Abstract
Background
As growing numbers of Medicaid enrollees receive health benefits through comprehensive managed care, researchers and policymakers seeking to understand the service use of these enrollees must rely on encounter data.
Objective
To assess the availability, completeness, and quality of physician, clinic, and outpatient service (OT), inpatient (IP), and prescription drug (RX) encounter claims to judge the usability of the 2008 Medicaid Analytical eXtract (MAX) encounter data.
Data
2008 MAX encounter data, which are derived from the state-submitted Medicaid Statistical Information System (MSIS) files.
Methods
For each basis of eligibility (BOE) group in each state that had at least ten percent participation in comprehensive managed care and submitted at least 200 encounter claims, the completeness and quality of the OT, IP, and RX encounter data were evaluated using comparison metrics created from the full-benefit, non-dual fee-for-service (FFS) population across all states with substantial FFS participation. Data that met both the completeness and quality criteria were considered usable.
Results
The completeness and the quality of the encounter data were high. The encounter data were considered usable for a least one BOE category for 22 of the 25 states that submitted OT encounter data, 20 of the 24 states that submitted IP data, and 13 of the 15 states that submitted RX data.
Conclusions
Most states that have comprehensive managed care plans are reporting OT, IP, and RX encounter data. Of those data, the majority are complete and of comparable quality to FFS data for adults, children, the disabled, and aged populations.
Keywords: Medicaid Managed Care, managed care data, encounter data
Introduction
As states expand their use of managed care arrangements to provide services to Medicaid enrollees, researchers and policymakers will need to analyze additional types of data to assess their service use. With 50 percent of all full-benefit1 Medicaid enrollees enrolled in comprehensive managed care in 2008, relying on fee-for-service (FFS) data to determine the service use of the Medicaid population is no longer sufficient (Borck et al., 2012). To capture the service use of comprehensive managed care enrollees, encounter data—claims records that contain information on utilization but not on Medicaid expenditures—must be evaluated as well.
To ensure that managed care enrollees receive the same level and quality of services as FFS enrollees, several states perform comprehensive checks on the data that they receive from managed care plans; however, the quality of the encounter data submitted by the states to the Medicaid Statistical Information System (MSIS) is not clear (Byrd, Verdier, Nysenbaum, & Schoettle, 2011). FFS data submitted to MSIS undergo extensive quality and validation checks and it is clear that the quality of FFS data differs over time and by state.2 While encounter data do not undergo the same validation and quality checks in either MSIS or Medicaid Analytic eXtract (MAX) processing that FFS data undergo, it is likely that there is variation in the quality of the encounter data as well.
According to actuaries and state Medicaid officials, encounter data for inpatient hospital (IP) and prescription drug (RX) services—which are provided by a relatively small number of providers—are typically easier to collect and may be more complete than “other services'” (OT) data. Most of the service use among Medicaid enrollees, however, including physician, clinic, and outpatient services, is captured in the OT file. In this brief, we use MAX 2008 data to assess the availability, completeness, and quality of encounter data for inpatient hospital (IP), prescription drug (RX), physician, outpatient, and clinic services (OT) from health maintenance organization (HMO)/health insuring organization (HIO) plans.
Methods
The data used in this analysis are from MAX 2008. Derived from MSIS, MAX was designed to enable research on Medicaid enrollment, service utilization, and expenditures by calendar year at the enrollee level. Analysis by calendar year is particularly important with encounter data, because some states that submit them do not do so in every quarterly MSIS submission (Byrd et al., 2011).
As states vary widely in terms of the mixture of Medicaid populations enrolled in capitated managed care programs, examining the volume of encounter data submissions for all groups within a state could be misleading. Many states rolled out comprehensive managed care to children and adult enrollees first, and only some have enrolled the aged and disabled populations in it. To facilitate more accurate state-by-state comparisons, the data were analyzed using the enrollee's basis-of-eligibility (BOE) classification—adult, child, disabled, or aged. The average 2008 capitation payment for enrollees in comprehensive managed care was much lower for adults and children than for aged and disabled beneficiaries, an indication that the expected level of service use, and therefore the expected volume of encounter claims, is lower among adults and children (Borck et al., 2012).
In MAX 2008, encounter data for comprehensive managed care enrollees were available for over half of the states in at least one type of file: IP, long-term care (LT), OT, or RX (Exhibit 1). The analysis was limited to fully capitated (comprehensive) managed care arrangement HMO/HIO plans, because they cover the widest range of services and are thought to have the highest quality encounter data.
