Abstract
Purpose
Role of intravitreal injection of dexamethasone implant (Ozurdex) for refractory macular thickening.
Methods
A case report of a 13-year-old boy with Rhodopsin-positive, CRB1-negative retinitis pigmentosa presenting with Coat's-like exudative vitreoretinopathy and treatment-resistant cystoid macular oedema.
Results
A reduction in the macular thickening following a single injection of Ozurdex.
Conclusion
We present our experience in successful treatment of refractory macular oedema with intravitreal injection of dexamethasone implant resulting in clinically significant resolution of macular thickening.
Keywords: Coat's disease, retinitis pigmentosa, rhodopsin, Ozurdex
Introduction
Coat's-like retinal telangiectatic, neovascular, and exudative changes represent an atypical presentation of retinitis pigmentosa (RP). Prevalence of this atypical form of RP has been documented to be 1–4%.1, 2, 3 The management of exudation and neovascular changes in these patients with RP poses significant challenges in the treatment, as the exudation tends to recur and become refractory to any treatment modality.
Purpose
We present the successful management of refractory macular oedema in a 13-year-old boy with a known diagnosis of autosomal dominant RP with Coat's-like exudative vitreoretinopathy. We report changes in the central macular thickness (CMT) and visual acuity (VA) with 0.7 mg of intravitreal injection of dexamethasone implant in the right eye.
Materials and methods
This is a follow-up of the case report published in the June 2011 edition of the journal ‘Eye'.4 Cystoid macular oedema (CMO) was treated previously with daily 500 mg of acetazolamide for 3 months. There was no significant improvement. Similarly, neither dorzolamide hydrochloride drops nor the orbital floor injection of Depo-Medrone (40 mg) was effective. He was subsequently treated with intravitreal anti-vascular endothelial growth factor agent, bevacizumab and then with intravitreal injection of triamcinolone acetonide with limited success.5 The effect of cryotherapy was reported previously.4
Following the initial report, the patient had recurrence of CMO. With continued thickening of the macula and drop in VA in the right eye, he was treated with a 0.7 mg of intravitreal injection of dexamethasone implant (Ozurdex, Allergan Inc., Irvine, CA, USA).
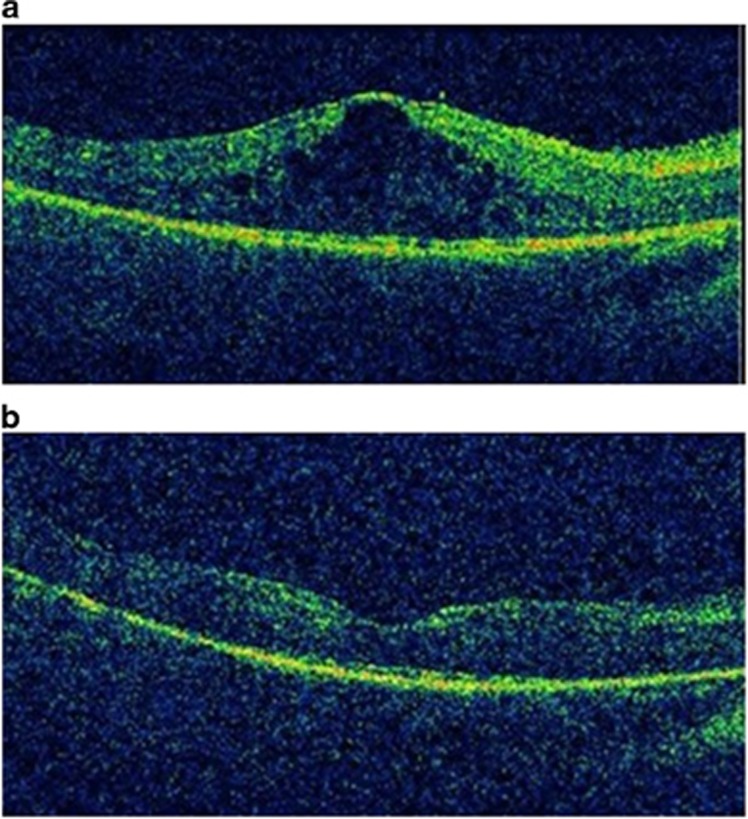
At present, VA was 1.01 logMAR OD and 0.24 logMAR OS. In the right eye, he had posterior subcapsular cataract and a fundus examination revealed telangiectasia with sub-retinal exudation in the peripapillary area and inferior retina. He also had significant CMO in the same eye. His intraocular pressure was 12 mm Hg and the optical coherence tomography (OCT) of the macula showed a CMT of 559 microns (Figure 1a). Fundus and OCT were unremarkable in the left eye.
Figure 1.
(a) Right eye: 3D-OCT before Ozurdex implantation demonstrates CMO. (b) Right eye: 3D-OCT, 6 weeks after Ozurdex implantation demonstrating resolved CMO. Scan quality is limited due to cataract.
