Abstract
Introduction
Acute low neoplasm ileus requires emergency surgery. Nowadays there are increased numbers of patients with comorbidities, which causes higher risk of intra- and postoperative complications.
Aim
To evaluate the clinical usefulness of endoscopic self-expandable stent placement for malignant colorectal ileus.
Material and methods
Twenty-one patients (8 women and 13 men), mean age 66.7 years, with low neoplasm obstruction, underwent endoscopic stenting of the stricture. This procedure was performed as a bridge to the surgery especially for high-risk patients. Eight of them had coagulation system impairment, 5 severe metabolic disorders, 4 circulatory insufficiency, 3 severe malnutrition and 1 patient undiagnosed synchronic rectal tumor. In 10 patients cancer was located in the sigmoid colon, in 7 in the rectum, in 2 in the ascending colon, and the transverse and ascending colon was involved in another 2 patients.
Results
All 21 patients (100%) underwent endoscopic stenting successfully. There were no complications after stent placement. The authors underline that placement of expandable metallic stents for patients with malignant colon obstruction with acute ileus is a safe and effective method. It gives an opportunity for quick balance of fluid, electrolyte, and the coagulation system and improvement of efficiency of the circulatory and respiratory system.
Conclusions
Endoscopic treatment of ileus helps precisely estimate tumor advancement and gives the possibility of a single stage radical surgical procedure.
Keywords: colorectal cancer, ileus, endoscopic stenting
Introduction
Ever since Dohmoto first placed an endoscopic prosthesis in a patient with a non-resectable rectal cancer in 1991, this method has found a wide range of application in the management of both benign and malignant gastrointestinal tract obstructions [1]. In the case of colorectal malignancies, there are three clinical indications for endoscopic stenting: palliative dilation of a non-resectable obstruction, treatment of neoplastic fistulas, and a preoperative obstruction decompression [2–6]. This latter indication becomes particularly important in patients with high operative risk, who require pharmacological preparation for surgery, for instance in the case of patients with coagulation disorders.
Aim
To evaluate the clinical application of endoscopic intestinal stenting in cases of neoplastic obstruction of the large intestine.
Material and methods
Between 2007 and 2010, 21 patients were subjected to endoscopic stenting due to acute malignant obstruction of the lower digestive tract at the 2nd Department of General and Gastroenterological Surgery of the Medical University of Bialystok. This group included 8 women and 13 men aged between 47 and 86 years (mean 66.7 years). The sigmoid colon was the most frequent location of malignancy (n = 10), followed by the upper rectum (n = 7). Other tumor locations included the descending, transverse, and ascending colon. Detailed data on the location of the malignant obstruction of the large intestine are summarized in Table I.
Table I.
Location of colorectal malignancies leading to an acute obstruction of the digestive tract
| Tumor location | Number of patients | Percent |
|---|---|---|
| Sigmoid colon | 10 | 47.6 |
| Rectum | 7 | 33.3 |
| Descending colon | 2 | 9.5 |
| Transverse colon | 1 | 4.8 |
| Ascending colon | 1 | 4.8 |
At the time of diagnosis of the obstruction, all patients presented with additional comorbidities. These markedly modulated the risk of intra- and perioperative complications. The most significant risk factors included clotting disorders in patients receiving anticoagulative therapy, and profound metabolic disorders. Detailed data on the comorbidities presented by our patients are summarized in Table II.
Table II.