Exhibit 1. Overview of Encounter Data Available in MAX 2008 for HMO/HIO Enrollees, by File Type.
| File Type | Number of States with Data, 2008a | Number of Encounter Claims, 2008 |
|---|---|---|
| IP | 29 | 1,947,019 |
| LT | 22 | 560,201 |
| OT | 34 | 350,312,637 |
| RX | 20 | 87,573,721 |
Includes all states that submitted encounter data regardless of the level of HMO/HIO participation in the state, the number of claims submitted, or whether prescriptions were covered as part of the comprehensive managed care program.
SOURCE: Mathematica's analysis of MAX 2008 data.
The OT file may contain up to 22 types of service, while IP may contain four, and RX two. For the OT analysis, “physicians” (type of service = 08), “outpatient hospital” (type of service = 11), and “clinic” (type of service = 12) services were chosen because these are services routinely sought and covered under Medicaid in all states, and managed care plans are accustomed to collecting and reporting these data for quality assurance, such as for the Healthcare Effectiveness Data and Information Set (HEDIS). “Inpatient hospital” (type of service = 01) services from the IP file were included, because while the IP file may contain three other types of service, “inpatient hospital” represents the vast majority of claims and services in the inpatient setting. “Prescribed drugs” (type of service = 16) were included from the RX file, but durable medical equipment was not.
Since analyzing both individually and together did not yield substantial differences, physician, outpatient, and clinic services are presented as a whole in this brief. Other types of services included in the OT file may not be as easily comparable across states or as complete. For example, the volume of rehabilitation or occupational therapy services relies heavily on how a state counts units of service, which can range on claims from 15-minute increments to hour-long visits. There were too few LT encounter claims for a cross-state analysis.3
A state was considered to have managed care if at least 1 percent of enrollees participated in comprehensive managed care at some point during the year. For prescription drug services, 12 states whose managed care arrangements did not include prescription drug benefits were excluded. Because states with low managed care enrollment are less likely to devote resources to producing high-quality encounter data, data for a particular BOE group were analyzed only if 10 percent or more of full-benefit Medicaid enrollees within that group were enrolled in an HMO/HIO plan. Data for a particular BOE group in a state were not analyzed if it had fewer than 200 claims, because measures based on a small number of records could skew estimates.
Metrics
To be usable, encounter data needed to be both complete and of comparable quality to FFS data for our analysis. This analysis took place in two phases to account for these two characteristics. To judge completeness, two measures were used to assess the volume of encounter data—the average number of claims per person and the percentage of enrollees with claims. To evaluate quality, metrics were used to assess the amount or quality of information on the encounter itself. For the analysis of the OT encounter claims, two quality measures were used for both the diagnosis code and procedure code fields—one indicating whether the field was filled and the second analyzing the format of the data in the field. For diagnosis code, the field was expected to be filled at a high rate because few physician, outpatient, and clinic services' claims are paid without a diagnosis code. To determine whether the diagnosis codes on encounter claims were comparable in the level of specificity to those reported on FFS claims, the length of the diagnosis code was evaluated. The more characters in the diagnosis code (more than three characters), the more specific the diagnosis is on the claim or encounter. Similarly, the procedure codes were expected to be filled at a high rate, but the heavy reliance of some states on procedure codes specific to the state make a national analysis more complicated. The procedure codes were evaluated to determine whether the reported data were in the standard national format. For the IP file, one quality measure was created for each of four fields that undergo scrutiny during the MSIS data quality and validation review process. For the RX file, one quality measure was created for each of two fields that we expect to see routinely filled on FFS claims. The metrics used for evaluation of completeness and quality are shown in Exhibit 2.
Exhibit 2. Metrics Developed to Analyze Medicaid Encounter Data in MAX 2008.
