Abstract
AIM: To conduct a systemic review and meta-analysis to investigate the role of early precut technique. Multiple randomized controlled trails (RCTs) have reported conflicting results of the early precut sphincterotomy.
METHODS: MEDLINE/PubMed, EMBASE, Cochrane Central Register of Controlled Trials and Database of Systematic Reviews, and recent abstracts from major conference proceedings were searched (June 2013). Randomized and non-randomized studies comparing early precut technique with prolonged standard methods were included. Pooled estimates of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP), cannulation and adverse events were analyzed by using odds ratio (OR). Random and fixed effects models were used as appropriate. Publication bias was assessed by funnel plots. Heterogeneity among studies was assessed by calculating I2 measure of inconsistency.
RESULTS: Seven randomized and seven non-randomized trials met inclusion criteria. Meta-analysis of RCTs showed a decrease trend for PEP with early precut sphincterotomy but was not statistically significant (OR = 0.58; 95%CI: 0.32-1.05; P = 0.07). No heterogeneity was noted among the studies with I2 of 0%.
CONCLUSION: Early precut technique for common bile duct cannulation decreases the trend of post-ERCP pancreatitis.
Keywords: Early precut, Endoscopic retrograde cholangiopancreatography cannulation, Post-endoscopic retrograde cholangiopancreatography pancreatitis, Randomized controlled trials, Meta-analysis
Core tip: Multiple trials are available in literature, but still the optimal timing of precut sphincterotomy is debatable. We conducted systemic review and meta-analysis to explore the effect of early precut sphincterotomy on post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis with emphasis on analysis of optimal timing of precut sphincterotomy. Our meta-analysis showed that early precut sphincterotomy decreases the odds of post-ERCP pancreatitis, particularly if done within 5-10 min of failed cannulation without compromising cannulation rates or increasing other complications.
INTRODUCTION
Common bile duct (CBD) cannulation is a prerequisite for any biliary therapeutic intervention in endoscopic retrograde cholangiopancreatography (ERCP). Even in experienced hands, cannulation may be difficult in 10%-20% of cases based on patient and procedure related factors[1]. Precut sphincterotomy is one of the rescue techniques in these difficult cannulations. The term “precut” refers to action of performing sphincterotomy before CBD access is achieved. In this technique, a cut is made at orifice and extended cephalad for a variable distance to expose CBD opening, commonly referred to as papillotomy. However, another technique has been described in which a cut is made few millimeters above papillary orifice and extended downwards, commonly referred to as fistulotomy. Both these techniques help in facilitating CBD access in difficult cannulation.
Although precut is a rescue step in difficult cannulation, it is considered a risk factor for ERCP adverse events, particularly pancreatitis. Several large prospective studies[2-6] and a meta-analysis[7] have identified precut sphincterotomy as an independent risk factor for post-ERCP pancreatitis (PEP), irrespective of the number of attempts. Therefore, the current practice is that precut sphincterotomy is used as a salvage measure when multiple attempts of cannulation have failed via standard methods. However, recent larger studies have identified repeated cannulation attempts with standard approach as a risk factor for PEP, rather than precut sphincterotomy itself[8,9]. Several randomized[10-16] and non-randomized studies[17-23] of small sample sizes have evaluated the role of early precut sphincterotomy vs repeated attempts at cannulation with or without guidewire for the prevention of PEP with varying results. Because of the varied results and small sample sizes of the studies, we performed a systematic review and meta-analysis to compare adverse events and cannulation rates in early precut vs standard conventional methods in CBD cannulation.
MATERIALS AND METHODS
Study selection
Articles and abstracts comparing early institution of precut sphincterotomy vs standard methods of cannulation with sphincterotome with or without guidewire for CBD cannulation and PEP were selected. Studies comparing two different modalities for CBD cannulation with using precut sphincterotomy as a rescue mechanism and/or case series were excluded. The literature search was restricted to adult patients. There were no language restrictions. Both full length and abstract publications were selected.
Literature search and identification of primary studies
All articles comparing early precut sphincterotomy with standard approach for CBD cannulation were searched irrespective of language, publication status (articles or abstracts), or results. A three-stage search strategy was adopted and implemented. First, a search of MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials using PubMed and Ovid as search engines (1966-June 2013). The search terms used were precut for CBD cannulation, precut sphincterotomy, precut papillotomy, precut endoscopic retrograde cholangiopancreatography, post-ERCP pancreatitis, post-ERCP pancreatitis and prevention, and/or post-ERCP pancreatitis risk factors. Second, reference lists of retrieved articles, reviews, and meta-analyses were scanned for additional articles. Third, a manual search of abstracts submitted to the Digestive Disease Week, American College of Gastroenterology, and United European Gastroenterology Week (2005-2013) was performed.
