Abstract
In patients with colorectal cancer (CRC), accurate preoperative evaluation is essential for a correct therapeutic plan. Colonoscopy and intravenous contrast-enhanced computed tomography (CT) are currently recommended in the preoperative work-up for CRC. Preoperative colonoscopy has some limitations such as misdiagnosis of synchronous cancers in cases of incomplete exploration of the colon and inaccurate tumor localization. Intravenous contrast-enhanced CT successfully documents distant metastases although it sometimes enables unsatisfactory locoregional staging. Computed tomography colonography (CTC) is obtained after gas insufflation of the colon and offers a comprehensive preoperative evaluation in patients with CRC, including a definition of the segmental location of the tumor, presence of synchronous lesions or lack thereof, and fairly accurate locoregional staging. CTC has some limitations, including a lack of biopsy capability, suboptimal sensitivity for synchronous small polyps, and unsatisfactory nodal staging. Bearing in mind these limitations, CTC could be employed as a “one-stop-shop” examination for preoperative assessment in patients with CRC.
Keywords: Colorectal cancer; Colonoscopy, Computed tomography colonography; Synchronous cancer; Cancer staging
Core tip: Computed tomography colonography (CTC) can be employed as a “one-stop-shop” examination for preoperative assessment in patients with colorectal cancer (CRC). CTC is well accepted and tolerated by patients and also accurate in the detection of significant colorectal lesions. In patients with CRC, CTC defines the segmental location of the tumor and the presence of synchronous lesions or lack thereof and provides fairly accurate locoregional staging.
INTRODUCTION
In Europe, colorectal cancer (CRC) is the second most frequent malignant neoplasia and the second most common cause of death from cancer[1]. Whereas in the United States, CRC accounts for the fourth highest incidence of cancer and the fourth leading cause of cancer-related deaths[2].
In European countries, the average relative five-year survival rate for patients with CRC is 54%[3]. However, patient prognosis and treatment largely depend on the disease stage at initial diagnosis. Accurate preoperative evaluation is essential for a correct therapeutic plan, including surgery (open or laparoscopic), radiotherapy or chemotherapy. In particular, a preoperative work-up is aimed to exclude the presence of synchronous cancers, to evaluate local invasion, and to detect nodal and distant metastases. Moreover, precise localization of the tumor is essential for surgical treatment planning, especially in the case of the laparoscopic approach.
A wide range of diagnostic tools is available to study patients with CRC, including optical colonoscopy, double contrast barium enema (DCBE), ultrasound (US), computed tomography (CT), computed tomography colonography (CTC), magnetic resonance (MR) and positron emission tomography (PET)[3,4]. CTC potentially represents a comprehensive examination for preoperative evaluation of patients with CRC. In particular, it is accurate in the detection of significant colorectal lesions[5-7]; enables evaluation of the entire colon, even in cases of obstructive lesions; and allows segmental localization of the tumor. At the same time, CTC permits staging of extra-colonic tumor spread, both locoregional and distant.
CRC may present with non-specific symptoms or signs (rectal bleeding, change in bowel habits, abdominal pain or anemia) or with acute bowel obstruction. Moreover, CRC may be discovered in asymptomatic subjects as the result of screening with fecal occult blood test, sigmoidoscopy, colonoscopy, or CTC. In all cases an ultimate diagnosis is generally made by colonoscopy and biopsy.
Herein, we shall review the technique, benefits and limitations of CTC as a preoperative examination in patients with already diagnosed CRC.
CTC TECHNIQUE
A state-of-the-art CTC examination requires adequate bowel preparation, optimal colonic distension and proper scanning technique[8]. Moreover, in patients with diagnosed CRC, CTC must be performed with an administration of intravenous-iodinated contrast media, as it allows extra-colonic organ evaluation, which is requested in search of distant metastases[8].
Bowel preparation for CTC in patients with known CRC is usually obtained with a three-day low fiber diet and the administration of a cathartic agent such as a polyetilenglycole solution the day before the CTC examination. In frail or elderly patients, a reduced cathartic preparation should be considered such as a three-day low fiber diet and the administration of 13.8 g of macrogol 3350 (Movicol; Norgine, Milan, Italy) diluted in a glass of water and given at the three main meals for three days before the examination[9]. Fecal tagging should be routinely used, as it improves colonic lesions detection without noticeably affecting image quality after administration of intravenous contrast media[8]. Fecal tagging is usually obtained with 50 mL of iodinated oral contrast agent (Gastrografin; Bayer Schering Pharma AG, Berlin, Germany) administered 2-3 h before the procedure.
Colonic distension should preferably be performed using an automatic carbon dioxide insufflator[10], although the manual insufflation of room air is acceptable. Before insufflation, if there are no contraindications, including hypersensitivity to the active principle, untreated narrow angle glaucoma and prostatic hypertrophy with urinary retention, we intravenously administer 20 mg of scopolamine butylbromide (Buscopan; Boehringer Ingelheim Italia, Milan, Italy) to improve colonic distension[11]. In patients with stenosing lesions, insufflation should be gradually performed and carefully monitored using CT scout views, as the risk of perforation, although extremely low for CTC, could be increased[12].
