Abstract
The recently described supplementary grading scale may be superior to the widely used Spetzler-Martin grading scale in the prediction of microsurgical outcomes for cerebellar arteriovenous malformations (AVM). We report two cases of ruptured cerebellar AVMs with the same Spetzler-Martin grade but different supplementary grades treated with microsurgical resection. Both patients had symptomatic brainstem compression from cerebellar hematomas and subsequently underwent uncomplicated surgeries; however, their outcomes were significantly different. It has previously been proposed that AVMs distort cerebellar anatomy in a different manner than supratentorial cerebral anatomy thereby potentially resulting in misrepresentation when utilizing the Spetzler-Martin grading scale. However, the components of the supplementary grading scale are independent of cerebellar anatomy, which may explain why it has been shown to be better than the Spetzler-Martin grading scale for prediction of surgical outcomes. In addition, due to the smaller volume of the posterior fossa compared to the supratentorial compartment, rupture of cerebellar AVMs may result in rapid and catastrophic neurological compromise. Therefore, the role of microsurgery may be more critical for AVMs of the cerebellar than for those located elsewhere. Simple and effective grading systems are invaluable tools for clinical and surgical decision-making, although the decisions rendered should always be made in conjunction with the patient's presentation and the physician's experience.
Keywords: Cerebellum, Intracranial arteriovenous malformations, Intracranial hemorrhages, Microsurgery, Stroke
INTRODUCTION
Cerebellar arteriovenous malformations (AVM) comprise 10-15% of intracranial AVMs. A previous report suggested that the Spetzler-Martin grading scale cannot accurately predict microsurgical outcomes for AVMs located in the cerebellum.2) Lawton et al. described the supplementary grading scale, which accounts for patient age, history of AVM rupture, and compactness of the nidus.1) We report two cases of ruptured cerebellar AVMs treated at our institution in which surgical outcomes showed correlation with the supplementary grade but not with the Spetzler-Martin grade.
CASE REPORTS
Case 1
A 16-year-old female presented with sudden onset headache, nausea, and vomiting followed rapidly by coma. Brain computed tomography (CT) showed a large cerebellar hematoma resulting in tonsillar herniation and obstructive hydrocephalus. CT angiography (CTA) showed a left tentorial AVM measuring 12×8 mm in the middle cerebellar peduncle supplied by the left superior cerebellar artery (SCA) and anterior inferior cerebellar arteries (AICA) and draining into the left transverse and straight sinuses (Fig. 1). The AVM was Spetzler-Martin grade II and supplementary grade I. Due to compression of the brain stem by the hematoma, the patient was taken emergently to the operating room in order to undergo suboccipital craniectomy and AVM resection. No residual nidus was observed on post-operative digital subtraction angiography (DSA). The patient had transient abducens and facial nerve palsies, which had resolved at the time of discharge. At 2-month follow-up, the patient had mild dysmetria and intermittent diplopia but had returned to playing softball.
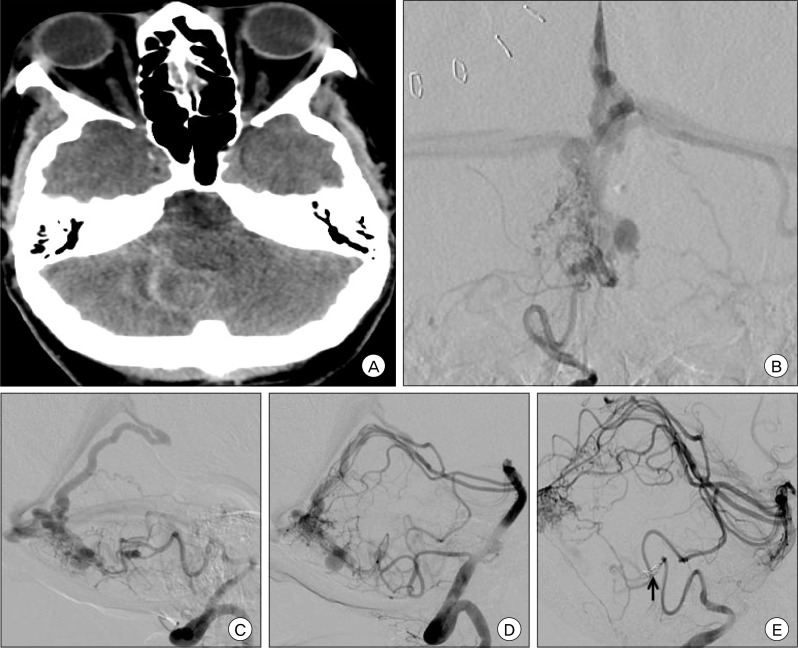
Fig. 1.
