Abstract
Hypersexual behavior has been identified as a sexual risk correlate among gay and bisexual men (GBM). The Hypersexual Behavior Inventory (HBI) has been shown to be a reliable and valid measure of hypersexual behavior in clinical populations, yet it has not been used to assess hypersexual behavior in non-clinical samples. We examined the psychometric properties of the HBI with survey data recorded between December 2009 and March 2010 in a sample of young men (N=366, M = 21.46 years old, SD = 1.95) who self-identified as gay (89%) or bisexual (11%), and assessed its association with unprotected receptive anal intercourse (URAI) partners and occasions. Using cross-sectional data of single, sexually active young GBM (YGBM), we used confirmatory factor analyses to test the HBI’s three-factor structure. Using negative binomial regressions, we then tested the association between the HBI subscales and sexual risk. After accounting for covariates, we found that sexual Control was a risk-factor for URAI partners and occasions, and Coping was found to be a protective factor for URAI occasions. In light of our findings, we discuss the importance of re-examining the theoretical assumptions of hypersexual behavior and propose HIV prevention strategies that may reduce young GBM’s vulnerability to HIV infection.
Keywords: hypersexuality, resilience, HIV, men who have sex with men, youth
Researchers have argued that HIV/AIDS risk may increase if individuals do not possess self-regulation in their sexual relationships (Benotsch, Kalichman, & Kelly, 1999; Coleman et al., 2010). Compared with men who exclusively have sex with women, gay and bisexual men (GBM) report higher rates of sex occasions and partners (e.g., Baum & Fishman, 1994; Cooper, Delmonico, & Burg, 2000; Parsons et al., 2008), and thus may have a higher likelihood of risky sexual behaviors that can lead to HIV infection. Indeed, young GBM (YGBM) account for nearly half of HIV/AIDS incidence, as well as the greatest increase in HIV/AIDS incidence between 2001 and 2006 compared to any other age group (Centers for Disease Control and Prevention [CDC], 2013). While not all sexual activity leads to an increased risk of sexually transmitted infection among YGBM (CDC, 2013), it is vital to understand the psychosocial correlates influencing young men’s risk-taking behaviors (Mustanski, Newcomb, DuBois, Garcia, & Grov, 2011). In this study, we examined the relationship between hypersexual and risky sexual behaviors in order to inform HIV prevention efforts for this population. Specifically, we contribute to these efforts by examining the psychometric properties of the Hypersexual Behavior Inventory (HBI; Reid & Carpenter, 2009) in a sample of YGBM and testing the relationship between scores on the inventory and unprotected receptive anal intercourse (URAI).
Hypersexual Behavior and Risky Sexual Behavior in YGBM
Hypersexual behavior is defined as, “difficulty regulating or diminishing sexual thoughts, urges, and behavior, to the extent that the individual or others experience negative consequences” (Reid & Carpenter, 2009, pg. 295). Thus, the clinical use of hypersexual behavior suggests a pathological dysregulation of sexual behavior that leads to dysfunctional and problematic life circumstances. Historically, there has been a lack of consensus among researchers regarding an appropriate name for the dysregulation of sexual behavior; a non-exhaustive list includes sexual compulsivity (Allers, Benjack, White, & Rousey, 1993), compulsive sexual behavior (Black, 1998), sexual addiction (Carnes, 1983), and sexual impulsivity (Barth & Kinder, 1987). Much of the past research on the relationship between sexual dysregulation and risky sexual behaviors is drawn from the investigation of sexual compulsivity; however, compulsive or addictive sexual behavior is driven by a perceived inability to control sexual behavior, and is often followed by intrusive and obsessive sexual urges (Carnes, 1983). Distinctively, hypersexual behavior is characterized as sexual behavior occurring in excess, as defined by individual or societal norms (Reid & Carpenter, 2009). Contrary to compulsive sexual disorder, hypersexual behavior need not reflect a perceived need to respond to a compulsive drive and/or an inability to control sexual behaviors. However, despite this distinction, past research on the significant relationship between sexual compulsivity and sexual risk behaviors underscores the importance of investigating the relationship between hypersexual behavior as a form of dysregulated sexual behavior and sexual risk behaviors.
Researchers have indicated a relationship between high scores on measures of sexual compulsivity and participation in risky sexual behavior (Benotsch et al., 1999; Coleman et al., 2010; Dodge et al., 2008; Grov, Parsons, & Bimbi, 2010). For sake of clarity, we used the nomenclature used by authors to define their samples to avoid conflating GBM with all MSM in our review of this literature. For example, Benotsch and colleagues (1999) found a significant relationship between sexual compulsivity and unprotected anal intercourse (UAI) among seropositive MSM. Similarly, Coleman and colleagues (2010) explored the relationship between compulsive sexual behavior and UAI with partners met online and offline in a sample of MSM. Results indicated that those who presented with high scores of compulsive sexual behavior were more likely to participate in UAI. However, as noted by both sets of authors (Benotsch et al., 1999; Coleman et al., 2010), the nature of UAI as a sexual risk behavior was not assessed in either study, indicating the possibility that UAI may have occurred with seroconcordant partners, which for many GBM could serve as a risk-reduction strategy. To further explore these findings, Grov and colleagues (2010) evaluated the association between sexual compulsivity and sexual risk behavior in a sample of MSM in New York City, and found a significant relationship between compulsive sexual behavior and unprotected sex with serodiscordant partners. Grov and colleagues (2010), however, acknowledged that other factors (e.g., age) may result in different relationships between excessive sexual behavior and risk behavior among GBM. We contribute to this literature by examining whether the relationship between hypersexual symptoms and URAI persists after accounting for partners’ HIV status and sociodemographic characteristics.
Developmental and cultural contexts may influence how hypersexual behavior manifests and how it is measured. Past research suggests that excessive sexual behavior is twice as prevalent in men as in women, and tends to peak in late adolescence and early adulthood (Kafka, 2010; Langstrom & Hanson, 2006). In the context of YGBM, for example, an increase in the number of sex partners and occasions may parallel the developmental exploration of same-sex desires and/or development of a minority sexual identity, and/or may be attributable to prior life events (e.g., child abuse), psychological distress, and substance use (Rosario et al., 1996; Rosario, Scrimshaw, & Hunter, 2006). For example, in a 1996 Swedish national survey of 2450 18- to 60-year-old men, Langstrom and Hanson (2006), found that those who scored high on a composite measure of hypersexuality (e.g., impersonal sex acts such as masturbation, as well as number of sex partners per active year, diversity of sexual experiences, and sexual satisfaction) were more likely to be younger, to have had their sexual debut at a younger age, and to have engaged in same-sex behavior. Although these sexual explorations may overlap with some of the diagnostic criteria for hypersexual behavior (e.g., frequent sexual thoughts and urges), we argue for the possibility that the increased sexual activity in YGBM may not necessarily imply a clinical dysregulation in sexual behavior. Instead, it may be a developmental reflection of their growing exploration of and/or comfort with their sexuality.