Comorbidities present in patients with acute malignant colorectal obstruction who qualified for endoscopic stenting
| Comorbidity | Number | Percent |
|---|---|---|
| Clotting disorders due to anticoagulant therapy | 8 | 38.1 |
| Metabolic disorders | 5 | 23.8 |
| Severe malnutrition | 3 | 14.3 |
| Cardiovascular insufficiency | 4 | 19.0 |
| Suspected synchronous rectal malignancy without histopathological diagnosis | 1 | 4.8 |
Clotting disorders were diagnosed in eight patients with malignant colorectal obstruction. One of these patients developed symptoms of acute intestinal obstruction two weeks after the implantation of a metal coronary stent as an endovascular treatment for a myocardial infarct. The patient was therefore under one-month double therapy with clopidogrel 75 mg and acetylsalicylic acid. Four other patients were receiving cardiologic doses of acetylsalicylic acid due to ischemic heart disease with a history of myocardial infarct. Two female patients were under warfarin treatment, and one was receiving acenocoumarol in the context of persistent atrial fibrillation. International normalized ratio (INR) remained within the therapeutic range in all the three individuals. Additionally, oral anticoagulants were administered in four other patients with cardiogenic vascular insufficiency and persistent atrial fibrillation. Five individuals with diabetes mellitus represented disorders of acid-base homeostasis, glycemic control, and water-electrolyte balance with hypokalemia. Three patients presented a weight loss greater than 15% of their usual weight in the past month, with serum albumin concentrations below 3.0 g/dl and total lymphocyte count inferior to 1000 cells/µl. A 3-cm ulceration located on the posterior rectal wall 3 cm proximal to the anal sphincters was revealed in one patient with an obstruction caused by a carcinoma of the rectosigmoid junction. This newly detected lesion, supposedly a synchronic malignancy, was not examined histopathologically at the time of this study.
Results
In all patients endoscopic stenting of the large intestine was performed within 24 h of obstruction diagnosis. No stenting-related complications were observed, and the intestinal patency was restored immediately after the endoscopic procedure (Photos 1 and 2).
Photo 1.
Abdominal X-ray taken in a standing position. The intestinal obstruction was eliminated by means of endoprosthesis placement. The endoscopically inserted self-expandable metal prosthesis can be observed in the mid-hypogastrium, overpassing the malignant obstruction of the sigmoid colon. The hepatic colonic flexure is still dilated and overflown with intestinal gases with visible air-fluid levels. The left colon was decompressed of retained fecal masses
Photo 2.
Computed tomography scan illustrating the wide rectal lumen with an expanded endoprosthesis. Intestinal loops show no signs of obstruction
Oral administration of fluids was possible as early as on the first postoperative day. Subsequently, laxative agents were administered and a low-residue diet was implemented. Once the gastrointestinal transit was restored, water-electrolyte imbalances were rapidly compensated. Anticoagulant therapy was continued with low-molecular-weight heparins. The decompression of the obstruction and a deference of the surgery allowed imaging studies such as computed tomography or transrectal ultrasonography to be performed, to precisely stage the malignancy. Oral nutrition was started on the second postoperative day. Patients were discharged home 3 to 10 days after the procedure. The mean duration of hospitalization was 4.6 days.
The patients were re-admitted 14 to 20 days after the procedure in order to perform scheduled surgery. Such an approach permitted a one-step operation (Photo 3) to be performed with simultaneous resection of regional lymph nodes (Photo 4).
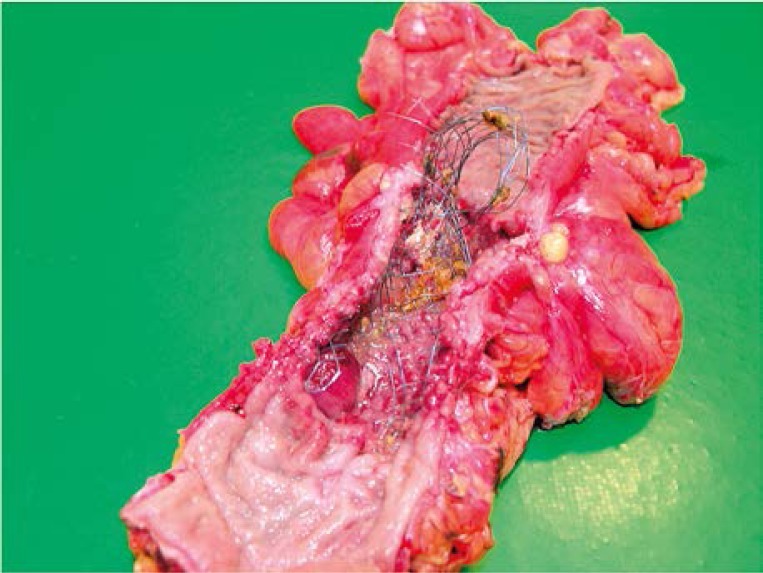
Photo 3.