Results
Both the patient and his father were confirmed to have a known pathogenic mutation for RP, Rho c.557C>G (p.Ser186Trp).6 Crumbs homologue 1 (CRB1)-mutation testing was negative. However his father did not have Coat's-like exudative vitreoretinopathy. Six weeks after the intravitreal dexamethasone implantation, he was reviewed and was found to have a vision of 0.89 in the right eye. His IOP was 17 mm Hg. A fundus examination showed minimal vitreous haze and resolving macular oedema. The exudation at the disc and the inferior retina had resolved. The CMT was 271 microns (Figure 1b). Improved CMT and VA were maintained at last visit 10 months later.
Discussion
Various other treatment modalities have been reported such as acetozolamide, vitrectomy, buckling, drainage of sub-retinal fluid, cryotherapy, endolaser photocoagulation, and silicone oil tamponade but with limited and transient success.7, 8
We hypothesised that the CMO developed in this patient because of non-VEGF-driven inflammation generated by Coats'-like exudation. This hypothesis is supported by the lack of improvement with an anti-vascular endothelial growth factor drug (Bevacizumab) and the immediate improvement with an intravitreal injection of a dexamethasone implant. There was no increase in the severity of the Coat's disease; hence we presume the recurrence of macular oedema is spontaneous and subject to the natural history of the condition. Cryotherapy augmentation was not considered in view of minimal exudation contrary to our earlier report where he had an exudative RD.
Vision did not recover completely in the right eye due to the co-existing posterior subcapsular cataract. There is no recurrence of macular oedema at 10 months follow-up. There is one other report of an adult Coat's disease treated with a combination of dexamethasone implant and retinal photocoagulation.9 The current communication is the first report of use of Ozurdex per se in the paediatric age group for the treatment of CMO in RP. It is also the first report of a rhodopsin mutation presenting with Coat's-like exudation. All previous reported cases have been associated with mutations in CRB1.10 Further studies are required to confirm the efficacy of the dexamethasone intravitreal implant in this rare condition.
Acknowledgments
We thank Dr DO Robinson, deputy head of Molecular Genetics, Wessex Regional Genetics Laboratory, Salisbury, UK for assistance with the genetic work.
The authors declare no conflict of interest.
References
- Kajiwara Y. Ocular complications of retinitis pigmentosa. Association with Coat's syndrome. Jpn J Clin Ophthalmol. 1980;34:947–955. [Google Scholar]
- Pruett RC. Retinitis pigmentosa: clinical observations and correlations. Trans Am Ophthalmol Soc. 1983;81:693–735. [PMC free article] [PubMed] [Google Scholar]
- Khan JA, Ide CH, Strickland MP. Coat's-type retinitis pigmentosa. Surv Ophthalmol. 1988;32 (5:317–332. doi: 10.1016/0039-6257(88)90094-x. [DOI] [PubMed] [Google Scholar]
- De Salvo G, Gemenetzi M, Luff AJ, Lotery AJ. Cystoid macular oedema successfully treated by cryotherapy in retinitis pigmentosa with Coats'-like retinal exudation. Eye (Lond) 2011;25 (6:821–822. doi: 10.1038/eye.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramasubramanian A, Shields CL. Bevacizumab for Coats' disease with exudative retinal detachment and risk of vitreoretinal traction. Br J Ophthalmol. 2012;96 (3:356–359. doi: 10.1136/bjophthalmol-2011-300141. [DOI] [PubMed] [Google Scholar]
- Matias-Florentino M, Ayala-Ramirez R, Graue-Wiechers F, Zenteno JC. Molecular screening of rhodopsin and peripherin/RDS genes in Mexican families with autosomal dominant retinitis pigmentosa. Curr Eye Res. 2009;34 (12:1050–1056. doi: 10.3109/02713680903283169. [DOI] [PubMed] [Google Scholar]
- Lee SY, Yoon YH. Pars plana vitrectomy for exuduative retinal detachment in coats-type retinitis pigmentosa. Retina. 2004;24 (3:450–452. doi: 10.1097/00006982-200406000-00017. [DOI] [PubMed] [Google Scholar]
- Tamura H, Miyamoto K, Kiryu J, Miyahara S, Katsuta H, Hirose F, et al. Intravitreal injection of corticosteroid attenuates leukostasis and vascular leakage in experimental diabetic retina. Invest Ophthalmol Vis Sci. 2005;46:1440–1444. doi: 10.1167/iovs.04-0905. [DOI] [PubMed] [Google Scholar]
- Martínez-Castillo S, Gallego-Pinazo R, Dolz-Marco R, Marín-Lambíes C, Díaz-Llopis. M. Adult Coats' disease successfully managed with the dexamethasone intravitreal implant (ozurdex®) combined with retinal photocoagulation. Case Rep Ophthalmol. 2012;3 (1:123–127. doi: 10.1159/000337481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Hollander AI, Heckenlively JR, van den Born LI, de Kok YJ, van der Velde-Visser SD, Kellner U, et al. Leber congenital amaurosis and retinitis pigmentosa with Coats-like exudative vasculopathy are associated with mutations in the Crumbs homologue 1 (CRB1) gene. Am J Hum Genet. 2001;69:198–203. doi: 10.1086/321263. [DOI] [PMC free article] [PubMed] [Google Scholar]