| Data Element | Reference Range (Number of States Meeting Metric) | |||
|---|---|---|---|---|
| Adults | Children | Disabled | Aged | |
| OT—Physician, Clinic, and Outpatient Visits Completeness Measures | ||||
| Average number of OT encounter claims per enrollee | 1.04–12.10 | 1.23–9.46 | 8.35–27.96 | 0.91–19.54 |
| (23 of 24) | (22 of 25) | (15 of 20) | (13 of 16) | |
| Percentage of enrollees with OT encounter claims | 34.33–92.45 | 36.15–93.40 | 66.35–92.39 | 19.57–92.26 |
| (22 of 24) | (23 of 25) | (14 of 20) | (15 of 16) | |
| Quality Measures | ||||
| Percentage of OT encounter claims with place of service code | 83.87–100 | 76.16–100 | 81.89–100 | 84.22–100 |
| (23 of 24) | (25 of 25) | (20 of 20) | (16 of 16) | |
| Percentage of OT encounter claims with primary diagnosis code | 98.17–100 | 86.09–100 | 94.84–100 | 97.02–100 |
| (24 of 24) | (25 of 25) | (20 of 20) | (16 of 16) | |
| Percentage of OT encounter claims with a primary diagnosis code length greater than 3 characters | 90.85–98.81 | 80.92–100 | 88.08–100 | 89.16–99.41 |
| (23 of 24) | (25 of 25) | (20 of 20) | (16 of 16) | |
| Percentage of OT encounter claims with a procedure (service) code | 71.47–100 | 82.13–100 | 78.78–100 | 82.68–100 |
| (20 of 24) | (21 of 25) | (17 of 20) | (13 of 16) | |
| Percentage of OT encounter claims with a procedure code in CPT-4 or HCPCS format | 60.77–100 | 64.32–100 | 66.88–100 | 70.41–100 |
| (21 of 24) | (22 of 25) | (18 of 20) | (15 of 16) | |
| IP—Inpatient Hospital Completeness Measures | ||||
| Average number of IP encounter claims per enrollee | 0.00–0.40 | 0.02–0.15 | 0.10–0.54 | 0.00–0.44 |
| (22 of 24) | (18 of 24) | (16 of 20) | (14 of 15) | |
| Percentage of enrollees with IP encounter claims | 0.21–32.51 | 1.06–13.08 | 7.55–25.39 | 3.62–22.39 |
| (23 of 24) | (20 of 24) | (15 of 20) | (11 of 15) | |
| Quality Measures | ||||
| Average length of stay | 2.01–3.90 | 2.04–6.48 | 5.35–8.61 | 3.32–10.49 |
| (23 of 24) | (22 of 24) | (9 of 20) | (14 of 15) | |
| Average number of diagnosis codes | 2.42–6.43 | 1.89–4.38 | 3.09–9.76 | 3.19–10.72 |
| (20 of 24) | (20 of 24) | (16 of 20) | (12 of 15) | |
| Percentage of IP claims with procedure codes | 48.17–100.00 | 18.72–76.39 | 30.70–71.13 | 25.05–73.55 |
| (18 of 24) | (23 of 24) | (15 of 20) | (13 of 15) | |
| Percentage of IP claims with UB accommodation codes | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% |
| (20 of 24) | (20 of 24) | (13 of 20) | (11 of 15) | |
| RX—Prescription Drugs Completeness Measures | ||||
| Average number of RX encounter claims per enrollee | 1.86–12.95 | 1.80–7.22 | 17.27–50.09 | 0–48.22 |
| (13 of 14) | (14 of 15) | (8 of 10) | (8 of 8) | |
| Percentage of enrollees with RX encounter claims | 26.79–88.04 | 31.46–80.84 | 68.14–89.30 | 12.21–89.82 |
| (13 of 14) | (14 of 15) | (9 of 10) | (7 of 8) | |
| Quality Measures | ||||
| Percentage of RX claims with date prescribed | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% |
| (13 of 14) | (14 of 15) | (9 of 10) | (7 of 8) | |
| Percentage of RX claims with quantity | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% | Values of ≥ 90% |
| (8 of 14) | (9 of 15) | (6 of 10) | (4 of 8) | |
NOTE. The parenthetical data show the number of states that had values within the acceptable range, out of the total number of states that had sufficient participation and encounter claims submitted for analysis.
UB = uniform billing, CPT-4 = Current Procedural Terminology, 4th Edition, HCPCS = Healthcare Common Procedure Coding System
SOURCE: Mathematica's analysis of the MAX 2008 IP, RX, OT, and Person Summary (PS) files.
Because managed care coverage varies by state and type of enrollee, the completeness and quality measures for OT, IP, and RX data were evaluated separately for each BOE for each state. To create comparison metrics, the average 2008 value and standard deviation were calculated for each completeness and quality metric for each BOE using the full-benefit, non-dual FFS population across all states with substantial FFS participation. For each comparison metric, the average FFS value was used as the midpoint of our reference range. The top of the reference range was set at two standard deviations above the FFS average, and the bottom at two standard deviations below the FFS average. The reference range was considered to be the acceptable range of values for the 2008 encounter data for that metric. The state's encounter data value was considered “good” if it fell within the reference range. For certain measures, state values were highly skewed, but typically either close to 100 percent or 0 percent for both FFS and encounter data. Rather than use the reference range based on the average value, a “good” value was defined as 90 percent or greater for these measures.
