Abstract
Objectives
Individuals with multiple (>2) chronic conditions (MCC) present many challenges to the health care system, such as effective coordination of care and cost containment. To assist health policy makers and to fill research gaps on MCC, we describe state-level variation of MCC among Medicare beneficiaries, with a focus on those with six or more conditions.
Methods:
Using Centers for Medicare & Medicaid Services administrative data for 2011, we characterized a beneficiary as having MCC by counting the number of conditions from a set of fifteen conditions, which were identified using diagnosis codes on the claims. The study population included fee-for-service beneficiaries residing in the 50 U.S. states and Washington, DC
Results:
Among beneficiaries with six or more chronic conditions, prevalence rates were lowest in Alaska and Wyoming (7%) and highest in Florida and New Jersey (18%); readmission rates were lowest in Utah (19%) and highest in Washington, DC (31%); the number of emergency department visits per beneficiary were lowest in New York and Florida (1.6) and highest in Washington, DC (2.7); and Medicare spending per beneficiary was lowest in Hawaii ($24,086) and highest in Maryland, Washington, DC, and Louisiana (over $37,000).
Conclusion:
These findings expand upon prior research on MCC among Medicare beneficiaries at the national level and demonstrate considerable state-level variation in the prevalence, health care utilization, and Medicare spending for beneficiaries with MCC. State-level data on MCC is important for decision making aimed at improved program planning, financing, and delivery of care for individuals with MCC.
Keywords: Administrative Data Uses, Chronic Disease, Geographic, Spatial Factors, Small area variations, Medicare
Introduction
While it is estimated that approximately one in four Americans have at least two chronic conditions that require ongoing medical care (Anderson, 2010), the burden of multiple (≥2) chronic conditions (MCC) among Medicare beneficiaries is even greater. Over two-thirds of Medicare beneficiaries in traditional Medicare, also known as fee-for-service, have two or more chronic conditions and about 1 in 7 (14%) have 6 or more. Among beneficiaries with three or more chronic conditions, one-third have hypertension and high cholesterol along with diabetes or ischemic heart disease (Centers for Medicare & Medicaid Services, 2012a). The co-occurrence of chronic conditions has far-reaching implications for treatment, coordination of care, and health care costs among Medicare beneficiaries. Beneficiaries with MCC have increased hospital readmissions and emergency department visits, which are commonly cited indicators of poor quality or poorly coordinated care, and important drivers of increased Medicare spending. MCC's burden is starkly demonstrated by the 14% of beneficiaries with 6 or more chronic conditions that account for almost half of total Medicare spending (Centers for Medicare & Medicaid Services, 2012a).
In 2010, the Department of Health and Human Services released a strategic framework on MCC to help in improving coordination of clinical services, public health programs, and research priorities relating to MCC. One of the framework's four main goals was to facilitate research addressing key knowledge gaps about MCC (U.S. Department of Health and Human Services, 2010). Previous research on MCC has focused on national-level populations—such as community-dwelling adults (Hwang, Weller, Ireys, & Anderson, 2001; Anderson, 2010), Medicare beneficiaries (Wolff, Starfied, & Anderson, 2002; Lochner & Cox, in press), and veteran populations (Lee et al., 2007; Steinman et al., 2012). While these studies have highlighted the important issue of MCC for health care, characterizing geographic variations of MCC would be useful for targeting service delivery, resource projections, and program planning. This would be particularly useful at the state-level, as states increasingly play a key role in the financing, regulation, and delivery of health care, yet few data sources support this level of analysis and, consequently, little is known about differences in health care use and spending across states for populations with MCC. Data from the Centers for Medicare & Medicaid Services (CMS) can fill these research gaps. We, therefore, used CMS data to examine state-level prevalence, utilization, and expenditure patterns of MCC to assist health policy makers and to further the research objectives of the HHS strategic framework, focusing on beneficiaries with six or more chronic conditions (MCC6+). In this report, we describe state-level patterns of MCC6+ populations in terms of prevalence, hospital readmission rates, emergency department visits, and Medicare spending.
Methods
Data Source and Study Population
Medicare is the United States' Federal health insurance program for persons aged 65 years or older, persons under age 65 years with certain disabilities, and persons of any age with end-stage renal disease (ESRD). We examined state-level patterns in MCC using the CMS administrative enrollment and claims data, for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse, a database with 100% of Medicare enrollment and fee-for-service claims data (Chronic Condition Data Warehouse, 2012).
The study population is limited to fee-for-service Medicare beneficiaries residing in the 50 U.S. states and Washington, DC, and who were continuously enrolled in Medicare fee-for-service parts A and B for 2011. We excluded beneficiaries with any Medicare Advantage enrollment during the year—since claims data are not available for these beneficiaries—and those who first became eligible for Medicare after January 1st of the calendar year. We included beneficiaries who died during the year up to their date of death if they met the other inclusion criteria. For 2011, the study population included 31.6 million Medicare beneficiaries and represented 61% of all Medicare beneficiaries enrolled during 2011. Most beneficiary exclusions were for persons enrolled in Medicare Advantage, which represented 13.4 million (approximately 26%) of the total Medicare population in 2011.
Measures
Chronic Conditions
The CMS Chronic Condition Warehouse database includes pre-defined indicators for 27 chronic conditions (Chronic Condition Data Warehouse, 2012). For this characterization of MCC, we included 18 of these conditions that are consistent with the parameters outlined in a recent report from the Department of Health and Human Services (Goodman, Posner, Huang, Parekh, & Koh, in press). Since we collapsed the four cancer sites into one cancer category, we included the following 15 conditions: arthritis, Alzheimer's disease and related dementia, asthma, atrial fibrillation, cancer (breast, colorectal, lung, and prostate), chronic kidney disease, chronic obstructive pulmonary disease (COPD), depression, diabetes, heart failure, hyperlipidemia, hypertension, ischemic heart disease, osteoporosis, and stroke. A Medicare beneficiary was considered to have a chronic condition if the CMS administrative data had a claim indicating that the beneficiary was receiving a service or treatment for the specific condition. For example, to identify a beneficiary with hyperlipidemia during 2010, at least 1 inpatient, skilled nursing facility, or home health claim, or 2 outpatient or carrier claims had to include any of the following diagnosis codes from the International Classification of Diseases, 9th Revision, Clinical Modification: 272.0, 272.1, 272.2, 272.3, 272.4. (Detailed information on the identification of chronic conditions is available at the Chronic Condition Data Warehouse, 2012). Chronic conditions were counted and grouped into four categories (0–1, 2–3, 4–5 and 6 or more).