The recommended scanning technique for preoperative CTC differs from that adopted for screening CTC, including patient positioning, scan parameters concerning the delivered radiation dose and administration of intravenous contrast media (Table 1)[13]. In our institution, for the preoperative evaluation of CRC, a preliminary unenhanced acquisition is performed in a prone position. Then, a portal phase supine scan is performed 70 s after the administration of contrast media[8]. The use of a multi-phasic CT protocol after administering contrast media may be chosen by the radiologist in specific clinical settings (e.g., patients with non-characterized liver focal lesions). An arterial phase thoracic acquisition can also be performed as part of staging, when appropriate. All images are then transferred to a dedicated workstation, which allows visualization of two-dimensional axial and multi-planar reformatted (MPR) images, three-dimensional endoluminal surface-shaded images (SSD) and double-contrast-like reconstructions of the colon.
Table 1.
Computed tomography colonography scanning technique for a 64-slice scanner1
| Preoperative CTC | Screening CTC | |
| IV contrast media | Yes | No |
| Patient position | Prone (unenhanced), supine (portal phase) | Supine, prone |
| Collimation | 32 mm × 0.6 mm | 32 mm × 0.6 mm |
| Tube voltage | 120 kV | 120 kV |
| Tube current | 140 eff mAs (unenhanced), 200 eff mAs (enhanced) | 50 eff mAs |
| Tube rotation time | 0.5 s | 0.5 s |
| Pitch | 1.4 | 1.4 |
| Section width | 1 mm | 1 mm |
| Reconstruction increment | 1 mm | 1 mm |
1Scan parameters for Sensation 64 (Siemens, Erlangen, Germany). CTC: Computed tomography colonography.
DIAGNOSIS OF SYNCHRONOUS CANCERS
An important issue regarding patients with CRC is the occurrence of synchronous cancers (SC), which are reported in 2%-11% of the cases[14-16]. A search for SC is routinely performed during open surgery for CRC, but intra-operative palpation of the colon can miss up to 69% of SC[17]. Moreover, in case of the laparoscopic approach to CRC, the surgeon cannot explore the entire colon in a search for simultaneous lesions. Missed diagnosis of SC can lead to increased morbidity and progression of CRC to a more advanced stage[18]. In fact, preoperative identification of SC implied a more extended colonic resection in 11%-44% of cases[18]. Because patients undergoing preoperative conventional colonoscopy have fewer local recurrences, fewer distant metastases and a longer disease-free survival time[19], full preoperative colonic evaluation with colonoscopy should always be performed in patients with CRC.
In case of incomplete colonoscopy due to an insuperable stenosing cancer or other causes (e.g., inadequate bowel preparation, anatomic variants, fixed colon segments, patient’s intolerance to the procedure), endoscopic diagnosis of synchronous lesions may be precluded. A recent study showed that advanced neoplasia could be missed in up to 4.3% of patients during incomplete colonoscopy, suggesting that further colonic evaluation is mandatory in these cases[20]. To complete evaluation of the colon, radiological examinations can be performed, such as double-contrast barium enema (DCBE) and CTC.
A multi-centric randomized trial comparing diagnostic performance of DCBE and CTC in patients with suspected CRC clearly showed that diagnostic accuracy of DCBE for CRC is not satisfactory[21]. In particular, barium enema missed 12 of 85 cancers[21]. However, CTC showed a sensitivity for cancer and adenomas larger than 10 mm comparable to colonoscopy, namely 96.1%[5] and 84%-92.2%[6,7]. Moreover, CTC is well tolerated by patients[22], and its complications are exceedingly rare[12]. However, CTC has some limitations. It does not allow the biopsy or removal of discovered lesions, precluding histological diagnosis. Moreover, its sensitivity for intermediate polyps (6-9 mm) is lower than that of colonoscopy, namely 70%, and even worse, 48%, for diminutive lesions (< 5 mm)[23]. In fact, small polyps can be overlooked by preoperative CTC.
Several studies showed that CTC represents a valuable tool to evaluate the proximal colon after incomplete colonoscopy[24-28], and the American Gastroenterologists Association (AGA) recognized that CTC is indicated for adults with failed colonoscopy[29]. Several studies evaluated the role of CTC in patients with CRC and incomplete colonoscopy. In patients with CRC, a CTC with complete colonic distension was achieved in 83% to 100% of the cases[24,30-32]. In a series of 174 patients with CRC, McArthur et al[32] showed that all synchronous cancers and 83.3% of synchronous polyps greater or equal to 10 mm were identified by CTC. Other studies with smaller groups of patients reported that CTC depicted all synchronous cancers and had a sensitivity for polyps greater or equal to 10 mm of 100%[24,30,31].
One study showed that CTC is technically feasible and well tolerated also in patients with CRC presenting with acute or subacute bowel obstruction[33]. Finally, a study proved that CTC is a safe and useful method for preoperative examination of the proximal colon after metallic stent placement in patients with acute colon obstruction caused by cancer[34].