For each BOE that met the analysis criteria, the state's value was compared to the FFS reference metric to determine if it fell within the acceptable range; the ranges are presented in Exhibit 2. The number of states that fell within the range is shown in parentheses for each measure. For example, 23 of the 24 states that met the thresholds for our analysis of OT data for adults had an average number of OT encounter claims per enrollee between 1.04 and 12.10, inclusively. For the OT, IP, and RX data, “complete” was defined as having values within the acceptable range for at least one of the two completeness metrics for that data type. For the OT data, “comparable quality” was defined as satisfying at least four of the five quality measures. For the IP data, “comparable quality” was defined as satisfying at least three of the four quality measures. For the RX data, “comparable quality” was defined as satisfying at least one of the two quality measures. A BOE within a state was considered to have “usable” data if the encounter data for that BOE met both the “complete” and “comparable quality” criteria.
Findings
OT Encounter Data
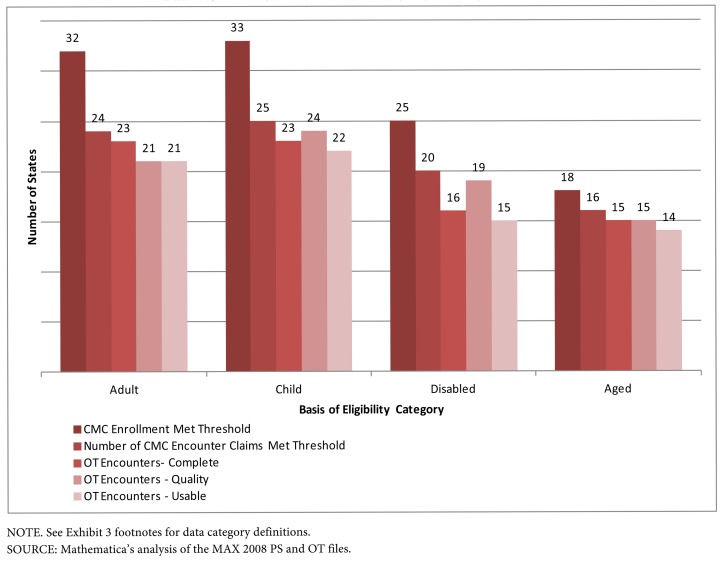
Exhibit 3 summarizes the availability, completeness, and quality of the OT encounter data for each state by BOE. Exhibit 4 illustrates how the criteria applied at each step of the analysis eliminated states from meeting the usability criteria. For example, 35 states had comprehensive managed care at some point during 2008. At least 10 percent of adult enrollees participated in comprehensive managed care in 32 of these 35 states. Of these 32 states, 24 (75 percent) submitted OT encounter claims for adults. The completeness of the adult OT encounter data was high, with 23 of 24 states submitting complete data. The quality of the encounter data was high as well, with 21 of 24 states submitting data of comparable quality to the FFS data. Because they met the criteria for both completeness and quality, the OT encounter data for adult enrollees are considered usable for 21 states (88 percent) that submitted data.
Exhibit 3. Summary of the 2008 MAX Encounter OT Claims.
| State Has Comprehensive Managed Care (CMC)a | Percentage of CMC Enrollees Met Thresholdb | State Submitted OT Encounter Claimsc | OT Encounter Records Are Completed | OT Encounter Records Are of Comparable Quality to FFS Datae | OT Encounter Data Are Usable for Researchf | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | ||
| Alabama | |||||||||||||||||||||
| Alaska | |||||||||||||||||||||
| Arizona | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Arkansas | |||||||||||||||||||||
| California | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Colorado | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Connecticut | |||||||||||||||||||||
| Delaware | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| DC | X | X | X | X | |||||||||||||||||
| Florida | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Georgia | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Hawaii | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Idaho | |||||||||||||||||||||
| Illinois | X | X | X | X | X | X | |||||||||||||||
| Indiana | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Iowa | X | ||||||||||||||||||||
| Kansas | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Kentucky | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Louisiana | |||||||||||||||||||||
| Maine | |||||||||||||||||||||
| Maryland | X | X | X | X | X | X | X | X | X | X | |||||||||||
| Massachusetts | X | X | X | X | |||||||||||||||||
| Michigan | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Minnesota | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Mississippi | |||||||||||||||||||||
| Missouri | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Montana | |||||||||||||||||||||
| Nebraska | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Nevada | X | X | X | ||||||||||||||||||
| New Hampshire | |||||||||||||||||||||
| New Jersey | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| New Mexico | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| New York | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| North Carolina | |||||||||||||||||||||
| North Dakota | |||||||||||||||||||||
| Ohio | X | X | X | X | X | ||||||||||||||||
| Oklahoma | |||||||||||||||||||||
| Oregon | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Pennsylvania | X | X | X | X | X | ||||||||||||||||
| Rhode Island | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| South Carolina | X | X | X | X | |||||||||||||||||
| South Dakota | |||||||||||||||||||||
| Tennessee | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Texas | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Utah | |||||||||||||||||||||
| Vermont | X | ||||||||||||||||||||
| Virginia | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Washington | X | X | X | ||||||||||||||||||
| West Virginia | X | X | X | ||||||||||||||||||
| Wisconsin | X | X | X | X | X | X | X | X | X | ||||||||||||
| Wyoming | |||||||||||||||||||||
| Total | 35 | 32 | 33 | 25 | 18 | 24 | 25 | 20 | 16 | 23 | 23 | 16 | 15 | 21 | 24 | 19 | 15 | 21 | 22 | 15 | 14 |
NOTE. A=Adults, C=Children, D=Disabled, E=Aged.
