro et al., 2000; Valdez, Banerjee, Ackerson, & Fernandez, 2002; Yancey, Tanjasiri, Klein, & Tunder, 1995; Zapka et al., 1993), as well as the involvement of lay health educators (Fernández et al., 2009b; Navarro et al., 1998; Navarro et al., 2000). Cognitive behavioral approaches have also shown encouraging results among Latinas (particularly sexual risk reduction; Koniak-Griffin et al., 2003). The purpose of this study is to describe the development of a theory-based, culturally relevant intervention focusing on primary (sexual risk reduction) and secondary (Pap smear) prevention of cervical cancer by combining these two approaches using intervention mapping (IM; Bartholomew, Parcel, Kok, & Gottlieb, 2001). Both the PEN-3 (sociological approach) and HBM (behavioral approach) guided the development and implementation of the intervention (Airhihenbuwa, 1992; Rosenstock, 1990).
BACKGROUND AND LITERATURE REVIEW
Although numerous studies have been conducted on HIV/STI prevention, there has been a lack of interventions focusing on the primary prevention of cervical cancer, that is, sexual risk reduction and HPV. Given the similarity of sexual preventive behaviors between HPV and other STIs, we believe that the findings from HIV/STI intervention trials can be extrapolated to HPV prevention (U.S. Department of Health and Human Services, 2001). Most effective programs addressing HIV/STI prevention have three components in common: information, skills training (problem solving, communication/negotiation, assertiveness, and self-efficacy), and promotion of personal responsibility for sexual decision making (Centers for Disease Control and Prevention, 1999). A review from Shepherd, Peersman, Weston, and Napuli (2000) also reported on the effectiveness of health education interventions to promote sexual risk reduction among low-income women. They found that educational programs that combined providing information with sexual negotiation skills were the most effective strategies (Shepherd et al., 2000). However, both reviews indicated that most of the studies did not have a Latino representation or that its representation was less than 30%.
Yabroff, Mangan, and Mandelblatt (2003) conducted a comprehensive review on interventions to increase Pap smears, and they found that there was a great variability in their effectiveness. Although only two interventions specifically targeted Latinas, this review provided important insights on the factors that have been associated with effective interventions. Overall, sociologic and a combination of sociologic/cognitive strategies had similar results in Pap smear increases ranging from 2.7% to 9.2%. The most effective approach in delivering a culturally specific intervention to Vietnamese Americans (18% increase in Pap smear rates) was the integration of sociologic, behavioral, and cognitive strategies by using lay health workers, educational brochures, and financial incentives (Dickey & Petitti, 1992). Although cognitive–behavioral strategies that focus on patients have shown promising results in promoting cervical cancer screening (Yabroff et al., 2003), none of these have been tested with Latinas.
Navarro et al. (1998, 2000) developed a successful sociologic community-based intervention to promote breast and cervical cancer screening among low-income Latinas using community health advisors. To our knowledge, this is the only breast and cervical cancer screening intervention among Latinas that is theory-based, developed specifically for this population, and has had its efficacy assessed through a randomized trial. However, this program had limitations: (a) Although a large percentage of participants were Latina immigrants, the focus of the program was on low-income Latinas and not Latina immigrants. As documented above, screening rates are much lower among Latina immigrants as compared to U.S.-born Latinas, as they may face different challenges regarding health care access and health information. (b) Moreover, there was a relatively low impact on behavior change in breast and cervical screening, particularly among women who never engaged in these behaviors. Thus, after a review of the literature relevant to both the primary and secondary prevention of cervical cancer screening, our plans for the proposed intervention were to combine aspects of the program developed by Navarro et al. that has been shown to be effective (cultural relevance, theory-based, and involvement of lay health educators) and cognitive–behavioral strategies that have been shown to be effective in other populations.