Researchers have also suggested that excessive sexual behavior may be used as a way to cope with stressful developmental and interpersonal life events, an assertion that could reflect an adaptive quality and a coping mechanism to avoid negative affect (Reid, Carpenter, & Lloyd, 2009). For example, Reid and colleagues (2009) found elevated levels of depression symptomatology in a sample of men seeking treatment for hypersexuality, suggesting that these patients “use the intoxicating features of sex to tranquilize themselves from the unpleasant aspects of a depressed mood state” (p.57). Furthermore, under the current clinical definition of hypersexual behavior, there is little acknowledgement that excessive sexual behavior can be an adaptive and developmentally and culturally normative way to deal with life stressors. Further, Reid (2007) asserts that the spectrum of “normal” sexual behavior is extremely broad and often subjective; thus, it is possible that some variants of hypersexual behavior may not be considered pathological in some populations.
In the context of YGBM, increases in sexual activity may reflect youths’ comfort with their sexual identity, and may serve to offset the unique set of stressors (e.g., stigma, discrimination) that they may experience as sexual minorities (Harper, 2007). Consequently, it is plausible that YGBM may express some hypersexuality symptoms (e.g., sexual thoughts and urges) and engage in sexual behavior, without necessarily placing themselves at risk for HIV/AIDS infection. To advance this body of knowledge and clarify the relationships observed in existing literature, it remains critical that we examine how hypersexuality manifests in YGBM’s lives. As a contribution to the literature, we sought to examine the psychometric characteristics of the Hypersexual Behavior Inventory (HBI; Reid, Garos, & Carpenter, 2011) in a sample of YGBM and to test whether the HBI was associated with their sexual risk behaviors.
Hypersexual Behavior Inventory
The HBI was created to measure hypersexual behavior and facilitate in the classification of hypersexual patients (Reid & Carpenter, 2009; Reid et al., 2011). In clinical samples, the HBI (Reid et al., 2011) has been characterized as a multi-faceted inventory with three subscales, including the following: a) the Control subscale, which measures the extent to which an individual perceives an inability to regulate his or her sexual behavior; b) the Coping subscale, which reflects tendencies to use sex as a way to deal with negative affect or stressful life events; and c) the Consequences subscale, as an indicator of the extent to which individuals continue to engage in sexual behavior despite perceived negative consequences of such behavior. Recently Reid and colleagues (2011) assessed the psychometric properties of the HBI with two studies using independent samples of treatment-seeking hypersexual men between the ages of 18 and 68. In the first study, item reduction and exploratory factor analyses provided support for the three-factor structure of the HBI and found high internal reliability for the overall HBI scale and its individual factors. In the second study, confirmatory factor analysis again revealed high internal reliability for the full scale and its subscales. Based on these results, Reid and colleagues (2011) confirmed that the psychometric properties of the HBI significantly reflect the constructs of the proposed Diagnostic and Statistical Manual (American Psychiatric Association [DSM-IV-TR], 2000) criteria for Hypersexual Disorder. Subsequently, a cutoff score of 53 or greater for the HBI was established based on samples of treatment-seeking hypersexual men and controls (i.e., non-clinical samples) (Reid, 2010; Reid et al., 2009).
Historically, researchers have used clinical tools in large sample-based survey research in order to understand correlates of sexual risk behavior and help inform HIV/AIDS intervention strategies. For example, using the Sexual Compulsivity Scale (Kalichman et al., 1994), researchers have sought to examine the relationship between sexual compulsivity and sexual behaviors in large community-based samples (Kelly, Bimbi, Nanin, Izienicki, & Parsons, 2009; Grov, Parsons, & Bimbi, 2010) in order to inform HIV/AIDS prevention strategies. While the intended purpose of the HBI is to aid in the diagnosis of hypersexual symptoms, the presence of high scores across the HBI domains may also serve to document whether GBM’s use of sex is linked to their sexual risk behaviors. At present, it remains unclear whether the HBI may help inform HIV/AIDS prevention strategies by indicating which domains are associated with YGBM’s sexual risk behavior and may be suitable targets for behavior change interventions. For example, positive associations between the HBI domains and sexual risk behaviors may indicate how dysregulation places young men at risk by increasing their exposure to multiple partners and opportunities to have unprotected sex (e.g., Control), and/or how it affects their lives (e.g., Consequences). On the other hand, an increase in sexual behavior as a way to cope with life stressors may not necessarily imply clinical hypersexuality or even problematic behavior. Consequently, an increase in sexual thoughts, feelings, and behaviors may also reflect YGBMs’ use of sex as a coping strategy (e.g., Coping), and may not necessarily lead to an increase in sexual risk behavior.
Study Goals and Objectives
This study had two overarching goals. First, we explored the factorial structure of the HBI with a sample of YGBM. Second, because URAI is the strongest predictor of HIV risk, we assessed the association between continuous scores on the three HBI domains and YGBM’s self-reported number of URAI partners and occasions in the past two months, respectively. Additionally, we sought to determine the prevalence of scores on the HBI that reach the cutoff score for clinical hypersexuality in this sample of YGBM. Based on these findings we discuss the implications of the HBI for assessment of hypersexual behavior among YGBM and propose HIV/AIDS intervention recommendations for this population.
METHODS
Sample
Data for this paper were collected as part of a cross-sectional observational study examining young men’s dating experiences online (Bauermeister, Leslie-Santana, Johns, Pingel, & Eisenberg, 2011). To be eligible for participation, men had to be between the ages of 18 and 24, single at the time of the study, and report having been sexually active with a male partner met on a dating website in the past six months. Participants were recruited through advertisements on two popular non-sex-specific social networking sites, referrals, and flyers posted at local venues (e.g., coffee shops, bars, bookshops) commonly frequented by sexual minority youth. Recruitment materials asked men to participate in a research study examining the use of dating websites to meet other men. We did not define “dating websites” to ensure inclusivity of sites that are marketed for romance (e.g., Match.com, Chemistry.com) or for broader social purposes (e.g., Gay.com, Manhunt.com). Social network advertisements were viewable only to men who fit our age range and who lived in the United States. Promotional materials displayed a synopsis of eligibility criteria, a mention of a $15 iTunes gift card incentive, and a link to the survey’s website.
We recorded 548 entries between December 2009 and March 2010, removing duplicates and falsified entries (N=49; 8.9% of all entries) by examining participants’ email addresses, IP addresses, and operating system and browser information (Bauermeister et al., 2012). We had a final tally of 499 entries in the survey, of which 52 (10%) were eligible and consented but did not continue with the survey (i.e., survey completion rate of 89.6%). Given the few observations across sexual and gender categories, we exclude from this report those participants who self-identified as straight or other (N=4; 0.4%), transgender (N=6; 1.6%), or had missing data on their sexual identity (N=6; 1.6%). For the purposes of the current study, we also excluded 44 participants who did not report being sexually active in the past two months and 21 participants who had missing data on our variables of interest.
Procedures
The web-survey was developed using current web-survey recommendations (Couper, 2008) and pilot tested prior to data collection with a sample of YGBM who were not included in the final sample. Study data were protected with a 128-bit SSL encryption and kept within a University of Michigan firewalled server. We acquired a Certificate of Confidentiality to protect study data. A Certificate of Confidentiality is issued by the National Institutes of Health and is designed to protect the privacy of research participants by protecting investigators and institutions from having to release information that could be used to identify participants (National Institutes of Health, 2013). A Certificate of Confidentiality was important for the current study because we asked participants to report sensitive information including sexual behaviors and HIV/AIDS status.