Anterior resection of the rectum. Surgical specimen of the large intestine with carcinoma of the rectosigmoid junction which obstructed the intestine entirely. The patency was restored by endoscopic insertion of a self-expandable metal stent
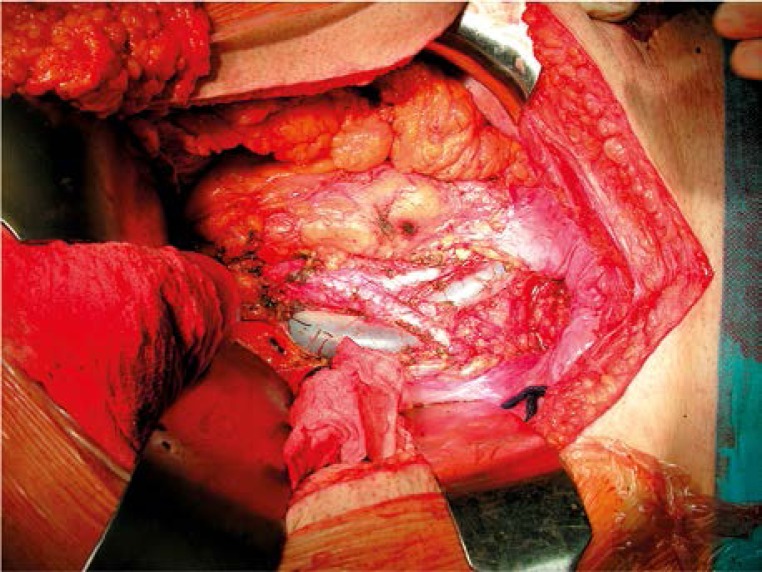
Photo 4.
Intraoperative image of the extent of the regional lymph node resection during the anterior resection of the rectum. Besides restoring patency, the endoscopically installed endoprosthesis was also helpful in preparing the intestine for a planned resection with extensive retroperitoneal periaortic lymph node removal
Liver metastases diagnosed during the computed tomography (CT) scan were synchronically removed in two patients. Detailed data on the extent of the performed surgery are presented in Table II.
One patient presenting with a resectable bifocal malignancy of the rectum did not consent to the surgical treatment.
None of the surgical patients developed hemostatic disorders intraoperatively. Non-severe postoperative complications, mostly infectious, were documented in 6 patients. Of these, 2 patients developed pneumonia and 3 individuals presented with surgical wound infections. An arrhythmia exacerbation was observed in 1 female patient, manifesting with hemodynamic symptoms.
Discussion
Approximately 30% of colorectal cancer patients present with an acute gastrointestinal tract obstruction. This requires an emergent surgical intervention due to the massive dilation of the intestine, associated with a risk of necrosis and perforation. Severe water-electrolyte imbalances and bacterial translocation markedly increase the postoperative morbidity rate. Prior to the implementation of surgical endoscopy, conservative treatment of lower digestive tract obstruction consisted of a trans-sphincteric insertion of Dennis’ catheter. Aside from endoscopic stenting, other less invasive techniques can be applied in order to restore patency in the case of non-resectable colorectal tumors. Partial ablation of the tumor can be achieved by means of laser coagulation, argon electrocoagulation, or alcoholic injections. Additionally, attempts are undertaken to dilate the obstruction using balloon, cryotherapy, and photodynamic therapy. However, the risk of tumor spread precludes the application of these modalities in patients with resectable tumors as well as in patients in whom the exact tumor stage is unknown.
