Abstract
Few natural disasters or intentional acts of war or terrorism have the potential for such severe impact upon a population and infrastructure as the intentional detonation of a nuclear device within a major U.S. city. In stark contrast to other disasters or even a “dirty bomb,” hundreds of thousands will be affected and potentially exposed to a clinically significant dose of ionizing radiation. This will result in immediate deaths and injuries and subsequently the development of Acute Radiation Syndrome (ARS). Additionally, millions more who are unlikely to develop ARS will seek medical evaluation and treatment, overwhelming the capacity of an already compromised medical system. In this paper, we propose that in vivo electron paramagnetic resonance (EPR) dosimetry be utilized to screen large numbers of potentially exposed victims, and that this screening process be incorporated into the medical-surge framework that is currently being implemented across the nation for other catastrophic public health emergencies. The National Incident Management System (NIMS), the National Response Framework (NRF), the Target Capabilities list (TCL), Homeland Security Presidential Directives (HSPD), as well as additional guidance from multiple federal agencies provides a solid framework for this response. The effective screening of potentially exposed victims directly following a nuclear attack could potentially decrease the number of patients seeking immediate medical care by greater than 90%.
Keywords: biological indicators, dosimetry, electrons, radiological terrorism
Introduction
The Intentional use of a nuclear weapon against the citizens of the United States is one of the most terrifying threats this nation faces. If a highly motivated and skilled terrorist or adversary were to detonate a nuclear device within a major U.S. city, it would immediately kill thousands of innocent citizens at the epicenter; traumatically injure, burn, or irradiate tens of thousands of additional citizens; and displace millions more (Bell and Dallas 2007). These factors, along with a significant loss of critical infrastructure and many billions of dollars worth of property damage, illustrate the contrast to other disasters and even “dirty bombs.” Over time, the deposition of radioactive fallout would affect millions of people for hundreds of miles extending out from ground zero, with long-lasting effects upon agriculture and other land uses (Hinton et al. 2007). In stark contrast to Hurricane Katrina (Franco et al. 2006; Meade and Molander 2006), a nuclear attack would likely come without warning and cause overwhelming death, injury, and illness in a very short period of time (Born et al. 2007). The initial emergency response would be severely handicapped by the shear scope of the incident and the direct loss of first responders and critical infrastructure such as hospitals, medical clinics, and fire and police stations (Dallas and Bell 2007). Electronic devices within the area would be immediately destroyed or rendered inactive by the electromagnetic pulse (EMP), seriously impacting communications and command and control. In spite of this overwhelmingly catastrophic event, the nation will have to respond quickly and efficiently to minimize the death and injury of our citizens.
The rapid screening of large numbers of victims at community-based treatment facilities would be critical to separate the worried-well from those truly affected to ensure that those victims who required medical care would receive it in a timely and efficient manner (Gale 1987; CDC 2007; Goans 2007). The surviving population would suffer from a wide spectrum of radiation exposure manifesting with different degrees of acute radiation syndrome (ARS), and when combined with other injuries, would yield variable survivability (Waselenko et al. 2004). This differing degree of injury and illness, the loss of infrastructure and the continuing nature of the event would further complicate the initial response, search and rescue, and eventual recovery process.
In this paper, we present an analysis of key factors that should be present to respond to a catastrophic nuclear event on U.S. soil, with special emphasis on the necessary capability to perform immediate biodosimetry screening for a large number of potentially exposed victims. We support the use of in vivo Electron Paramagnetic Resonance (EPR) as one of the biodosimetric technologies to provide the needed capability for screening and complementing the medical triage process for ARS. In vivo EPR dosimetry is a Viable method of accurately determining the dose of ionizing radiation received by a victim of a nuclear device detonation (Williams et al. 2007, 2010) and is a technology that can be incorporated into existing systems in the United States to deal with catastrophic public health emergencies.
Background and Context
Scope and unique aspects of a catastrophic nuclear event
The intentional detonation of a nuclear device upon U.S. soil is one of the 15 scenarios the U.S. Department of Homeland Security (DHS) describes that could have a significant impact on this nation (U.S. DHS 2005). A catastrophic nuclear event has several important characteristics that make this scenario especially troublesome. An adversary such as a terrorist can specifically target a highly populated urban area that also contains important secondary targets, including infrastructure necessary for critical government or civilian functions. An attack could also be timed to significantly impact world events, such as an election. An intentional attack would likely come without warning to maximize death and destruction. The combined blast overpressure, radiation and thermal effects would lead to more widespread destruction than even a major hurricane or earthquake (Alt et al. 1989). The initial response would be significantly hindered by the widely impacted area and by the direct loss, contamination or injury of first responders, and the subsequent loss of medical infrastructure necessary to care for large numbers of patients. Also, first responders would be required to closely monitor their environment and would be limited by the need to wear personal protection equipment during rescue and recovery operations. These first responders would also face an onslaught of a large civilian population requiring decontamination, screening, medical treatment, housing, food, water, and eventual evacuation from the affected area. In addition, a nuclear event continues to evolve over time, with increasing numbers of victims, continued loss of infrastructure, and the ongoing progression of the affected area from fallout deposition.