Upon entering the study site, participants were asked to enter a valid and private email address, which served as their username. This allowed participants to save their answers and, if unable to complete the questionnaire in one sitting, continue the questionnaire at a later time. Participants were then asked to answer four questions (i.e., age, relationship status, use of the Internet, sexual activity with partners met online) to determine their eligibility. If eligible, participants were presented with a detailed consent form that explained the purpose of the study (i.e., exploring how YGBM use the Internet for dating) and their rights as participants. YGBM were asked to acknowledge that they read and understood each section of the consent form, respectively (i.e., participation involvement, protection of privacy, uses of data, potential benefit, compensation, terms of the Certificate of Confidentiality, changing their mind about participation, and who to contact if they had questions). Consented participants then answered a confidential 30–45 minute questionnaire that covered assessments regarding their sociodemographic characteristics, HIV status, Internet use, relationship ideals, sexual and substance use behaviors, and general mood over the last few months. For those questionnaires that were incomplete, participants were sent two reminder emails that encouraged them to complete the questionnaire; one email was sent a week after they had started the questionnaire and another was sent a week before the questionnaire was scheduled to close. The University of Michigan Institutional Review Board approved all study procedures.
Measures
Demographic characteristics
Respondents were asked to report their age (in years). Respondents were asked to report if they considered themselves of Latino or Hispanic ethnicity, followed by several racial categories: African American or Black, Asian or Pacific Islander (API), White or European American, Native American, and Other. We combined the Native American and Other race categories, given the limited number of observations. We then created dummy variables for each race/ethnicity group. White participants served as the referent group.
Sexual behavior
Respondents were asked to report their sexual behavior with men and women during the previous two months using the Sexual Practices Assessment Schedule (Carballo-Diéguez & Dolezal, 1995). For this measure, sexual behavior was defined as, “exclusively anal, vaginal, or oral sex.” Questions were posed both in formal language and vernacular (in italics) to increase comprehension. For this report, we include questions regarding receptive anal intercourse (RAI) in the prior two months. If participants reported at least one occasion of RAI, they were asked to report the number of unprotected RAI (URAI) occasions in the past two months, as well as the number of URAI partners with whom they had sex.
Partner serodiscordance
Participants were asked whether they had been tested for HIV, if they had received their test result, and whether they were HIV infected (no actual HIV test was performed). Participants who reported having URAI with one or more partners were asked, “Of those men, how many had actually told you they were HIV-negative and you had no reasons to doubt it?” and “Of those men, how many do you know to be HIV-positive?” The difference in the wording between the two questions was based on our interest in knowing if the participant had been expressly told by the partner that he was HIV-negative (as opposed to assuming seronegativity given that the partner “looked healthy”), and our acknowledgement that someone may find out a partner’s HIV-positive status without actually discussing it (e.g., finding HIV prescription drugs in his medicine cabinet). Those partners who were included in neither the HIV-negative nor the HIV-positive counts were considered of unknown HIV status. We created a dummy variable to measure the risk of having one or more potentially serodiscordant URAI partner(s) in the previous two months (0 = seroconcordant, 1 = one or more serodiscordant partners). Among HIV-negative participants, having a serodiscordant partner was operationalized as having one or more partners who were HIV-positive or of unknown HIV status. Among HIV-positive participants, a serodiscordant partner was operationalized as having one or more partners who were HIV-negative or of unknown HIV status. Among participants with HIV status unknown, having a serodiscordant partner was operationalized as having one or more partners who were HIV-positive or of unknown HIV status.
Hypersexual Behavior Inventory (HBI)
We used the Hypersexual Behavior Inventory (Reid et al., 2011) to 1) assess the psychometric properties of the Inventory with this sample of YGBM, and 2) determine the relationship between the factors of the HBI (Control, Coping, and Consequences) and URAI. Respondents were presented the HBI items in a random order to avoid order effects and were asked to report their level of agreement with nineteen items (1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Often, 5 = Very Often) related to sexual attitudes and behaviors. For this measure, sex was defined as, “any activity or behavior that stimulates or arouses a person with the intent to produce an orgasm or sexual pleasure.” Participants were asked questions related to the three factors of the HBI: Control (e.g., “My sexual behavior controls my life”), Coping (e.g., “Doing something sexual helps me cope with stress”), and Consequences (e.g., “I sacrifice things I really want in life in order to be sexual”).
Decisional balance to use condoms
We used the Decisional Balance subscale for Pleasure and Emotional Connection (Bauermeister, Carballo-Diéguez, Ventuneac, & Dolezal, 2009) to examine participants’ decisional balance to use or forego condoms with partners. Participants were asked to answer seven items twice. Each statement first referred to sex without condoms, followed by an identical statement asking about sex with condoms. Items included “Sex [with/without] condoms is very intimate to me” and “Sex [with/without] condoms makes me feel close to my partner.” Participants rated each statement using a five-point scale ranging from 1 = Strongly Disagree to 5 = Strongly Agree. Respondents’ score was computed by summing the net difference between unprotected sex and condom use scores across the statements. Greater positive scores reflect greater benefits/gains associated with unprotected sex, whereas negative scores reflect greater benefits/gains associated with condom use (Cronbach’s α = .94).
Pleasure interference
Participants were asked a single item (“How much do condoms interfere with your sexual satisfaction when you are penetrated anally?”) rated on a ten-point scale ranging from 1=Not at all to 10 = A lot.
Data Analytic Strategy
We first examined the distribution of the variables under study, followed by a confirmatory factor analysis with the HBI items. We used EQS (Bentler, 1985) for the confirmatory factor analysis (CFA). Contrary to factor analysis or linear regression, Structural Equation Modeling (SEM) permits the simultaneous testing of the psychometric adequacy of the latent factors and the correlations between the HBI factors (i.e., the association between Control, Coping, and Consequences) while adjusting for the reliability of the observed measures (Bedeian, Day, & Kelloway, 1997). We estimated our models using the maximum likelihood (ML) convergence in order to minimize inadequate covariance estimates (Reise, Waller, & Comrey, 2000).
For parsimony and conceptual clarity, we then removed items not loading into factors adequately (factor loading ≤ .50) or contributing to more than one latent factor (Nunnally & Bernstein, 1994). We used the provided overall goodness-of-fit measures to inform our model modifications. Following the guidelines proposed by Raykov, Tomer, and Nesselroade (1991) for adequate reporting of SEM, we considered three goodness-of-fit indices for our nested models: Bentler-Bonnet’s Normed Fit Index (NFI), Bentler-Bonnet’s Non-Normed Fit Index (NNFI) (Bentler & Bonnet, 1980), and the Comparative Fit Index (CFI) (Bentler, 1990). We also included the ratio between each model’s χ2 statistic and its degrees of freedom (DF), and the root mean-square error of approximation (RMSEA) as indices of misfit (Boomsma, 2000). Criteria for successful measurement models include having values of .95 or higher among fit indices, a 3:1 χ2 to DF ratio, and values of .06 or lower for RMSEA (Hu & Bentler, 1999). Finally, Cronbach’s alpha reliability coefficients were computed for each latent factor (Nunnally & Bernstein, 1994).