Data extraction
Data extraction was independently performed by two investigators (Choudhary A and Winn J) and reviewed by a third investigator (Bechtold ML) for agreement. The two independent investigators extracted data from each study using a common data extraction form. Details of study design (randomization/blinding/concealment), number of subjects and dropouts, methods of precut, timing of precut in precut group, total duration and attempts in conventional group, use of guidewire and stents, inclusion and exclusion criteria, other adverse events, cannulation rate, and PEP were evaluated. All studies were assigned a quality score based upon the Jadad scale, with five being of high quality and zero being of poor quality[24]. Disagreements were discussed and resolved by consensus.
Statistical analysis
Statistical pooling of the data was done for randomized controlled trials (RCTs). Data from non-randomized studies were excluded from the statistical pooling. Primary outcome was the incidence of PEP. Secondary outcomes were the cannulation rates and overall adverse events. All data was analyzed according to both per-protocol and intention-to-treat analysis. The effects of early precut application were analyzed by calculating pooled estimates of PEP, cannulation rates, and other adverse events. Separate analyses were performed for each outcome by using odds ratio (OR) or weighted mean difference (WMD). Random or fixed effects models were used as appropriate. A statistically significant result was indicated by 95%CI not including 1 and a P-value of < 0.05. Whenever statistical significance was detected, an absolute risk reduction with 95%CI and the number needed-to-treat (NNT) with 95%CI were calculated. Rev Man 5.2 software was utilized for statistical analysis of the data. Subgroup and cumulative analysis were performed to the evaluate the effect of timing of precut sphincterotomy, study size, study quality, different methods of precut, fellows’ participation and role of pancreatic duct stent in precut application, and PEP. Publication bias was assessed by funnel plot. Heterogeneity among studies was assessed by calculating I2 measure of inconsistency with P < 0.05 being considered statistically significant.
Non-randomized studies: Data from the non-randomized studies were also extracted as described above. Retrospective or prospective non-randomized studies were included. Case series were excluded from the analysis. Primary and secondary outcomes analyzed were similar as stated above.
RESULTS
Initial search resulted in 1209 relevant articles. Out of these, 58 were selected for final review as shown in Figure 1. All articles were independently reviewed by two authors (AC and JW). Seven randomized controlled (n = 1032) (Figure 1) and seven non-randomized studies (n = 3548) met the inclusion criteria and were selected for final review and analysis. Both randomized and non-randomized studies were analyzed separately. Table 1 shows the details and Jadad scores for the selected RCTs (5 = excellent quality, 0 = poor quality). All studies were of adequate quality (Jadad scores ≥ 2). Included studies were conducted in different parts of the world, including three studies in Europe, two in Asia, and one each in Canada and Australia respectively. All studies except one were single-center studies. Table 2 represents baseline characteristics of subjects in the included randomized studies[10-16]. Mean age of subject ranged from 55.9-71 years. The majority of studies had a predominant female subject population. Indications for ERCP varied in all trials with CBD stone as predominant indication in majority of trials ranging from 10.3% to 74.5%. Four trials included subjects with sphincter of Oddi dysfunction (SOD)[10,14-16] with one trial having 21.2% of subjects with a possible SOD diagnosis[14]. Five trials included subjects with malignancy leading to obstructive jaundice[10-13,15]. All studies excluded patient who had previous sphincterotomy, history of acute pancreatitis at the time of procedure, and patients with altered anatomy. Table 3 showed interventions done in various trials. Timing for precut sphincterotomy varied among the studies. Two studies[12,14] used precut as initial method of cannulation in early precut group, whereas two trials[13,16] used five minutes of failed cannulation as a marker for difficult cannulation before precut sphincterotomy. The other three trials used 10 min or multiple attempts of failed cannulation[10,11,15] before precut sphincterotomy. In standard cannulation group, additional time of 10-20 min are allowed in different trials before proceeding to precut as one of the rescue methods or aborting the procedure. Methods of precut sphincterotomy varied among different studies. Four studies[10,13,15,16] used papillotomy, two studies used fistulotomy[10,14], and one study used both fistulotomy and papillotomy[11]. All trials except one[15] used guidewire for cannulation. Only one trial used pancreatic duct (PD) stent for PEP[16] prevention in subjects with inadvertent PD cannulation. Additionally, only one trial[13] provided separate data about adverse events when precut was applied as one of the rescue methods in conventional group. In two trials[15,16] fellows participated in the procedure (Table 4).
Figure 1.
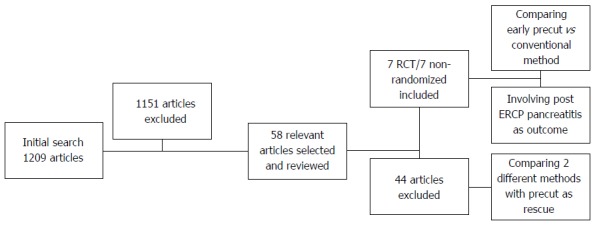
Article identification and selection algorithm. RCT: Randomized controlled trial; ERCP: Endoscopic retrograde cholangiopancreatography.
Table 1.