Hospital Readmissions
A readmission was defined as an admission to an acute care hospital for any cause within 30 days of discharge from an acute care hospital. Except when the patient died during the stay, each inpatient stay was classified as an index admission, a readmission, or both. Transfer from one acute care hospital to another on the same day was counted as a single stay and, thus, one index admission. Under this definition, a readmission for a given year (e.g., 2011) could occur as late as January 30 of the following year (e.g., 2012) (Centers for Medicare & Medicaid Services, 2013a). Readmission rates are calculated as the number of readmissions divided by the number of admissions and expressed as a percentage of all admissions.
Emergency Department Visits
The total number of emergency department visits a beneficiary had in 2011 included visits where the beneficiary was released from the outpatient setting and where the beneficiary was admitted to an inpatient setting. ED visits are presented as the number of visits per beneficiary (Centers for Medicare & Medicaid Services, 2013a).
Medicare Spending
Medicare spending included total Medicare payments for all Medicare covered services in 2011 and is presented as Medicare spending per beneficiary (per capita). To make Medicare payments across geographic areas comparable, and to reflect variation due to utilization patterns, payments have been standardized to remove geographic differences in payment rates for individual services, such as those that account for local wages or input prices (Centers for Medicare & Medicaid Services, 2013b).
Results
Exhibit 1 presents the characteristics of Medicare fee-for-service beneficiaries by state in 2011. Nationally, beneficiaries aged 65 years and older represented 82.6% of the Medicare population, but by state ranged from 73.9% in West Virginia to 87.7% in Arizona. Overall, while 9.7% of beneficiaries were non-Hispanic Black and 5.6% were Hispanic, there was considerable racial and ethnic variation by state: the percentage of non-Hispanic Black beneficiaries was lowest in Idaho and Montana (0.2%) and highest in Washington, DC (65.4%), followed by Mississippi (27.8%) and Louisiana (26.8%). The percentage of Hispanic beneficiaries was lowest in North Dakota, Maine, Kentucky, and West Virginia (all 0.4%), and highest in New Mexico (29.7%) followed by Texas (17.6%) and California (17.1%). More than one in five beneficiaries (22.1%) was enrolled in both Medicare and Medicaid, also referred to as dual-eligibles: the percentage of dual-eligibles was lowest in Arizona (11.1%) and Utah (11.8%) and highest in Maine (40.3%) and Washington, DC (36.1%).
Exhibit 1. Characteristics of the Medicare Population by State: 2011.
| Age1 | Sex | Race/ethnicity2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Less than 65 years | 65 years and older | Men | Women | Non Hispanic White | Non Hispanic Black | Hispanic | Asian/PI | Medicare-Medicaid enrollee3 | |
| Percentage (%) | |||||||||
| National | 17.5 | 82.6 | 44.4 | 55.6 | 81.1 | 9.7 | 5.6 | 2.2 | 22.1 |
| Alabama | 22.4 | 77.7 | 43.7 | 56.3 | 78.9 | 19.9 | 0.5 | 0.3 | 22.3 |
| Alaska | 17.4 | 82.6 | 49.4 | 50.6 | 74.7 | 2.7 | 2.3 | 3.8 | 24.7 |
| Arizona | 12.3 | 87.7 | 47.6 | 52.4 | 84.7 | 2.3 | 7.8 | 1.0 | 11.1 |
| Arkansas | 21.3 | 78.7 | 44.7 | 55.3 | 87.3 | 10.7 | 0.9 | 0.4 | 23.7 |
| California | 17.3 | 82.7 | 45.8 | 54.2 | 64.6 | 5.9 | 17.1 | 10.2 | 32.0 |
| Colorado | 16.0 | 84.0 | 46.4 | 53.6 | 84.9 | 3.2 | 9.5 | 1.2 | 15.4 |
| Connecticut | 14.4 | 85.6 | 42.6 | 57.4 | 86.6 | 6.3 | 4.8 | 1.2 | 26.4 |
| Delaware | 15.3 | 84.7 | 44.3 | 55.7 | 81.1 | 14.9 | 1.9 | 1.1 | 16.7 |
| Florida | 13.2 | 86.8 | 44.9 | 55.1 | 81.7 | 7.7 | 8.8 | 1.0 | 19.3 |
| Georgia | 20.0 | 80.0 | 44.1 | 55.9 | 75.3 | 21.7 | 1.4 | 1.0 | 23.1 |
| Hawaii | 12.9 | 87.2 | 47.0 | 53.0 | 28.1 | 1.0 | 5.8 | 54.2 | 16.3 |