At least one percent of enrollees participated in HMO/HIO at some point during 2008.
At least 10 percent of enrollees in the BOE participated in HMO/HIO at some point during the year.
In addition to having at least 10 percent HMO/HIO participation, the state submitted at least 200 encounter claims for the BOE.
The BOE-specific metric was met for at least one of the two completeness measures: (1) percentage of enrollees with OT encounter claims (TOS = 08, 11, 12) and (2) average number of OT encounter claims per enrollee.
The BOE-specific metric was met for at least four of the five quality measures: (1) percentage of OT claims with place of service, (2) percentage of OT claims with a primary diagnosis code, (3) percentage of claims with a primary diagnosis code with a character length greater than 3, (4) percentage of claims with a procedure (service) code, and (5) percentage of claims with a procedure code in CPT-4 or HCPCS format.
Both the completeness and quality standards were met for the BOE.
SOURCE: Mathematica's analysis of the MAX 2008 PS and OT files.
Exhibit 4. Summary of the MAX 2008 OT Encounter Claims by Basis of Eligibility Category.
Data can also be considered usable for 22 of the 25 states (88 percent) submitting data for children. Fifteen of the 20 states submitting data for disabled enrollees (75 percent) met both completeness and quality thresholds, and of the 16 states submitting encounter claims for the aged, 14 submitted data that can be considered usable.
The OT encounter data were considered usable for at least one BOE category for 24 of the 25 states (96 percent) that submitted these data. Eighteen states (72 percent) provided usable encounter data for all the BOE categories for which they submitted data (Arizona, Delaware, Georgia, Hawaii, Illinois, Indiana, Kansas, Kentucky, Michigan, Missouri, Nebraska, New Jersey, New Mexico, New York, Oregon, Tennessee, Texas, and Virginia). Only one state (Maryland) submitted OT encounter data that did not meet the usability criteria for any BOE. The remaining 6 states met the criteria for some BOEs but not others.
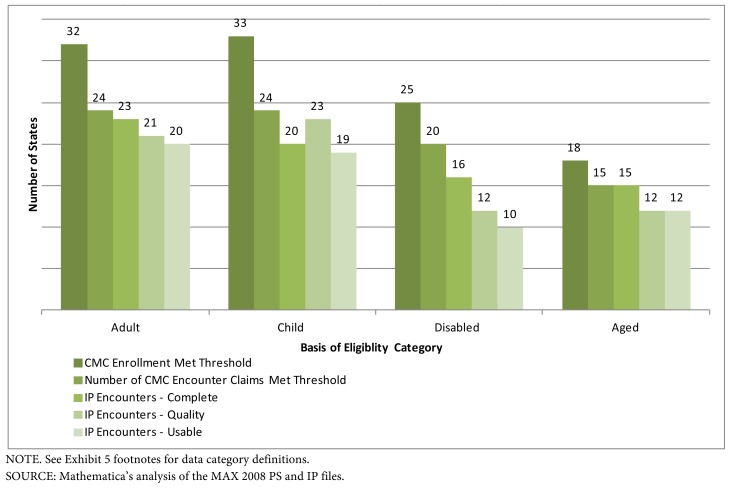
IP Encounter Data
Exhibit 5 summarizes the availability, completeness, and quality of the IP encounter data for each state by BOE. Exhibit 6 illustrates how the criteria applied at each step of the analysis eliminated states from meeting the usability criteria. The completeness and the quality of the IP encounter data were high. They were considered usable for at least one BOE category for 22 of the 25 states that submitted these data (88 percent). Thirteen states (52 percent) provided usable data for all of the BOE categories for which they submitted data (Arizona, Hawaii, Indiana, Kansas, Kentucky, Missouri, Nebraska, New Jersey, New Mexico, Oregon, Virginia, Washington, and Wisconsin). Of the 25 states that submitted suitable IP encounter data for the analysis, three states did not meet the criteria for usability for any BOE. The remaining nine states met the criteria for some BOEs but not others.
