Abstract
Objectives. We assessed associations between activity and hip fracture in men.
Methods. The Health Professionals Follow-up Study reported time spent walking, sitting, and in 10 other discretionary activities every 2 years in 35 996 men aged 50 years and older from 1986 to 2010. We calculated hazard ratios (HRs) for risk of hip fracture by amount of activity and sitting in Cox proportional hazards models, adjusted for age, body mass index, smoking, medication use, disease diagnoses, and diet.
Results. Over 24 years, participants reported 490 low-trauma hip fractures. Energy expenditure from all activities was weakly associated with lower risk of fracture. More walking time, with little other exercise, lowered risk by 43% (HR = 0.57; 95% confidence interval [CI] = 0.39, 0.83 for ≥ 4 vs < 1 hours/week), and risk decreased linearly with more frequent walking (P < .001). Brisk (vs leisurely) pace lowered risk by 47%. Sitting lowered risk (HR = 0.62; 95% CI = 0.43, 0.89 for ≥ 50 vs < 20 hours/week), primarily among those who also walked for exercise. We observed no benefit of strenuous activity.
Conclusions. Walking is a relatively safe and easy activity for hip fracture prevention.
Most research on osteoporosis and hip fractures has been conducted in older women; the occurrence in men is much lower because of their greater bone size and shorter life span and because they do not experience a precipitous decrease in endogenous sex hormones analogous to menopause. Although only about one third of the hip fractures in the United States occur in men,1 subsequent morbidity and mortality is greater than in women.2 Alcohol abuse, glucocorticoid excess, and hypogonadism are established risk factors for decreased bone health in men,3 but less is known about lifestyle influences. In particular, the effect of physical activity on hip fracture risk may differ by gender because men have more lean body mass and greater bone mineral density at the hip than women of comparable size.4
Evidence from epidemiological studies suggests that active adults can reduce their risk of hip fracture by 20% to 60% from that of sedentary adults.5,6 However, the type, frequency, intensity, and duration of activity required for adult bone health are not well defined. Also, more research specific for men is needed because results from previous studies conducted with large mixed-gender populations were highly influenced by the predominance of hip fractures in women. Studies that have focused on men tend to demonstrate a similar benefit from activity to that found for women,7–14 although small sample sizes, crude measures of activity, and baseline assessments applied to long periods of follow-up limit the strength and detail of these results.
We examined discretionary physical activity and inactivity assessed every 2 years in relation to risk of hip fracture among men aged 50 years and older over 24 years of follow-up in the Health Professionals Follow-up Study. We previously reported that total activity, and walking in particular, were associated with a lower risk of hip fracture in postmenopausal women in the Nurses’ Health Study,15 results derived from a similar activity assessment.
METHODS
At baseline, beginning in January 1986, the Health Professionals Follow-up Study enrolled 51 529 male health professionals aged 40 years and older, living across the United States. On the initial questionnaire, participants provided a medical history and information on lifestyle and risk factors related to cancer, heart disease, and other medical conditions. The study mailed follow-up questionnaires every 2 years to update individual characteristics and to identify incident diagnoses. Each biennial questionnaire assessed time spent in recreational and outdoor activities; time spent sitting was added in 1990. The study ascertained deaths from family members, the postal service, and the National Death Index.16,17
We followed the study population from 1986 to 2010. At baseline, men who were aged 50 to 75 years entered the analysis. Younger men entered when they reached age 50 years. We excluded participants at entry if they did not report their activity on the most recent assessment; had reported a previous hip fracture or a diagnosis of osteoporosis, cancer, heart disease, or stroke; were unable to climb a flight of stairs; or had difficulty with balance or activities of daily living. We excluded men of African American or Asian ancestry (< 3% of the cohort) because of differing fracture risks. The final study population comprised 35 996 men.
Each biennial questionnaire asked participants to report all hip fractures, with the date of occurrence and a description of the circumstances. As health professionals, cohort members were capable of accurately reporting these events.18 Over the 24 years of follow-up, participants reported 546 hip fractures. We did not include fractures attributable to malignancy or major traumatic events (e.g., motor vehicle accidents, skiing) as cases, leaving 490 hip fractures for analysis. Eighty-five percent of these fractures occurred when slipping, tripping, falling from the height of a chair, or another similar low-trauma event. The mean age at hip fracture was 77 years (range = 51–96 years). Kaplan-Meier plots of the cumulative incidence of hip fracture over age and over study follow-up are in Figure A (available as a supplement to this article at http://www.ajph.org).
Physical Activity and Inactivity
Each biennial questionnaire assessed physical activity as the average time per week spent during the past year in specific recreational and outdoor activities. The initial assessment in 1986 listed 8 activities: walking, jogging, running (≤ 10 minutes/mile), bicycling, calisthenics or exercise machines, tennis, racquetball or squash, and lap swimming. Questionnaires added heavy outdoor work in 1988, weight lifting in 1990, and moderate outdoor work in 2004. Each activity had a choice of 11 categories, ranging from zero to 11 or more hours per week. Participants also reported their usual walking pace as easy, average, or brisk (< 2, 2–2.9, or ≥ 3 mph) and the number of flights of stairs climbed daily.