| Idaho | 16.8 | 83.2 | 47.3 | 52.7 | 94.2 | 0.2 | 3.3 | 0.6 | 17.7 |
| Illinois | 14.7 | 85.4 | 43.3 | 56.8 | 80.7 | 11.6 | 5.0 | 1.7 | 18.7 |
| Indiana | 17.5 | 82.5 | 43.6 | 56.4 | 90.4 | 7.0 | 1.5 | 0.5 | 18.6 |
| Iowa | 13.6 | 86.5 | 43.4 | 56.6 | 96.5 | 1.5 | 0.8 | 0.5 | 17.2 |
| Kansas | 15.0 | 85.0 | 43.6 | 56.4 | 91.5 | 4.2 | 2.5 | 0.7 | 16.2 |
| Kentucky | 24.8 | 75.2 | 45.7 | 54.3 | 93.6 | 5.2 | 0.4 | 0.3 | 24.9 |
| Louisiana | 22.8 | 77.2 | 44.9 | 55.2 | 70.1 | 26.8 | 1.8 | 0.7 | 31.6 |
| Maine | 22.0 | 78.0 | 45.3 | 54.7 | 97.8 | 0.4 | 0.4 | 0.3 | 40.3 |
| Maryland | 13.9 | 86.2 | 42.7 | 57.3 | 72.7 | 21.8 | 1.8 | 2.7 | 15.7 |
| Massachusetts | 20.0 | 80.0 | 43.1 | 56.9 | 87.1 | 4.4 | 5.1 | 1.9 | 28.4 |
| Michigan | 20.3 | 79.8 | 44.4 | 55.6 | 83.6 | 12.6 | 1.6 | 0.9 | 20.7 |
| Minnesota | 21.6 | 78.4 | 46.1 | 53.9 | 93.0 | 2.9 | 1.0 | 1.2 | 19.7 |
| Mississippi | 23.8 | 76.2 | 43.8 | 56.2 | 70.9 | 27.8 | 0.5 | 0.4 | 32.0 |
| Missouri | 19.6 | 80.4 | 44.3 | 55.7 | 90.1 | 7.8 | 0.9 | 0.5 | 21.0 |
| Montana | 14.4 | 85.6 | 47.3 | 52.8 | 93.9 | 0.2 | 1.0 | 0.3 | 15.7 |
| Nebraska | 12.9 | 87.1 | 43.4 | 56.6 | 93.9 | 2.7 | 1.8 | 0.5 | 16.2 |
| Nevada | 15.9 | 84.1 | 48.5 | 51.5 | 78.3 | 6.8 | 8.2 | 4.3 | 16.1 |
| New Hampshire | 16.8 | 83.2 | 44.1 | 55.9 | 96.7 | 1.0 | 0.9 | 0.5 | 16.3 |
| New Jersey | 13.2 | 86.8 | 42.1 | 57.9 | 79.0 | 10.1 | 7.1 | 2.6 | 15.8 |
| New Mexico | 19.8 | 80.3 | 47.5 | 52.5 | 61.0 | 1.7 | 29.7 | 0.6 | 23.9 |
| New York | 17.9 | 82.1 | 43.2 | 56.8 | 77.5 | 10.1 | 7.4 | 3.2 | 28.1 |
| North Carolina | 19.5 | 80.5 | 43.3 | 56.7 | 78.1 | 18.8 | 1.1 | 0.7 | 22.7 |
| North Dakota | 12.5 | 87.5 | 44.0 | 56.0 | 95.7 | 0.3 | 0.4 | 0.3 | 15.7 |
| Ohio | 20.1 | 80.0 | 44.9 | 55.1 | 87.8 | 9.6 | 1.2 | 0.7 | 22.4 |
| Oklahoma | 18.3 | 81.7 | 44.5 | 55.5 | 84.0 | 5.3 | 1.6 | 0.6 | 20.8 |
| Oregon | 16.8 | 83.2 | 47.9 | 52.2 | 92.9 | 1.1 | 2.6 | 1.4 | 17.1 |
| Pennsylvania | 17.0 | 83.0 | 43.3 | 56.8 | 89.5 | 6.8 | 1.9 | 1.0 | 19.7 |
| Rhode Island | 23.5 | 76.5 | 43.4 | 56.6 | 87.4 | 3.7 | 6.1 | 1.0 | 27.5 |
| South Carolina | 18.6 | 81.4 | 44.3 | 55.7 | 77.1 | 21.1 | 0.8 | 0.4 | 18.6 |
| South Dakota | 12.4 | 87.6 | 44.6 | 55.4 | 93.9 | 0.3 | 0.5 | 0.3 | 16.8 |
| Tennessee | 19.9 | 80.1 | 44.3 | 55.7 | 87.7 | 10.7 | 0.6 | 0.5 | 24.1 |
| Texas | 15.9 | 84.2 | 44.5 | 55.5 | 70.1 | 9.8 | 17.6 | 1.7 | 22.0 |
| Utah | 14.7 | 85.3 | 45.7 | 54.3 | 92.5 | 0.6 | 4.1 | 1.4 | 11.8 |
| Vermont | 17.9 | 82.2 | 45.1 | 54.9 | 97.5 | 0.4 | 0.6 | 0.4 | 27.2 |
| Virginia | 15.5 | 84.6 | 43.7 | 56.3 | 79.2 | 16.2 | 1.5 | 2.2 | 16.9 |
| Washington | 16.4 | 83.6 | 46.1 | 53.9 | 87.7 | 2.6 | 3.0 | 4.2 | 20.0 |
| Washington, DC | 19.5 | 80.5 | 41.8 | 58.2 | 28.8 | 65.4 | 3.2 | 1.4 | 36.1 |
| West Virginia | 26.1 | 73.9 | 47.8 | 52.2 | 96.3 | 2.6 | 0.4 | 0.2 | 26.4 |
| Wisconsin | 17.2 | 82.8 | 44.1 | 55.9 | 92.5 | 3.8 | 1.5 | 0.8 | 20.9 |
| Wyoming | 13.0 | 87.1 | 47.0 | 53.1 | 93.5 | 0.5 | 3.8 | 0.4 | 14.2 |
NOTES.
Medicare beneficiaries younger than 65 primarily are disabled.
Row totals do not sum to 100%, because "other" group not shown. Race/ethnicity is based upon an enhancement to the SSA race code, which uses geography and Census surname information to improve the classification of Hispanic and Asian/Pacific Islander Medicare beneficiaries. More information is available at http://www.cms.gov/Research-Statistics-Data-and-Systems/Research/HealthCareFinancingReview/downloads/08springpg27.pdf
Medicare beneficiaries also enrolled in Medicaid are known as "dual eligible."
SOURCE: CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse (www.ccwdata.org).
In 2011, approximately two-thirds (67.3%) of Medicare beneficiaries had two or more chronic conditions (MCC2+) and 14% had six or more (MCC6+). Prevalence rates were lowest in Alaska and Wyoming (50% for MCC2+ and 7% for MCC6+), and highest in Florida and New Jersey (75% for MCC2+ and 18% for MCC6+; Exhibit 2).