The medical effects of other public health emergencies may be minimized by immunizations, prophylaxis, isolation and quarantine, barrier protection, and even some basic healthcare practices, such as social distancing and hand washing. Managing casualties from a nuclear attack, on the other hand, will significantly challenge this nation. Medical interventions for radiation exposures are severely limited and require specific screening and triage to identify patients requiring specialized medical care. Survivors of a nuclear event will need to be screened rapidly and triaged into the appropriate medical care category to increase survivability (Weinstock et al. 2008). In more severe cases of ARS, medical resources across the nation will be limited in availability (Kaji et al. 2006). Furthermore, these medical interventions have a higher efficacy the sooner they are given after exposure, further highlighting the need for a rapid screening process (Jarrett et al. 2007).
Previously-published modeling efforts have demonstrated the distribution of casualties from a nuclear device detonation in a population center such as the District of Columbia (Dallas 2008), resulting in hundreds of thousands of casualties from prompt thermal and radiation effects, along with additional casualties resulting from blast pressure wave effects, thermal burns, and fallout radiation exposure (U.S. DHS 2005). There would also be a complete and immediate loss of infrastructure within several kilometers of the initial blast area, and continuing radiation exposure would contaminate the surrounding area depending on the initial blast size, weather patterns, and structural protection.
Unaffected hospitals, clinics, and other community-based facilities in the entire region would be quickly overwhelmed and will run short of critical medical supplies, personal protection equipment, and staff needed to continue to care for patients from the incident or to continue providing ongoing critical medical care within the region.
Impact on population level
To further complicate matters, after an event of such magnitude there are two important populations that need attention. The first population includes those patients with true radiation exposures, injury, and illness; and the other includes those patients presenting with psychological distress and/or who are minimally exposed or not exposed at all, otherwise known as the worried-well. The first group, patients with varying degrees of radiation exposure and injury, will require different medical needs often at different times. The different degrees of protection that people might obtain from shelter, length of exposure, and varying patterns of fallout would result in a wide distribution of individual radiation exposure-dose. The second group, the worried-well, could number millions more. The need to identify victims within each of these groups that have been sufficiently exposed and require further triage into the appropriate medical care is essential to match the need of victims to the resources that are currently available to respond to the incident. This need to separate the worried-well from those truly affected highlights the necessity for a rapid screening capability to accommodate entire populations.
Acute radiation syndrome and its physiologic effects
Acute radiation syndrome occurs when an individual has symptoms and physiologic changes following exposures to substantial doses of ionizing radiation. Although the threshold at which patients become symptomatic following substantial exposure to ionizing radiation varies, an immediate one-time dose of 0.75 Gy to 1 Gy is sufficient to cause symptoms of nausea (CDC 2005). Lower blood lymphocyte counts are noted within several days in people who have received 1 Gy to 3 Gy, along with vomiting and weight loss; this is referred to as hematopoietic syndrome. At higher doses of 3 Gy to 6 Gy, the gastrointestinal syndrome is evident, characterized by excessive diarrhea and risk of infection from a shedding intestinal lumen and decreased immune system function. Due to both the severity of symptoms and challenges in medical management, the expected mortality rate in this exposure range is approximately 50%. Doses exceeding 10 Gy are nearly always fatal, due to cerebrovascular syndrome resulting from brain edema, central nervous system damage, and vascular effects. As a further predictor of expected mortality, radiation overexposure is categorized into two lethal dose ranges for the population who receive no medical treatments during the 60-d period following a nuclear device detonation. The lethal dose for 50% of patients exposed after 60 d without treatment (LD50/60) is approximately 3.5 Gy. The lethal dose for 90% of patients exposed after 60 d without medical treatment (LD 90/60) is approximately 5 Gy. The main factor leading to 60-d mortality in these cases is infection from gastrointestinal symptoms, complicated by a compromised immune system (AFRRI 2003; Waselenko et al. 2004; CDC 2005; Jarrett et al. 2007; U.S. DHHS 2008).
The syndrome of the worried-well
Complicating the variation in exposure dose for the truly exposed population from the initial blast and fallout is the impact of the worried-well, which could potentially number millions more.
Many patients who are not directly ill or injured from an actual event become increasingly anxious and concerned about their own health, which can also exacerbate underlying psychological or chronic medical conditions. Often these patients feel they have valid medical concerns and seek medical assistance and treatment alongside patients who are ill or directly injured from the incident. Unfortunately, these patients commonly arrive first, expecting the healthcare infrastructure to perform effective medical screening for symptoms and exposure-dose assessment and potentially delaying treatment of patients actually requiring care (Okumura et al. 1998a). The ratio of worried-well to those actually affected would likely be between five to one and ten to one (U.S. DHS 2005). Therefore, entire populations might be psychologically stressed, with many exhibiting the initial signs and symptoms of ARS. Nausea and vomiting are typical early symptoms of ARS, where time to emesis is regarded as a dose-screening tool that indicates individual exposure-dose. However, these symptoms are also commonly seen in patients who are extremely distressed or in close proximity to patients exhibiting similar symptoms—potentially confounding this method's reliability (Demidenko et al. 2010).