Quality analysis of included randomized trials
| Study | Year | Center | Country | Type of RCT | Allocation concealment | Intention to-treat | Jadad score |
| Cennamo et al[13] | 2009 | Single | Italy | Non blinded | A | Yes | 3 |
| Tang et al[15] | 2005 | Single | Canada | Non blinded | A | Yes | 3 |
| Khatibian et al[14] | 2008 | Single | Iran | Non blinded | B | Yes | 3 |
| de Weerth et al[12] | 2006 | Single | Germany | Non blinded | B | Yes | 3 |
| Zhou et al[11] | 2006 | Single | China | Non blinded | B | N/A | 2 |
| Manes et al[10] | 2009 | Multi | Italy | Non blinded | A | Yes | 3 |
| Swan et al[16] | 2013 | Single | Australia | Non blinded | A | N/A | 2 |
Allocation concealment: A: Adequate; B: Unclear; N/A: Data not available; RCT: Randomized controlled trail.
Table 2.
Baseline patient characteristics of included trials
| Study |
Patients (n) |
Age (year in mean) |
Female |
Malignant jaundice |
CBD stone |
SOD |
||||||
| E | Std | E | Std | E | Std | E | Std | E | Std | E | Std | |
| Cennamo et al[13] | 36 | 110 | 681 | 711 | 55.5% | 53.6% | 33.3% | 25.4% | 66.6% | 74.5% | 0 | 0 |
| Tang et al[15] | 32 | 30 | 64.6 | 67.2 | 53.1% | 53.3% | 34.3% | 33.3% | 21.9% | 13.3% | 3.1% | 6.7% |
| Khatibian et al[14] | 106 | 112 | 56.6 | 55.9 | 53.8% | 67% | N/A | N/A | 51.9% | 68.8% | 21.2% | 12.8% |
| de Weerth et al[12] | 145 | 146 | 66 | 64 | 66% | 66% | 40% | 23% | 46.8% | 59.5% | N/A | N/A |
| Zhou et al[11] | 43 | 48 | 62.7 | 64.3 | 39.5% | 39.5% | 30.2% | 25% | 20.9% | 22.9% | N/A | N/A |
| Manes et al[10] | 77 | 74 | 66 | 65 | 35% | 35.1% | 33.7% | 40.5% | 53.2% | 41.9% | 0 | 2.7% |
| Swan et al[16] | 39 | 34 | 59 | 57 | 72% | 66% | N/A | N/A | 10.3% | 17.6% | 5.1% | 8.8% |
Age in median year. E: Early pre cut; Std: Standard method of cannulation; N/A: Data not available; CBD: Common bile duct; SOD: Sphincter of oddi dysfunction.
Table 3.
Interventions in various trials and pancreatitis definitions
| Study | Precut timing | Timing for std cannulation | Type of pre cut | Use of GW | PD stent/PP | PEP criteria | Fellow involvement |
| Cennamo et al[13] | 5 min of failed cannulation or 3 pancreatic duct cannulation | 20 min post randomization | Papillotomy | Yes | No | Consensus | No |
| Criteria | |||||||
| Tang et al[15] | 12 min of failed cannulation | 15 min post randomization | Papillotomy | No | No | Consensus | Yes |
| Criteria | |||||||
| Khatibian et al[14] | Immediate precut | 15 min post randomization | Fistulotomy | Yes | No | Consensus | No |
| Criteria | |||||||
| de Weerth et al[12] | Immediate precut | 20 min post randomization or 3 pancreatic cannulation | Papillotomy | Yes | N/A | Consensus | No |
| Criteria | |||||||
| Zhou et al[11] | 10 min of failed cannulation or 3 pancreatic duct cannulation | N/A | Papillotomy and fistulotomy | Yes | N/A | N/A | N/A |
| Manes et al[10] | 10 min of failed cannulation or 5 pancreatic duct cannulation | 10 min post randomization | Fistulotomy | Yes | No | Consensus | N/A |
| Criteria | |||||||
| Swan et al[16] | 5 min of failed cannulation or 2 pancreatic duct cannulation | 10 min post randomization | Papillotomy | Yes | Yes1 | Consensus | Yes |
| Criteria |
Subjects with inadvertent PD cannulation. GW: Guidewire; PP: Pharmacological prophylaxis for post ERCP pancreatitis; N/A: Data not available; PD: Pancreatic duct; PEP: Post ERCP pancreatitis; ERCP: Endoscopic retrograde cholangiopancreatography.
Table 4.