Exhibit 2. Prevalence of Multiple Chronic Conditions among Medicare Beneficiaries by State: 2011.
| Number of Chronic Conditions | ||||
|---|---|---|---|---|
| 0 to 1 | 2 to 3 | 4 to 5 | 6+ | |
| Prevalence (%) | ||||
| National | 32.7 | 31.5 | 21.8 | 14.0 |
| Alabama | 30.0 | 33.2 | 23.1 | 13.8 |
| Alaska | 50.1 | 29.0 | 14.0 | 6.9 |
| Arizona | 37.0 | 31.9 | 20.1 | 11.0 |
| Arkansas | 35.9 | 31.7 | 20.7 | 11.8 |
| California | 36.1 | 30.1 | 20.6 | 13.2 |
| Colorado | 44.4 | 30.0 | 16.6 | 9.1 |
| Connecticut | 30.3 | 33.1 | 22.5 | 14.2 |
| Delaware | 25.9 | 34.0 | 25.2 | 14.9 |
| Florida | 25.6 | 30.9 | 25.3 | 18.2 |
| Georgia | 30.9 | 32.8 | 22.8 | 13.5 |
| Hawaii | 33.4 | 35.3 | 21.8 | 9.5 |
| Idaho | 44.0 | 30.3 | 17.2 | 8.6 |
| Illinois | 31.7 | 31.8 | 21.7 | 14.9 |
| Indiana | 31.9 | 32.1 | 21.8 | 14.3 |
| Iowa | 37.1 | 32.9 | 19.7 | 10.3 |
| Kansas | 35.6 | 32.5 | 20.4 | 11.6 |
| Kentucky | 30.4 | 31.5 | 22.9 | 15.3 |
| Louisiana | 30.5 | 30.9 | 22.9 | 15.7 |
| Maine | 36.3 | 32.6 | 19.6 | 11.5 |
| Maryland | 29.9 | 32.8 | 23.1 | 14.2 |
| Massachusetts | 32.7 | 33.1 | 21.0 | 13.2 |
| Michigan | 30.5 | 30.2 | 22.3 | 16.9 |
| Minnesota | 46.0 | 29.7 | 15.9 | 8.3 |
| Mississippi | 33.4 | 32.8 | 21.3 | 12.5 |
| Missouri | 32.5 | 31.5 | 21.9 | 14.1 |
| Montana | 46.6 | 30.3 | 15.6 | 7.5 |
| Nebraska | 40.0 | 31.0 | 18.5 | 10.6 |
| Nevada | 38.7 | 30.4 | 19.7 | 11.2 |
| New Hampshire | 35.9 | 33.2 | 19.8 | 11.2 |
| New Jersey | 26.5 | 30.4 | 25.3 | 17.9 |
| New Mexico | 41.4 | 30.8 | 18.5 | 9.3 |
| New York | 30.0 | 30.0 | 23.4 | 16.6 |
| North Carolina | 31.4 | 34.4 | 21.9 | 12.3 |
| North Dakota | 40.3 | 31.0 | 18.3 | 10.3 |
| Ohio | 30.1 | 31.1 | 22.8 | 16.1 |
| Oklahoma | 33.7 | 30.9 | 21.5 | 14.0 |
| Oregon | 43.5 | 31.3 | 16.9 | 8.3 |
| Pennsylvania | 29.1 | 32.0 | 23.4 | 15.6 |
| Rhode Island | 30.5 | 32.8 | 22.9 | 13.8 |
| South Carolina | 30.1 | 34.9 | 22.8 | 12.2 |
| South Dakota | 41.3 | 31.5 | 17.7 | 9.5 |
| Tennessee | 31.1 | 32.3 | 22.2 | 14.5 |
| Texas | 31.7 | 29.8 | 22.2 | 16.3 |
| Utah | 43.7 | 30.3 | 17.0 | 8.9 |
| Vermont | 41.6 | 33.3 | 16.8 | 8.3 |
| Virginia | 32.1 | 34.0 | 21.8 | 12.2 |
| Washington | 42.8 | 30.9 | 17.3 | 9.0 |
| Washington, DC | 36.6 | 30.5 | 20.4 | 12.5 |
| West Virginia | 30.5 | 31.6 | 23.0 | 14.9 |
| Wisconsin | 37.6 | 31.5 | 19.5 | 11.3 |
| Wyoming | 50.2 | 28.3 | 14.4 | 7.2 |
SOURCE: CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse (www.ccwdata.org).
Exhibits 3 and 4 present state-level hospital readmission and ED visit rates, respectively, by number of beneficiary's chronic conditions for 2011. Nationally, 19.1% of Medicare hospital admissions were followed by a readmission within 30 days, with readmission rates increasing directly in relation to the number of chronic conditions. Nationally, the readmission rate for beneficiaries without MCC was 8.9% and increased to 25.0% for beneficiaries with MCC6+. Across states, the readmission rate for beneficiaries with MCC6+ was lowest in Utah (19.5%) and highest in Washington, DC (30.5%). Among Medicare beneficiaries with MCC6+, hospital readmissions were 30–50% higher in Washington, DC, West Virginia, and Maryland when compared with Utah and Idaho.
Exhibit 3. Hospital Readmissions within 30-days among Medicare Beneficiaries by Multiple Chronic Conditions by State: 2011.