METHOD
Intervention Mapping (IM)
Intervention development is a process that begins with examining existing interventions, determining challenges and barriers in the unique setting or population, conducting careful process and formative evaluations, revising the intervention materials, and ending with dissemination. IM is one such systematic process that can be used in program development (Bartholomew et al., 2001). Bartholomew and colleagues (2001) proposed five steps that should be taken when developing an intervention: (a) delineating proximal program objectives—this step specifies “who and what will change as a result of the intervention” by determining the proximal objectives and outcomes and by defining the target audience, including inclusion and exclusion criteria; (b) selecting theory-based intervention methods and strategies—once the objectives, outcomes, and target audience are identified, the research team begins to brainstorm methods and how they can be organized to be consistent with the theoretical framework as well as the proposed objectives and outcomes; (c) developing a program plan—this phase consists of operationalizing the strategies established under Step 2 to concretize implementation plans; (d) planning for adoption in implementation—this step consists of actual implementation of the intervention and all the necessary components, taking into account the context in which the intervention will be implemented; and (4) creating evaluation plans and instruments—this step will determine whether decisions made throughout the process were correct and how intervention efficacy will be determined in terms of process and outcomes evaluation (Bartholomew et al., 2001). These steps should take place after a comprehensive needs assessment is conducted.
All phases of intervention development were reviewed and approved by the university’s institutional review board. All participants went through the informed consent procedures and signed consent forms.
RESULTS: INTERVENTION DEVELOPMENT
Needs Assessments
We first explored the sociocultural factors associated with cervical cancer and screening among Latina immigrants using focus groups (Garcés, Scarinci, & Harrison, 2006; Scarinci et al., 2003) as well as the sociocultural factors associated with sexual risk reduction through qualitative interviews with Latino and Latina immigrants. Based on the qualitative findings, we developed a quantitative questionnaire that addresses the primary and secondary prevention of cervical cancer that was administered and validated among 202 Latina immigrants (unpublished data). The relevant findings from the qualitative and quantitative studies are described in Table 1.
TABLE 1.
Summary of Preliminary Findings Based on the PEN-3 and HBM
| Theoretical Constructs |
Preliminary Findings |
|---|---|
| Perceptions (PEN-3) | Positive
|
Negative
|
|
| Enablers (PEN-3) | Positive
|
Negativea
|
|
| Nurturers (PEN-3) | Positive
|
Negative
|
|
| Perceived susceptibility (HBM) | Negative
|
| Perceived severity (HBM) |
|
| Perceived barriers (HBM) | Negative (because of the nature of this component, the “positive” classification does not apply)
|
| Perceived benefits (HBM) | Positive
|
Negative
|
|
| Self-efficacy (HBM) | Positive
|
Negative
|
NOTE: HBM = Health Belief Model; HPV = human papilloma virus; STI = sexually transmitted infection.
Structural perceived barriers overlap with negative enablers
Identification of Outcomes and Proximal Objectives
Based on the results of the qualitative and quantitative needs assessments, we conducted two focus groups with Latina immigrants (n = 13) in which we presented the findings and asked for their input regarding intervention development. The findings were presented according to the data presented in Table 1 but in a manner that could be easily understood by participants (including examples). We then engaged in a discussion with participants about whether they agreed or disagreed with these findings. We addressed topics such as intervention format, recruitment and retention, information delivery format, target audience (women, men, or both), who should deliver the intervention, etc.
Some suggestions from the focus groups were that (a) primary and secondary prevention should be addressed together as part of the same program under the umbrella of “health promotion among women,” (b) the topic should be addressed in small groups of women so that they would be comfortable asking questions and discussing sensitive issues, and (c) the intervention should focus on women only. One of the groups also suggested “friendship circles” in which one woman hosts the sessions in her home and invites her friends to attend. Through this format, they could motivate each other to overcome the barriers to primary and secondary prevention of cervical cancer (social networks).
To document efficacy of the intervention, we chose two measurable primary outcomes (i.e., cervical cancer screening as recommended by U.S. Preventive Services Task Force and increased partner communication regarding sexual behavior) and one secondary outcome (i.e., changes in knowledge, attitudes, and beliefs regarding the relationship between HPV infection and cervical cancer).
Selecting Theory-Based Intervention Methods and Strategies
Once the outcomes were identified, we proceeded with the research design. The choice of group randomized trial versus randomization at the individual level was based on the fact that word of mouth is very powerful among the target audience. As such, the chosen unit of randomization was apartment complexes and trailer parks. Through this approach, we could minimize some threats to internal validity (e.g., resentful demoralization, contamination) by including in the same groups participants who are likely to talk to each other.