We did not perform an expectation-maximization (EM) imputation for missing data in our analyses, as we were unable to assure that data were missing at random (Raghunathan, 2004). Even after accounting for missing data due to listwise deletions, however, we had ample statistical power for the CFA (MacCallum, Browne, & Sugawara, 1996). We used the Wald Test (for removing parameters) and LaGrange Multiplier Test (for adding parameters) to assess whether items contributed to more than one factor (i.e., cross-loading items). Nevertheless, to identify whether listwise deletion could have introduced bias, we compared participants with missing data to those retained in the analyses across our variables of interest. We then examined the bivariate relationships between the variables of interest and conducted multivariate analyses using generalized linear models with a negative binomial distribution (Land, McCall, & Nagin, 1996; Lawless, 1987; McCullagh & Nelder, 1989) to account for overdispersion in the count data of sexual behavior outcomes (Cohen, Cohen, West, & Aiken, 2003; Gardner, Mulvey, & Shaw, 1995).
We examined whether regression models would be better estimated using a Total HBI score, as compared to models separating the three HBI factors. Careful inspection and comparison of model fit indicators (e.g., log-likelihood estimates) indicated that the models using the three factors were statistically better for both URAI partners and URAI occasions, respectively. We adjusted for age, race/ethnicity, decisional balance to forego condoms, pleasure interference, and partner serodiscordance in our models. We included these covariates in our analyses to avoid potential confounds when estimating the relationship between the HBI and URAI partners and URAI occasions, respectively. To avoid artificially increasing the Type-I error rate, we examined the omnibus test for each model and the Wald χ2 statistic of each predictor (Fleiss, Levin, & Paik, 2003).
RESULTS
Participants
Our analytic sample for this report consisted of 366 sexually-active young men (M = 21.46 years old, SD = 1.95) who self-identified as gay (89.1%) or bisexual (10.9%). Close to three quarters of the sample self-identified as White or European American (73%); the remainder of the sample identified as Hispanic or Latino (10.1%), Asian or Pacific Islander (7.9%), Black or African American (5.5%), or Native American or Other (3.6%). Participants who completed our survey lived in 44 of the 50 US states and territories, including Puerto Rico, and had comparable demographic characteristics across the four US Census regions (19.5% from the Northeast, 24.8% from the Midwest, 28.1% from the South, and 26.0% from the West; 7 participants did not provide information on their state of residence). Educational attainment varied across our sample: less than a high school education (2.2%), completed high school (10.1%), technical or associate degree (3.8%), some college (46.6%), completed college (20.8%), currently pursuing a graduate degree (12.1%), and completed a graduate education (4.4%).
The majority of the sample (78%) were below the HBI clinical cutoff point (HBI < 53 points). YGBM who scored at or above the HBI clinical cutoff point were more likely to report a greater number of total partners in the prior two months (mean in log number of partners = .68, SD = .31) than those below the cutoff point (mean in log number of partners = .56, SD = .26; t366 = 3.19, p<.01). Further, those who scored at or above the cutoff point indicated a greater number of URAI partners (mean in log number of URAI partners = .24, SD =.32) than those who scored below the cutoff point (M = .14, SD =.24, t366 = 2.57, p <0.05). Likewise, those who scored at or above the cutoff point indicated a greater number of UIAI partners (mean in log UIAI partners = .23, SD =.34) than those who scored below the cutoff point (mean in log UIAI partners =.13, SD =.21; t366 = 2.58, p < 0.05). YGBM below, at, and above the HBI clinical cutoff did not differ in age, race/ethnicity, decisional balance to use condoms, condom interference with pleasure, or partner serostatus.
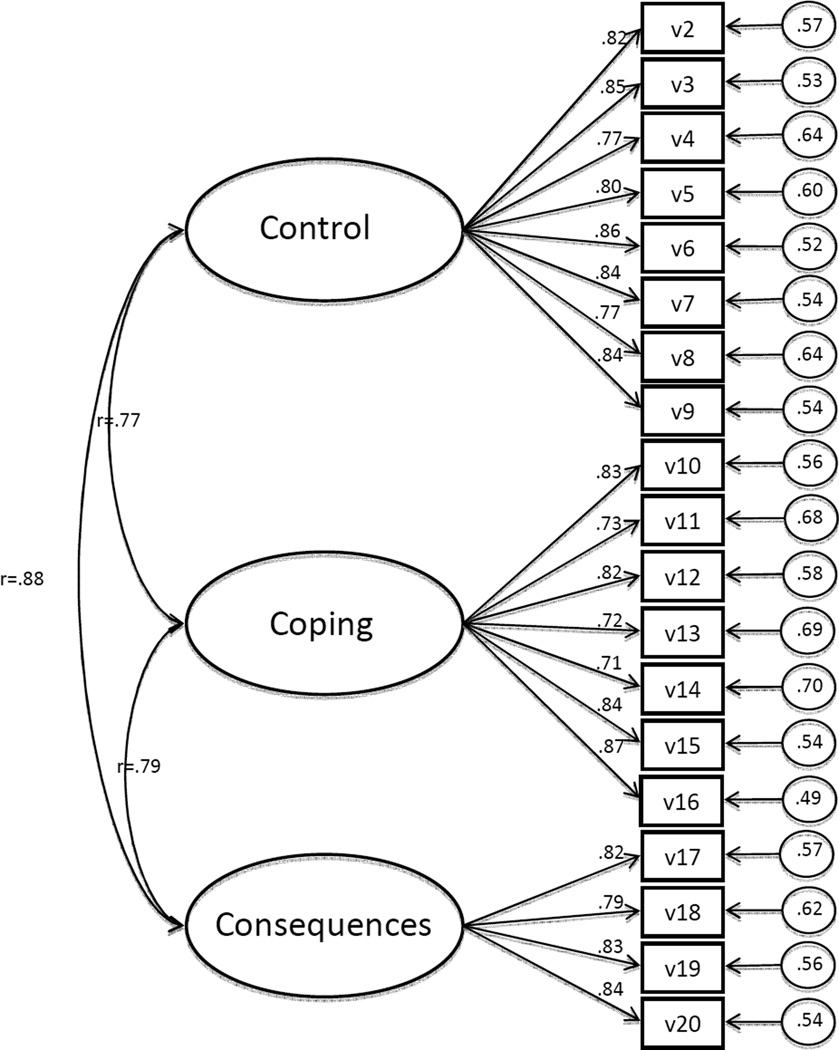
Confirmatory Factor Analysis
We included the mean and standard deviations for each HBI variable in Table 1. The original three-factor solution (see Figure 1) explained 77% of the total variance and fit the data moderately well: χ2 (df = 149) = 576.14, NFI = 0.91, NNFI = 0.92, CFI = 0.93, RMSEA = 0.086. In order to improve the model fit, we examined the Wald and LaGrange Multiplier Tests. Performing these tests did not indicate the removal of any parameters, but rather suggested that several items contributed to more than one factor. Among the Control items, we found v4 (“My attempts to change my sexual behavior fail”), v8 (“My sexual cravings and desires feel stronger than my self-discipline”), and v9 (“Sexually, I behave in ways I think are wrong”) also contributed to the Consequences subscale. Among the Coping items, we found that v16 (“I use sex as a way to try and help myself deal with my problems”) also loaded onto the Consequences scale. Finally, among the Consequences items, we found v17 (“I sacrifice things I really want in life in order to be sexual”) and v19 (“My sexual behavior controls my life”) loaded onto the Control subscale as well. Allowing these variables to contribute to more than one latent factor resulted in improvements in the overall model fit: χ2 (df = 142) = 386.11, NFI = 0.94, NNFI = 0.96, CFI = 0.96, RMSEA = 0.066.