| Number of Chronic Conditions | |||||
|---|---|---|---|---|---|
| Overall | 0 to 1 | 2 to 3 | 4 to 5 | 6+ | |
| Readmission rate (%) | |||||
| National | 19.1 | 8.9 | 10.3 | 13.5 | 25.0 |
| Alabama | 18.1 | 9.0 | 10.0 | 13.3 | 24.0 |
| Alaska | 14.9 | 8.4 | 10.0 | 13.1 | 21.3 |
| Arizona | 18.0 | 7.7 | 9.6 | 13.2 | 24.8 |
| Arkansas | 18.5 | 8.7 | 10.2 | 13.9 | 25.1 |
| California | 19.3 | 8.6 | 10.5 | 13.9 | 25.3 |
| Colorado | 15.7 | 7.7 | 9.7 | 13.1 | 21.7 |
| Connecticut | 19.3 | 10.4 | 11.2 | 14.2 | 24.8 |
| Delaware | 17.8 | 8.1 | 8.6 | 12.2 | 22.9 |
| Florida | 19.5 | 9.2 | 10.2 | 12.6 | 24.4 |
| Georgia | 18.7 | 9.2 | 10.1 | 13.6 | 24.5 |
| Hawaii | 16.3 | 7.5 | 10.4 | 11.3 | 22.5 |
| Idaho | 14.2 | 7.3 | 8.7 | 11.9 | 20.4 |
| Illinois | 21.1 | 9.5 | 11.5 | 14.5 | 27.1 |
| Indiana | 18.5 | 8.1 | 9.7 | 12.4 | 24.4 |
| Iowa | 16.6 | 9.0 | 10.2 | 13.5 | 22.3 |
| Kansas | 16.6 | 7.9 | 9.7 | 12.8 | 22.5 |
| Kentucky | 20.1 | 7.9 | 9.7 | 13.6 | 26.1 |
| Louisiana | 19.8 | 10.3 | 10.9 | 14.3 | 25.0 |
| Maine | 17.0 | 8.1 | 10.2 | 12.8 | 22.6 |
| Maryland | 21.3 | 10.4 | 11.3 | 14.5 | 27.4 |
| Massachusetts | 19.9 | 9.2 | 12.0 | 14.6 | 25.9 |
| Michigan | 20.1 | 8.3 | 9.6 | 12.9 | 25.8 |
| Minnesota | 17.6 | 9.7 | 11.2 | 14.6 | 24.7 |
| Mississippi | 19.6 | 10.6 | 11.4 | 15.1 | 25.7 |
| Missouri | 19.4 | 8.6 | 10.5 | 13.4 | 25.7 |
| Montana | 14.7 | 7.6 | 9.3 | 13.4 | 20.8 |
| Nebraska | 16.3 | 8.0 | 9.9 | 12.3 | 22.7 |
| Nevada | 19.1 | 8.4 | 10.4 | 14.1 | 26.1 |
| New Hampshire | 17.4 | 7.2 | 9.9 | 13.2 | 23.3 |
| New Jersey | 21.2 | 9.6 | 10.6 | 13.9 | 26.2 |
| New Mexico | 16.5 | 7.8 | 10.2 | 13.6 | 22.6 |
| New York | 20.7 | 10.5 | 11.2 | 14.2 | 26.3 |
| North Carolina | 18.2 | 9.4 | 10.1 | 13.2 | 24.1 |
| North Dakota | 16.7 | 11.3 | 9.1 | 13.5 | 22.7 |
| Ohio | 20.2 | 8.4 | 10.6 | 13.3 | 25.9 |
| Oklahoma | 17.8 | 7.9 | 10.0 | 13.0 | 23.5 |
| Oregon | 15.3 | 7.8 | 8.9 | 12.8 | 21.8 |
| Pennsylvania | 19.0 | 8.6 | 9.9 | 13.2 | 24.4 |
| Rhode Island | 20.0 | 11.8 | 12.2 | 13.9 | 25.9 |
| South Carolina | 17.5 | 9.0 | 9.6 | 12.5 | 23.6 |
| South Dakota | 15.6 | 8.5 | 9.3 | 13.2 | 21.3 |
| Tennessee | 19.4 | 8.4 | 9.9 | 13.4 | 25.3 |
| Texas | 18.5 | 8.4 | 9.8 | 12.7 | 23.5 |
| Utah | 14.1 | 7.4 | 8.7 | 12.2 | 19.5 |
| Vermont | 16.0 | 8.2 | 10.2 | 13.1 | 22.0 |
| Virginia | 18.9 | 8.8 | 10.3 | 13.5 | 25.2 |
| Washington | 16.7 | 8.3 | 9.8 | 12.9 | 23.5 |
| Washington, DC | 23.6 | 11.1 | 13.0 | 17.7 | 30.5 |
| West Virginia | 21.4 | 8.2 | 10.4 | 14.4 | 27.7 |
| Wisconsin | 16.8 | 10.2 | 9.6 | 12.8 | 22.5 |
| Wyoming | 15.4 | 7.6 | 8.6 | 13.5 | 22.9 |
SOURCE: CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse (www.ccwdata.org).
Exhibit 4. Emergency Department Visits Among Medicare Beneficiaries by Multiple Chronic Conditions by State: 2011.
| Number of Chronic Conditions | |||||
|---|---|---|---|---|---|
| Overall | 0 to 1 | 2 to 3 | 4 to 5 | 6+ | |
| ED visits per beneficiary | |||||
| National | 0.7 | 0.2 | 0.5 | 0.8 | 2.0 |
| Alabama | 0.7 | 0.3 | 0.5 | 0.8 | 2.0 |
| Alaska | 0.6 | 0.2 | 0.6 | 1.0 | 2.3 |
| Arizona | 0.6 | 0.2 | 0.4 | 0.8 | 2.0 |
| Arkansas | 0.7 | 0.2 | 0.5 | 0.9 | 2.1 |
| California | 0.6 | 0.2 | 0.4 | 0.7 | 1.8 |
| Colorado | 0.6 | 0.2 | 0.5 | 1.0 | 2.1 |
| Connecticut | 0.7 | 0.3 | 0.5 | 0.9 | 2.0 |
| Delaware | 0.6 | 0.2 | 0.4 | 0.7 | 1.8 |
| Florida | 0.6 | 0.2 | 0.3 | 0.6 | 1.7 |
| Georgia | 0.7 | 0.3 | 0.5 | 0.9 | 2.1 |
| Hawaii | 0.5 | 0.2 | 0.3 | 0.6 | 1.8 |
| Idaho | 0.6 | 0.2 | 0.5 | 0.9 | 2.0 |
| Illinois | 0.7 | 0.2 | 0.4 | 0.8 | 2.0 |
| Indiana | 0.7 | 0.3 | 0.5 | 0.8 | 2.1 |
| Iowa | 0.6 | 0.2 | 0.5 | 0.9 | 2.0 |
| Kansas | 0.6 | 0.2 | 0.4 | 0.8 | 1.9 |
| Kentucky | 0.8 | 0.3 | 0.5 | 0.9 | 2.2 |
| Louisiana | 0.8 | 0.3 | 0.5 | 0.9 | 2.2 |
| Maine | 0.8 | 0.4 | 0.6 | 1.1 | 2.4 |
| Maryland | 0.7 | 0.2 | 0.4 | 0.8 | 2.2 |
| Massachusetts | 0.8 | 0.3 | 0.6 | 0.9 | 2.2 |
| Michigan | 0.8 | 0.3 | 0.5 | 0.8 | 2.1 |
| Minnesota | 0.6 | 0.3 | 0.6 | 1.1 | 2.2 |
| Mississippi | 0.8 | 0.3 | 0.6 | 1.1 | 2.4 |