Throughout our needs assessments, we found that Latina immigrants were also very interested in nutrition and diabetes prevention. To avoid a number of potential threats to internal validity (e.g., resentful demoralization among staff running a “control” group as compared to the “intervention” group) and address a need in the community, we proposed two “interventions” (cervical cancer vs. nutrition and diabetes prevention). It was also clear from the findings in the needs assessment phase that cognitive–behavioral strategies should be a cornerstone of the proposed intervention given all the identified intrapersonal barriers (e.g., fear of results, embarrassment). The crucial component of this phase was to identify intervention strategies that have been shown to be effective in the literature and to integrate them with the proposed theoretical constructs and the results of the needs assessments. Table 2 details the matrices that link the theoretical constructs with intervention objectives and strategies.
TABLE 2.
Proposed Intervention: Objectives and Strategies as They Relate to the PEN-3 and Health Belief Model
| Theoretical Constructs |
Intervention Objectives | Strategies—Group Sessions | Strategies—Individual Sessions |
| Perceptions (PEN-3) |
|
|
|
| Enablers (PEN-3)/Perceived Barriers (HBM)a |
|
|
|
| Nurturers (PEN-3) |
|
|
|
| Perceived susceptibility (HBM) |
|
|
|
| Perceived severity (HBM) |
|
|
|
| Perceived benefits (HBM) |
|
|
|
| Self-efficacy (HBM) |
|
|
|
NOTE: HBM = Health Belief Model; HPV = human papilloma virus.
Structural perceived barriers overlap with negative enablers. Therefore, they were grouped in the same category for intervention purposes.
Participants received a “directory”, including medical and social services available in the community. This directory provides hours, costs, availability of interpreters, services, etc.
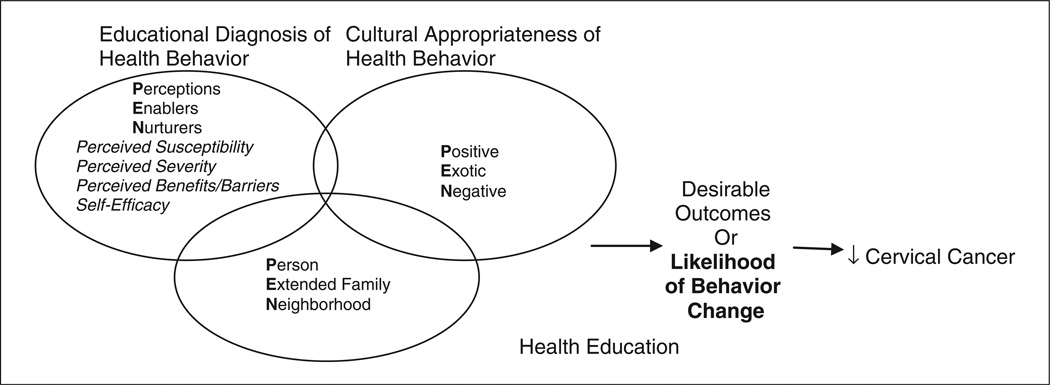
Also of relevance are the use of theoretical models that guided the proposed intervention and how we made it “culturally relevant” by using the PEN-3 and the HBM (see Figure 1; Airhihenbuwa, 1992; Rosenstock, 1990). Under the PEN-3, perceptions include the knowledge, attitudes, and beliefs that may contribute or hinder engagement in a particular health behavior. Enablers are community or structural factors such as the availability of resources, accessibility, referrals, etc. Nurturers refer to reinforcing factors that the target audience receive from their social networks. The third and most important and unique dimension of the model is the cultural appropriateness of a health behavior, in which the perceptions, enablers, and nurturers are classified as positive (factors that lead the target audience to engage in a particular health behavior), exotic (practices that have no harmful health consequences and should not be changed but incorporated in the intervention), and negative (factors that lead the target audience to not engage in the health behavior or to engage in a harmful behavior) (Airhihenbuwa, 1992; Garcés et al., 2006; Scarinci et al., 2003).
FIGURE 1. Theoretical Models (PEN-3 and Health Belief Model) Used in the Intervention Development.
SOURCE: Adapted from Airhihenbuwa (1992) and Rosenstock (1990).