For each activity on the questionnaire we assigned a metabolic equivalent (MET) score,19 which is the metabolic rate associated with that activity calculated in comparison with resting rate. Scores for activities in the list ranged from 2 METs for walking at an easy pace to 7 METs for jogging and 12 for running. We calculated energy expenditure for each activity as the MET score multiplied by the reported hours spent per week (MET-h/wk). We calculated energy expenditure from walking using a MET score based on walking pace. We determined total discretionary physical activity from the sum of the energy expenditure from all individual activities. As the number of activities on the questionnaire increased over time, total activity also increased. To account for this, we analyzed the data with quintiles specific for each questionnaire. We examined intensity of activity with separate analyses of walking, running and jogging combined, and strenuous activity, which incorporated activities with a MET score of 6 or higher (i.e., running, jogging, biking, swimming, tennis, racquetball or squash, and calisthenics or exercise machines).
We evaluated the ability of the questionnaire to assess total activity over the previous year in 238 participants.20 Compared with 4 week-long diaries collected seasonally, correlations were 0.58 for strenuous activity and 0.40 for walking. In addition, the correlation between strenuous activity and resting pulse was −0.45. The physical activity questionnaire has been shown to predict coronary heart disease,21 diabetes,22 and colon cancer23 in this cohort.
To assess inactivity, the study added sitting to the biennial questionnaires beginning in 1990, with 6 separate questions for time spent sitting while at work; riding in a car, bus, or train; and at home while watching TV, reading, on the computer, or other sedentary situation. Response options offered 13 duration categories, with a maximum of 40 or more hours per week, for reporting each sitting situation. Total weekly time spent sitting was a sum of the 6 reports. Sitting, in particular TV watching, has been shown to predict type 2 diabetes in this cohort.24
Diet and Nondiet Measures
The study assessed diet every 4 years with a food-frequency questionnaire, on which participants reported their frequency of consumption over the previous year for specified amounts of more than 130 foods. We calculated nutrient intakes from the reported food frequencies and use of multivitamins and nutrient supplements. In validation studies, the food frequency questionnaire has been shown to be a suitable instrument for discriminating between levels of dietary intakes.25,26
All biennial questionnaires assessed body weight; smoking status and number of cigarettes smoked per day; current use of thiazide diuretics, furosemide-like diuretics, and oral steroids; and diagnoses of osteoporosis, cancer, heart disease, stroke, and diabetes. We calculated body mass index (BMI; defined as weight in kilograms divided by height in meters squared) from current weight and height reported at the 1986 baseline. Most biennial questionnaires assessed difficulty climbing a flight of stairs and difficulty with balance.
Statistical Analysis
Each participant contributed person-time from the return date of the 1986 baseline questionnaire or the questionnaire at which he first reached 50 years of age and was censored at the date of hip fracture or death, his last questionnaire response, or the end of follow-up on January 1, 2010. We used Cox proportional hazards models to compute hazard ratios (HRs) with 95% confidence intervals (CIs) for risk of hip fracture within categories of each exposure compared with a low reference group. We conditioned the models on months of age and questionnaire cycle to account for age and time. We calculated multivariable HRs from models adjusted simultaneously for all assessed risk factors for hip fracture, which we entered into the models as time-dependent covariates updated with each 2-year questionnaire cycle.
To best examine long-term activity and inactivity after age 50 years, we used cumulatively averaged measures; that is, at the beginning of each cycle, we averaged the current assessment with all previous measures. To calculate a dose–response effect, we derived a P value for linear trend (Ptrend) from median values per decile of total activity and continuous values of walking, strenuous activity, running and jogging, and sitting. We calculated multiplicative interaction between exposures with the Wald test for continuous data (Pinteraction). We set significance at P < .05.
RESULTS
Age-adjusted characteristics of the study population of men aged 50 years and older at their entry into analysis are shown by levels of total discretionary physical activity and sitting in Table 1. Time spent sitting was not associated with total activity (r = 0.03). BMI was higher on average in men with lower activity (r = −0.15) but was not associated with sitting. Dietary intakes were similar across all levels of activity and sitting. Although the smoking rate in this cohort was low, men with the lowest activity were more likely to smoke. Over follow-up, 4% of participants reported a diagnosis of osteoporosis (mean age = 74 years).
TABLE 1—
Age and Age-Adjusted Characteristics Among Men Aged ≥ 50 Years at Entry Into Analysis, by Levels of Total Discretionary Physical Activity and Sitting: Health Professionals Follow-up Study, United States
| Total Weekly Activitya |
Total Weekly Sitting |
|||||
| Characteristics | Quintile 1, Mean or % | Quintile 3, Mean or % | Quintile 5, Mean or % | < 20 Hours, Mean or % | 30–39 Hours, Mean or % | ≥ 50 Hours, Mean or % |
| Age, y | 56.7 | 57.4 | 56.6 | 61.0 | 58.7 | 57.0 |
| Activity | ||||||
| Total,a MET-h/wk | 6.0 | 26.6 | 74.8 | 31.3 | 34.7 | 33.0 |
| Walking, h/wk | 0.5 | 2.0 | 5.2 | 2.5 | 2.9 | 2.9 |
| Strenuous,b h/wk | 0.1 | 0.9 | 4.8 | 1.8 | 1.9 | 1.7 |
| Running and jogging, h/wk | 0.0 | 0.2 | 1.3 | 0.5 | 0.5 | 0.4 |
| Sitting, h/wk | ||||||
| Total | 33.6 | 34.9 | 35.0 | 11.8 | 34.5 | 62.1 |
| While watching TV | 3.0 | 2.6 | 2.6 | 4.8 | 10.9 | 15.3 |
| BMI, kg/m2 | 26.4 | 25.7 | 25.0 | 25.6 | 25.6 | 25.7 |
| Height, cm | 178 | 178 | 179 | 178 | 178 | 178 |
| Dietary intake/d | ||||||
| Calcium,c mg | 883 | 910 | 937 | 917 | 916 | 909 |
| Vitamin D,c μg | 9.8 | 10.5 | 11.1 | 10.8 | 10.8 | 10.5 |
| Retinol,c μg | 1504 | 1603 | 1659 | 1581 | 1509 | 1467 |
| Vitamin K,c mg | 168 | 187 | 203 | 196 | 181 | 181 |
| Protein,c g | 91 | 92 | 92 | 92 | 91 | 91 |
| Caffeine, mg | 258 | 227 | 215 | 224 | 229 | 235 |
| Alcohol, g | 11.2 | 11.5 | 12.3 | 10.4 | 11.4 | 12.0 |
| Cigarette smoker | 13 | 8 | 6 | 8 | 6 | 7 |
| Multivitamin user | 40 | 45 | 46 | 41 | 42 | 41 |
| Calcium supplement user | 14 | 16 | 18 | 11 | 13 | 12 |
| Thiazide diuretic user | 10 | 9 | 7 | 6 | 5 | 6 |
Note. BMI = body mass index; MET-h/wk = metabolic equivalent hours per week.