Outcome of various studies
| Study |
Primary cannulation rates |
ITT |
Overall complication |
Pancreatitis |
Cholangitis |
Bleeding |
Perforation |
Need for second ERCP |
||||||||
| E | Std | E | Std | E | Std | E | Std | E | Std | E | Std | E | Std | E | Std | |
| Cennamo et al[13] | 33/36 | 104/110 | 36/36 | 110/110 | 3/36 | 7/110 | 1/36 | 6/110 | N/A | N/A | 1/36 | 1/110 | 1/36 | 0/110 | 3/36 | 6/110 |
| Tang et al[15] | 24/32 | 22/30 | 31/32 | 28/30 | 4/32 | 3/30 | 2/32 | 2/30 | 1/32 | 0/30 | 1/32 | 0/30 | 0/32 | 0/30 | 0/32 | 1/30 |
| Khatibian et al[14] | 88/106 | 100/112 | 105/106 | 111/112 | 3/106 | 3/112 | 2/106 | 3/112 | 0/106 | 0/112 | 0/106 | 0/112 | 1/106 | 0/112 | 18/106 | 12/112 |
| de Weerth et al[12] | 145/145 | 145/146 | 145/145 | 146/146 | 3/145 | 5/146 | 3/145 | 4/146 | N/A | N/A | 0/145 | 1/146 | 0/145 | 0/146 | 0/145 | 1/146 |
| Zhou et al[11] | 39/43 | 36/48 | N/A | N/A | 4/43 | 7/48 | 1/43 | 2/48 | 0/43 | 2/48 | 1/43 | 0/48 | 0/43 | 0/48 | N/A | N/A |
| Manes et al[10] | 63/77 | 66/74 | 71/77 | 71/74 | 11/77 | 16/74 | 2/77 | 11/74 | N/A | N/A | 5/77 | 2/74 | 0/74 | 1/77 | 14/77 | 8/74 |
| Swan et al[16] | 34/39 | 29/34 | N/A | N/A | 9/39 | 8/34 | 8/39 | 6/34 | N/A | N/A | 1/39 | 2/34 | 0/39 | 0/34 | N/A | N/A |
E: Early pre cut; Std: Standard method of cannulation; N/A: Data not available; ITT: Intention to treat; ERCP: Endoscopic retrograde cholangiopancreatography.
Publication bias was evaluated by funnel plot with no significant publication bias identified (Figure 2).
Figure 2.
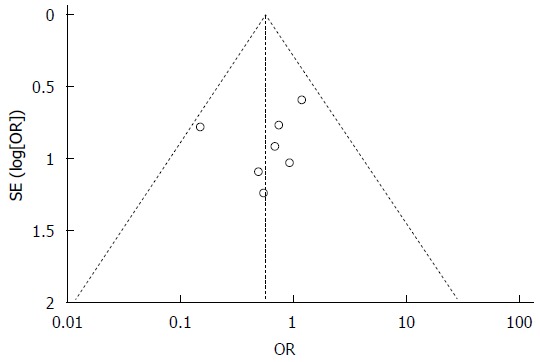
Funnel plot for publication bias.
Post-ERCP pancreatitis
All trials, except one trial[11] used the consensus definition[25] for defining PEP. In this trial, no information was provided about definition of PEP. All seven trials provided data regarding PEP. PEP was documented in 19 of 478 (3.9%) patients with early precut group vs 34 of 554 (6.1%) patients in the standard cannulation group. On pooled analysis, a trend toward decreased PEP was noticed with early precut sphincterotomy but did not reach statistical significance (OR = 0.58; 95%CI: 0.32-1.05, P = 0.07, Figure 3). No heterogeneity was noted among the studies with I2 of 0%.
Figure 3.
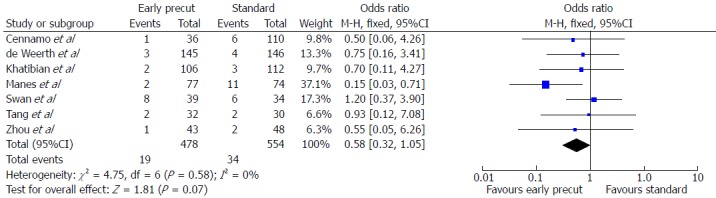
Forrest plot demonstrating post endoscopic retrograde cholangiopancreatography pancreatitis.
Subgroup and cumulative analyses were performed to evaluate the effect of various factors on PEP. Subgroup analysis was performed based on timing and methods of precut application, quality of study, use of PD stent, and fellows’ participation during the procedure. Cumulative analysis was performed based on the timing of precut application, year of studies, size, and quality of studies.
Timing of precut
On sub-group analysis, no significant effect was noticed with immediate precut sphincterotomy[12,14] (OR = 0.73, 95%CI: 0.23-2.33, P = 0.59) but a trend toward decreased PEP was noticed with pooled analysis of trials with precut sphincterotomy after 5-12 min[10,11,13,15,16] of failed cannulation (OR = 0.53, 95%CI: 0.26-1.07, P = 0.08). Similarly, a trend for PEP reduction was noticed on analysis of trials with precut sphincterotomy within 5-10 min (OR = 0.49, 95%CI: 0.23-1.04, P = 0.07)[10,11,13,16].
On cumulative analysis based on timing of precut sphincterotomy, no significant effect was noticed with immediate[12,14] (OR = 0.73, 95%CI: 0.23-2.33, P = 0.59) or immediate and within 5 min of failed cannulation[12-14,16] (OR = 0.85, 95%CI: 0.40-1.80, P = 0.67); however, a definite trend toward decreased PEP was noted with immediate and within 10 min of failed cannulation[10-14,16] (OR = 0.55, 95%CI: 0.29-1.03, P = 0.06, Table 5).
Table 5.