Although the PEN-3 model takes into account cultural sensitivity and appropriateness in the data collection process and intervention development, we believe that there are other components that may be relevant when examining primary and secondary prevention of cervical cancer among Latina immigrants. These components are addressed in the HBM. Under the HBM, individuals will change their behavior(s) to prevent a particular disease if (a) they consider themselves as susceptible to the disease or condition (e.g., they can be exposed to HPV), (b) if they perceive that such disease or condition can have serious consequences (e.g., HPV can lead to cervical cancer which can be fatal), (c) they perceive that they are threatened by the disease or condition, (d) they perceive that engagement in a particular behavior (e.g., getting screening) will be beneficial in reducing the susceptibility to and/or the severity of the disease, and (e) they believe that the benefits outweigh the barriers or costs (Rosenstock, 1990). Rosenstock (1990) argues that the concept of self-efficacy (i.e., the individual’s belief that he or she can perform the action to prevent a particular disease or condition) should be added to the HBM. The final model incorporates the components of the PEN-3 and the HBM (see Figure 1).
To make our proposed intervention culturally relevant, we identified specific cultural values that are considered to be central in the Latino culture and may play a role in cervical cancer prevention. It has been suggested that the importance of family (familiarismo) is one of the key Latino values (Mendoza & Petersen, 2000). Family members tend to rely on each other for support when dealing with problems and difficulties (including health problems). The concept of familiarismo also involves the extended family, which is made up of blood relatives as well as close friends (“compadres” and “comadres”; Marin & Marin, 1991). This is particularly relevant when dealing with immigrants. When coming to a new country, Latinos tend to turn to their co-nationals for support and assistance (Mendoza & Petersen, 2000). These communities can sometimes behave like families with extremely close ties (Marin & Marin, 1991).
Being an allocentric culture, Latinos tend to trust individuals more than institutions. They tend to prefer personal and individual attention and seek relationships that are nurturing, intimate, and respectful rather than confrontational (personalismo; Marin & Marin, 1991; Mendoza & Petersen, 2000). Given the traditional gender role norms in the Latino culture, Latino men tend to be dominant and women tend to be submissive to and dependent on their husbands and other males (machismo; Mendoza & Petersen, 2000). These “uneven” gender role norms have important implications for primary prevention of cervical cancer, because women may lack the negotiation skills and assertiveness necessary to engage in safe sexual practices. And finally fatalismo, which refers to the acceptance that things cannot be changed and control is usually placed in God’s hands (Chavez et al., 1997).
Developing a Program Plan
Once the matrices were in place, we proceeded with writing the intervention manuals. The intervention consisted of eight sessions (six group sessions and two individual sessions; see Table 3). There was a behavioral cue associated with each session. In the first session, participants receive a “friendship box” to keep all the information cards as well as a bracelet. In each session, a charm corresponding to the knowledge and skill learned was added to the bracelet.
TABLE 3.
Content of the Group and Individual Sessions
| Session | Content |
|---|---|
| Group Session 1 |
|
| Group Session 2 |
|
| Group Session 3 |
|
| Group Session 4 |
|
| Individual Session 1 |
|
| Group Session 5 |
|
| Individual Session 2 |
|
| Group Session 6 |
|
Based on evidence from the literature review (Fernández et al., 2009b; Navarro et al., 1998; Navarro et al., 2000), we elected to employ lay health educators (LHEs) for intervention delivery as they are from the targeted community, they have the ability to reach the unreached, they are able to tailor health messages to the target audience, and above all, they are trusted individuals in the community.
Planning for Adoption in Implementation
Once the intervention was developed, we began by first eliciting feedback from LHEs and lay health advisors (volunteers) who were already participating in another program. Then, the intervention was piloted among 10 Latina immigrants meeting the inclusion criteria for the trial. Because modifications and suggestions were minor, only one set of pilot testing was conducted.
Once the intervention was finalized, operation and training manuals and strategies were finalized, including recruitment and retention strategies. Recruitment was done by literally canvassing the community to first identify the potential recruitment sites. Once the sites were identified, LHEs used a door-to-door approach to invite women to participate in the program. In terms of retention efforts, we implemented multiple strategies that include contact with participants at least once a month: phone calls, quarterly newsletters, and quarterly pot-luck dinners. Also, LHEs kept a detailed record on all participants ranging from contacts initiated by the participant and/or educator to special celebrations (e.g., birth of a child, husband’s illness).
Creating Evaluation Plans and Instruments
The evaluation consisted of process and outcome evaluation. Process evaluation or treatment fidelity was addressed at five levels based on the NIH Behavior Change Consortium recommendations (study design, staff training, delivery of treatment, receipt of treatment, and enactment of treatment skills) as outlined in Table 4 (Bellg et al., 2004). Outcome evaluation included assessments of all components of the proposed theoretical models as well as the proposed primary and secondary outcomes. The outcome evaluation consisted of baseline, postintervention, and 12- and 24-month follow-up assessments.