From recreational and outdoor activities.
Running and jogging, biking, swimming, tennis, racquetball or squash, and calisthenics or exercise machines.
Intake from foods and supplements, adjusted for total energy intake.
Total discretionary physical activity was inversely associated with risk of hip fracture in a simple model adjusted only for age and questionnaire cycle (Ptrend = .03; Table 2). However, the linear association was attenuated after adjustment for all other risk factors (Ptrend = .10). In the categorical analysis, the HR for hip fracture in the highest versus lowest quintile of total activity was 0.83 (95% CI = 0.62, 1.11), with similarly lower HRs in all quintiles above the reference group.
TABLE 2—
Risk of Hip Fracture Among Men Aged ≥ 50 Years, by Total and Types of Discretionary Physical Activity: Health Professionals Follow-up Study, United States, 1986–2010
| Variable | Hip Fractures, No. | Person-Yearsa | Simple Model,b HR (95% CI) | Multivariable Model,c HR (95% CI) |
| Total activityd,e | ||||
| Quintile 1 | 121 | 126.7 | 1.00 (Ref) | 1.00 (Ref) |
| Quintile 2 | 99 | 129.4 | 0.82 (0.63, 1.08) | 0.85 (0.65, 1.13) |
| Quintile 3 | 98 | 128.9 | 0.81 (0.62, 1.07) | 0.85 (0.64, 1.13) |
| Quintile 4 | 81 | 128.6 | 0.69 (0.51, 0.92) | 0.71 (0.53, 0.96) |
| Quintile 5 | 91 | 128.6 | 0.78 (0.59, 1.03) | 0.83 (0.62, 1.11) |
| Ptrendf | .03 | .1 | ||
| Walking,e h/wk | ||||
| < 1.0 | 114 | 171.8 | 1.00 (Ref) | 1.00 (Ref) |
| 1.0–1.9 | 98 | 143.1 | 0.85 (0.64, 1.12) | 0.85 (0.64, 1.13) |
| 2.0–2.9 | 82 | 98.0 | 0.94 (0.70, 1.26) | 0.98 (0.73, 1.32) |
| 3.0–3.9 | 71 | 62.4 | 1.00 (0.74, 1.36) | 1.01 (0.73, 1.38) |
| 4.0–5.9 | 66 | 80.6 | 0.75 (0.55, 1.02) | 0.73 (0.53, 1.01) |
| ≥ 6.0 | 59 | 86.4 | 0.54 (0.39, 0.74) | 0.56 (0.40, 0.79) |
| Ptrendf | <.001 | <.001 | ||
| Walking pace,g mph | ||||
| < 2 | 96 | 39.4 | 1.00 (Ref) | 1.00 (Ref) |
| 2 | 229 | 287.6 | 0.52 (0.41, 0.67) | 0.59 (0.45, 0.77) |
| ≥ 3 | 137 | 267.2 | 0.46 (0.35, 0.61) | 0.53 (0.39, 0.72) |
| Strenuous activity,e,h h/wk | ||||
| None | 87 | 133.7 | 1.00 (Ref) | 1.00 (Ref) |
| < 1.0 | 191 | 204.4 | 1.06 (0.81, 1.38) | 1.07 (0.82, 1.41) |
| 1.0–1.9 | 90 | 108.6 | 1.11 (0.81, 1.51) | 1.13 (0.82, 1.56) |
| 2.0–2.9 | 39 | 68.1 | 0.83 (0.56, 1.22) | 0.85 (0.57, 1.27) |
| 3.0–3.9 | 28 | 39.9 | 0.93 (0.60, 1.44) | 1.03 (0.65, 1.61) |
| ≥ 4.0 | 55 | 87.6 | 0.94 (0.66, 1.33) | 1.04 (0.72, 1.50) |
| Ptrendf | .25 | .6 | ||
| Running and jogging,e h/wk | ||||
| None | 329 | 392.0 | 1.00 (Ref) | 1.00 (Ref) |
| < 0.5 | 96 | 123.5 | 0.79 (0.62, 1.00) | 0.85 (0.67, 1.08) |
| 0.5–0.9 | 27 | 41.0 | 0.89 (0.59, 1.33) | 1.02 (0.68, 1.53) |
| 1.0–1.9 | 19 | 43.3 | 0.73 (0.45, 1.17) | 0.78 (0.48, 1.27) |
| ≥ 2.0 | 19 | 42.4 | 0.87 (0.54, 1.41) | 0.97 (0.60, 1.58) |
| Ptrendf | .72 | .98 |
Note. CI = confidence interval; HR = hazard ratio; MET-h/wk = metabolic equivalent hours per week.