Modern examples have demonstrated significant numbers of people in psychological distress compared to those truly affected. Even with an effective strategy of public notification and timely evacuation, this population will continue to overburden the emergency response system.
Case example of small population affected: Goiania, Brazil, 1987
The 1987 Goiania, Brazil, incident illustrates how the worried-well syndrome can permeate a population, even when only a small percentage is affected. A 137Cs source at an abandoned hospital was scavenged, disassembled and distributed within a community. Some 250 individuals were directly contaminated, resulting in four deaths from sepsis and hemorrhaging related to ARS. These patients were identified in part from an Olympic stadium setup for screening and identification of the population. Over 112,000 individuals were initially monitored for external radioactive contamination and symptoms, resulting in the identification of approximately 250 individuals with signs of radioactive contamination. This resulted in a ratio of worried-well to directly-affected of over 400 to 1 (IAEA 1988).
Case example of emergency response medical surge: 1995, Tokyo, subway sarin attacks
The 1995 Tokyo subway sarin attack is another example of the impact of the worried-well on emergency response. During the peak morning commute at approximately 8 AM, a religious cult released sarin gas aboard subway trains. Patients began arriving with symptoms at a nearby hospital within 30 minutes, and within one hour nearly 500 patients presented. As the incident continued to evolve and intense media reporting continued, there was a constant flow of patients arriving at medical facilities throughout the day. By the end of the incident, the total medical surge involved over 250 Tokyo hospitals and clinics. These facilities confirmed that they had examined over 5,500 patients, and there were additional unconfirmed reports that closer to 9,000 patients had presented to local healthcare facilities. Of those 5,500 confirmed patients, 98 were hospitalized. An additional 984 were determined to be moderately ill, 37 were severely ill, 17 were critically injured, and there were no fatalities. In this case, with the confirmed number of examined patients actually exhibiting symptoms, the ratio of worried-well to sick patients was at least 4 to 1. One possible confounder of this statistic is that the symptoms of sarin exposure closely model those of extreme distress, such as nausea, vomiting and headache, with no diagnostic test to rule out the possibility of exposure (Okumura et al. 1998a).
Case example of population-based screening and prophylaxis: 2001 United States anthrax attacks
During the October 2001 anthrax attacks—the first bioterrorism attack within the United States—a series of contaminated letters was mailed to high-profile public figures such as Senator Tom Daschle and Tom Brokaw of NBC News. Additionally, postal workers from postal processing facilities in Maryland and New Jersey were directly affected, and several bystanders became symptomatic from cutaneous or inhalation anthrax. In all, some 22 individuals developed anthrax poisoning and 5 died. Over 20,000 were determined to be at risk and advised to seek treatment in the form of medical prophylaxis. Over 200,000 individuals were estimated to have eventually contacted health departments, emergency rooms, or local healthcare providers requesting either diagnostic testing or antibiotic prophylaxis. In this case, the ratio of worried-well to those at risk was well over 100 to 1 (Blank et al. 2003).
Medical Response to a Nuclear Event
Difficulties encountered by first responders in a nuclear event
First responders will face a seemingly impossible task when initially responding to a nuclear event Each individual responder will be overwhelmed with the scope of death and destruction before them and will have considerable personal concerns about their own health and the health of their families. Their initial task will be to establish order and scene safety, then to proceed to decontaminate, perform search and rescue, evacuate, screen, triage and treat patients. Initially they will have very little support and will only have the resources currently available to them. Over time, the nation will provide a massive and prolonged response, optimally utilizing systems already in place for other public health emergencies. Most likely, medically trained first responders will not be available for performing radiation-dose-exposure screening, since their primary focus would be on evacuation, decontamination, initial treatment of the sick and injured, and search and rescue. A significant advantage of in vivo EPR dosimetry screening is that non-medically trained personnel can operate the equipment.
Resolving the difficulty in mass casualty care: Community-based response centers
Over the past several years, the federal government has provided guidance on how to provide medical surge capacity during a catastrophic public health emergency. The cornerstone of this guidance is the Medical Surge Target Capabilities List (TCL) (U.S. DHS 2007). By and large, each state has come up with a way of increasing hospital-based surge capacity and providing community-based surge capacity when hospital resources are overwhelmed. One common method is known as the Modular Emergency Medical System or MEMS (U.S. Army SBCCOM 2001a). This system provides guidance to states, sub-state regions, and communities to develop emergency response modules such as Neighborhood Emergency Help Centers (NEHC) (U.S. Army SBCCOM 2001b) or Acute Care Centers (ACC) (U.S. Army SBCCOM 2003). The NEHC would provide outpatient treatment, while an ACC would provide low acuity inpatient treatment within community-based buildings of opportunity during catastrophic public health emergencies. The NEHC can provide basic medical evaluation, treatment and support for mass casualty care, depending on the exact scenario and exact care required. An ACC can provide a basic level of care within a community-based setting for patients who would normally be hospitalized. The Centers for Disease Control and Prevention (CDC) has also provided guidance for the development of Points of Distribution (PODs). PODs are designed to provide prophylactic antibiotics to large urban areas in response to an anthrax attack (AHRQ 2004). The CDC has provided models for radiological reception centers to service evacuated populations and monitor them for external contamination (CDC 2007).