Table 1.
Mean and standard deviation of Hypersexual Behavior Inventory items
| Mean(SD) | |
|---|---|
| Control | |
| Even though I promised myself I would not repeat a sexual behavior, I find myself returning to it (v2) |
2.15(1.20) |
| I engage in sexual activities that I know I will later regret (v3) | 2.13(1.07) |
| My attempts to change my sexual behavior fail (v4) | 2.18(1.17) |
| I do things sexually that are against my values and beliefs (v5) | 1.92(1.11) |
| Even though my sexual behavior is irresponsible or reckless I find it difficult to stop (v6) | 2.04(1.14) |
| I feel like my sexual behavior is taking me in a direction I don't want to go (v7) | 2.06(1.14) |
| My sexual cravings and desires feel stronger than my self-discipline (v8) | 2.29(1.21) |
| Sexually, I behave in ways I think are wrong (v9) | 1.84(1.15) |
| Coping | |
| I use sex to forget about the worries of daily life (v10) | 2.21(1.15) |
| Doing something sexual helps me feel less lonely (v11) | 2.49(1.15) |
| I turn to sexual activities when I experience unpleasant feelings (v12) | 2.47(1.19) |
| When I feel restless, I turn to sex in order to soothe myself (v13) | 2.68(1.19) |
| Doing something sexual helps me cope with stress (v14) | 2.99(1.15) |
| Sex provides a way for me to deal with emotional pain I feel (v15) | 1.99(1.11) |
| I use sex as a way to try and help myself deal with my problems (v16) | 2.00(1.10) |
| Consequences | |
| I sacrifice things I really want in life in order to be sexual (v17) | 1.91(1.04) |
| My sexual thoughts and fantasies distract me from accomplishing important tasks (v18) | 2.30(1.11) |
| My sexual behavior controls my life (v19) | 1.87(1.03) |
| My sexual activities interfere with aspects of my life such as work or school (v20) | 1.89(1.03) |
Notes. Participants answered items on a 5-point scale: 1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Often, 5 = Very Often.
Figure 1.
Hypersexual Behavior Inventory
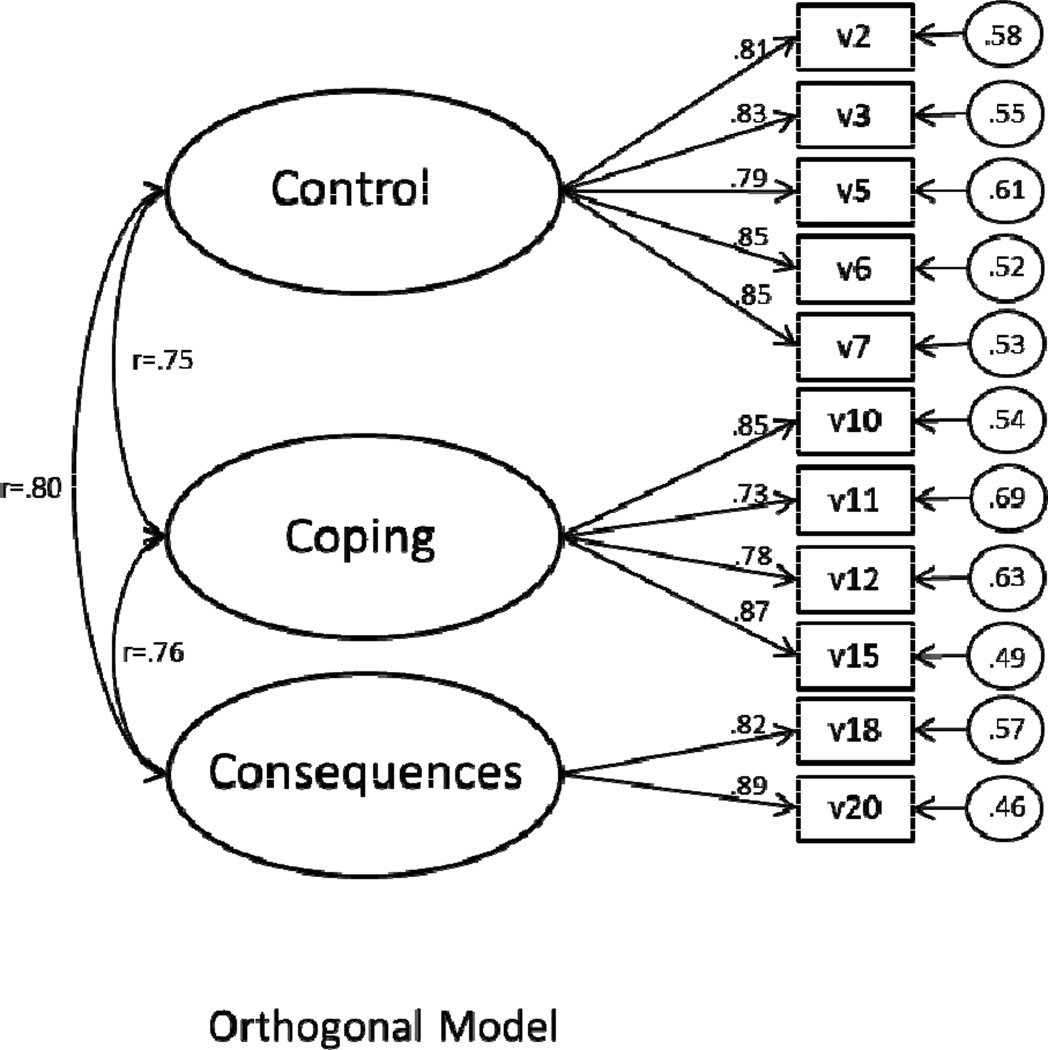
Given the number of cross-loading items in our model, however, we were concerned that our ability to measure each of the three factors separately would be inadequate. Therefore, we reran our model after removing the cross-loaded items (see the orthogonal model in Figure 2) and found significant improvements in our CFA model fit statistics: χ2 (df = 41) = 81.13, NFI = 0.97, NNFI = 0.98, CFI = 0.99, RMSEA = 0.049. We found strong reliability for the three HBI subscales: Control (α=.92; 5 items), Coping (α=.88; 4 items), and Consequences (α=.83; 2 items).
Figure 2.
Revised Hypersexual Behavior Inventory (no cross-loadings)
Sample Characteristics and Missing Data Analyses
Participants reported an average of four male partners in the past two months (M = 4.07, SD = 5.88). Sixty-seven percent (N = 246) of the sample reported engaging in receptive anal intercourse in the past two months. Among those who had receptive anal intercourse, over half of the sample reported engaging in URAI with one or more partners (M = 1.38, SD = 3.24). Sixty-three percent (N = 232) of the sample also reported engaging in insertive anal intercourse, with over half of the sample reporting UIAI with one or more partners (M = 1.33, SD = 3.00). The majority of participants self-reported being HIV-negative (N = 277; 74.6%). Eleven participants disclosed being HIV-positive (3.0%), and over a fifth of the sample did not know their HIV status (N = 82; 22.4%).