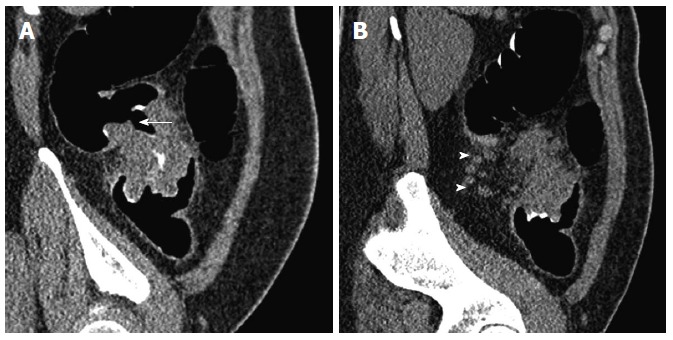
Overall, the above data indicate that CTC, despite its limitations, should be the examination of choice to complete colonic examination after incomplete colonoscopy in patients with CRC (Figure 1), as it reliably detects synchronous cancers and polyps, allowing surgical removal of cancer and/or post-operative endoscopic polypectomy.
Figure 1.
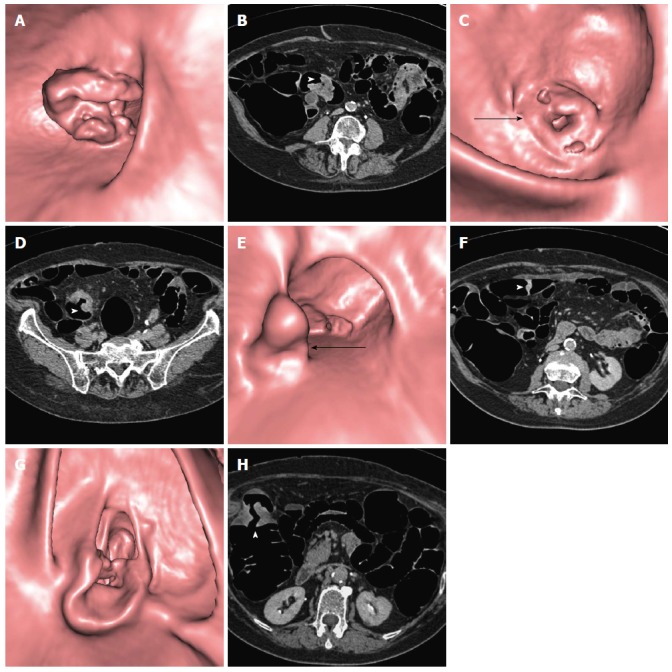
Computed tomography colonography performed in an 83-year-old female with incomplete colonoscopy due to stenosing adenocarcinoma of the sigmoid colon. Computed tomography colonography (CTC) identified three other synchronous colonic tumors confirmed as adenocarcinomas at surgery. CTC endoluminal and axial source images are shown. A, B: Distal stenosing lesion of the sigmoid (arrowhead); C, D: Proximal stenosing lesion of the sigmoid (arrow and arrowhead); E, F: Vegetating lesion of the transverse colon (arrow and arrowhead); G, H: Stenosing lesion of the right flexure (arrowhead).
TUMOR LOCALIZATION
Tumor localization is another significant issue of preoperative work-up for CRC, especially in the case of the laparoscopic approach. Laparoscopic surgery for CRC is increasing in clinical practice as it showed comparable results to those of open surgery in randomized trials[35]. Accurate preoperative localization is fundamental in laparoscopy-assisted colectomy because the colon cannot be palpated during the procedure and the lesion may not be apparent on the serosal surface, adding the risk of removing the wrong colonic segment[36].
Precise endoscopic localization of the tumor can be challenging as anatomical landmarks may not be readily apparent at colonoscopy and often only the distance from the anal verge is recorded. The endoscopist can also be confounded by the presence of a redundant colon or anatomic variants. In fact, studies showed that colonoscopy has a suboptimal accuracy in locating the tumor, which can be incorrect in 14%-21% of the cases[37,38], especially in the sigmoid and descending colon[37].
Other techniques can be used to precisely localize colonic lesions, such as barium enema, CTC, endoscopic tattooing, and intraoperative colonoscopy[39].
As DCBE is a suboptimal tool to detect CRC, its usefulness for tumor localization is questionable. Moreover, DCBE does not clearly show the position of the various colonic segments in the three dimensions leading to potential errors, especially in the transverse and sigmoid colon. CTC clearly demonstrates the involved colonic segment, the length of tumor extension and its relationship with adjacent organs, vascular structures and peritoneal spaces. On 94 patients with CRC, the accuracy of CTC for tumor localization was 94.7%[39]. In 65 patients with CRC, the sensitivity and specificity of CTC in determining the location of colonic masses were found to be 100% and 96%, respectively, whereas colonoscopy failed to precisely localize the tumor in 24% of cases[40].
CANCER STAGING
Treatment of CRC depends on the preoperative assessment of disease extension. Colorectal carcinomas are clinically staged using the TNM system established by the American Joint Committee on Cancer (Table 2)[41]. Chest and abdominal CT is recommended for the preoperative staging of CRC by the European Society of Medical Oncology[3] and by the American College of Radiology[4], with the exception of rectal cancer, for which magnetic resonance is more accurate for T staging. Although CT is the examination of choice, disappointing results have been reported with staging accuracy, ranging from 48% to 77%[42]. CTC potentially represents a comprehensive examination for CRC staging, as it allows for the evaluation of the inner and outer colonic wall (T stage), pericolonic lymph nodes (N) and distant metastases (M) (Figure 2).