The incidence of ischemic heart disease and colorectal cancer increases with population age. Asymptomatic development is a characteristic of gastrointestinal malignancies. Clinical symptoms appear no earlier than when the function of the affected organ is impaired by a growing tumor. Anemia belongs to the early signs of malignancy, and is not necessarily associated with tumor size. It results from chronic bleeding from the tumor and can develop as early as during the first stages of the disease. Progressive hypochromic anemia enhances myocardial ischemia, leading to an acute coronary insufficiency. Presently, the treatment of complicated ischemic heart disease is associated with a growing number of patients who require anticoagulant therapy. In patients in whom the ischemic heart disease co-exists with an acute malignant obstruction due to colorectal cancer, emergency surgery is associated with high risk of complications. Endoscopic stenting aimed at rapid decompression of the intestine and preparing the patient for a scheduled operation becomes the method of choice in this group. In our patient with a fresh myocardial infarct, restoring the intestinal patency by endoscopic stenting enabled the continuation of clopidogrel therapy until the epithelialization of the coronary stent was complete. Hematologists recommend discontinuing clopidogrel 7 days prior to scheduled surgery. However, some authors deny the necessity of clopidogrel therapy discontinuation [7]. Although the frequency of postoperative bleeding requiring transfusion was higher in patients who maintained a clopidogrel treatment as compared to those in whom the antiplatelet therapy was discontinued prior to surgery, these two groups did not differ in terms of hematocrit levels or the number of perioperative transfusions. Furthermore, no significant differences were observed in the duration of stay in the intensive care unit, duration of hospitalization, late morbidity rate, or all-cause mortality.
Endoscopic stenting constitutes an effective and safe treatment modality in acute malignant obstruction of the large intestine. Stent insertion was possible in all 21 patients included in this study, and enabled rapid decompression of the intestine. Many other authors report high effectiveness of this method [8–13]. The rate of successful stent insertions in malignant intestinal obstructions ranges between 64% and 100%. According to Athreya, the success rate of stenting in 102 patients with malignant obstruction of the large intestine was 85% [14]. In 80 patients, the intestinal patency was restored with the use of one prosthesis, while 7 required the installation of two prostheses. Crosta performed successful stenting in 23 out of 24 (95.8%) patients treated due to acute colorectal obstruction caused by a non-resectable malignancy [15]. During the early postoperative period, complications in the form of stent displacement were documented in only 2 patients.
The restoration of intestinal patency does not only allow for rapid compensation of metabolic disorders and nutritional status improvement; it also enables the continuation of further diagnostics in order to determine the stage of malignancy. Vitale et al. performed successful endoprosthesis implantations in 50 out of 57 colorectal cancer patients, which corresponds to 87.8% [16]. In 31 (62%) stented patients, the malignancy proved to be resectable. In 29 patients from this group (93.4%), preoperative colonoscopy was possible due to stent placement. It revealed a synchronous colorectal tumor in 3 individuals (9.6%), which influenced the extent of further resection.
Endoscopic stenting enables a planned one-stage radical operation. In the case of acute malignant obstruction, the mortality and morbidity rates after emergency colorectal resections, particularly those involving the left colon, are 23% and 50%, respectively [17]. In comparison, the mortality rate after a scheduled colorectal resection is lower than 5%. According to the available literature, the long-term survival of patients treated surgically after endoscopic stenting of an obstruction is shorter than in those who were treated surgically on an emergency basis, similar to the duration of recurrence-free survival [4]. In spite of these limitations, endoscopic stenting remains a valuable therapeutic modality enabling preparation of patients for radical colorectal surgery.
Conclusions
In the authors’ opinion, the preoperative endoscopic stenting of an acute malignant obstruction of the large intestine is a valuable therapeutic modality in the case of high-risk patients. It constitutes a safe and effective method to restore the digestive tract patency. This allows for rapid compensation of water-electrolyte imbalances, normalization of the clotting system, and an improvement of the cardiovascular and pulmonary capacity. Furthermore, the application of this method enables precise determination of the clinical stage of the malignancy. Finally, the preparation of the intestine for scheduled surgery is enabled and allows for one-stage radical surgical procedures.