When we compared participants with missing data (n=81) to those retained in the current analyses, we found that participants with missing data reported fewer sexual partners in the prior two months (t = 6.75, p < .001), fewer URAI occasions (t = 2.44, p < .05), and fewer URAI partners (t = 2.48, p < .05) than those kept in the subsequent analyses. We found no differences across age, race/ethnicity, serodiscordant status, hypersexual behavior scores, decisional balance to forego condoms, or pleasure interference.
Negative Binomial Regression Analysis
After examining the bivariate Pearson correlations across study variables (see Table 2), we tested the association between the HBI factors and the number of partners with whom participants’ had engaged in URAI (X2(11) = 138.63; p < .001). In our multivariate models (see Table 3), Control was the only HBI factor associated with URAI partners (AOR=1.07, 95% Confidence Interval [CI] = 1.02, 1.13: p < .01). URAI partners were also associated with decisional balance to forego condom use (AOR=1.56, 95% CI = 1.30, 1.87; p < .001), and condom interference with pleasure (AOR=1.15, 95% CI = 1.07, 1.23; p < .001). The likelihood of having URAI partners was greater among participants reporting at least one serodiscordant partner (AOR=2.02, 95% CI = 1.09, 3.77; p < .05).
Table 2.
Pearson’s bivariate correlations across variables of interest including revised HBI subscales.
| Age | Control | Coping | Consequences | Decisional Balance |
Pleasure Interference |
Serodiscordance | |
|---|---|---|---|---|---|---|---|
| Control | −.05 | ||||||
| Coping | −.01 | .65** | |||||
| Consequences | .04 | .69** | .63** | ||||
| Decisional Balance | .07 | .18** | .14** | .16** | |||
| Pleasure Interference | .14** | .14** | .10 | .07 | .47** | ||
| Serodiscordance | −.02 | .10* | .05 | .09 | .14** | .08 | |
| Hispanic | −.05 | .03 | .10 | −.02 | .04 | −.06 | −.05 |
| Black | −.05 | −.02 | −.03 | −.05 | −.13* | −.07 | −.03 |
| API | .10* | .06 | .01 | −.05 | .01 | .01 | −.03 |
| Nat. Am. / Other | .06 | .03 | .08 | −.01 | .04 | .13* | −.04 |
Correlation is significant at the 0.05 level (2-tailed)
Correlation is significant at the 0.01 level (2-tailed)
Table 3.
Multivariate Negative Binomial regression examining the relationship between URAI partners and URAI occasions and revised HBI subscales, respectively.
| URAI Partners | URAI Occasions | |||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | Wald χ2 | AOR | 95% CI | Wald χ2 | |
| Age | 1.02 | (.93, 1.12) | .21 | .94 | (.87, 1.01) | 2.67 |
| Control | 1.06* | (1.00, 1.12) | 3.72 | 1.07** | (1.02, 1.13) | 6.55 |
| Coping | .98 | (.91, 1.04) | .59 | .93** | (.88, .99) | 5.19 |
| Consequences | 1.05 | (.91, 1.21) | .43 | .98 | (.86, 1.12) | .09 |
| Decisional Balance | 1.56*** | (1.30, 1.87) | 22.33 | 2.52*** | (2.09, 3.05) | 91.14 |
| Pleasure Interference | 1.15*** | (1.07, 1.23) | 16.35 | 1.07* | (1.01, 1.14) | 4.56 |
| Serodiscordant Partner | 2.02* | (1.09, 3.77) | 4.92 | 1.22 | (.67, 2.22) | .41 |
| Hispanic a | 1.76* | (1.09, 2.86) | 5.33 | .98 | (.62, 1.55) | .01 |
| B | .66 | (.29, 1.53) | .92 | ..63 | (.30, 1.34) | 1.45 |
| Asian Pacific Islander | .65 | (.32, 1.30) | 1.51 | .61 | (.33, 1.14) | 2.41 |
| Native American or Other Race | 1.55 | (.67, 3.62) | 1.04 | 1.39 | (.63, 3.07) | .66 |
p < .05
p < .01
p < .001.
Whites serve as the comparison group.
We then examined the associations between HBI factors and URAI occasions (X2(11) _= 249.46; p < .001). Participants scoring higher on the Control subscale (AOR=1.07, 95% CI = 1.02, 1.13; p < .01) were more likely to report a greater number of URAI occasions. Participants scoring higher on the Coping subscale, on the other hand, were less likely to report multiple URAI occasions (AOR=.93, 95% CI =.88, .99; p < .01). We found no association between URAI occasions and Consequences. URAI occasions was related to decisional balance to forego condoms (AOR=2.52, 95% CI = 2.09, 3.05; p < .001) and pleasure interference (AOR=1.07, 95% CI = 1.01, 1.14; p < .05), respectively.
DISCUSSION
The goal of this study was to examine the factor structure of the HBI in a sample of YGBM and assess its relationship to HIV/AIDS risk behaviors. Our confirmatory factor analysis supports the three-factor structure of the original HBI (Reid et al., 2011), suggesting its use in populations of YGBM. In the original scale development study, Reid and colleagues (2011) reduced items based on exploratory factor analysis, yet chose to include these cross-loaded items. While much of the original variance was maintained in this model, it is possible that this pragmatic approach may have ignored some of the theoretical and content overlap of scale items. Our findings suggest, however, that while the factor structure of the original HBI offers a reasonable fit, several items are cross-loaded (i.e., measuring more than one domain) and limit the conceptual clarity of each factor as an independent domain. These items were worded in such a way that, although they align with the theorized Control and Coping domains they also loaded onto the Consequences domain. A potential interpretation of the presence of these cross-loaded items may be that YGBM who report higher scores on Control or Coping items are also more likely to report that they have experienced consequences as a result of their sexual behaviors. For example, YGBM who ascribe negative consequences to their sexual practices may also be more likely to have tried to change their sexual behaviors (v4), feel that their sexual cravings are stronger than their self-discipline (v8), and/or feel that they sexually behave in ways that are wrong (v9). Given the cross-sectional nature of our study, however, we are unable to examine these temporal hypotheses. Future longitudinal research examining the temporal associations between Coping, Control and Consequences may be warranted.
In our revised CFA, Control items measured YGBM’s inability to self-regulate their sexual behavior and the anticipated regret resulting from it. Consistent with past research (Benotsch et al., 1999; Coleman et al., 2010), a decreased ability to control sexual urges and desires was associated with a greater number of URAI partners and occasions, respectively. These findings suggest that YGBM may benefit from strategies that help them regulate their sexual behavior in order to reduce their risk of HIV/AIDS infection. However, it is important to remain aware that an increase in sexual activity (e.g., multiple partnerships, increased occasions) can be a developmentally normative behavior for YGBM in emerging adulthood (Harper, 2007). Consequently, intervention approaches should focus on assisting YGBM who wish to explore their sexuality to do so openly and safely, and include opportunities for YGBM to promote individual self-regulation and control (e.g., condom negotiation) as part of their sexual decision-making. Further, health professionals should think critically about labeling increased sexual activity as pathology and prioritize reducing stigma that is directed toward YGBM who experience an increase in sexual activity as a means of exploring their sexual identity.