Table 2.
TNM staging of colorectal cancer1
| Stage | Description |
| Primary tumor (T) | |
| T1 | Tumor invades submucosa |
| T2 | Tumor invades muscularis propria |
| T3 | Tumor invades through the muscularis propria into the subserosa, or into the non-peritonealized pericolic tissues |
| T4 | Tumor directly invades other organs or structures and/or perforates the visceral peritoneum |
| Regional lymph nodes (N) | |
| N0 | No regional lymph node metastases |
| N1 | Metastases in 1-3 regional lymph nodes |
| N2 | Metastases in ≥ 4 regional lymph nodes |
| Distant metastases (M) | |
| M0 | No distant metastases |
| M1 | Distant metastases |
1American Joint Committee on Cancer (AJCC).
Figure 2.
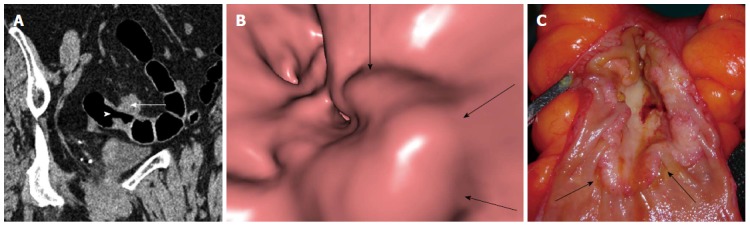
Stenosing adenocarcinoma of the sigmoid colon. A: A Computed tomography colonography (CTC) oblique coronal reconstructed image depicts the lesion (arrowhead) and its nodular infiltrating margins in pericolonic fat (arrow); B: An endoluminal CTC image better shows lobulated inner borders (arrows) of the lesion; C: A surgical specimen from left hemicolectomy shows the stenosing lesion with its lobulated inner borders (arrows).
Several studies evaluated accuracy of CTC for T and N staging of CRC[42-47]. Because CT cannot discriminate the different bowel wall layers, a simplified T staging system has been proposed for CTC reports with a grouped T1/T2 category for lesions confined to the bowel wall, T3 category for lesions invading subserosal fat and T4 category for cancer invading adjacent organs[42].
To distinguish T1/T2 from T3 cancers, both colonic wall deformity and lesion outer borders should be considered. As suggested by Utano et al[44], intestinal wall deformity associated with CRC and observed on SSD reconstructions can be classified into arc type, trapezoid type, and apple-core type. Arc type is defined as a smooth concave wall deformity, trapezoid type is defined as a square-like irregular wall deformity involving less than 50% of the circumference of the lumen, and apple-core type is defined as a trapezoidal wall deformity involving more than 50% of the circumference of the lumen. The arc or trapezoid type is associated with T1/T2 cancers (Figure 3), whereas the apple-core type is associated with T3/T4 (Figure 4). In a series of 246 patients with CRC, the sole evaluation of wall shape deformity, as described above, showed an overall accuracy for T staging of 79%[44]. With a similar classification of wall deformity, an accuracy of 77.6% was reported in another study[43].
Figure 3.
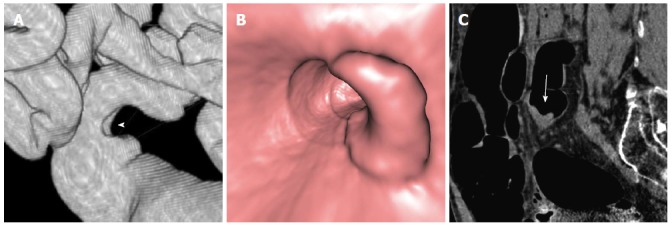
Computed tomography colonography of a T2 vegetating lesion of the sigmoid colon. A: A Computed tomography colonography (CTC) SSD reconstructed image shows a trapezoid type wall deformity of the sigmoid colon (arrowhead); B: A CTC endoluminal image demonstrates that wall involvement is less than 50%of luminal circumference. C: A CTC sagittal reconstructed image shows that the lesion (arrow) has sharp margins.
Figure 4.
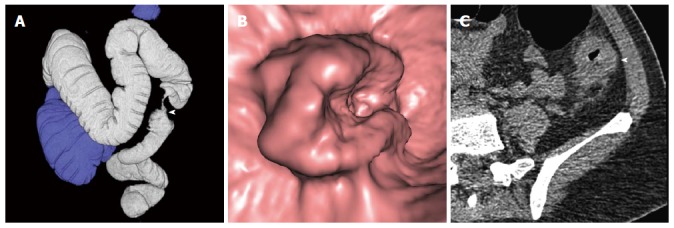
Computed tomography colonography of a T3 stenosing lesion of the descending colon. A: A Computed tomography colonography (CTC) SSD reconstructed image shows an apple-core type wall deformity of the descending colon (arrowhead); B: A CTC endoluminal image demonstrates that wall involvement is more than 50% of the luminal circumference; C: A CTC axial source image shows that the lesion (arrowhead) has nodular infiltrating margins.