In thousands.
Adjusted for age and questionnaire cycle.
Adjusted for age; questionnaire cycle; body mass index; height; smoking status; use of furosemide diuretics, thiazide diuretics, and oral steroids; incident diagnoses of osteoporosis, cancer, heart disease, stroke, and diabetes; and intake of calcium, vitamin D, retinol, protein, vitamin K, caffeine, and alcohol. In addition, walking and strenuous activity were adjusted for one another, walking pace was adjusted for walking h/wk, and running and jogging were adjusted for other activities.
Median MET-h/wk of total activity per quintile were quintile 1, 5.9; quintile 2, 15.7; quintile 3, 26.1; quintile 4, 40.2; quintile 5, 69.5.
Cumulatively averaged over follow-up.
For linear trend over median values/decile of total activity and over continuous values of walking, strenuous activity, and running and jogging.
Analysis of walking pace excluded men who reported zero time spent walking.
Running, jogging, biking, swimming, tennis, racquetball or squash, and calisthenics or exercise machines.
Walking was the most popular activity in this cohort and contributed 37% of the total MET hours per week over follow-up. More time spent walking was associated with a significant linear decrease in risk of hip fracture (Ptrend < .001) even after we controlled for strenuous activity and all other risk factors (Table 2). In the categorical analysis, risk was 44% lower in men who walked 6 hours or more than in men who walked less than 1 hour per week (HR = 0.56; 95% CI = 0.40, 0.79). To better focus on walking, we limited the analysis to men who spent less than 1 hour per week in strenuous activity and found a strong inverse association between 4 or more hours per week of walking and risk of hip fracture (HR = 0.57; 95% CI = 0.39, 0.83; Ptrend < .001), with a weaker association in men with more frequent strenuous activity (HR = 0.76; 95% CI = 0.49, 1.17; Ptrend = 0.13). A faster walking pace was independently associated with significantly lower risk of hip fracture. Risk was 41% lower for average and 47% lower for brisk pace than for easy pace in a multivariable model that included time spent walking. When we examined duration and pace together, men who walked at a brisk pace for 4 or more hours per week had a 62% lower risk of hip fracture than those who walked less than 4 hours per week at an easy pace (HR = 0.38; 95% CI = 0.26, 0.56).
In contrast to walking, more time spent in strenuous activity did not reduce risk of hip fracture (HR = 1.04; 95% CI = 0.72, 1.50 for ≥ 4 hours/week vs none; Table 2). Running and jogging in particular were also not associated with hip fracture risk (HR = 0.97; 95% CI = 0.60, 1.58 for ≥ 2 hours/week vs none).
We excluded men from entering our analysis if they had previously reported difficulty with balance or climbing a flight of stairs. We did not include incident reports in the statistical models because they appeared to be intermediate variables on the pathway between activity and hip fracture. Specifically, men in the lowest quintile of total activity had a significant 39% higher risk of developing difficulty with stairs or balance than men in the highest quintile, and men who reported difficulty with stairs or balance had a significant 68% higher risk of hip fracture than those without either difficulty. Consistent with their role as intermediate variables, difficulty with balance and climbing a flight of stairs greatly attenuated the association between total activity and hip fracture when added to the multivariable model (HR = 0.94; 95% CI = 0.70, 1.26 for the highest vs lowest quintile, Ptrend = .35).
More time spent sitting was associated with a lower risk of hip fracture even after adjustment for total activity and all other risk factors (Table 3). Risk was a significant 38% lower in men who sat for 50 or more hours per week than in men who sat for less than 20 hours (HR = 0.62; 95% CI = 0.43, 0.89), with a linear trend in decreasing risk with more frequent sitting (Ptrend = .03). Because sitting while watching TV has been particularly predictive of chronic diseases in this cohort, we examined it separately and found that it was inversely associated with risk of hip fracture (HR = 0.69; 95% CI = 0.48, 0.98 for ≥ 15 vs < 3 hours/week; Ptrend = .04). We observed no association for any other sitting situations (HR = 0.95; 95% CI = 0.67, 1.35 for ≥ 36 vs < 12 hours/week).