Regardless of the specific incident, each of the community-based treatment models has common elements. Within these community-based response centers is the need to greet, register, track, screen and sort (e.g., triage) individuals for further medical management, action and/or treatment with a high patient throughput of 250–500 per hour using multiple stations. Staffing considerations include medically-trained personnel, such as physicians and nurses, for medical screening, and non-medically-trained personnel, such as administrative support, police, and volunteers, to total approximately 150 personnel. These staffing considerations can be optimized to deliver specific treatment depending on the incident.
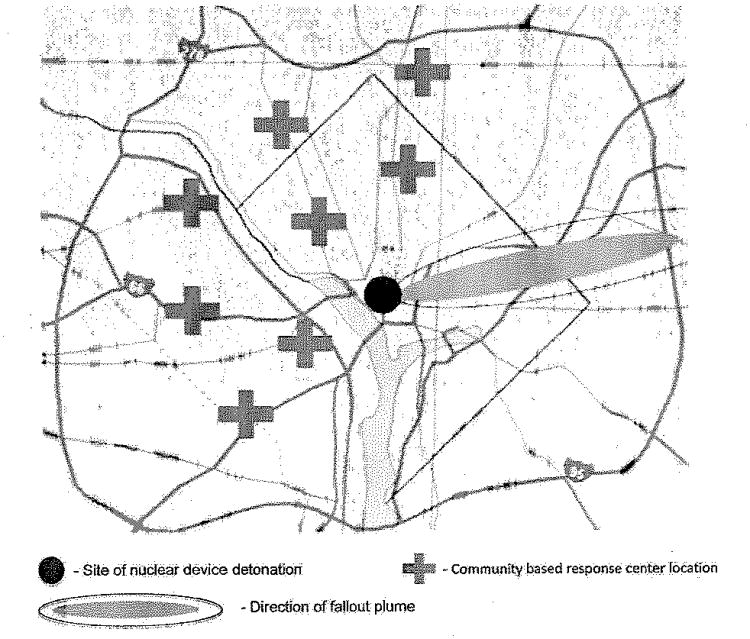
Optimum location of such community-based response centers should be in safe zones, along paths of evacuation from the area affected by the nuclear detonation and fallout deposition zones. Establishing these centers at obvious landmarks, major transportation routes, and in close proximity to healthcare facilities while making the locations accessible by public and emergency transportation will aid patients in seeking medical care, screening, and assistance. Fig. 1 highlights theoretical placement of such community-based response centers related to a generalized nuclear detonation in Washington, DC (Fig. 1) (Nationalatlas.gov).
Fig. 1.
Up to this point, we have considered the needed capability for after-the-fact dose estimation of radiation exposure level in the context of a catastrophic nuclear event involving a large number of people. In the remainder of this paper we will focus on a framework we have developed to implement in vivo EPR dosimetry technology considering factors at the micro and macro system level.
An Emergency Response Framework that Incorporates EPR Technology for Improved Response to a Nuclear Attack
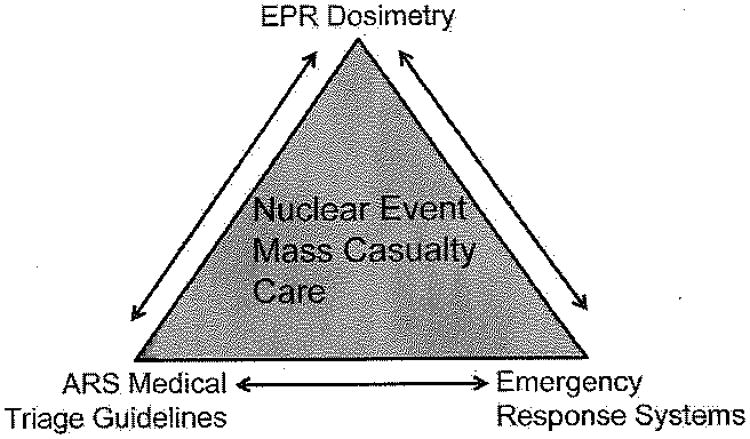
In the context of emergency response to a catastrophic nuclear event, three interrelated components are essential to provide effective and efficient screening, medical triage for the ARS, and medical treatment. These components include a) a high throughput biodosimetry technology, b) an emergency response system that would deliver the capability provided by the technology, and c) the policies and guidelines that will support the technology and emergency support system (Fig. 2).