Colonic wall outer margins should also be evaluated to distinguish T1/T2 from T3 cancers. Rounded or nodular advancing margins in perivisceral fat are considered an expression of a T3 stage cancer[42]. The presence of spiculations within the fat is not universally considered a sign of pericolonic fat invasion, as spiculations can be caused by inflammatory reactions and extramural fibrosis[48]. Direct invasion or absence of a fat cleavage plane from an adjacent organ indicates a T4 stage cancer. Using the above-mentioned criteria, the overall accuracy of CTC for T staging ranged from 66% to 95%[42-47].
The identification of nodal involvement with CT is limited by the use of dimensional and other morphological criteria, such as clustering. In particular, as proposed by Filippone et al[42], N1 stage can be assumed on CTC if a cluster of three nodes is present, independent of their size, or if fewer than three lymph nodes are present, with at least one of the nodes measuring 10 mm or more in the long axis. In stage N2 neoplasms, more than three perivisceral lymph nodes are identified, regardless of their size (Figure 5). Using these criteria, the overall accuracy of CTC for N staging ranged from 70% to 85%[42-47]. Notably, the accuracy of CTC for nodal staging may be unsatisfactory because the presence of regional lymph-node metastases represents an important indication for adjuvant chemotherapy, and up to 30% of node-negative patients eventually develop distant metastases, possibly as a consequence of lymph-node micrometastases[49].
Figure 5.
Computed tomography colonography of a T3 N2 stenosing computed tomography colonography of the descending colon. A: A Computed tomography colonography (CTC) sagittal reconstructed image shows the lesion (arrow); B: A CTC sagittal reconstructed image demonstrates four subcentimetric perivisceral lymph nodes (arrowheads).
It has been emphasized that the use of MPR images[45], and in particular of true axial images along the short axis of the colonic segment[50], improves the depiction of the outer margins of the lesion, of the relationships with adjacent organs and of regional lymph nodes, leading to more accurate T and N staging.
Finally, similar to standard contrast-enhanced abdominal CT, CTC with intravenous contrast administration allows for the identification of liver metastases (Figure 6), retroperitoneal or iliac lymph node enlargement, and the presence of peritoneal carcinosis (Figure 7). Moreover, scans conducted at the level of the lower pulmonary lobes can identify lung metastases.
Figure 6.
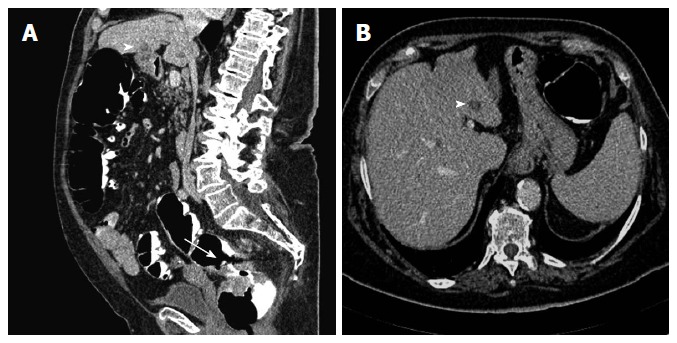
Computed tomography colonography of T3 M1 rectal cancer. A: A sagittal reconstructed image shows the rectal tumor (arrow) and a hepatic metastasis appearing as a hypoattenuating focal lesion (arrowhead); B: An axial source image demonstrates that the metastatic lesion is located in the third hepatic segment (arrowhead).
Figure 7.
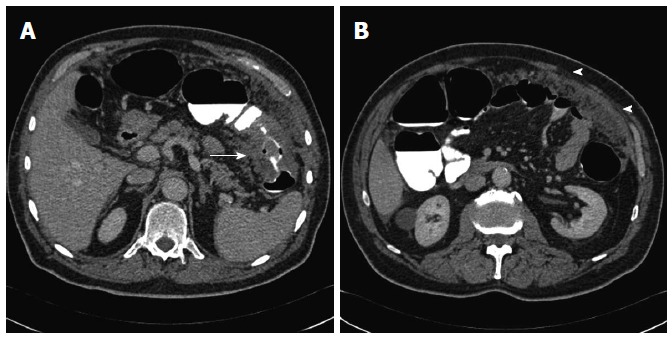
Computed tomography colonography of a T3 M1 stenosing Computed tomography colonography of the transverse colon. A: A Computed tomography colonography (CTC) axial source image shows the lesion (arrow); B: A CTC axial source image depicts marked omental thickening (arrowheads) consistent with peritoneal carcinosis.
CONCLUSION
CTC is a reliable technique to define the precise segmental location of CRC, to establish the presence of synchronous cancers and polyps greater than 10 mm, and to perform a fairly accurate tumor staging. These factors notwithstanding, CTC has some limitations, including a lack of biopsy capability, suboptimal sensitivity for synchronous small polyps, and unsatisfactory nodal staging. Bearing in mind these limitations, CTC could be employed as a “one-stop-shop” examination for preoperative assessment in patients with CRC.