Subgroup and cumulative analysis for timing of precut sphincterotomy
| Timing of precut | OR | P value |
| Subgroup analysis | ||
| Immediate | 0.73; 95%CI: 0.23-2.33 | 0.59 |
| 5-10 min | 0.49; 95%CI: 0.23-1.04 | 0.07 |
| 5-12 min | 0.53; 95%CI: 0.26-1.07 | 0.08 |
| Cumulative analysis | ||
| Immediate | 0.73; 95%CI: 0.23-2.33 | 0.59 |
| Immediate and within 5 min | 0.85; 95%CI: 0.40-1.80 | 0.67 |
| Immediate and within 10 min | 0.55; 95%CI: 0.29-1.03 | 0.06 |
Methods of precut
Four studies[12,13,15,16] used papillotomy, whereas two studies[10,14] used fistulotomy. One trial[11] used both fistulotomy and papillotomy, hence was excluded from this subgroup analysis. On pooled analysis, fistulotomy significantly decreases the odds of PEP (OR = 0.27, 95%CI: 0.09-0.82, P = 0.02). The absolute risk difference was 5% (95%CI: 1%-10%) and the NNT was 20. On the other hand, papillotomy failed to show significant odds reduction for PEP (OR = 0.89, 95%CI: 0.41-1.92, P = 0.77, Table 6).
Table 6.
Odd’s ratio for outcomes
| Outcomes | OR | P value |
| Methods of precut | ||
| Fistulotomy | 0.27; 95%CI: 0.09-0.82 | 0.02 |
| Papillotomy | 0.89; 95%CI: 0.41-1.92 | 0.77 |
| Study quality | ||
| High quality study | 0.44; 95%CI: 0.21-0.93 | 0.03 |
| Sample size > 100 | 0.39; 95%CI: 0.17-0.89 | 0.02 |
Use of stent for PEP prophylaxis
One study[16] used pancreatic duct stent as PEP prophylaxis, but only in cases where pancreatic duct was inadvertently cannulated. On pooled analysis, after excluding this study, a significant reduction in odds of pancreatitis in early precut group in comparison to standard cannulation group was noted (OR = 0.45, 95%CI: 0.22-0.91, P = 0.03).
Fellow participation
In two trials[15,16], fellows participated in the study and initiated the procedure. Sub-group analysis on exclusion of these two trials showed significant odds reduction of PEP with early precut sphincterotomy (OR = 0.40, 95%CI: 0.19-0.88, P = 0.02) with no heterogeneity.
Quality of study
Subgroup analysis of studies with Jadad score of 3 or more[10,12-15] showed significant less odds of pancreatitis with early precut sphincterotomy in comparison to standard cannulation group (OR = 0.44, 95%CI: 0.21-0.93, P = 0.03) with no heterogeneity.
Year and size of study
No difference in results were noted on cumulative analysis based on year of study, but a significant odds reduction for PEP was observed on analysis of studies with Jadad score of 3 or more with study size more than 100 subjects[10,12-14] (OR = 0.39; 95%CI: 0.17-0.89, P = 0.02). No heterogeneity was noted.
Cannulation rate
All seven trials provided data regarding primary cannulation rates. Pooled per-protocol and intention-to-treat analysis of cannulation rates showed no difference between both groups (OR = 0.90; 95%CI: 0.59-1.37, P = 0.62, Figure 4). No significant heterogeneity was noted.
Figure 4.
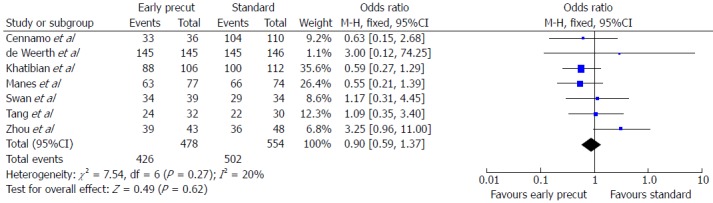
Forrest plot demonstrating cannulation rates.
Need for second ERCP
All except two trials[11,16] provided data on need for second ERCP. Pooled analysis was performed and showed no difference for the need for second ERCP for cannulation (OR = 1.54; 95%CI: 0.91-2.61, P = 0.11). No heterogeneity was noted.
Overall adverse events
The adverse events provided in all trials were PEP, perforation, cholangitis, and bleeding. On pooled analysis, trend towards lower overall adverse events was noted in early precut group (7.7%) in comparison to standard cannulation group (8.8%) but this did not reach statistical significance (OR = 0.80; 95%CI: 0.50-1.27, P = 0.34). Only three perforations were noted in all trials involving 1032 patients, two of which occurred in precut group. On pooled analysis, no significant difference was noticed between both groups (OR = 1.96; 95%CI: 0.40-9.56, P = 0.40) with no significant heterogeneity. Similar results were noted for bleeding and cholangitis (OR = 1.54; 95%CI: 0.59-3.99, P = 0.38; OR = 0.68; 95%CI: 0.11-4.25, P = 0.68) respectively, with no significant heterogeneity.