Fig. 2.
The Emergency Response Systems
The emergency response system is one of the key components of this framework; the integration of biodosimetry technologies into existing emergency response systems would increase their usefulness and provide the needed screening capacity and capabilities.
As emergency response methodology continues to develop an all-hazards approach (Hodge et al. 2007) for response to threats that face the nation, response models are increasingly more generalized for the various threats of natural disasters, pandemic disease outbreaks, and acts of terrorism. A biodosimetry method suited for population-based screening subsequent to a nuclear event should be easily integrated into community-based response centers. In order to accomplish such seamless integration, biodosimetry methods should be congruent with existing systems in terms of staffing requirements and cycle times and resources with immediate results.
A consolidated model for emergency response: The Target Capabilities Framework
The United States Department of Homeland Security has proposed a framework for examining the threats to this nation using an all-hazards approach. The National Incident Management System (NIMS) (U.S. DHS 2004) provides a standardized command and control system for incident response, and the National Response Framework (NRF) (U.S. DHS 2008) provides the guidance for response, roles and responsibilities. The Target Capabilities List (TCL) (U.S. DHS 2007) within the NRF uses the principles of threat analysis that created the National Planning Scenarios, of which the 10 kt detonation of an improvised nuclear device in a metropolitan area is included (U.S. DHS 2005). Within the mission area analysis, the Homeland Security All-Hazards Taxonomy was developed, including four mission areas of prevention, prediction, response, and recovery. Meeting the need for medical evaluation and triage of the millions potentially affected by a catastrophic nuclear event falls into the response category of caring for the public. Corresponding response mission capabilities relevant to catastrophic nuclear events include:
emergency triage and pre-hospital treatment;
medical surge capabilities; and
medical supplies management and distribution.
Within these mission capabilities are specific tasks and effective strategies for the response to a catastrophic nuclear event. Supporting this framework is Homeland Security Presidential Directive 21 (HSPD-21), highlighting a national strategy for public health and medical preparedness in response to catastrophic health events such as weapons of mass destruction. HSPD-21 outlines requirements for mass casualty care and stresses the importance of a rapid and integrated approach (The White House 2008).
Emergency triage and pre-hospital treatment
The all-hazards community-based response centers share certain embedded requirements to triage populations for ARS. A biodosimetry method that functions as a high accuracy screening test will provide results of clinical relevance to medical management and treatment. This method must be able to, at a minimum, accurately separate the worried well from those who will truly become symptomatic from ARS. Therefore, up to 90% of patients may be eliminated as unlikely to develop any acute symptoms. That is, the 5:1 to 10:1 ratio of worried-well patients to those truly affected and symptomatic may be rapidly ruled out. A screening test able to accurately predict the ARS sub-syndromes is of additional value. In addition, this biodosimetry method should provide an immediate result well within just several minutes per patient. Ideally it would also provide or integrate individual dose exposure into Emergency Medical Services (EMS) run report databases or hospital-or field-deployed electronic medical records systems. Thus, such a method will provide direct input to the existing all-hazards community-based response models.
Medical surge
Resource allocation is a key component of medical surge considerations. When dedicated laboratories or healthcare professionals are involved in screening populations, those resources are less available for the treatment and management of casualties. In the scenario of a catastrophic nuclear event, the surrounding region and neighboring states will be significantly impacted and will also have a decreased ability to respond. System level capacity of those services will also be degraded. Likewise, resource allocation at the clinical microsystem level is just as important. Within community-based centers, the ability for such screening tests for ARS to be operated by non-medically trained personnel will enable clinical specialists and providers to focus upon delivering care to those who are in greatest need.
Medical equipment and supplies—management and distribution
Two key considerations for medical equipment and supply management and distribution are portability and consumable materials. For integration into national assets such as the Strategic National Stockpile, the portability of a biodosimetry method is a key consideration. As supplies are staged for delivery anywhere in the country with a maximum response time within 12 h, the size, portability, ability to withstand temperature extremes, ability to be stored for extended periods of time and remain functional, and rapid setup and ease of operation once onsite are all vital aspects. In terms of sustaining operations onsite, minimizing the amount of consumable materials required and the specialty nature of required consumables also enhances sustainable operations.
Biodosimetry Methods and EPR
In this section, we discuss a potentially useful physical biodosimetric technology that can provide the needed capability for mass casualty triage in the event of a catastrophic nuclear incident. In utilizing biodosimetry methods for assessing radiation exposure dose to determine treatment, we maintain that no one method forms a comprehensive solution. We need to use multiple complementary methods, from the population-screening scenario to the clinic and hospital setting, properly allocating and utilizing both medical and non-medical resources, to effectively address the impact of ARS upon victims and patients.