Footnotes
P- Reviewers: Lin MS, Niu ZS, Stefano AD S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
References
- 1.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society, Inc. 2013. Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-037129.pdf.
- 3.Labianca R, Nordlinger B, Beretta GD, Brouquet A, Cervantes A. Primary colon cancer: ESMO Clinical Practice Guidelines for diagnosis, adjuvant treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v70–v77. doi: 10.1093/annonc/mdq168. [DOI] [PubMed] [Google Scholar]
- 4.Dewhurst C, Rosen MP, Blake MA, Baker ME, Cash BD, Fidler JL, Greene FL, Hindman NM, Jones B, Katz DS, et al. ACR Appropriateness Criteria pretreatment staging of colorectal cancer. J Am Coll Radiol. 2012;9:775–781. doi: 10.1016/j.jacr.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 5.Pickhardt PJ, Hassan C, Halligan S, Marmo R. Colorectal cancer: CT colonography and colonoscopy for detection--systematic review and meta-analysis. Radiology. 2011;259:393–405. doi: 10.1148/radiol.11101887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pickhardt PJ, Choi JR, Hwang I, Butler JA, Puckett ML, Hildebrandt HA, Wong RK, Nugent PA, Mysliwiec PA, Schindler WR. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349:2191–2200. doi: 10.1056/NEJMoa031618. [DOI] [PubMed] [Google Scholar]
- 7.Johnson CD, Chen MH, Toledano AY, Heiken JP, Dachman A, Kuo MD, Menias CO, Siewert B, Cheema JI, Obregon RG, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008;359:1207–1217. doi: 10.1056/NEJMoa0800996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neri E, Halligan S, Hellström M, Lefere P, Mang T, Regge D, Stoker J, Taylor S, Laghi A. The second ESGAR consensus statement on CT colonography. Eur Radiol. 2013;23:720–729. doi: 10.1007/s00330-012-2632-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campanella D, Morra L, Delsanto S, Tartaglia V, Asnaghi R, Bert A, Neri E, Regge D. Comparison of three different iodine-based bowel regimens for CT colonography. Eur Radiol. 2010;20:348–358. doi: 10.1007/s00330-009-1553-9. [DOI] [PubMed] [Google Scholar]
- 10.Burling D, Taylor SA, Halligan S, Gartner L, Paliwalla M, Peiris C, Singh L, Bassett P, Bartram C. Automated insufflation of carbon dioxide for MDCT colonography: distension and patient experience compared with manual insufflation. AJR Am J Roentgenol. 2006;186:96–103. doi: 10.2214/AJR.04.1506. [DOI] [PubMed] [Google Scholar]
- 11.Taylor SA, Halligan S, Goh V, Morley S, Bassett P, Atkin W, Bartram CI. Optimizing colonic distention for multi-detector row CT colonography: effect of hyoscine butylbromide and rectal balloon catheter. Radiology. 2003;229:99–108. doi: 10.1148/radiol.2291021151. [DOI] [PubMed] [Google Scholar]
- 12.Sosna J, Blachar A, Amitai M, Barmeir E, Peled N, Goldberg SN, Bar-Ziv J. Colonic perforation at CT colonography: assessment of risk in a multicenter large cohort. Radiology. 2006;239:457–463. doi: 10.1148/radiol.2392050287. [DOI] [PubMed] [Google Scholar]
- 13.Sali L, Grazzini G, Ventura L, Falchini M, Borgheresi A, Castiglione G, Grimaldi M, Ianniciello N, Mallardi B, Zappa M, et al. Computed tomographic colonography in subjects with positive faecal occult blood test refusing optical colonoscopy. Dig Liver Dis. 2013;45:285–289. doi: 10.1016/j.dld.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Adloff M, Arnaud JP, Bergamaschi R, Schloegel M. Synchronous carcinoma of the colon and rectum: prognostic and therapeutic implications. Am J Surg. 1989;157:299–302. doi: 10.1016/0002-9610(89)90555-2. [DOI] [PubMed] [Google Scholar]
- 15.Cunliffe WJ, Hasleton PS, Tweedle DE, Schofield PF. Incidence of synchronous and metachronous colorectal carcinoma. Br J Surg. 1984;71:941–943. doi: 10.1002/bjs.1800711210. [DOI] [PubMed] [Google Scholar]
- 16.Fante R, Roncucci L, Di GregorioC MG, Losi L, Benatti P, Pedroni M, Percesepe A, De Pietri S, Ponz de Leon M. Frequency and clinical features of multiple tumors of the large bowel in the general population and in patients with hereditary colorectal carcinoma. Cancer. 1996;77:2013–2021. doi: 10.1002/(SICI)1097-0142(19960515)77:10<2013::AID-CNCR8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 17.Heald RJ, Bussey HJ. Clinical experiences at St. Mark’s Hospital with multiple synchronous cancers of the colon and rectum. Dis Colon Rectum. 1975;18:6–10. doi: 10.1007/BF02587230. [DOI] [PubMed] [Google Scholar]