TABLE 3—
Risk of Hip Fracture Among Men Aged ≥ 50 Years, by Hours of Sitting per Week: Health Professionals Follow-up Study, United States, 1990–2010
| Variable | Cases, No. | Person-Yearsa | Simple Model,b HR (95% CI) | Multivariable Model,c HR (95% CI) |
| Total sitting,d h/wk | ||||
| < 20 | 132 | 101.2 | 1.00 (Ref) | 1.00 (Ref) |
| 20–29 | 108 | 118.4 | 0.78 (0.60, 1.01) | 0.78 (0.59, 1.02) |
| 30–39 | 106 | 123.1 | 0.80 (0.61, 1.04) | 0.81 (0.62, 1.06) |
| 40–49 | 67 | 94.3 | 0.73 (0.54, 1.00) | 0.76 (0.56, 1.04) |
| ≥ 50 | 43 | 85.7 | 0.63 (0.44, 0.90) | 0.62 (0.43, 0.89) |
| Ptrende | .02 | .03 | ||
| Watching TV,d h/wk | ||||
| < 3 | 67 | 74.7 | 1.00 (Ref) | 1.00 (Ref) |
| 3–5 | 106 | 109.5 | 0.93 (0.67, 1.27) | 0.99 (0.71, 1.37) |
| 6–8 | 88 | 105.6 | 0.80 (0.57, 1.10) | 0.85 (0.61, 1.19) |
| 9–14 | 113 | 118.3 | 0.79 (0.58, 1.08) | 0.87 (0.63, 1.21) |
| ≥ 15 | 82 | 114.7 | 0.63 (0.45, 0.88) | 0.69 (0.48, 0.98) |
| Ptrende | .01 | .04 | ||
| Other sitting,d h/wk | ||||
| < 12 | 122 | 97.0 | 1.00 (Ref) | 1.00 (Ref) |
| 12–18 | 116 | 103.5 | 0.93 (0.71, 1.20) | 1.00 (0.77, 1.32) |
| 19–26 | 93 | 115.4 | 0.74 (0.55, 0.97) | 0.79 (0.59, 1.06) |
| 27–35 | 69 | 103.0 | 0.70 (0.51, 0.96) | 0.80 (0.57, 1.10) |
| ≥ 36 | 56 | 103.8 | 0.84 (0.60, 1.17) | 0.95 (0.67, 1.35) |
| Ptrende | .13 | .54 |
Note. CI = confidence interval; HR = hazard ratio.
In thousands.
Adjusted for age and questionnaire cycle.
Adjusted for age; questionnaire cycle; total activity; body mass index; height; smoking status; use of furosemide diuretics, thiazide diuretics, and oral steroids; incident diagnoses of osteoporosis, cancer, heart disease, stroke, and diabetes; and intake of calcium, vitamin D, retinol, protein, vitamin K, caffeine, and alcohol. In addition, sitting watching TV and other sitting were adjusted for one another.
Cumulatively averaged over follow-up.
For linear trend over continuous hours of sitting.
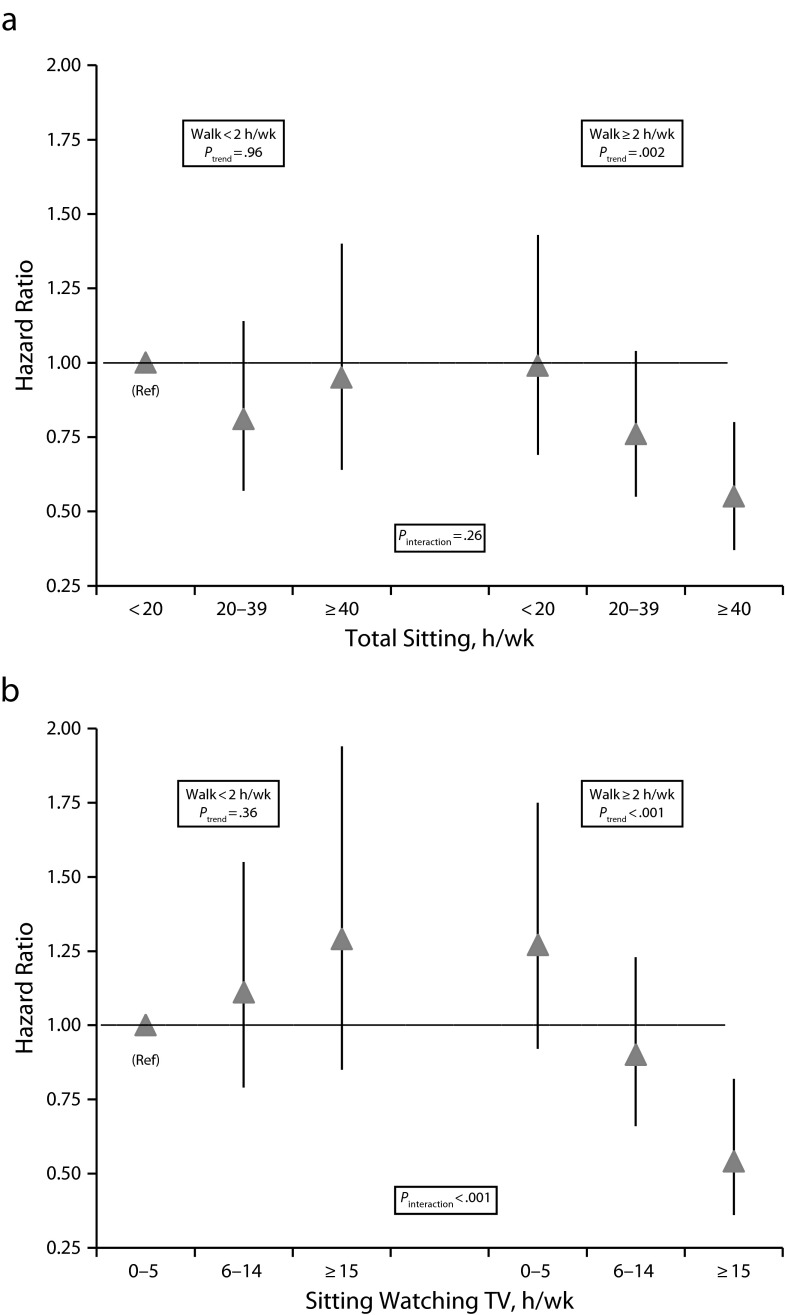
To better determine the effect of activity on the association between sitting and hip fracture, we cross-classified sitting by median time spent walking, because walking was the activity most predictive of fracture (Figure 1). Participants in the highest sitting category (≥ 40 hours/week) had a significant 45% lower risk of hip fracture than men in the lowest sitting (< 20 hours/week) and lower walking (< 2 hours/week) categories if they also walked for 2 or more hours per week (HR = 0.55; 95% CI = 0.37, 0.80) but not if they did less walking (relative risk = 0.95; 95% CI = 0.64, 1.20). Results were similar and stronger when we cross-classified time spent sitting while watching TV with walking (Pinteraction < .001).