Capacity of current biodosimetry methods
Current biodosimetry methods are very limited in their capability to respond to the tens to hundreds of thousands of expected victims of a catastrophic nuclear event. As individual symptoms are not reliable enough to rule out ARS, screening is vital to ensure that symptomatic patients who have received high levels of radiation exposure are accurately diagnosed. Biodosimetry methods should be designed to accommodate such high throughput; current methods are limited in terms of throughput and cycle time. Additionally, deployable biodosimetry methods should be capable of patient-screening cycle times that match the throughput of community-based response centers. This ensures that the appropriate number of biodosimetry processing applications may be allocated to each site to screen the population in need.
The in vivo EPR dosimetry method
In vivo EPR tooth dosimetry has the ability to fill the need for population-based screening due to its characteristics and inherent advantages compared to other methods. In vivo EPR dosimetry possesses several properties relevant to population-based screening. It
is non-invasive;
is not affected by biological processes such as stress or repair mechanisms;
has a long-term stability of signal over time;
is able to provide output immediately after the measurement;
is able to operate in a variety of environments;
is able to be operated by minimally trained individuals; and
has a minimal cost per measurement.
Integration of EPR technology into emergency response for a nuclear attack
The inherent characteristics of in vivo EPR dosimetry enable the technology to easily integrate into emergency response systems to meet the need for screening of mass casualties. The technology is highly deployable, with individual unit prototypes that are tabletop-sized and weigh less than 50 kg now in development. These current systems have a standard error of prediction of approximately 150 cGy for inserted molar teeth and 200–250 cGy for intact canine teeth based upon 5-min measurements with the potential for reducing this error to 50 cGy (Williams et al. 2010; Demidenko et al. 2007). The ability to provide the result immediately makes this method feasible for emergency response systems where follow-up tracking is impractical. The current cycle time of 5 min enables this method for high-throughput primary screening of hundreds of patients per hour at a response center when using multiple systems. Such a design will make in vivo EPR dosimetry feasible for immediate population-based screening to rule out the worried-well within existing systems for emergency response. For purposes of rapid screening, the uncertainty can be as high as ±100 cGy and yet still be very useful for screening. In vivo EPR dosimetry does measure cumulative lifetime dose; however, the varying baseline levels across the general population would be expected to have negligible impact on the screening process and their eventual triage.
Comparison with other methods
Other methods of screening for ARS, such as lymphocyte depletion kinetics and cytogenetics, have been successfully used in small incidents. However, these methods require intensive clinical resources, such as laboratories to process biological samples (e.g., blood collection), and are complicated by both transportation logistics and the time it takes to transport and process laboratory tests (up to many days for cytogenetics). Deploying these assets with appropriately trained personnel to affected areas during a large-scale accident would be a major challenge. Newer biologically-based methods still in development have some potential. But even if these methods can be made fully field-deployable and won't require transport to specialized laboratories, they are likely to have a high potential for results to be confounded by factors like stress and trauma. These inherent negative characteristics of other biodosimetry methods pose significant limitations and barriers for implementation for mass casualty care in a nuclear event. In contrast, physically-based dosimetric techniques, especially in vivo EPR dosimetry, can be optimized for functioning in such an environment.
The EPR dosimetry human-subjects exercise
A human-subjects exercise was conducted in May 2008 to demonstrate the ability of the in vivo EPR dosimetry technology under development, to attempt its integration into emergency response systems, to explore the relationship with medical triage guidelines, and to evaluate and improve further development, with key input from relevant end users. This exercise, conducted by the Dartmouth EPR Center for Viable Systems and the New England Center for Emergency Preparedness (NECEP), demonstrated the current capabilities of the technology using 10 simulated exposed human subjects from a catastrophic nuclear event. The details of this exercise and relevance to in vivo EPR dosimetry as a tool for population-based screening and integration are discussed in a companion paper (Nicolalde et al. 2010).
ARS Medical Triage Guidelines
Effective screening tools for ARS, such as in vivo EPR dosimetry, and the community-based emergency response systems that use such screening tools will need appropriate medical triage guidelines to further separate those that have a higher level of exposure and therefore an increased probability to develop ARS. Conventional triage systems can rapidly categorize patients according to the patient's level of injury, whether or not they have an immediate need for lifesaving interventions, and their likelihood of survival. These systems have been tested and proven in a historical context, and continue to be used in mass casualty environments including both natural and manmade disasters. In a catastrophic nuclear event, these triage categories are complicated for those with either injury or radiation exposure alone and further complicated by combined injury and exposure, and the fact that non-clinical personnel will perform the screening. Refinement of these triage categories will ensure their accuracy when combined with in vivo EPR dosimetry screening. The screening will then properly identify patients according to their predicted dose response, therefore being a valuable tool to help balance the need for clinical care with the current medical resources available.
Refinement of medical triage guidelines should include categories that reflect the predicted physiologic response and symptoms of ARS. Categories should also include broad guidelines of medical treatment and management, employing therapies and novel treatments where they may benefit patients the most. Consideration of the appropriate care setting and clinical resource burden of patients in those respective triage categories will ensure proper resource allocation. Overall, this process will enable planners and clinical decision makers to consider the impact and burden of patients categorized by this process and to structure the entire response of mass-casualty care accordingly.