| Missouri | 0.7 | 0.3 | 0.5 | 0.9 | 2.1 |
| Montana | 0.6 | 0.2 | 0.5 | 1.0 | 2.0 |
| Nebraska | 0.5 | 0.2 | 0.4 | 0.8 | 1.7 |
| Nevada | 0.6 | 0.2 | 0.5 | 0.8 | 2.0 |
| New Hampshire | 0.7 | 0.3 | 0.6 | 1.0 | 2.2 |
| New Jersey | 0.6 | 0.2 | 0.4 | 0.6 | 1.8 |
| New Mexico | 0.6 | 0.2 | 0.5 | 0.8 | 2.0 |
| New York | 0.6 | 0.2 | 0.4 | 0.7 | 1.6 |
| North Carolina | 0.7 | 0.3 | 0.5 | 0.9 | 2.2 |
| North Dakota | 0.6 | 0.2 | 0.5 | 0.8 | 1.8 |
| Ohio | 0.8 | 0.3 | 0.5 | 0.9 | 2.2 |
| Oklahoma | 0.7 | 0.3 | 0.5 | 0.9 | 2.1 |
| Oregon | 0.6 | 0.2 | 0.5 | 0.9 | 2.2 |
| Pennsylvania | 0.7 | 0.3 | 0.4 | 0.7 | 1.9 |
| Rhode Island | 0.8 | 0.3 | 0.5 | 0.9 | 2.2 |
| South Carolina | 0.7 | 0.3 | 0.4 | 0.8 | 2.0 |
| South Dakota | 0.5 | 0.2 | 0.4 | 0.8 | 1.7 |
| Tennessee | 0.7 | 0.2 | 0.5 | 0.9 | 2.2 |
| Texas | 0.7 | 0.2 | 0.4 | 0.7 | 1.9 |
| Utah | 0.6 | 0.2 | 0.5 | 0.9 | 1.8 |
| Vermont | 0.7 | 0.3 | 0.6 | 1.0 | 2.3 |
| Virginia | 0.7 | 0.2 | 0.5 | 0.9 | 2.2 |
| Washington | 0.6 | 0.2 | 0.5 | 0.9 | 2.2 |
| Washington, DC | 0.9 | 0.3 | 0.7 | 1.2 | 2.7 |
| West Virginia | 0.8 | 0.3 | 0.5 | 0.9 | 2.3 |
| Wisconsin | 0.6 | 0.2 | 0.5 | 0.9 | 2.0 |
| Wyoming | 0.6 | 0.2 | 0.6 | 1.1 | 2.3 |
SOURCE: CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse (www.ccwdata.org).
Nationally, the average ED visit rate was 0.7 visits per beneficiary, with rates more than eightfold greater among beneficiaries with MCC6+ when compared with beneficiaries without MCC (2.0 versus 0.2 respectively). State-level ED visits for beneficiaries with MCC6+ ranged from approximately 1.7 per beneficiary in Florida, Nebraska, and South Dakota to 2.7 in Washington, DC.
Exhibit 5 presents state-level per capita Medicare spending by number of beneficiary's chronic conditions for 2011. The average Medicare spending per beneficiary was $9,436 and increased to $31,543 for beneficiaries with MCC6+. For beneficiaries with MCC6+, per capita spending was lowest in Hawaii ($24,086), followed by Oregon, Maine, and New York (all with per capita spending < $28,000), and highest in Maryland, Washington, DC, and Louisiana at more than $37,000 per beneficiary.
Exhibit 5. Medicare Spending for Beneficiaries with Multiple Chronic Conditions by State: 2011.
| Number of Chronic Conditions | |||||
|---|---|---|---|---|---|
| Overall | 0 to 1 | 2 to 3 | 4 to 5 | 6+ | |
| Per capita Medicare spending ($) | |||||
| National | 9,436 | 2,097 | 5,677 | 11,628 | 31,543 |
| Alabama | 9,502 | 2,250 | 5,727 | 11,792 | 30,542 |
| Alaska | 6,420 | 1,894 | 5,839 | 12,541 | 29,292 |
| Arizona | 8,568 | 2,247 | 6,016 | 12,066 | 30,815 |
| Arkansas | 8,735 | 1,963 | 5,705 | 12,117 | 31,598 |
| California | 8,886 | 1,978 | 5,683 | 11,294 | 31,427 |
| Colorado | 8,080 | 2,230 | 6,664 | 13,453 | 31,524 |
| Connecticut | 9,268 | 2,236 | 5,548 | 11,247 | 29,886 |
| Delaware | 9,203 | 2,160 | 4,891 | 9,982 | 30,004 |
| Florida | 11,167 | 2,357 | 5,990 | 11,633 | 31,654 |
| Georgia | 9,370 | 2,227 | 5,781 | 11,694 | 30,584 |
| Hawaii | 5,849 | 1,428 | 3,763 | 8,040 | 24,086 |
| Idaho | 7,662 | 2,194 | 6,561 | 12,967 | 28,953 |
| Illinois | 9,828 | 1,979 | 5,469 | 11,711 | 33,139 |
| Indiana | 9,580 | 2,026 | 5,380 | 11,676 | 32,724 |
| Iowa | 8,090 | 2,314 | 5,880 | 11,821 | 28,728 |
| Kansas | 9,119 | 2,321 | 6,186 | 12,861 | 31,655 |
| Kentucky | 9,321 | 1,910 | 5,142 | 10,779 | 30,488 |
| Louisiana | 11,622 | 2,276 | 6,393 | 13,629 | 37,194 |
| Maine | 8,042 | 2,163 | 5,603 | 11,364 | 27,841 |
| Maryland | 10,715 | 2,146 | 5,752 | 12,300 | 37,642 |
| Massachusetts | 9,436 | 2,393 | 5,777 | 11,833 | 32,280 |
| Michigan | 9,956 | 2,092 | 5,458 | 11,049 | 30,723 |
| Minnesota | 7,767 | 2,160 | 6,500 | 13,743 | 31,940 |
| Mississippi | 10,420 | 2,322 | 6,538 | 14,131 | 35,854 |
| Missouri | 9,305 | 2,034 | 5,682 | 11,524 | 30,755 |
| Montana | 7,133 | 2,228 | 6,420 | 13,103 | 28,174 |
| Nebraska | 8,791 | 2,213 | 6,545 | 13,651 | 31,814 |
| Nevada | 9,079 | 1,995 | 6,059 | 12,689 | 35,463 |
| New Hampshire | 8,173 | 2,065 | 5,443 | 11,426 | 30,149 |