FIGURE 1—
Risk of hip fracture by (a) total sitting and (b) sitting watching TV, cross-classified with median time spent walking: Health Professionals Follow-up Study, United States, 1990–2010.
Note. In (a) and (b) triangles denote the hazard ratio; vertical lines denote the 95% confidence interval. Ptrend is for linear trend over continuous values of sitting within categories of walking. Pinteraction is for multiplicative interaction between continuous values of sitting and walking. Models were adjusted for age; questionnaire cycle; body mass index; height; smoking status; use of furosemide diuretics, thiazide diuretics, and oral steroids; incident diagnoses of osteoporosis, cancer, heart disease, stroke, and diabetes; and intakes of calcium, vitamin D, retinol, protein, vitamin K, caffeine, and alcohol. In addition, sitting watching TV was adjusted for other time spent sitting.
For each of the activity and inactivity exposures, we checked for interaction with age, BMI, smoking, alcohol consumption, and calcium and vitamin D intake, but found no significant results (all, Pinteraction > .05). Despite lack of significant interaction, we observed a significant inverse association between total activity and risk of hip fractures in men aged 77 years or older (HR = 0.59; 95% CI = 0.38, 0.92 for highest vs lowest quintile; Ptrend = .02) but not in men younger than 77 years (HR = 1.11; 95% CI = 0.75, 1.65; Ptrend = .96). However, this may be partially explained by the fact that walking accounted for about half of the energy expenditure in the highest quintile of total activity in the older men, whereas strenuous activity was the much larger contributor to the highest quintile in the younger men. The association between walking and hip fractures was inverse in both the younger (Ptrend = .02) and older (Ptrend = .002) men.
DISCUSSION
In our 24-year analysis of discretionary physical activity in men aged 50 years and older, energy expenditure from all activities was weakly associated with decreased risk of hip fracture. However, for men whose primary activity was walking, 4 or more hours per week was associated with a significant 43% lower risk than walking less than 1 hour. This is very similar to the 41% lower risk we previously reported for postmenopausal women.15 Unlike in the men, total activity in women also demonstrated a significant inverse association. This may be because walking was the major activity in women: 66% of women's total energy expenditure and only 37% of men's came from walking. We did not observe any association between strenuous activity or running and jogging and risk of hip fractures in men. Although strenuous activity increases muscle strength, and impact from running and jogging in particular improves bone density, these activities are also associated with a higher risk of falling,5 which may offset the benefits. On the other hand, most middle-aged and elderly men in our sample did little running and jogging, making it difficult to observe a possible benefit.
Regular physical activity may work in several ways to prevent hip fractures. Most hip fractures result from a fall,27 and clinical trials have demonstrated that regular activity can reduce fall occurrence28,29 through improvement in muscle strength30,31 and balance.32,33 Site-specific weight-bearing exercise and resistance training can also reduce hip fracture risk by increasing the mechanical load on bone, which promotes remodeling and an increase in density.34,35
In general, prospective studies have reported lower risks of hip fracture in active than in inactive middle-aged and older men despite limitations of crude or single-activity assessments. In Norway, sedentary men had a significant 150% greater risk of hip fracture than those who participated in recreational sports at least 3 hours per week,12 and in Denmark, risk was 25% lower in participants with 2 or more hours per week of moderate activity than in sedentary men.11 Both studies assessed activity with a simple 4-level activity scale; therefore, details of type and intensity could not be examined. A US study reported a significant 49% lower risk in men who engaged in active exercise for 1 or more hours per day than in men who worked out for less than half an hour,7 a surprisingly large reduction in risk in light of the narrow distinction between activity categories. A meta-analysis of these and 5 smaller prospective studies yielded a significant 45% lower risk of hip fracture in men with moderate to vigorous physical activity than in less active participants.6 More recently, the Tromsø Study followed men aged 55 years and older for 15 years after a baseline assessment of time spent in light and hard leisure-time activity that was then used for classification into 3 activity levels.14 Men in the top level of moderate to high activity were found to have a significant 37% lower risk of hip fracture than did sedentary men. Our findings did not fully support this previous research, despite a more than 10-fold difference in energy expenditure between our top and bottom quintiles of total activity.