TABLE 4.
Treatment Fidelity Strategies Used in the Intervention
| Level | Goals | Strategies |
| Study design |
|
|
| Staff training |
|
|
| Delivery of treatment |
|
|
| Receipt of treatment |
|
|
| Enactment of treatment skills |
|
|
DISCUSSION
The intervention development process began with the rapid growth of the Latino population in the Southern states coupled with the evidenced cervical cancer disparities between Latinas and Whites. Through IM, we were able to establish a logical planning process (taking into account the needs and assets in these new communities) based on theoretical models of behavior change and intervention development (PEN-3 and HBM). The conception of this study was based on our own difficulties in finding articles in the literature that detail step by step the process of intervention development. With a few exceptions (Fernandez, Gonzales, Tortolero-Luna, Partida, & Bartholomew, 2005; Gans et al., 2003), most papers allude to intervention development, but their primary focus is on methodology and results. Therefore, we made an attempt to report, in detail, all the steps that were taken and how decisions were made with the intent of providing some insights to other investigators who plan to develop theory-based, culturally relevant interventions.
In this process, we learned a number of lessons. Consistent with the experience of Gans and colleagues (Gans et al., 2003), the development of a well-thought-out intervention took more time and resources than initially anticipated. The development of this intervention took years and multiple funding mechanisms. Because little was known about cervical cancer screening among Latina immigrants in the United States, we needed to gain a better understanding of the sociocultural factors associated with two very distinct behaviors (Pap smear and sexual risk reduction) that not only required different methodologies (focus groups vs. individual interviews) but also different conceptualizations.
In the process of doing the needs assessments, it became clear to the investigators that a group randomized trial would be more appropriate than randomization at the individual level given the power of word of mouth in this population as well as suggestions by the target audience about hosting the sessions where they lived. The use of group-randomized designs is particularly widespread in the evaluation of health care and screening strategies. Although randomization of individuals would be more desirable from the perspective of statistical power, it was unfeasible from an operational point of view in this proposed project. Randomization of subjects in groups, rather than each individual separately, has important consequences for sample size estimation, interpretation, and analysis. The groups of participants are likely to be heterogeneous, giving rise to a component of variation that one must take into consideration. In addition, individuals within a group are more likely to resemble each other more than individuals in different groups, thereby violating the assumption of statistical independence between subjects.
However, these issues can be addressed in the statistical analysis whereas threats to internal validity (e.g., diffusion of treatment, compensatory rivalry, and resentful demoralization) could not. Given the powerful influence of word of mouth among Latinos, we could minimize these threats by including participants who are likely to talk to each other in the same group.
Community involvement, made possible through relationships forged during previous outreach efforts, cannot be underscored enough. In this process, it was critical to receive the input of the target audience as well as the staff. However, being an unassertive culture, it takes time to establish trust so honest feedback can be obtained rather than socially desirable answers. The involvement of our volunteers from a parallel outreach program in the community was crucial to establishing trust in the community and recruiting and retaining such a large number of participants in a randomized clinical trial (n = 543).
A third lesson was flexibility. The goals and proposed methodology were fluid and changed between the submission of grant proposals and implementation in the community. This flexibility contributed to the process of establishing trust in the community because it was not the academic institution dictating how assessments and intervention development were going to take place. Both sides (community and academicians) contributed to the process so that a final product could be obtained without sacrificing the scientific integrity of the project or the integrity of the community. For example, initially, we proposed having a control group addressing general information. However, in our needs assessment we identified a major interest in the community in learning about nutrition and diabetes prevention. As such, we developed a second intervention to address these needs.
The development of a “culturally relevant” intervention is not readily apparent at the inception of a needs assessment. Through the assessments, the relevant aspects of the culture became more salient, and it is only through carefully listening and reading “between the lines” that these nuances could be incorporated in the behavior change intervention. Utilizing cultural values to reinforce the messages without running the risk of being stereotypical is a very sensitive matter. How these values are incorporated within an intervention is critical to the process. For instance, the “collectivism” or reliance on each other was openly reinforced in every session and clearly used as a motivator for women to share with one another and help each other. On the other hand, the “machismo” was handled in a completely different manner. To promote partner communication, we needed to understand this “cultural value” so we could empower participants without putting them at risk (e.g., domestic violence), but not openly address this value with participants.