Systemic review of non-randomized studies
We also analyzed the data from non-randomized studies (Table 7). Seven studies met the inclusion criteria (n = 3548). Three studies were published as manuscripts and four as abstracts. All studies were done recently. Sample size varied from 57 to 2004 patients. In two studies[21,22], precut was applied immediately, in three other studies[17,18,23], precut was applied after 10 failed attempts at biliary cannulation, and in one study[20], it was applied after 10 min of failed cannulation or five inadvertent pancreatic duct cannulations. A statistically significant reduction of PEP with early precut application was noted in two studies[20,23]. In the other five studies, a low incidence of PEP was noted with early precut but did not reach statistical significance. The range of PEP varied from 0%-10.3% in early precut group vs 5.8%-42.8% in standard group.
Table 7.
Summary of non-randomized studies
| Study (lead author/year) | Country | Publication type | Mean age | Females | Pre cut application | n | Pancreatitis | P | |
| EP Std methods | |||||||||
| Giussani et al[17], 2008 | Italy | Abstract | N/A | N/A | < 10 cannulation attempts | 804 | 8.3% | 11.6% | NS |
| Testoni et al[18], 2010 | Italy | Article | N/A | 50.20% | < 10 cannulation attempts | 308 | 7.6% | 15.4% | NS |
| Xinopoulos et al[19], 2009 | N/A | Abstract | N/A | N/A | N/A | 134 | 8.3% | 8.5% | NS |
| Madacsy et al[20], 2009 | Hungary | Article | 57 | 91% | 10 min of failed cannulation or 5 pancreatic duct cannulation | 57 | 0% | 42.8% | < 0.05 |
| Ayoubi et al[21], 2009 | Italy | Abstract | 68.6 (median) | 58.9% | Immediate precut | 173 | 1.1% | 5.8% | NS |
| De La Mora-Levy et al[22], 2011 | Mexico | Abstract | N/A | N/A | Immediate precut | 68 | 10.3% | 10.2% | NS |
| Testoni et al[23], 2011 | Italy | Article | N/A | 49.7% | < 10 cannulation attempts | 2004 | 3.3% | 14.3% | < 0.05 |
N/A: Data not available; NS: Non significant; EP: Early pre cut; Std: Standard method of cannulation.
DISCUSSION
Successful bile duct cannulation remains the cornerstone for therapeutic ERCP. Multiple innovative techniques and tools have been developed for safe and successful cannulation. However, despite these techniques, cannulation may be unsuccessful in 10%-20% of cases based on experience of endoscopist and multiple procedural and patient related factors[1]. In these difficult cannulations, PEP is considered one of the most feared adverse events with varied incidence. Precut sphincterotomy is considered as a last resort and is one of the rescue techniques, given its implication as an independent risk factor for PEP irrespective of number of attempts[7]. Contrary to this, a few recent trials have suggested that increasing number of attempts at biliary cannulation is a risk factor for PEP rather than precut itself[8,9]. In one of the trials, risk of PEP has already increased to 14% as a result of multiple failed cannulation attempts at the time of precut sphincterotomy[26]. Recently, Bailey et al[27] demonstrated incremental increase in the incidence of PEP with increasing cannulation attempts; 11.5% with 10 to 14 attempts and 15% with > 15 attempts.
In our meta-analysis, a trend toward decreased PEP and other adverse events with similar cannulation rates with early precut sphincterotomy was observed. Although the overall pooled analysis did not reach statistical significance, on subgroup analysis of high quality studies, a significant odds reduction for PEP was observed with early precut sphincterotomy in comparison to standard approach. Similar results were observed on subgroup and cumulative analyses based on size of study as well as study quality. These results should be interpreted with caution, as studies used different time periods before considering precut sphincterotomy, with timing varying from immediate precut[12,14] to after 12 min of failed cannulation[15]. Though, above result of decrease trend in PEP is similar to previous meta-analysis[28] but in this current meta-analysis, an attempt was made by conducting cumulative and subgroup analysis to find the optimal timing before considering the cannulation as difficult and attempting precut sphincterotomy. In subgroup analysis, no difference was observed between immediate precut sphincterotomy and standard method of cannulation, but a trend toward decreased PEP was observed in subgroup analysis if precut sphincterotomy was performed within 5-10 min[10,11,13,16] of failed cannulation (P < 0.06). Similar results were observed on cumulative analysis. No difference was observed on immediate precut sphincterotomy (P = 0.59) and 5 min of failed cannulation (P = 0.67), but trend toward decreased PEP was observed with 10 min of failed cannulation (P = 0.06), similar to the subgroup analysis (Table 5). Interestingly, in contrast to popular belief, immediate precut application did not increase the risk of PEP on subgroup and cumulative analyses. PEP was noted in 1.9% in immediate pre-cut group in comparison to 2.7% in the standard group (P = 0.59).
Although in the present meta-analysis, a significant odds reduction of PEP with early precut sphincterotomy was noted on subgroup analysis of trials without fellow participation and fistulotomy, these results are based on exclusion of trials with smaller number of subjects (for fellow participation)[15,16] and analysis of only two trials (for fistulotomy)[10,14]. Overall incidences of other adverse events reported were very low in all the trials for both the groups and no difference was noted on pooled analysis. Similarly, cannulation rates were similar in both groups but not all the trials presented the data about the time required for cannulation.