Pre-operative (A) non-contrast brain computed tomography (CT), axial view, shows a large cerebellar hematoma with severe effacement of the fourth ventricle, resultant hydrocephalus, and tonsillar herniation. Brain CT angiography (CTA), axial (B), coronal (C), and sagittal (D) views shows a Spetzler-Martin Grade II, supplementary grade I left cerebellar arteriovenous malformation (AVM) measuring 12×8 mm in size, supplied by the left superior cerebellar artery (SCA) and anterior inferior cerebellar artery (AICA) and draining into the left transverse and straight sinuses. Post-operative angiography with left vertebral artery injection, AP (E) and lateral (F) views, shows no residual AVM, consistent with complete microsurgical obliteration.
Case 2
A 59 year-old female was found unresponsive. Brain CT showed a subarachnoid hemorrhage and fourth ventricular hemorrhage resulting in obstructive hydrocephalus necessitating placement of an emergent external ventricular drain. DSA showed a right cerebellar AVM measuring 14×15×13 mm supplied by the bilateral SCAs and posterior inferior cerebellar arteries (PICA) with multiple perinidal aneurysms arising from the feeding right PICA (Fig. 2). The AVM was Spetzler-Martin Grade II and supplementary grade III. Endovascular embolization with polyvinyl alcohol (PVA) and occlusion of the right PICA proximal to the aneurysms was performed prior to surgical resection. The patient subsequently underwent suboccipital craniectomy for AVM resection. The patient's post-operative course was notable for persistent dysphagia requiring placement of a gastrostomy tube, placement of a ventriculoperitoneal shunt, and subclavian thrombus necessitating long-term anticoagulation. The patient was discharged to a nursing home after three weeks of hospitalization.
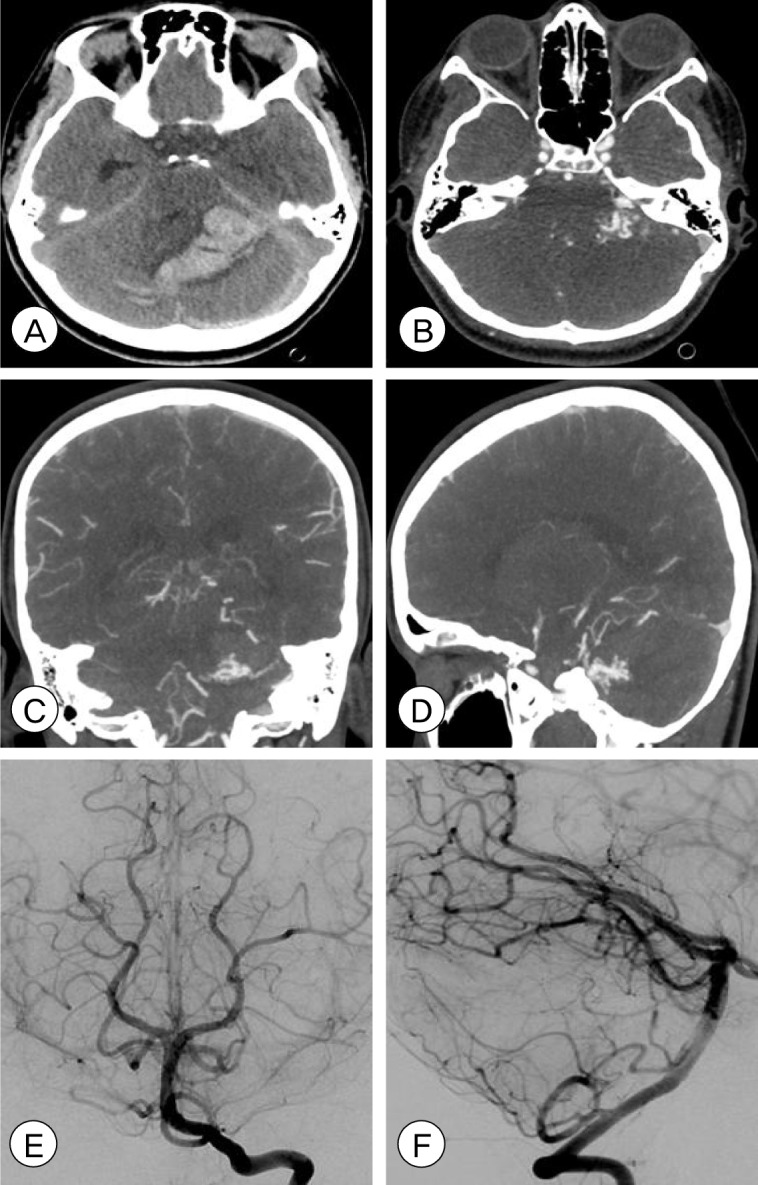
Fig. 2.