- 18.Achiam MP, Burgdorf SK, Wilhelmsen M, Alamili M, Rosenberg J. Inadequate preoperative colonic evaluation for synchronous colorectal cancer. Scand J Surg. 2009;98:62–67. doi: 10.1177/145749690909800112. [DOI] [PubMed] [Google Scholar]
- 19.Howard ML, Greene FL. The effect of preoperative endoscopy on recurrence and survival following surgery for colorectal carcinoma. Am Surg. 1990;56:124–127. [PubMed] [Google Scholar]
- 20.Neerincx M, Terhaar sive Droste JS, Mulder CJ, Räkers M, Bartelsman JF, Loffeld RJ, Tuynman HA, Brohet RM, van der Hulst RW. Colonic work-up after incomplete colonoscopy: significant new findings during follow-up. Endoscopy. 2010;42:730–735. doi: 10.1055/s-0030-1255523. [DOI] [PubMed] [Google Scholar]
- 21.Halligan S, Wooldrage K, Dadswell E, Kralj-Hans I, von Wagner C, Edwards R, Yao G, Kay C, Burling D, Faiz O, et al. Computed tomographic colonography versus barium enema for diagnosis of colorectal cancer or large polyps in symptomatic patients (SIGGAR): a multicentre randomised trial. Lancet. 2013;381:1185–1193. doi: 10.1016/S0140-6736(12)62124-2. [DOI] [PubMed] [Google Scholar]
- 22.Gluecker TM, Johnson CD, Harmsen WS, Offord KP, Harris AM, Wilson LA, Ahlquist DA. Colorectal cancer screening with CT colonography, colonoscopy, and double-contrast barium enema examination: prospective assessment of patient perceptions and preferences. Radiology. 2003;227:378–384. doi: 10.1148/radiol.2272020293. [DOI] [PubMed] [Google Scholar]
- 23.Mulhall BP, Veerappan GR, Jackson JL. Meta-analysis: computed tomographic colonography. Ann Intern Med. 2005;142:635–650. doi: 10.7326/0003-4819-142-8-200504190-00013. [DOI] [PubMed] [Google Scholar]
- 24.Neri E, Giusti P, Battolla L, Vagli P, Boraschi P, Lencioni R, Caramella D, Bartolozzi C. Colorectal cancer: role of CT colonography in preoperative evaluation after incomplete colonoscopy. Radiology. 2002;223:615–619. doi: 10.1148/radiol.2233010928. [DOI] [PubMed] [Google Scholar]
- 25.Gryspeerdt S, Lefere P, Herman M, Deman R, Rutgeerts L, Ghillebert G, Baert F, Baekelandt M, Van Holsbeeck B. CT colonography with fecal tagging after incomplete colonoscopy. Eur Radiol. 2005;15:1192–1202. doi: 10.1007/s00330-005-2644-x. [DOI] [PubMed] [Google Scholar]
- 26.Copel L, Sosna J, Kruskal JB, Raptopoulos V, Farrell RJ, Morrin MM. CT colonography in 546 patients with incomplete colonoscopy. Radiology. 2007;244:471–478. doi: 10.1148/radiol.2442060837. [DOI] [PubMed] [Google Scholar]
- 27.Sali L, Falchini M, Bonanomi AG, Castiglione G, Ciatto S, Mantellini P, Mungai F, Menchi I, Villari N, Mascalchi M. CT colonography after incomplete colonoscopy in subjects with positive faecal occult blood test. World J Gastroenterol. 2008;14:4499–4504. doi: 10.3748/wjg.14.4499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pullens HJ, van Leeuwen MS, Laheij RJ, Vleggaar FP, Siersema PD. CT-colonography after incomplete colonoscopy: what is the diagnostic yield. Dis Colon Rectum. 2013;56:593–599. doi: 10.1097/DCR.0b013e3182781668. [DOI] [PubMed] [Google Scholar]
- 29.Rockey DC, Barish M, Brill JV, Cash BD, Fletcher JG, Sharma P, Wani S, Wiersema MJ, Peterson LE, Conte J. Standards for gastroenterologists for performing and interpreting diagnostic computed tomographic colonography. Gastroenterology. 2007;133:1005–1024. doi: 10.1053/j.gastro.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Leksowski K, Rudzinska M, Rudzinski J. Computed tomographic colonography in preoperative evaluation of colorectal tumors: a prospective study. Surg Endosc. 2011;25:2344–2349. doi: 10.1007/s00464-010-1566-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung DJ, Huh KC, Choi WJ, Kim JK. CT colonography using 16-MDCT in the evaluation of colorectal cancer. AJR Am J Roentgenol. 2005;184:98–103. doi: 10.2214/ajr.184.1.01840098. [DOI] [PubMed] [Google Scholar]
- 32.McArthur DR, Mehrzad H, Patel R, Dadds J, Pallan A, Karandikar SS, Roy-Choudhury S. CT colonography for synchronous colorectal lesions in patients with colorectal cancer: initial experience. Eur Radiol. 2010;20:621–629. doi: 10.1007/s00330-009-1589-x. [DOI] [PubMed] [Google Scholar]