In our analysis, we did not include data from non-randomized studies, however, similar results were observed on review of non-randomized studies with decreasing trend in PEP with early precut sphincterotomy, except in two trials in which a significant reduction of PEP was observed with early precut sphincterotomy.
Strengths of the present meta-analysis include inclusion of both randomized and non-randomized trials to explore literature, no significant heterogeneity for any of the analyzed outcomes was noted, and inclusion of good quality trials conducted in different parts of the world. Additionally, for the first time, an attempt was made to explore optimal timing of precut sphincterotomy. There are several limitations of the present study which include the following. First, relatively few numbers of studies were available to adequately conduct subgroup analysis to determine optimal timing and techniques of precut sphincterotomy. Second, no recommendations can be made about the role of precut sphincterotomy in the high-risk population as trials have heterogeneous subject population undergoing ERCP with only a few trials including subjects with SOD. Finally, the role of PD stenting and other pharmacologic interventions for PEP prophylaxis, which are considered as routine and standard of care in difficult cannulation as shown in previous meta-analysis and randomized trial[29,30], is unclear with early precut sphincterotomy. Future multi-center randomized controlled trials are needed not only to determine the optimal timing and technique of precut sphincterotomy, but also to explore the role of prophylactic PD stenting and other pharmacological interventions in combinations with precut sphincterotomy in difficult cannulations.
In conclusion, early precut sphincterotomy decreases the trend of PEP, particularly if done within 5-10 min of failed cannulation without compromising cannulation rates or increasing other adverse events.
ACKNOWLEDGMENTS
The authors wish to acknowledge Quratulain Annie Ahmed for her help with designing, formatting and editing of tables.
COMMENTS
Background
Despite multiple innovative techniques and tools, common bile duct cannulation remains difficult in 10%-20% of cases. Precut sphincterotomy is considered as last resort, given its implication as an independent risk factor for post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP) irrespective of number of attempts. Recently few published trials compared the outcomes and risks of early precut with varied results.
Research frontiers
Multiple randomized and non-randomized trials with small sample sizes have analyzed the effects of early precut sphincterotomy with varied results. In the field of PEP and precut sphincterotomy, the research hot spot is to find the optimal time of precut application in difficult cannulation cases.
Innovations and breakthroughs
Early precut sphincterotomy decreases the trend of PEP in comparison to conventional methods of cannulation, especially if done within 5-10 min of failed cannulation without compromising cannulation rates or increasing other adverse effects.
Applications
Precut sphincterotomy can be safely performed within 5-10 min of failed conventional cannulation methods.
Terminology
Early precut sphincterotomy decreases the trend of PEP without increasing any other adverse effects or compromising cannulation rates.
Peer review
This is a well conducted meta-analysis on the outcomes and risk of PEP with early precut sphincterotomy.
Footnotes
P- Reviewers: Akyuz U, Kapetanos D, Ojeda AG S- Editor: Cui XM L- Editor: A E- Editor: Liu XM
References
- 1.Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M, Williamson PJ, et al. Are we meeting the standards set for endoscopy Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56:821–829. doi: 10.1136/gut.2006.097543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 3.Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652–656. doi: 10.1067/mge.2002.129086. [DOI] [PubMed] [Google Scholar]
- 4.Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423. doi: 10.1111/j.1572-0241.2001.03594.x. [DOI] [PubMed] [Google Scholar]
- 5.Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson ML, Williamson PR, et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39:793–801. doi: 10.1055/s-2007-966723. [DOI] [PubMed] [Google Scholar]
- 6.Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1–10. doi: 10.1016/s0016-5107(98)70121-x. [DOI] [PubMed] [Google Scholar]
- 7.Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003;35:830–834. doi: 10.1055/s-2003-42614. [DOI] [PubMed] [Google Scholar]
- 8.Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–88. doi: 10.1016/j.gie.2008.10.039. [DOI] [PubMed] [Google Scholar]