CONCLUSION
Despite the great advances in cervical cancer discovery and development as well as implementation of novel strategies in cancer prevention and control, cervical cancer disparities still persist between Whites and Latinas, particularly among Latina immigrants. As such, the development, implementation, and evaluation of theory-based, culturally relevant interventions are an important step in narrowing this gap. However, there are a limited number of published papers on how to develop such interventions. The use of IM is a promising methodology in thinking logically and “completing the puzzle” in a very organized and well-thought-out manner. It has helped to facilitate the development of a novel intervention that focused on Latina immigrants which could be used as a template for interventions aimed at increasing primary and secondary prevention of cervical cancer in this population.
Acknowledgments
This work was supported by grants from the National Cancer Institute: R01CA111799; R03CA093143; U01CA086117.
REFERENCES
- Airhihenbuwa CO. Health promotion and disease prevention strategies for African Americans: A conceptual model. In: Braithwaite RL, Taylor SE, editors. Health issues in the Black community. San Francisco, CA: Jossey-Bass; 1992. pp. 267–280. [Google Scholar]
- American Cancer Society. Cancer facts & figures, 2009. Atlanta, GA: Author; 2009. Retrieved from http://www.cancer.org/docroot/STT/content/STT_1x_Cancer_Facts__Figures_2009.asp. [Google Scholar]
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Intervention mapping: Designing theory- and evidence-based health promotions programs. Mountain View, CA: Mayfield; 2001. [Google Scholar]
- Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Preventive Medicine. 2004;39:465–473. doi: 10.1016/j.ypmed.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Bellg AJ, Borelli B, Resnick B, Hecht J, Minicucci DS, Ory M, Czajkowski S Treatment Fidelity Workgroup of the NIH Behavior Change Consortium. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology. 2004;23:443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Byrd T, Chavez R, Wilson KM. Barriers and facilitators of cervical cancer screening among Hispanic women. Ethnicity & Disease. 2007;17:129–134. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Compendium of HIV prevention interventions with evidence of effectiveness. Atlanta, GA: Author; 1999. [Google Scholar]
- Chavez LR, Hubbell FA, McMullin JM, Martinez RG, Mishra SI. Structure and meaning in models of breast and cervical cancer risk factors: A comparison of perceptions among Latinas, Anglo women, and physicians. Medical Anthropology Quarterly. 1995;9:40–74. doi: 10.1525/maq.1995.9.1.02a00030. [DOI] [PubMed] [Google Scholar]
- Chavez LR, Hubbell FA, Mishra SI, Valdez RB. The influence of fatalism on self-reported use of Papanicolaou smears. American Journal of Preventive Medicine. 1997;13:418–424. [PubMed] [Google Scholar]
- Dickey LL, Petitti D. A patient-held mini-record to promote adult preventive care. Journal of Family Practice. 1992;34:457–463. [PubMed] [Google Scholar]
- Fernández ME, Diamond PM, Rakowski W, Gonzales A, Tortolero-Luna G, Williams J, Morales-Campos DY. Development and validation of a cervical cancer screening self-efficacy scale for low-income Mexican American women. Cancer Epidemiology and Biomarkers Prevention. 2009a;18:866–875. doi: 10.1158/1055-9965.EPI-07-2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez ME, Gonzales A, Tortolero-Luna G, Partida S, Bartholomew LK. Using intervention mapping to develop a breast and cervical cancer screening program for Hispanic farm workers: Cultivando la Salud. Health Promotion Practice. 2005;6:394–404. doi: 10.1177/1524839905278810. [DOI] [PubMed] [Google Scholar]
- Fernández ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W, Vernon SW. Effectiveness of Cultivando la Salud: A breast and cervical cancer screening promotion program for low-income Hispanic women. American Journal of Public Health. 2009b;99:936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gans KM, Kumanyika SK, Lovell HJ, Risica PM, Goldman R, Odoms-Young A, Lasater TM. The development of SisterTalk: A cable TV-delivered weight control program for Black women. Preventive Medicine. 2003;37:654–667. doi: 10.1016/j.ypmed.2003.09.014. [DOI] [PubMed] [Google Scholar]
- Garcés IC, Scarinci IC, Harrison L. An examination of sociocultural factors associated with health and health care seeking among Latina immigrants. Journal of Immigrant and Minority Health. 2006;8:377–385. doi: 10.1007/s10903-006-9008-8. [DOI] [PubMed] [Google Scholar]