| New Jersey | 10,023 | 1,957 | 5,150 | 10,084 | 30,131 |
| New Mexico | 7,197 | 1,820 | 5,543 | 11,174 | 28,606 |
| New York | 9,260 | 2,018 | 5,361 | 10,361 | 27,889 |
| North Carolina | 8,768 | 2,228 | 5,502 | 11,523 | 29,704 |
| North Dakota | 7,943 | 2,050 | 6,029 | 12,413 | 28,773 |
| Ohio | 10,057 | 1,979 | 5,405 | 11,316 | 32,404 |
| Oklahoma | 9,695 | 2,038 | 5,971 | 12,512 | 32,073 |
| Oregon | 6,858 | 2,019 | 5,660 | 11,666 | 26,876 |
| Pennsylvania | 9,763 | 2,019 | 5,312 | 10,982 | 31,511 |
| Rhode Island | 8,854 | 2,170 | 5,337 | 10,868 | 28,696 |
| South Carolina | 8,975 | 2,254 | 5,542 | 11,480 | 30,631 |
| South Dakota | 7,805 | 2,097 | 5,930 | 13,022 | 29,130 |
| Tennessee | 9,626 | 2,066 | 5,510 | 11,684 | 31,891 |
| Texas | 11,084 | 2,012 | 6,046 | 12,806 | 35,534 |
| Utah | 8,419 | 2,579 | 7,077 | 13,950 | 30,997 |
| Vermont | 7,186 | 2,157 | 5,690 | 11,702 | 29,186 |
| Virginia | 8,427 | 1,979 | 5,138 | 10,929 | 30,114 |
| Washington | 7,450 | 2,070 | 5,947 | 12,088 | 29,188 |
| Washington, DC | 9,996 | 1,959 | 6,217 | 13,341 | 37,357 |
| West Virginia | 8,733 | 1,764 | 4,734 | 9,937 | 29,550 |
| Wisconsin | 8,069 | 2,031 | 5,552 | 11,568 | 29,119 |
| Wyoming | 7,475 | 2,160 | 6,912 | 14,550 | 32,666 |
SOURCE: CMS administrative enrollment and claims data for Medicare beneficiaries enrolled in the fee-for-service program for 2011, which are available from the CMS Chronic Condition Data Warehouse (www.ccwdata.org).
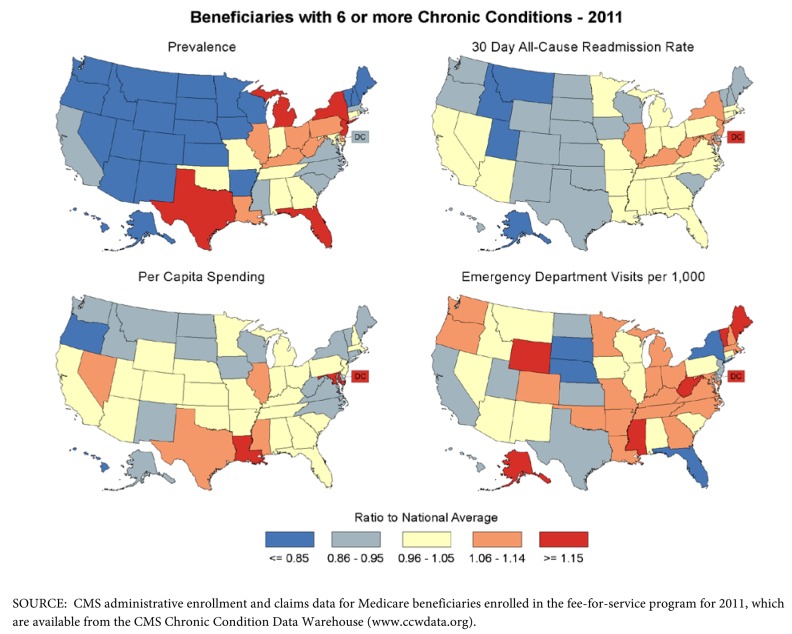
Maps of the state-to-national ratio for each measure for beneficiaries with MCC6+ are shown in Exhibit 6. For states in the Pacific and Mountain West, and for most states in the Midwest, the prevalence of beneficiaries with MCC6+ was below the national average; in comparison, the prevalence generally was higher in the Northeast and South. In particular, the prevalence of beneficiaries with MCC6+ in Florida and New Jersey was approximately 30% higher than the national average. Medicare hospital readmissions, ED visits, and Medicare spending were highest in Washington, DC where, for beneficiaries with MCC6+, they were at least 15% higher than the national average.
Exhibit 6. State Maps of Prevalence, Hospital Readmissions, ED visits, and Medicare Spending for Medicare Beneficiaries with Six or More Chronic Conditions by State: 2011.
Discussion
Descriptions of MCC among persons in the United States have been produced primarily through analyses of national level data sets and studies using data sources in individual states (Koroukian, Murray, & Madigan, 2006; Anderson, 2010; Boyd et al., 2010; Centers for Medicare & Medicaid Services, 2012a; Freid, Bernstein, & Bush, 2012; Miller, Paschall, & Svendsen, 2006). This study of over 31 million Medicare beneficiaries—the first to examine state-specific patterns of MCC among this large population—documented substantial state-level variability among Medicare beneficiaries in MCC prevalence, healthcare utilization, and expenditures across the United States. For example, the Mountain states show a low prevalence of beneficiaries with MCC6+, and most also tend to have readmission rates and per capita spending for this population that are below the national average. Examples of intriguing intrastate differences include New York and Texas. New York had a high prevalence of beneficiaries with MCC6+, although Medicare spending per beneficiary and rates for hospital readmission and ED visits were near or below the national average for each indicator. Texas had rates for readmissions and ED visits below the national average, while Medicare spending was more than 10% higher than the national average. Findings such as these highlight the need for further study of state variations in MCC that can identify specific factors underlying these patterns, such as differences in distributions of underlying risk factors, combinations and types of conditions, and the amount and the way care is delivered across the country.