- 9.Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139–147. doi: 10.1111/j.1572-0241.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 10.Manes G, Di Giorgio P, Repici A, Macarri G, Ardizzone S, Porro GB. An analysis of the factors associated with the development of complications in patients undergoing precut sphincterotomy: a prospective, controlled, randomized, multicenter study. Am J Gastroenterol. 2009;104:2412–2417. doi: 10.1038/ajg.2009.345. [DOI] [PubMed] [Google Scholar]
- 11.Zhou PH, Yao LQ, Xu MD, Zhong YS, Gao WD, He GJ, Zhang YQ, Chen WF, Qin XY. Application of needle-knife in difficult biliary cannulation for endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2006;5:590–594. [PubMed] [Google Scholar]
- 12.de Weerth A, Seitz U, Zhong Y, Groth S, Omar S, Papageorgiou C, Bohnacker S, Seewald S, Seifert H, Binmoeller KF, et al. Primary precutting versus conventional over-the-wire sphincterotomy for bile duct access: a prospective randomized study. Endoscopy. 2006;38:1235–1240. doi: 10.1055/s-2006-944962. [DOI] [PubMed] [Google Scholar]
- 13.Cennamo V, Fuccio L, Repici A, Fabbri C, Grilli D, Conio M, D’Imperio N, Bazzoli F. Timing of precut procedure does not influence success rate and complications of ERCP procedure: a prospective randomized comparative study. Gastrointest Endosc. 2009;69:473–479. doi: 10.1016/j.gie.2008.09.037. [DOI] [PubMed] [Google Scholar]
- 14.Khatibian M, Sotoudehmanesh R, Ali-Asgari A, Movahedi Z, Kolahdoozan S. Needle-knife fistulotomy versus standard method for cannulation of common bile duct: a randomized controlled trial. Arch Iran Med. 2008;11:16–20. [PubMed] [Google Scholar]
- 15.Tang SJ, Haber GB, Kortan P, Zanati S, Cirocco M, Ennis M, Elfant A, Scheider D, Ter H, Dorais J. Precut papillotomy versus persistence in difficult biliary cannulation: a prospective randomized trial. Endoscopy. 2005;37:58–65. doi: 10.1055/s-2004-826077. [DOI] [PubMed] [Google Scholar]
- 16.Swan MP, Alexander S, Moss A, Williams SJ, Ruppin D, Hope R, Bourke MJ. Needle knife sphincterotomy does not increase the risk of pancreatitis in patients with difficult biliary cannulation. Clin Gastroenterol Hepatol. 2013;11:430–436.e1. doi: 10.1016/j.cgh.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Giussani A, Mariani C, Vailati C, Masci E, Testoni PA. Early pre-cutting reduces the risk of post ERCP pancreatitis. Dig Liver Dis. 2008;40S:S1–S195. [Google Scholar]
- 18.Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753–1761. doi: 10.1038/ajg.2010.136. [DOI] [PubMed] [Google Scholar]
- 19.Xinopoulos D, Bassioukas SP, Kypreos D, Dimitroulopoulos D, Korkolis DP, Tsamakidis K, Patsavela S, Paraskevas E. Do pappilary manipulations with a guide wire increase the incidence of post ERCP pancreatitis Lessons learned form 1858 consecutive therapeutic ERCPs from a single institution. Gastrointest Endosc. 2009;69:AB 157–158. [Google Scholar]
- 20.Madácsy L, Kurucsai G, Fejes R, Székely A, Székely I. Prophylactic pancreas stenting followed by needle-knife fistulotomy in patients with sphincter of Oddi dysfunction and difficult cannulation: new method to prevent post-ERCP pancreatitis. Dig Endosc. 2009;21:8–13. doi: 10.1111/j.1443-1661.2008.00819.x. [DOI] [PubMed] [Google Scholar]
- 21.Ayoubi M, Castellino F, Leone N, Framarin L, Rosina F. Comparison between needle-knife fistulotomy and standard cannulation in ERCP: A single endoscopist experience. Dig Liver Dis. 2009;41 Suppl 1:S11. [Google Scholar]
- 22.De La Mora-Levy J, Barojas PF, Octavio Alonso-Larraga J, Hernandez-Guerrero A, Ramirez Solis ME, Sobrino-Cossio SR. Inicial Precut vs An Algorithmic Approach Using a Wire-Guided Sphincterotome for Selective Biliary Cannulation. Gastrointest Endosc. 2011;73:AB 361. [Google Scholar]
- 23.Testoni PA, Giussani A, Vailati C, Testoni S, Di Leo M, Mariani A. Precut sphincterotomy, repeated cannulation and post-ERCP pancreatitis in patients with bile duct stone disease. Dig Liver Dis. 2011;43:792–796. doi: 10.1016/j.dld.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 24.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 26.Vandervoort J, Carr-Locke DL. Needle-knife access papillotomy: an unfairly maligned technique. Endoscopy. 1996;28:365–366. doi: 10.1055/s-2007-1005482. [DOI] [PubMed] [Google Scholar]
- 27.Bailey AA, Bourke MJ, Kaffes AJ, Byth K, Lee EY, Williams SJ. Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video) Gastrointest Endosc. 2010;71:266–271. doi: 10.1016/j.gie.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 28.Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk Meta-analysis of randomized controlled trials. Endoscopy. 2010;42:381–388. doi: 10.1055/s-0029-1243992. [DOI] [PubMed] [Google Scholar]
- 29.Choudhary A, Bechtold ML, Arif M, Szary NM, Puli SR, Othman MO, Pais WP, Antillon MR, Roy PK. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc. 2011;73:275–282. doi: 10.1016/j.gie.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 30.Elmunzer BJ, Scheiman JM, Lehman GA, Chak A, Mosler P, Higgins PD, Hayward RA, Romagnuolo J, Elta GH, Sherman S, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366:1414–1422. doi: 10.1056/NEJMoa1111103. [DOI] [PMC free article] [PubMed] [Google Scholar]