Exhibit 5. Summary of the 2008 MAX Encounter IP Claims.
| State Has Comprehensive Managed Care (CMC)a | Percentage of CMC Enrollees Met Thresholdb | State Submitted IP Encounter Claimsc | IP Encounter Records Are Completed | IP Encounter Records Are of Comparable Quality to FFS Datae | IP Encounter Data Are Usable for Researchf | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | ||
| Alabama | |||||||||||||||||||||
| Alaska | |||||||||||||||||||||
| Arizona | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Arkansas | |||||||||||||||||||||
| California | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Colorado | X | X | X | X | X | X | X | X | X | ||||||||||||
| Connecticut | |||||||||||||||||||||
| Delaware | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| DC | X | X | X | X | |||||||||||||||||
| Florida | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Georgia | X | X | X | ||||||||||||||||||
| Hawaii | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Idaho | |||||||||||||||||||||
| Illinois | X | X | X | X | |||||||||||||||||
| Indiana | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Iowa | X | ||||||||||||||||||||
| Kansas | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Kentucky | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Louisiana | |||||||||||||||||||||
| Maine | |||||||||||||||||||||
| Maryland | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Massachusetts | X | X | X | X | |||||||||||||||||
| Michigan | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||
| Minnesota | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Mississippi | |||||||||||||||||||||
| Missouri | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Montana | |||||||||||||||||||||
| Nebraska | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Nevada | X | X | X | ||||||||||||||||||
| New Hampshire | |||||||||||||||||||||
| New Jersey | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| New Mexico | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| New York | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| North Carolina | |||||||||||||||||||||
| North Dakota | |||||||||||||||||||||
| Ohio | X | X | X | X | X | ||||||||||||||||
| Oklahoma | |||||||||||||||||||||
| Oregon | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Pennsylvania | X | X | X | X | X | ||||||||||||||||
| Rhode Island | X | X | X | X | X | X | X | X | X | X | |||||||||||
| South Carolina | X | X | X | X | |||||||||||||||||
| South Dakota | |||||||||||||||||||||
| Tennessee | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Texas | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Utah | |||||||||||||||||||||
| Vermont | X | ||||||||||||||||||||
| Virginia | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Washington | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| West Virginia | X | X | X | ||||||||||||||||||
| Wisconsin | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Wyoming | |||||||||||||||||||||
| Total | 35 | 32 | 33 | 25 | 18 | 24 | 24 | 20 | 15 | 23 | 20 | 16 | 15 | 21 | 23 | 12 | 12 | 20 | 19 | 10 | 12 |
NOTE. A=Adults, C=Children, D=Disabled, E=Aged.
At least one percent of enrollees participated in HMO/HIO at some point during 2008.
At least 10 percent of enrollees in the BOE participated in HMO/HIO at some point during the year.
In addition to having at least 10 percent HMO/HIO participation, the state submitted at least 200 encounter claims for the BOE.
The BOE-specific metric was met for at least one of the two completeness measures: (1) percentage of enrollees with IP encounter claims and (2) average number of IP encounter claims per enrollee.
The BOE-specific metric was met for at least three of the four quality measures: (1) average length of stay, (2) average number of diagnosis codes, (3) percentage of claims with procedure code, and (4) percentage of claims with UB accommodation codes.
Both the completeness and quality standards were met for the BOE.
SOURCE: Mathematica's analysis of the MAX 2008 PS and IP files.
Exhibit 6. Summary of the MAX 2008 IP Encounter Claims by Basis of Eligibility Category.
RX Encounter Data
Exhibit 7 summarizes the availability, completeness, and quality of the RX encounter data for each state by BOE. Exhibit 8 illustrates how the criteria applied at each step of the analysis eliminated states from meeting the usability criteria. Almost every state that submitted RX encounter data submitted data that were complete and of comparable quality to FFS data for every BOE group. Thirteen states provided usable data for every BOE group for which they submitted data (Arizona, California, Georgia, Indiana, Kansas, Kentucky, Maryland, Michigan, Missouri, New Mexico, Rhode Island, Virginia, and Washington).