References
- 1.Dohmoto M. New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endoscopia Digestiva. 1991;3:1507–12. [Google Scholar]
- 2.Baron TH. Colorectal stents. Tech Gastrointest Endosc. 2003;5:182–90. [Google Scholar]
- 3.Harris GJ, Senagore AJ, Lavery IC, Fazio VW. The management of neoplastic colorectal obstruction with colonic endolumenal stenting devices. Am J Surg. 2001;181:499–506. doi: 10.1016/s0002-9610(01)00622-5. [DOI] [PubMed] [Google Scholar]
- 4.Bonin EA, Baron TH. Update on the indications and use colonic stents. Curr Gastroenterol Rep. 2010;12:374–82. doi: 10.1007/s11894-010-0136-x. [DOI] [PubMed] [Google Scholar]
- 5.Samaraee AA, Fasih T, Hayat M. Use of self-expandable stents for obstructive distal and proximal large bowel cancer: a retrospective study in a single centre. J Gastrointest Canc. 2010;41:43–6. doi: 10.1007/s12029-009-9106-7. [DOI] [PubMed] [Google Scholar]
- 6.Carne PWG, Frye JNR, Robertson GM, Frizelle FA. Stents or open operation for palliation of colorectal cancer: a retrospective, cohort study of perioperative outcome and long term survival. Dis Colon Rectum. 2004;47:1455–61. doi: 10.1007/s10350-004-0624-x. [DOI] [PubMed] [Google Scholar]
- 7.Ozao-Choy J, Tammaro Y, Fradis M, et al. Clopidogrel and bleeding after general surgery procedures. Am Surg. 2008;74:721–5. [PubMed] [Google Scholar]
- 8.Li YD, Cheng YS, Li MH, et al. Management of acute malignant colorectal obstruction with a novel self-expanding metallic stent as a bridge to surgery. Eur J Radiol. 2010;73:566–71. doi: 10.1016/j.ejrad.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Branger F, Thibaudeau E, Mucci-Hennekinne S, et al. Management of acute malignant large bowel obstruction with self-expanding metal stent. Int J Colorectal Dis. 2010;25:1481–5. doi: 10.1007/s00384-010-1003-9. [DOI] [PubMed] [Google Scholar]
- 10.Song HY, Kim JH, Kim KR, et al. Malignant rectal obstruction within 5 cm of the anal verge: is there role for expandable metallic stent placement? Gastrointest Endosc. 2008;68:713–20. doi: 10.1016/j.gie.2007.12.051. [DOI] [PubMed] [Google Scholar]
- 11.Mauro MA, Koehler RE, Baron TH. Advances in gastrointestinal intervention: the treatment of gastroduodenal and colorectal obstructions with metallic stents. Radiology. 2000;215:659–69. doi: 10.1148/radiology.215.3.r00jn30659. [DOI] [PubMed] [Google Scholar]
- 12.Shin SJ, Kim TI, Kim BC, et al. Clinical application of self-expandable metallic stent for treatment of colorectal obstruction caused by extrinsic invasive tumors. Dis Colon Rectum. 2008;51:578–83. doi: 10.1007/s10350-008-9207-6. [DOI] [PubMed] [Google Scholar]
- 13.Lee KM, Shin SJ, Hwang JC, et al. Comparison of uncovered stent with covered stent for treatment of malignant colorectal obstruction. Gastrointest Endosc. 2007;66:931–5. doi: 10.1016/j.gie.2007.02.064. [DOI] [PubMed] [Google Scholar]
- 14.Athreya S, Moss J, Urquhart G, et al. Colorectal stentig for colonic obstruction: the indications, complications, effectiveness and outcome – 5 year review. EJR. 2006;60:91–4. doi: 10.1016/j.ejrad.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 15.Crosta C, Trovato C, Fiori G, et al. Metal sten placement in acute malignant colorectal obstruction. Dig Liver Dis. 2006;38:341–6. doi: 10.1016/j.dld.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Vitale MA, Villotti G, d'Alba L, et al. Preoperative colonoscopy after self-expandable metallic stent placement in patients with acute neoplastic colon obstruction. Gastrointest Endosc. 2006;63:814–9. doi: 10.1016/j.gie.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 17.Runkel NS, Schlag P, Schwarz V, Herfarth C. Outcome after emergency surgery for cancer of the large intestine. Br J Surg. 1991;78:183–8. doi: 10.1002/bjs.1800780216. [DOI] [PubMed] [Google Scholar]