Our revised Coping construct measured YGBM’s use of sex as a strategy to alleviate stress, and suggested that this domain may be associated with HIV/AIDS risk reduction among YGBM. Specifically, YGBM who used sex as a coping mechanism reported fewer URAI occasions. Coping had no association with URAI partners. Taken together, these findings suggest that YGBM are able to minimize their risk (e.g., negotiate condoms), irrespective of their number of partners. Instead of pathologizing youth for using sex as a way to cope with stress, health professionals may want to consider the meaning that YGBM ascribe to unprotected sex as they explore their sexuality. Specifically, our findings suggest that YGBM’s HIV/AIDS risk increased if participants valued unprotected sex over sex with condoms (e.g., decisional balance) as an opportunity to create an emotional connection with a partner (Bauermeister et al., 2009). Together, these findings suggest that HIV/AIDS intervention approaches should focus on the meaning ascribed to a sexual encounter (e.g., decisional balance to make an emotional connection), alongside the reasons why YGBM have sex.
Our revised Consequences subscale removed two items cross-loading with control, leaving the construct with two items focused on how YGBM’s sexuality may interfere with other tasks in their lives (e.g., work, school). As a result, it is unsurprising that we found no association between Consequences and our sexual risk behavior outcomes. The limited variability within the subscale is particularly problematic as it not only limits our ability to understand how hypersexual behavior affects people’s lives but also hinders our ability to create an index of severity resulting from the accumulation of multiple consequences. In recognition of these theoretical challenges, researchers have begun to re-examine the subscale’s measurement and to re-conceptualize the domains that may be affected due to hypersexual behavior (Reid, Garos, & Fong, 2012). Future research should explore the Consequences domain qualitatively and revisit its quantitative assessment.
Our study possesses several strengths and limitations deserving mention. First, even though we estimated that close to 20% of the sample would meet clinical criteria based on HBI cutoff scores, we were unable to determine whether this subsample is currently receiving psychological services, therefore limiting our assumption that we are assessing the psychometric properties of the HBI on a non-clinical sample of YGBM. Second, because of the nature of this study as an online survey, we were unable to cross-validate our HBI scores with a face-to-face clinical interview and determine whether participants scoring high on the HBI scale are in fact presenting a hypersexual disorder. Future research on the HBI in YGBM populations should consider individual interviews in a clinical setting as a way to validate the proposed model. Third, we recruited from several sources (e.g., online and in community venues) yet did not record the specific source of recruitment for each participant. Consequently, we were unable to control for differences in recruitment strategy. Fourth, our sample was highly educated with the majority of the participants reporting some college education or more. Future research should aim to increase the generalizability of these findings to a more diversely educated sample of YGBM. Fifth, the observed relationships between the HBI constructs and sexual risk behavior may have been influenced by measurement factors (e.g., criterion contamination) and additional variables, which we were unable to account for in our final model. Future research should replicate our findings and extend this work by investigating the possible interplay of potential covariates (e.g., different sexual practices, drug/alcohol use, self-regulation, and the influence of executive control in this younger population). Additionally, our sample was comprised of YGBM between the ages of 18 and 24. Consequently, although our findings speak to the emerging adulthood period, we are unable to extrapolate our findings to older GBM and/or sexual minority youth who don’t identify as gay or bisexual. Nevertheless, this study underscores the importance of assessing the psychometric properties of the HBI and its relation to sexual risk behavior in a population- and age-specific manner. Future research should explore the appropriateness and utility of the HBI in other populations of interest (e.g., sexual minority women, older GBM). Finally, it should be noted that the adjusted odds ratios for the HBI subscales and sexual risk are modest, which may reflect the fact that over three-quarters of the sample reported HBI scores below the clinical cutoff. We recommend that future research explore the aforementioned relationships between HBI subscales and sexual risk on larger sample of YGBM who meet and/or exceed the clinical cutoff. These limitations notwithstanding, this study raises important questions regarding how we conceptualize hypersexuality and sexual risk behavior among YGBM, and underscores the influence of age and cultural norms in YGBM’s sexual behavior. Consistent with prior work, YGBM who show a heightened lack of control over their sexual behavior were more likely to participate in a greater amount of risky sexual behavior, emphasizing the importance of including skill-building activities that promote sexual self-regulation and decision making in HIV/AIDS interventions. On the other hand, our findings also suggest that hypersexual behavior may reflect the use of sex as an adaptive strategy in coping with life stressors. Consequently, while it is possible that risky sexual behavior (e.g., URAI) may lead to heightened HIV vulnerability, we must also acknowledge the social and psychological value that sex plays in YGBM’s lives. Taken together, our findings underscore the need to contextualize sexual behavior within a developmental framework, understanding its role as both a risk and promotive factor in YGBM’s lives, and to adapt our existing measures of hypersexual behavior accordingly.
Acknowledgments
This research was supported by a Career Development K01 award to Dr. Bauermeister, (K01-MH087242) from the National Institutes of Mental Health.
Contributor Information
Emily Yeagley, Email: eyeagley@umich.edu, Department of Health Behavior and Health Education, School of Public Health, University of Michigan.
Andrew Hickok, Email: ahickok@umich.edu, Department of Health Behavior and Health Education, School of Public Health, University of Michigan.
José A. Bauermeister, Email: jbauerme@umich.edu, Department of Health Behavior and Health Education, School of Public Health, University of Michigan.