Exhibit 7. Summary of the 2008 MAX Encounter RX Claims.
| State Has Comprehensive Managed Care (CMC)a | Percentage of CMC Enrollees Met Thresholdb | State Submitted RX Encounter Claimsc | RX Encounter Records Are Completed | RX Encounter Records Are of Comparable Quality to FFS Datae | RX Encounter Data Are Usable for Researchf | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | A | C | D | E | ||
| Alabama | |||||||||||||||||||||
| Alaska | |||||||||||||||||||||
| Arizona | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Arkansas | |||||||||||||||||||||
| California | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Colorado | X | X | X | X | X | ||||||||||||||||
| Connecticut | |||||||||||||||||||||
| Delaware | |||||||||||||||||||||
| DC | X | X | X | X | |||||||||||||||||
| Florida | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||||
| Georgia | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Hawaii | X | X | X | X | |||||||||||||||||
| Idaho | |||||||||||||||||||||
| Illinois | |||||||||||||||||||||
| Indiana | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Iowa | |||||||||||||||||||||
| Kansas | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Kentucky | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Louisiana | |||||||||||||||||||||
| Maine | |||||||||||||||||||||
| Maryland | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Massachusetts | X | X | X | X | |||||||||||||||||
| Michigan | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Minnesota | X | X | X | X | X | X | X | X | X | X | X | X | |||||||||
| Mississippi | |||||||||||||||||||||
| Missouri | X | X | X | X | X | X | X | X | X | X | X | ||||||||||
| Montana | |||||||||||||||||||||
| Nebraska | |||||||||||||||||||||
| Nevada | X | X | X | ||||||||||||||||||
| New Hampshire | |||||||||||||||||||||
| New Jerseyg | |||||||||||||||||||||
| New Mexico | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| New Yorkg | |||||||||||||||||||||
| North Carolina | |||||||||||||||||||||
| North Dakota | |||||||||||||||||||||
| Ohio | X | X | X | X | X | ||||||||||||||||
| Oklahoma | |||||||||||||||||||||
| Oregong | |||||||||||||||||||||
| Pennsylvania | X | X | X | X | X | ||||||||||||||||
| Rhode Island | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| South Carolina | X | X | X | X | |||||||||||||||||
| South Dakota | |||||||||||||||||||||
| Tennessee | |||||||||||||||||||||
| Texas | |||||||||||||||||||||
| Utah | |||||||||||||||||||||
| Vermont | X | ||||||||||||||||||||
| Virginia | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Washington | X | X | X | X | X | X | X | ||||||||||||||
| West Virginia | |||||||||||||||||||||
| Wisconsing | |||||||||||||||||||||
| Wyoming | |||||||||||||||||||||
| Total | 24 | 23 | 23 | 18 | 11 | 14 | 15 | 10 | 8 | 13 | 14 | 9 | 8 | 13 | 14 | 9 | 7 | 12 | 13 | 9 | 7 |
NOTE. A=Adults, C=Children, D=Disabled, E=Aged.
At least one percent of enrollees participated in HMO/HIO/PACE at some point during 2008. There were 12 states in which MC plans did not provide a pharmacy benefit: CT, DE, IA, IL, NE, NJ, NY, OR, TN, TX, WI, and WV (Bagchi, Verdier, & Esposito, 2012).
At least 10 percent of enrollees in the BOE participated in HMO/HIO at some point during the year.
In addition to having at least 10 percent HMO/HIO participation, the state submitted at least 200 encounter claims for the BOE.
The BOE-specific metric was met for at least one of the two completeness measures: (1) percentage of enrollees with RX encounter claims and (2) average number of RX encounter claims per enrollee.
The BOE-specific metric was met for at least one of the two quality measures: (1) percentage of RX claims with date prescribed and (2) percentage of RX claims with quantity.
Both the completeness and quality standards were met for the BOE.
NJ, NY, OR, and WI submitted RX encounter data even though prescription drugs were not included in the HMO benefit package. Bagchi et al., (2012) identify which states "carved out" their pharmacy benefits.
SOURCE: Mathematica's analysis of the MAX 2008 PS and RX files.
Exhibit 8. Summary of the MAX 2008 RX Encounter Claims by Basis of Eligibility Category.
Caveats
In this brief, selected FFS-based metrics were used to make a preliminary judgment about the quality and completeness of the data for inpatient hospitalization, physician services, outpatient hospital services, clinic services, and prescription medication. This approach has been useful, because it illustrates that a reasonable quantity of encounter data is available in MAX and that they appear to be of good quality on basic measures. It is assumed that, like the FFS data, the MAX data that fall within acceptable ranges accurately depict what is happening in the state. This analysis is limited, however, by its assumption that FFS data provide a reasonable benchmark for judging the encounter data, which may not be the case, depending on the particular populations a state chooses to enroll in managed care. While populations receiving services through comprehensive managed care plans are likely to differ from FFS populations in important ways, metrics within two standard deviations were used to account for differences in utilization patterns that may reflect differences in populations or inherent differences between the FFS and managed care delivery systems. The use of two standard deviations is consistent with confidence intervals typically used in statistical analyses, but for measures with a lot of variation in the FFS data, this sometimes resulted in a wide reference range. Additionally, it may be difficult to extend the analysis of selected OT measures to other types of services in the OT file. It will depend on the type of service, whether the type of service is covered by managed care arrangements, and how consistently services are billed across states or within plan arrangements.