Since high-accuracy biodosimetry methods such as in vivo EPR dosimetry can effectively screen victims in a large population exposed during a catastrophic nuclear event, these measurements may be used to not only refine triage categories for radiation exposure dose, but also to involve considerations for medical management, treatment, and resource allocation. The details of triage category modification and other considerations are discussed in a companion paper (Rea et al. 2010).
Conclusion
The detonation of a nuclear device in an urban area within the United States would significantly challenge and overwhelm this nation's response capability. Critical to our ability to minimize the medical consequences of such an event is the capacity to screen and triage patients into the appropriate medical care required. In this setting, timely and appropriate medical care can decrease the morbidity and mortality seen in such an event. Current clinical methods to screen for radiation exposure may be inaccurate; for example, emesis can be a manifestation of psychological stress. Current laboratory methods can accurately measure the radiation dose received, but have severe logistical, time and staffing limitations that make them impractical for use in catastrophic settings. In vivo EPR dosimetry, utilized within the current national efforts to respond to public health emergencies, can be an effective tool with the potential to significantly increase the survivability of victims of a catastrophic nuclear attack.
Acknowledgments
Research supported by the National Institute of Health (NIH) award number U19AI067733, and Defense Advanced Research Project Agency (DARPA) award number HR0011-08-C-0023.
Disclaimer: The views, opinions, and/or findings contained in this article are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the Defense Advanced Research Projects Agency or the Department of Defense.
Disclaimer from J. A. Geiling: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
References
- Agency for Healthcare Research and Quality. The Weill/Cornell bioterrorism and epidemic outbreak response model. [Accessed 28 October 2008];2004 Available at ahrq.goV/research/biomodel3/
- Alt LA, Forcino DC, Walder RI. Nuclear events and their consequences. In: Walker RI, Cerveny TJ, editors. Medical consequences of nuclear warfare Part I, vol 2 Textbook of military medicine. Falls Church, VA: TMM Publications, Office of the Surgeon General; 1989. [Google Scholar]
- Armed Forces Radiobiology Institute. Medical management of radiological casualties handbook. Bethesda, MD: Armed Forces Radiobiology Research Institute; 2003. [Google Scholar]
- Bell WC, Dallas CE. Vulnerability of populations and the urban health care systems to nuclear weapon attack—examples from four American cities. Int J Health Geogr. 2007;6(5) doi: 10.1186/1476-072X-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank S, Moskin LC, Zucker JR. An ounce of prevention is a ton of work: Mass antibiotic prophylaxis for anthrax, New York City, 2001. [Accessed 28 October 2008];Emerg Infect Dis. 2003 Jun; doi: 10.3201/eid0906.030118. Available at cdc.gov/ncidod/EID/vol9no6/03-0118.htm. [DOI] [PMC free article] [PubMed]
- Born CT, Briggs SM, Ciraulo DL, Frykberg ER, Hammond JS, Hirshberg A, Lhowe DW, O'Neill PA. Disasters and mass casualties: I. General principles of response and management. J Am Acad Orthop Surg. 2007;15:388–396. doi: 10.5435/00124635-200707000-00004. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Acute radiation syndrome: A fact sheet for physicians [online] [Accessed 28 October 2008];2005 Available at bt.cdc.gov/radiation/pdf/arsphysicianfactsheetpdf.
- Centers for Disease Control and Prevention. Population monitoring in radiation emergencies: a guide for state and local public health planners. Atlanta, GA: Centers for Disease Control and Prevention (CDC); 2007. [Google Scholar]
- Dallas CE. Impact of small nuclear weapons on Washington, DC: Outcomes and emergency response recommendations. [Accessed 27 October 2008]; Written statement to accompany testimony at the United States Senate Hearing for the Committee on Homeland Security and Governmental Affairs, titled “Nuclear terrorism: Confronting the challenges of the day after.” Available at hsgac.senate.gov/public/_files/041508Dallas.pdf.