Walking was linearly associated with a decreased risk of hip fracture in the men in our sample. A faster walking pace was also associated with a lower risk, perhaps because of a greater impact on bones. Other studies have reported a lower risk of hip fracture for men who walked than for sedentary men,12,36 although the benefit was not as great as that from regular participation in sports.12 Walking programs of up to 1 year have not demonstrated significant preservation of bone mass,37 but this does not rule out the possibility that regular walking over many years may help to preserve bone. Also, walking may work to prevent hip fractures through other factors than bone density, such as improvement in balance38 and lower-extremity muscle strength39,40 and reduction in falling.40,41
It is important to assess inactivity in relation to risk of hip fracture, because sedentary behaviors and activity are independent measures.42,43 Contrary to expectation, more time spent sitting was associated with a significantly lower risk of hip fracture in participants in our study. However, this was only true for men who also performed a minimum amount of activity—walking at least 2 hours per week. This interaction with walking was strongest for sitting while watching TV, perhaps because people are more able to accurately report their TV time. Beyond the relatively small amount of time per day engaged in the specific physical activities on our questionnaire, more time spent sitting may be a marker for less time spent in pursuits that provide an opportunity for falling. For example, household activities have been associated with a higher fall risk in men.44 It is also possible that although BMI did not differ by time spent sitting, the percentage of body mass that is fat may be higher in men who do more sitting, producing a more estrogenic state. In contrast to our finding in men, our previous investigation in postmenopausal women found that sitting was not associated with risk of hip fracture.15
The strengths of our study were the focus on men, the prospective design with repeat assessments of physical activity and sitting, and the large number of hip fractures over 24 years of follow-up. Participants reported times spent in specific activities, which allowed us to quantify total activity by energy expenditure and to separately examine low- and high-intensity activities. A limitation was that we lacked data on frequency of falling. The results pertain to free-living White men aged 50 years and older and may not be generalizable to men of other racial or ethnic backgrounds or to a more elderly, frail, or institutionalized population.
More time spent walking, particularly brisk walking, was associated with a lower risk of hip fracture in middle-aged and older men. Walking is already the most common exercise among older adults45 and is relatively safe and easy to perform, making it a suitable activity to promote for prevention of hip fractures.
Acknowledgments
This research was supported by the National Institutes of Health (grants CA87969 and AG031395).
Human Participant Protection
This study was approved by the institutional review board of Brigham and Women’s Hospital.
References
- 1.Mussolino ME, Looker AC, Madans JH, Langlois JA, Orwoll ES. Risk factors for hip fracture in White men: the NHANES I Epidemiologic Follow-up Study. J Bone Miner Res. 1998;13(6):918–924. doi: 10.1359/jbmr.1998.13.6.918. [DOI] [PubMed] [Google Scholar]
- 2.Haentjens P, Magaziner J, Colón-Emeric CS et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bilezikian JP. Osteoporosis in men. J Clin Endocrinol Metab. 1999;84(10):3431–3434. doi: 10.1210/jcem.84.10.6060. [DOI] [PubMed] [Google Scholar]
- 4.Nieves JW, Formica C, Ruffing J et al. Males have larger skeletal size and bone mass than females, despite comparable body size. J Bone Miner Res. 2005;20(3):529–535. doi: 10.1359/JBMR.041005. [DOI] [PubMed] [Google Scholar]
- 5.Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000;48(8):883–893. doi: 10.1111/j.1532-5415.2000.tb06884.x. [DOI] [PubMed] [Google Scholar]
- 6.Moayyeri A. The association between physical activity and osteoporotic fractures: a review of the evidence and implications for future research. Ann Epidemiol. 2008;18(11):827–835. doi: 10.1016/j.annepidem.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Paganini-Hill A, Chao A, Ross RK, Henderson BE. Exercise and other factors in the prevention of hip fracture: the Leisure World Study. Epidemiol. 1991;2(1):16–25. doi: 10.1097/00001648-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Meyer HE, Tverdal A, Falch JA. Risk factors for hip fracture in middle-aged Norwegian women and men. Am J Epidemiol. 1993;137(11):1203–1211. doi: 10.1093/oxfordjournals.aje.a116622. [DOI] [PubMed] [Google Scholar]
- 9.Joakimsen RM, Fønnebo V, Magnus JH, Størmer J, Tollan A, Søgaard J. The Tromsø Study: physical activity and the incidence of fractures in a middle-aged population. J Bone Miner Res. 1998;13(7):1149–1157. doi: 10.1359/jbmr.1998.13.7.1149. [DOI] [PubMed] [Google Scholar]
- 10.Kujala UM, Kaprio J, Kannus P, Sarna S, Koskenvuo M. Physical activity and osteoporotic hip fracture risk in men. Arch Intern Med. 2000;160(5):705–708. doi: 10.1001/archinte.160.5.705. [DOI] [PubMed] [Google Scholar]
- 11.Høidrup S, Sørensen TIA, Strøger U, Lauritzen JB, Schroll M, Grønbek M. Leisure-time physical activity levels and changes in relation to risk of hip fracture in men and women. Am J Epidemiol. 2001;154(1):60–68. doi: 10.1093/aje/154.1.60. [DOI] [PubMed] [Google Scholar]
- 12.Michaëlsson K, Olofsson H, Jensevik K et al. Leisure physical activity and the risk of fracture in men. PLoS Med. 2007;4(6):e199. doi: 10.1371/journal.pmed.0040199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trimpou P, Landin-Wilhelmsen K, Odén A, Rosengren A, Wilhelmsen L. Male risk factors for hip fracture—a 30-year follow-up study in 7,495 men. Osteoporos Int. 2010;21(3):409–416. doi: 10.1007/s00198-009-0961-7. [DOI] [PubMed] [Google Scholar]