References
- Allers CT, Benjack KJ, White J, Rousey JT. HIV vulnerability and the adult survivor of childhood sexual abuse. Child Abuse & Neglect. 1993;17(2):291–298. doi: 10.1016/0145-2134(93)90048-a. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental health disorders. 4th ed. Washington DC: Author; 1994. [Google Scholar]
- Barth RJ, Kinder BN. The mislabeling of sexual impulsivity. Journal of Sex & Marital Therapy. 1987;13:12–13. doi: 10.1080/00926238708403875. [DOI] [PubMed] [Google Scholar]
- Baum MD, Fishman JM. AIDS, sexual compulsivity, and gay men: A group treatment approach. In: Cadwell SA, Burnham Rr, Forstein M, editors. Therapists on the front line: Psychotherapy with gay men in the age of AIDS. Arlington, VA US: American Psychiatric Association; 1994. pp. 255–274. [Google Scholar]
- Bauermeister JA, Carballo-Diéguez A, Ventuneac A, Dolezal C. Assessing motivation to engage in intentional condomless anal intercourse in HIV-risk contexts (bareback sex) among men who have sex with men. AIDS Education & Prevention. 2009;21(2):156–168. doi: 10.1521/aeap.2009.21.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Leslie-Santana M, Johns MM, Pingel E, Eisenberg A. Mr. Right and Mr. Right Now: Romantic and casual partner-seeking online among young men who have sex with men. AIDS and Behavior. 2011;15(2):261–272. doi: 10.1007/s10461-010-9834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Pingel E, Zimmerman MA, Couper M, Carballo-Diéguez A, Strecher VJ. Data quality in web-based HIV/AIDS research: Handling Invalid and Suspicious Data. Field Methods. 2012;24(3):272–291. doi: 10.1177/1525822X12443097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedeian AG, Day DV, Kelloway E. Correcting for measurement error attenuation in structural equation models: some important reminders. Educational & Psychological Measurement. 1997;57:785–799. [Google Scholar]
- Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in hiv-seropositive men who have sex with men: Prevalence and predictors of high-risk behaviors. Addictive Behaviors. 1999;24(6):857–868. doi: 10.1016/s0306-4603(99)00056-8. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Theory and implementation of EQS, A structural equations program. Los Angeles: BMDP Statistical Software; 1985. [Google Scholar]
- Bentler PM, Bonnet DG. Significance tests and goodness-of-fit in the analysis of covariance structures,”. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Black DW. Compulsive sexual behavior: A review. Journal of Practical Psychiatry and Behavioral Health. 1998;4:219–229. [Google Scholar]
- Boomsma A. Reporting analyses of covariance structures. Structural Equation Modeling. 2000;7(3):461–483. [Google Scholar]
- Carballo-Diéguez A, Dolezal C. Association between history of childhood sexual abuse and adult HIV-risk sexual behavior in Puerto Rican men who have sex with men. Child Abuse & Neglect. 1995;19(5):595–605. doi: 10.1016/0145-2134(95)00018-4. [DOI] [PubMed] [Google Scholar]
- Carnes P. Out of the shadows: Understanding sexual addiction. Minneapolis: Hazeldon; 1983. [Google Scholar]
- Centers for Disease Control. HIV among gay and bisexual men. 2013 Retrieved from http://www.cdc.gov/hiv/topics/msm/
- Coleman E, Horvath K, Miner M, Ross M, Oakes M, Rosser B. Compulsive sexual behavior and risk for unsafe sex among internet using men who have sex with men. Archives of Sexual Behavior. 2010;39(5):1045–1053. doi: 10.1007/s10508-009-9507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ US: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- Cooper A, Delmonico DL, Burg R. Cybersex users, abusers, and compulsives: New findings and implications. Sexual Addiction & Compulsivity. 2000;7(1–2):5–29. [Google Scholar]
- Couper MP. Designing Effective Web Surveys. Cambridge, MA: Cambridge University Press; 2008. [Google Scholar]
- Dodge B, Reece M, Herbenick D, Fisher C, Satinsky S, Stupiansky N. Relations between sexually transmitted infection diagnosis and sexual compulsivity in a community-based sample of men who have sex with men. Sexually Transmitted Infections. 2007;84:324–327. doi: 10.1136/sti.2007.028696. [DOI] [PubMed] [Google Scholar]
- Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. Third ed. Hoboken, New Jersey: John Wiley & Sons, Inc; 2003. [Google Scholar]
- Gardner W, Mulvey E, Shaw E. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial. Psychological Bulletin. 1995;118(3):392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives Of Sexual Behavior. 2010;39(4):940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper GW. Sex isn't that simple: Culture and context in HIV prevention interventions for gay and bisexual male adolescents. American Psychologist. 2007;62(8):806–819. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kafka MP. Hypersexual disorder: A proposed diagnosis for DSM-V. Archives Of Sexual Behavior. 2010;39(2):377–400. doi: 10.1007/s10508-009-9574-7. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment. 1994;62:385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- Kelly BC, Bimbi DS, Nanin JE, Izienicki H, Parsons JT. Sexual Compulsivity and Sexual Behaviors Among Gay and Bisexual Men and Lesbian and Bisexual Women. Journal Of Sex Research. 2009;46(4):301–308. doi: 10.1080/00224490802666225. [DOI] [PubMed] [Google Scholar]
- Krueger RB, Kaplan MS. The paraphilic and hypersexual disorders: An overview. Journal of Psychiatric Practice. 2001;7:391–403. doi: 10.1097/00131746-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Land KC, McCall PL, &Nagin DS. A comparison of Poisson, negative binomial, and semiparametric mixed Poisson regression models. Sociological Methods and Research. 1996;24:387–442. [Google Scholar]
- Langstrom N, Hanson RK. High rates of sexual behavior in the general population: Correlates and predictors. Archives of Sexual Behavior. 2006;35:37–52. doi: 10.1007/s10508-006-8993-y. [DOI] [PubMed] [Google Scholar]
- Lawless JF. Negative binomial and mixed Poisson regression. The Canadian Journal of Statistics. 1987;3:209–225. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- McCullagh PP, Nelder JA. Generalized linear models. 2nd edition. London: Chapman and Hall; 1989. [Google Scholar]
- Mustanski B, Newcomb M, DuBois S, Garcia S, Grov C. HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and intervention. Journal of Sex Research. 2011;48(2–3):218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Health. Certificate of confidentiality kiosk. 2013 Retrieved from < http://grants.nih.gov/grants/policy/coc/>.
- Nunnally JC, Bernstein IH. Psychometric Theory. Third ed. New York: McGraw-Hill, Inc; 1994. [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Archives Of Sexual Behavior. 2008;37(5):817–826. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annual Review of Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- Raykov T, Tomer A, Nesselroade JR. Reporting structural equation modeling results in Psychology and Aging: Some proposed guidelines. Psychology and Aging. 1991;6(4):499–503. doi: 10.1037//0882-7974.6.4.499. [DOI] [PubMed] [Google Scholar]
- Reid RC. Assessing readiness to change among clients seeking help for hypersexual behavior. Sexual Addiction & Compulsivity. 2007;14(3):167–186. [Google Scholar]
- Reid RC, Carpenter BN. Exploring relationships of psychopathology in hypersexual patients using the MMPI-2. Journal Of Sex & Marital Therapy. 2009;35(4):294–310. doi: 10.1080/00926230902851298. [DOI] [PubMed] [Google Scholar]
- Reid RC, Carpenter BN, Lloyd TQ. Assessing psychological symptom patterns of patients seeking help for hypersexual behavior. Sexual And Relationship Therapy. 2009;24(1):47–63. [Google Scholar]
- Reid RC, Garos S, Carpenter B. Reliability, validity, and psychometric development of the Hypersexual Behavior Inventory in an outpatient sample of men. Sexual addiction and compulsivity. 2011;18(1):30–51. [Google Scholar]
- Reid RC, Garos S, Fong T. Psychometric development of the Hypersexual Behavior Consequences Scale. Journal of Behavioral Addictions. 2012;1(3):115–122. doi: 10.1556/JBA.1.2012.001. [DOI] [PubMed] [Google Scholar]
- Reise SP, Waller N, Comrey AL. Factor analysis and scale revision. Psychological Assessment. 2000;12:287–297. doi: 10.1037//1040-3590.12.3.287. [DOI] [PubMed] [Google Scholar]
- Rosario M, Meyer-Bahlburg H, Hunter J, Exner TM, Gwadz M, Keller AM. The psychosexual development of urban lesbian, gay, and bisexual youths. The Journal of Sex Research. 1996;33(2):113–126. [Google Scholar]
- Rosario M, Scrimshaw E, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education and Prevention. 2006;18(5):444–460. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]