- Dallas CE, Bell WC. Prediction modeling to determine the adequacy of medical response to urban nuclear attack. Disaster Med Public Health Prep. 2007;1:80–89. doi: 10.1097/DMP.0b013e318159a9e3. [DOI] [PubMed] [Google Scholar]
- Demidenko E, Williams BB, Swartz HM. Radiation dose prediction using time to emesis data in the case of nuclear terrorism. Radiat Res. 2009 doi: 10.1667/RR1552.1. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco C, Toner E, Waldhorn R, Maldin B, O'Toole T, Inglesby TV. Systemic collapse: Medical care in the aftermath of Hurricane Katrina. Biosecur Bioterror. 2006;4:135–146. doi: 10.1089/bsp.2006.4.135. [DOI] [PubMed] [Google Scholar]
- Gale RP. Immediate medical consequences of nuclear accidents. Lessons from Chernobyl. JAMA. 1987;258:625–628. [PubMed] [Google Scholar]
- Goans RE. A note on the number of survey stations required in a mass casualty radiation event. Health Phys. 2007;93:705–706. doi: 10.1097/01.HP.0000275290.08589.f3. [DOI] [PubMed] [Google Scholar]
- Hinton TG, Alexakhin R, Balonov M, Gentner N, Hendry J, Prister B, Strand P, Woodhead D. Radiation-induced effects on plants and animals: Findings of the United Nations Chernobyl Forum. Health Phys. 2007;93:427–440. doi: 10.1097/01.HP.0000281179.03443.2e. [DOI] [PubMed] [Google Scholar]
- Hodge JG, Jr, Gostin LO, Vernick JS. The pandemic and all-hazards preparedness act: Improving public health emergency response. JAMA. 2007;297:1708–1711. doi: 10.1001/jama.297.15.1708. [DOI] [PubMed] [Google Scholar]
- International Atomic Energy Agency. The radiological incident in Goiania. Vienna: International Atomic Energy Agency; 1988. [Google Scholar]
- Jarrett DG, Sedlak RG, Dickerson WE, Reeves GI. Medical treatment of radiation injuries—Current US status. Radiat Meas. 2007;42:1063–1074. [Google Scholar]
- Kaji A, Koenig K, Bey T. Surge capacity for healthcare systems: a conceptual framework. Acad Emerg Med. 2006;13:1157–1159. doi: 10.1197/j.aem.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Meade C, Molander RC. Technical Report of the RAND Center for Terrorism Risk Management Policy. Santa Monica: RAND Corporation; 2006. Considering the effects of a catastrophic terrorist attack. [Google Scholar]
- Okumura T, Suzuki K, Fukuda A, et al. The Tokyo subway sarin attack: Disaster management, Part 1: Community emergency response. Acad Emerg Med. 1998a;5:613–617. doi: 10.1111/j.1553-2712.1998.tb02470.x. [DOI] [PubMed] [Google Scholar]
- Okumura T, Suzuki K, Fukuda A, et al. The Tokyo subway sarin attack: Disaster management, Part 2: Hospital response. Acad Emerg Med. 1998b;5:618–624. doi: 10.1111/j.1553-2712.1998.tb02471.x. [DOI] [PubMed] [Google Scholar]
- National Atlas of the United States. State boundaries of the United States. [Accessed 5 November 2008]; Available at www.nationalatlas.gov/mld/statesp.html.
- U.S. Army Soldier and Biological Chemical Command. Modular emergency medical system: Expanding local healthcare structure in a mass casualty terrorism incident. Aberdeen: U.S. Army Soldier and Biological Chemical Command (SBCCOM); 2001a. [Google Scholar]
- U.S. Army Soldier and Biological Chemical Command. Neighborhood emergency help center: a mass casualty care strategy for biological terrorism incidents. Aberdeen: U.S. Army Soldier and Biological Chemical Command (SBCCOM); 2001b. [Google Scholar]
- U.S. Army Soldier and Biological Chemical Command. Modular emergency medical system: concept of operations for the acute care center (ACC) Aberdeen: U.S. Army Soldier and Biological Chemical Command (SBCCOM); 2003. [Google Scholar]
- U.S. Department of Health and Human Services. Radiation event emergency management, U.S. Dept. of Health and Human Services—REMM [online] [Accessed 31 October 2008];2008 Available at www.remm.nlm.gov/
- U.S. Department of Homeland Security. National Incident Management System. Washington, DC: U.S. Department of Homeland Security; 2004. [Google Scholar]
- U.S. Department of Homeland Security. National planning scenarios Created for use in national, federal, state, and local homeland security preparedness activities. Washington, DC: 2005. [Accessed 31 October 2008]. (draft). Available at: media.washingtonpost.com/wp-srv/nation/nationalsecurity/earlywarning/NationalPlanningScenariosApril2005.pdf. [Google Scholar]
- U.S. Department of Homeland Security. Target capabilities list. Washington, DC: U.S. Department of Homeland Security; 2007. [Google Scholar]
- U.S. Department of Homeland Security. National response framework. Washington, DG: U.S. Department of Homeland Security; 2008. [Google Scholar]
- Waselenko JK, MacVittie TJ, Blakely WF, et al. Medical management of the acute radiation syndrome: recommendations of the strategic national stockpile radiation working group. Ann Intern Med. 2004;140:1037–1051. doi: 10.7326/0003-4819-140-12-200406150-00015. [DOI] [PubMed] [Google Scholar]
- The White House. [Accessed 07 November 2008];Homeland Security Presidential Directive/HSPD-21. Available at www.whitehouse.gov/news/releases/2007/10/20071018-10.html.
- Weinstock DM, Case C, Jr, Bader JL, et al. Radiologic and nuclear events: Contingency planning for hematologists/oncologists. Blood. 2008;111:5440–5445. doi: 10.1182/blood-2008-01-134817. [DOI] [PMC free article] [PubMed] [Google Scholar]