- 14.Morseth B, Ahmed LA, Bjørnerem Å et al. Leisure time physical activity and risk of non-vertebral fracture in men and women aged 55 years and older: the Tromsø Study. Eur J Epidemiol. 2012;27(6):463–471. doi: 10.1007/s10654-012-9665-y. [DOI] [PubMed] [Google Scholar]
- 15.Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288(18):2300–2306. doi: 10.1001/jama.288.18.2300. [DOI] [PubMed] [Google Scholar]
- 16.Stampfer MJ, Willett WC, Speizer FE et al. Test of the National Death Index. Am J Epidemiol. 1984;119(5):837–839. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 17.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol. 1994;140(11):1016–1019. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 18.Colditz GA, Martin P, Stampfer MJ et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol. 1986;123(5):894–900. doi: 10.1093/oxfordjournals.aje.a114319. [DOI] [PubMed] [Google Scholar]
- 19.Ainsworth BE, Haskell WL, Leon AS et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Chasan-Taber S, Rimm EB, Stampfer MJ et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7(1):81–86. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 22.Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennekens CH. A prospective study of exercise and incidence of diabetes among US male physicians. JAMA. 1992;268(1):63–67. [PubMed] [Google Scholar]
- 23.Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122(5):327–334. doi: 10.7326/0003-4819-122-5-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med. 2001;161(12):1542–1548. doi: 10.1001/archinte.161.12.1542. [DOI] [PubMed] [Google Scholar]
- 25.Feskanich D, Rimm EB, Giovannucci EL et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93(7):790–796. doi: 10.1016/0002-8223(93)91754-e. [DOI] [PubMed] [Google Scholar]
- 26.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135(10):1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- 27.Parkkari J, Kannus P, Palvanen M et al. Majority of hip fractures occur as a result of a fall and impact of the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int. 1999;65(3):183–187. doi: 10.1007/s002239900679. [DOI] [PubMed] [Google Scholar]
- 28.Buchner DM, Cress ME, de Latuer BJ et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci. 1997;52(4):M218–M224. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- 29.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28(6):513–518. doi: 10.1093/ageing/28.6.513. [DOI] [PubMed] [Google Scholar]
- 30.Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43(11):1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- 31.Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc. 1999;47(10):1208–1214. doi: 10.1111/j.1532-5415.1999.tb05201.x. [DOI] [PubMed] [Google Scholar]
- 32.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomized controlled trial of a general practice programme of home-based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Phys Ther. 1997;77(1):46–57. doi: 10.1093/ptj/77.1.46. [DOI] [PubMed] [Google Scholar]
- 34.Layne JE, Nelson ME. The effects of progressive resistance training on bone density: a review. Med Sci Sports Exerc. 1999;31(1):25–30. doi: 10.1097/00005768-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Kelley GA, Kelley KS, Tran ZV. Exercise and bone mineral density in men: a meta-analysis. J Appl Physiol. 2000;88(5):1730–1736. doi: 10.1152/jappl.2000.88.5.1730. [DOI] [PubMed] [Google Scholar]
- 36.Moayyeri A, Besson Hervé B, Luben RN, Wareham NJ, Khaw K-T. The association between physical activity in different domains of life and risk of osteoporotic fractures. Bone. 2010;47(3):693–700. doi: 10.1016/j.bone.2010.06.023. [DOI] [PubMed] [Google Scholar]
- 37.Kohrt WM, Bloomfield SA, Little KD, Nelson ME, Yingling VR. American College of Sports Medicine Position Stand: physical activity and bone health. Med Sci Sports Exerc. 2004;36(11):1985–1996. doi: 10.1249/01.mss.0000142662.21767.58. [DOI] [PubMed] [Google Scholar]
- 38.Clary S, Barnes C, Bemben D, Knehans A, Bemben M. Effects of ballates, step aerobics, and walking on balance in women aged 50–75 years. J Sports Sci Med. 2006;5(3):390–399. [PMC free article] [PubMed] [Google Scholar]
- 39.Asikainen T-M, Suni JH, Pasanen ME et al. Effect of brisk walking in 1 or 2 daily bouts and moderate resistance training on lower-extremity muscle strength, balance, and walking performance in women who recently went through menopause: a randomized, controlled trial. Phys Ther. 2006;86(7):912–923. [PubMed] [Google Scholar]
- 40.Stewart AD, Stewart A, Reid DM. Correcting calf girth discriminates the incidence of falling but not bone mass by broadband ultrasound attenuation in elderly female subjects. Bone. 2002;31(1):195–198. doi: 10.1016/s8756-3282(02)00811-6. [DOI] [PubMed] [Google Scholar]
- 41.Pereira MA, Kriska AM, Day RD, Cauley JA, LaPorte RE, Kuller LH. A randomized walking trial in postmenopausal women: effects on physical activity and health 10 years later. Arch Intern Med. 1998;158(15):1695–1701. doi: 10.1001/archinte.158.15.1695. [DOI] [PubMed] [Google Scholar]
- 42.Burton NW, Khan A, Brown WJ, Turrell G. The association between sedentary leisure and physical activity in middle-aged adults. Br J Sports Med. 2012;46(10):747–752. doi: 10.1136/bjsm.2010.081430. [DOI] [PubMed] [Google Scholar]
- 43.Finni T, Haakana P, Pesola AJ, Pullinen T. Exercise for fitness does not decrease the muscular inactivity time during normal daily life. Scand J Med Sci Sports. doi: 10.1111/j.1600-0838.2012.01456.x. 2012;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 44.Chan BKS, Marshall LM, Winters KM, Faulkner KA, Schwartz AV, Orwoll ES. Incident fall risk and physical activity and physical performance among older men: the Osteoporotic Fractures in Men Study. Am J Epidemiol. 2007;165(6):696–703. doi: 10.1093/aje/kwk050. [DOI] [PubMed] [Google Scholar]
- 45.Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 1996. [Google Scholar]