Pre-operative (A) non-contrast brain CT, axial view, shows diffuse cerebellar subarachnoid hemorrhage and intraventricular hemorrhage of the fourth ventricle resulting in obstructive hydrocephalus. Pre-operative angiography with right vertebral artery injection, AP (B) and lateral (C) views, and left vertebral artery injection, lateral view (D) shows a Spetzler-Martin Grade II, supplementary grade III right cerebellar arteriovenous malformation (AVM) measuring 14×15×13 mm in size, supplied by the bilateral superior cerebellar arteries (SCAs) and posterior inferior cerebellar arteries (PICAs) and draining into the vein of Galen. There are multiple feeding artery aneurysms on the right PICA as well as several venous dilatations of the deep draining vein. After pre-operative polyvinyl alcohol (PVA) particle embolization through the right PICA, the feeding artery was occluded with coils (arrow) as shown on this DSA right vertebral artery injection lateral view (E).
DISCUSSION
Cerebellar AVMs are a unique subset of intracranial AVMs that present with hemorrhage more frequently than supratentorial AVMs. Due to the relatively small volume of the posterior fossa and their proximity to the brainstem, rupture of cerebellar AVMs may quickly result in devastating neurological consequences. Conversely, neurological decline may be reversed by timely decompression. Neither of the patients described here had operative complications however, they showed significantly different outcomes following resection. The first patient had an eloquent AVM with superficial venous drainage while the second patient had a non-eloquent AVM with deep venous drainage. Based on the Spetzler-Martin grading scale, both AVMs were grade II. However, based on the disparity in age, the first patient was younger than 20 years and the second patient was older than 40 years, the supplementary grades were I and III, respectively.1) This is perhaps an indication of the deteriorating neuroregenerative capability of the brain that accompanies aging.
The utility of grading scales lies in the simplification of complex management decisions into an algorithm for which certain characteristics of patient and lesion may be correlated with treatment outcomes. The Spetzler-Martin grading scale is the most widely used grading system for AVMs.3) Rodriguez-Hernandez et al. hypothesized that the predictive capability of the supplementary grading scale was superior to that of the Spetzler Martin grading scale for assessment of outcomes following microsurgical resection of cerebellar AVMs.2) Deep venous drainage is a better indicator of the depth of the nidus for cerebral AVMs than for cerebellar AVMs. Cerebellar anatomy is altered by AVMs in a different manner than cerebral anatomy such that the supplementary grading scale may be better than the Spetzler-Martin grade for prediction of surgical outcomes. In comparison with ruptured cerebral AVMs, which may be managed conservatively followed by radiosurgery for achievement of obliteration, ruptured cerebellar AVMs may be better treated by surgical resection, especially when the associated hemorrhage results in symptomatic compression of surrounding neural structures.
In conclusion, the surgical risk for cerebellar AVMs may be predicted by either the Spetzler-Martin or supplementary grading scales, although the supplementary scale may show better correlation with outcomes.1-3) However, neither grading system can substitute for experienced clinical and surgical judgment.
References
- 1.Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010 Apr;66(4):702–713. doi: 10.1227/01.NEU.0000367555.16733.E1. discussion 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodríguez-Hernández A, Kim H, Pourmohamad T, Young WL, Lawton MT University of California, San Francisco Arteriovenous Malformation Study Project. Cerebellar arteriovenous malformations: Anatomic subtypes, surgical results, and increased predictive accuracy of the supplementary grading system. Neurosurgery. 2012 Dec;71(6):1111–1124. doi: 10.1227/NEU.0b013e318271c081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986 Oct;65(4):476–483. doi: 10.3171/jns.1986.65.4.0476. [DOI] [PubMed] [Google Scholar]