- Hubbell FA, Chavez LR, Mishra SI, Valdez RB. Beliefs about sexual behavior and other predictors of Papanicolaou smear screening among Latinas and Anglo women. Archives of Internal Medicine. 1996;11:2353–2358. [PubMed] [Google Scholar]
- Koniak-Griffin D, Lesser J, Nyamathi A, Uman G, Stein JA, Cumberlan WG. Project CHARM: An HIV prevention program for adolescent mothers. Family and Community Health. 2003;26:94–107. doi: 10.1097/00003727-200304000-00003. [DOI] [PubMed] [Google Scholar]
- Marin G, Marin BV. Research with Hispanic populations. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Mendoza M, Petersen MC. New Latino immigration to Tennessee: Practicing culturally sensitive health care. Journal of the Tennessee Medical Association. 2000;93:371–376. [Google Scholar]
- Navarro AM, McNicholas JL, Senn KL, Kaplan RM, Campo MC, Roppe B. Use of cancer screening tests among Latinas: One and two years after participation in the Por La Vida Darnos Cuenta program. Women and Cancer. 2000;2:23–30. [Google Scholar]
- Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. American Journal of Preventive Medicine. 1998;15:32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- Pan American Health Organization. A brief snapshot of the situation: Cervical cancer in Latin America and the Caribbean, 2001. 2001 Retrieved from http://www.paho.org/English/HCP/HCN/CCBriefSnapshot.htm. [Google Scholar]
- Pisani P, Parkin DM, Bray F, Ferlay J. Estimates of worldwide mortality from 25 cancers in 1990. International Journal of Cancer. 1999;83:870–873. doi: 10.1002/(sici)1097-0215(19991210)83:6<870::aid-ijc35>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Rock CL, Michael CW, Reynolds K, Ruffin MT. Prevention of cervix cancer. Critical Reviews in Oncology/Hematology. 2000;33:169–185. doi: 10.1016/s1040-8428(99)00073-6. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. The Health Belief Model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 1990. pp. 39–61. [Google Scholar]
- Scarinci IC, Beech BM, Kovach KW, Bailey T. An examination of sociocultural factors associated with cervical cancer screening among low-income Latina immigrants of reproductive age. Journal of Immigrant Health. 2003;5:119–128. doi: 10.1023/a:1023939801991. [DOI] [PubMed] [Google Scholar]
- Shepherd J, Peersman G, Weston R, Napuli I. Cervical cancer and sexual lifestyle: A systematic review of health education interventions targeted at women. Health Education and Research. 2000;15:681–694. doi: 10.1093/her/15.6.681. [DOI] [PubMed] [Google Scholar]
- Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: Results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- Tortolero-Luna G, Mitchell MF, Swan DC, Tucker RA, Wideroff L, Icenogle JP. A case-control study of human papillomavirus and cervical squamous intraepithelial lesions (SIL) in Harris County, Texas: Differences among racial/ethnic groups. Cadernos de Saúde Pública. 1998;14:149–159. doi: 10.1590/s0102-311x1998000700015. [DOI] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services. The Surgeon General’s call to action to promote sexual health and responsible sexual behavior. Washington, DC: Author; 2001. [Google Scholar]
- Valdez A, Banerjee K, Ackerson L, Fernandez M. A multimedia breast cancer education intervention for low-income Latinas. Journal of Community Health. 2002;27:33–51. doi: 10.1023/a:1013880210074. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Mangan P, Mandelblatt J. Effectiveness of interventions to increase Papanicolaou smear use. Journal of the American Board of Family Practice. 2003;16:188–203. doi: 10.3122/jabfm.16.3.188. [DOI] [PubMed] [Google Scholar]
- Yancey AK, Tanjasiri SP, Klein M, Tunder J. Increased cancer screening behavior in women of color by culturally sensitive video exposure. Preventive Medicine. 1995;24:142–148. doi: 10.1006/pmed.1995.1027. [DOI] [PubMed] [Google Scholar]
- Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of cancer screening practices by Hispanic women: Analysis by subgroup. Preventive Medicine. 1999;29:466–477. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- Zapka JG, Harris DR, Hosmer D, Costanza ME, Mas E, Barth R. Effect of a community health center intervention on breast cancer screening among Hispanic American women. Health and Services Research. 1993;28:223–235. [PMC free article] [PubMed] [Google Scholar]