Because FFS data are not without completeness and quality issues, a state's encounter data did not have to meet all completeness and quality measures to be considered usable. If all of the measures had to be met, the number of states with usable data for at least one BOE would have dropped. Among the 24 states that had comprehensive managed care participation of 10 percent or more for adults and that submitted encounter claims, the number with usable data for research on OT encounters would fall from 21 (88 percent) to 17 (71 percent; data not shown), where Florida would not meet the completeness threshold, and Arizona, Hawaii, and Rhode Island would not meet the quality threshold. Among the 24 states that had comprehensive managed care participation of 10 percent or more for adults and that submitted encounter claims, the number with usable data for research on IP encounters would fall from 20 (83 percent) to 12 (50 percent), where Rhode Island would not meet the completeness threshold, and California, Florida, Kansas, Maryland, Michigan, New Mexico, and Virginia would not meet the quality threshold. Among the 14 states that had comprehensive managed care participation of 10 percent or more for adults and that submitted encounter claims, the number with usable data for research on RX encounters would fall from 12 (86 percent) to 7 (50 percent), where California, Georgia, Missouri, New Mexico, and Virginia would not meet the quality threshold.
Conclusions
This brief provides an assessment of OT, IP, and RX encounter data included in the MAX 2008 data files. The results are encouraging. Most states that have comprehensive managed care plans are reporting selected OT, IP, and RX encounter data. Of those data, the majority are complete and of comparable quality to the FFS data for adults, children, the disabled, and aged populations. Although several actuaries and state officials involved in Medicaid administration at the state level have hypothesized that IP and RX data might be more complete and of higher quality than OT data, because they are collected from fewer providers (Byrd et al., 2011), this analysis did not confirm that hypothesis. The OT data appear to be complete and of about the same quality as FFS data for more states than the IP data.
This analysis will aid researchers in determining which states with notable comprehensive managed care enrollment may be reasonable to analyze. By knowing the usability of the encounter data for physician and clinic encounters, inpatient and outpatient visits, and prescription drugs, researchers and policymakers can reasonably consider adding the analysis of encounter data when assessing Medicaid service utilization in states with substantial enrollment in comprehensive managed care.
Acknowledgement
The authors wish to acknowledge the contributions of several individuals to the preparation of this report. We wish to thank Mei-Ling Mason, Ashley Zlatinov, and Rosalie Malsberger for providing expert statistical programming assistance. Julie Sykes and Maggie Colby provided helpful comments. Finally, we wish to thank Cara Petroski in the Office of Information Products and Data Analysis, Centers for Medicare & Medicaid Services for her commitment to the development and continual improvement of MAX for Medicaid research.
Footnotes
A full-benefit Medicaid enrollee is an individual eligible for Medicaid or CHIP and entitled to the full scope of Medicaid or CHIP benefits. We identify a full-benefit enrollee in this study as an enrollee with a restricted benefits flag in the data record equal to one for any month of enrollment in the calendar year.
State-specific FFS data anomalies are documented in the MSIS and MAX anomaly tables.
Encounter claims in the LT file are clustered among very few states in MAX 2008 data. After imposing our analysis criteria, there were too few encounters for a cross-state analysis of LT data.
References
- Borck R, Dodd AH, Zlatinov A, Verghese S, Malsberger R, Petroski C. The Medicaid Analytic eXtract 2008 Chartbook. Washington, DC: Centers for Medicare & Medicaid Services; 2012. [Google Scholar]
- Byrd V, Verdier J, Nysenbaum J, Schoettle A. Technical Assistance for Medicaid Managed Care Encounter Reporting to the Medicaid Statistical Information System, 2010. Washington, DC: Mathematica Policy Research; 2011. Feb, Final report submitted to Centers for Medicare & Medicaid Services. [Google Scholar]
- Bagchi A, Verdier J, Esposito D. Table 1. Washington, DC: Centers for Medicare & Medicaid Services; 2012. Mar, Statistical Compendium: Medicaid Pharmacy Benefit Use and Reimbursement in 2008. [Google Scholar]