- 33.Maras-Simunic M, Druzijanic N, Simunic M, Roglic J, Tomic S, Perko Z. Use of modified multidetector CT colonography for the evaluation of acute and subacute colon obstruction caused by colorectal cancer: a feasibility study. Dis Colon Rectum. 2009;52:489–495. doi: 10.1007/DCR.0b013e318197d789. [DOI] [PubMed] [Google Scholar]
- 34.Cha EY, Park SH, Lee SS, Kim JC, Yu CS, Lim SB, Yoon SN, Shin YM, Kim AY, Ha HK. CT colonography after metallic stent placement for acute malignant colonic obstruction. Radiology. 2010;254:774–782. doi: 10.1148/radiol.09090842. [DOI] [PubMed] [Google Scholar]
- 35.Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 36.Wexner SD, Cohen SM, Ulrich A, Reissman P. Laparoscopic colorectal surgery--are we being honest with our patients. Dis Colon Rectum. 1995;38:723–727. doi: 10.1007/BF02048029. [DOI] [PubMed] [Google Scholar]
- 37.Vignati P, Welch JP, Cohen JL. Endoscopic localization of colon cancers. Surg Endosc. 1994;8:1085–1087. doi: 10.1007/BF00705725. [DOI] [PubMed] [Google Scholar]
- 38.Piscatelli N, Hyman N, Osler T. Localizing colorectal cancer by colonoscopy. Arch Surg. 2005;140:932–935. doi: 10.1001/archsurg.140.10.932. [DOI] [PubMed] [Google Scholar]
- 39.Cho YB, Lee WY, Yun HR, Lee WS, Yun SH, Chun HK. Tumor localization for laparoscopic colorectal surgery. World J Surg. 2007;31:1491–1495. doi: 10.1007/s00268-007-9082-7. [DOI] [PubMed] [Google Scholar]
- 40.Neri E, Turini F, Cerri F, Faggioni L, Vagli P, Naldini G, Bartolozzi C. Comparison of CT colonography vs. conventional colonoscopy in mapping the segmental location of colon cancer before surgery. Abdom Imaging. 2010;35:589–595. doi: 10.1007/s00261-009-9570-3. [DOI] [PubMed] [Google Scholar]
- 41.Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 7th ed. New York: Wiley-Blackwell; 2009. [Google Scholar]
- 42.Filippone A, Ambrosini R, Fuschi M, Marinelli T, Genovesi D, Bonomo L. Preoperative T and N staging of colorectal cancer: accuracy of contrast-enhanced multi-detector row CT colonography--initial experience. Radiology. 2004;231:83–90. doi: 10.1148/radiol.2311021152. [DOI] [PubMed] [Google Scholar]
- 43.Nagata K, Endo S, Kudo SE, Kitanosono T, Kushihashi T. CT air-contrast enema as a preoperative examination for colorectal cancer. Dig Surg. 2004;21:352–358. doi: 10.1159/000081543. [DOI] [PubMed] [Google Scholar]
- 44.Utano K, Endo K, Togashi K, Sasaki J, Kawamura HJ, Horie H, Nakamura Y, Konishi F, Sugimoto H. Preoperative T staging of colorectal cancer by CT colonography. Dis Colon Rectum. 2008;51:875–881. doi: 10.1007/s10350-008-9261-0. [DOI] [PubMed] [Google Scholar]
- 45.Jin KN, Lee JM, Kim SH, Shin KS, Lee JY, Han JK, Choi BI. The diagnostic value of multiplanar reconstruction on MDCT colonography for the preoperative staging of colorectal cancer. Eur Radiol. 2006;16:2284–2291. doi: 10.1007/s00330-006-0316-0. [DOI] [PubMed] [Google Scholar]
- 46.Mainenti PP, Cirillo LC, Camera L, Persico F, Cantalupo T, Pace L, De Palma GD, Persico G, Salvatore M. Accuracy of single phase contrast enhanced multidetector CT colonography in the preoperative staging of colo-rectal cancer. Eur J Radiol. 2006;60:453–459. doi: 10.1016/j.ejrad.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 47.Stabile Ianora AA, Moschetta M, Pedote P, Scardapane A, Angelelli G. Preoperative local staging of colosigmoideal cancer: air versus water multidetector-row CT colonography. Radiol Med. 2012;117:254–267. doi: 10.1007/s11547-011-0782-6. [DOI] [PubMed] [Google Scholar]
- 48.Hulsmans FJ, Tio TL, Fockens P, Bosma A, Tytgat GN. Assessment of tumor infiltration depth in rectal cancer with transrectal sonography: caution is necessary. Radiology. 1994;190:715–720. doi: 10.1148/radiology.190.3.8115617. [DOI] [PubMed] [Google Scholar]
- 49.van der Pas MH, Meijer S, Hoekstra OS, Riphagen II, de Vet HC, Knol DL, van Grieken NC, Meijerink WJ. Sentinel-lymph-node procedure in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol. 2011;12:540–550. doi: 10.1016/S1470-2045(11)70075-4. [DOI] [PubMed] [Google Scholar]
- 50.Anderson EM, Betts M, Slater A. The value of true axial imaging for CT staging of colonic cancer. Eur Radiol. 2011;21:1286–1292. doi: 10.1007/s00330-010-2019-9. [DOI] [PubMed] [Google Scholar]