This study begins to address key knowledge gaps about the burden of MCC in this important population, and directly addresses goals of the HHS Strategic Framework on MCC, specifically the fourth goal supporting targeted research about individuals with MCC (U.S. Department of Health and Human Services, 2010). Yet, to help place this study's findings and these state-level estimates in context, it is important to consider the study's methods and measures. Foremost, estimates of MCC will be influenced by the number and type of conditions that are used in a study such as this. Although we included a broad set of common chronic conditions in our determination of MCC, our list of conditions excluded several behavioral and mental health disorders, such as substance abuse disorders and schizophrenia, which were not available as pre-defined chronic conditions in our data source, the Chronic Condition Warehouse. However, our definition of MCC is based upon a standard approach that is consistent with the parameters outlined in a recent report from the Department of Health and Human Services (Goodman et al., in press). State level prevalence estimates of MCC can be affected by using diagnoses on administrative claims to infer the presence of a chronic condition. Variability in coding diagnoses can lead to both the over and under diagnosis of specific conditions and affect estimates of chronic conditions (Singh, 2009). Also, there is evidence that regional variation in care is associated with the supply of health care resources, which can affect the state-level prevalence of MCC. In states where there are more health care resources, more care is received and more claims are generated (Wennberg, Fisher, Goodman, & Skinner, 2008). Thus, in places where more health care resources are available, the likelihood that diagnoses will be identified may be increased. Finally, these state-level estimates are measures of the overall magnitude of MCC in the Medicare population and do not take into account differences in the composition of beneficiaries across states. While state differences in beneficiary characteristics, such as the proportion of disabled or dually-eligible beneficiaries, may account for some of the observed state-to-state variability, these estimates—particularly since they represent the first examination of state-level patterns of MCC—are more useful for the planning and delivery of health care services at the state-level.
States play a key role in health monitoring, surveillance, and program planning, and because states are attentive to the rising health care costs of an aging population that is living longer, but with more chronic illness, states also must address the regulation, financing, and delivery of health care. In addition, states are taking a leadership role in health care reform and are important partners in initiatives aimed at improving the quality, safety, and affordability of health care, as exemplified by programs such as the Partnership for Patients, Health Care Innovation Awards, and the State Innovation Models (see http://partnershipforpatients.cms.gov/ and http://innovation.cms.gov/). For these reasons, state-level data sources that provide timely, quality, and relevant data are important and necessary to inform health policy.
Like other well established examples of state-level data systems, such as the Behavioral Risk Factor Surveillance System (BRFSS; Centers for Disease Control and Prevention, 2013) and the Youth Risk Behavior Surveillance System (YRBSS; (Centers for Disease Control and Prevention, 2004), CMS is making available new public-use data resources on chronic conditions among Medicare beneficiaries. These resources can further support studies of this kind, including an interactive analytic dashboard that allows for the examination of geographic MCC patterns (Centers for Medicare & Medicaid Services, 2012b, available at www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/index.html). This study, also, may provide a foundation for conducting similar analyses at sub-state and other jurisdictional levels that are more local—including, for example, hospital referral regions, counties, and communities—where strategies, interventions, and other health care services can be optimally tailored to individuals and populations with MCC.
Footnotes
Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Department of Health & Human Services or its operating divisions, the Centers for Medicare & Medicaid Services and Centers for Disease Control and Prevention.
References
- Anderson G. Chronic Care: Making the Case for Ongoing Care. 2010 Retrieved from http://www.rwjf.org/content/rwjf/en/research-publications/find-rwjf-research/2010/01/chronic-care.html.
- Boyd C, Leff B, Weiss C, Wolff J, Clark R, Richards T. Full Report: Clarifying Multimorbidity to Improve Targeting and Delivery of Clinical Services for Medicaid Populations. Center for Health Care Strategies, Inc.; 2010. December 2010. Retrieved from http://www.chcs.org/usr_doc/Clarifying_Multimorbidity_for_Medicaid_report-FINAL.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2013. Retrieved from http://www.cdc.gov/brfss/index.htm. [Google Scholar]
- Centers for Disease Control and Prevention. Methodology of the Youth Risk Behavior Surveillance System. MMWR. Recommendations and Reports: Morbidity and Mortality Weekly Report. 2004;53(RR-12):1–13. [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. Chronic Conditions among Medicare Beneficiaries, Chartbook. 2012 Edition . Baltimore, MD: 2012a. 2012. Retrieved from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/2012ChartBook.html. [Google Scholar]
- Centers for Medicare & Medicaid Services. Chronic Conditions. 2012b Retrieved from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/index.html.
- Centers for Medicare & Medicaid Services. Geographic Variation Public Use File: A Methodological Overview. Baltimore, MD: 2013a. 2013. Retrieved from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/index.html. [Google Scholar]
- Centers for Medicare & Medicaid Services. Geographic Variation Public Use File: Technical Supplement on Standardization. Baltimore, MD: 2013b. 2013. Retrieved from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/index.html. [Google Scholar]
- Chronic Condition Data Warehouse. Chronic Condition Categories. 2012 Retrieved from http://www.ccwdata.org/chronic-conditions/index.htm.
- Freid VM, Bernstein AB, Bush MA. NCHS data brief, No. 100. Hyattsville, MD: National Center for Health Statistics; 2012. Multiple Chronic Conditions Among Adults Age 45 and Over: Trends Over the Past 10 Years. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db100.pdf. [PubMed] [Google Scholar]
- Goodman RA, Posner S, Huang ES, Parekh A, Koh HK. Defining and Measuring Chronic Conditions: Imperatives for Research, Policy, Program, and Practice. Preventing Chronic Disease. doi: 10.5888/pcd10.120239. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang W, Weller W, Ireys H, Anderson G. Out-of-Pocket Medical Spending for Care of Chronic Conditions. Health Affairs. 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- Koroukian SM, Murray P, Madigan E. Comorbidity, Disability, and Geriatric Syndromes in Elderly Cancer Patients Receiving Home Health Care. Journal of Clinical Oncology. 2006;24:2304–2310. doi: 10.1200/JCO.2005.03.1567. [DOI] [PubMed] [Google Scholar]
- Lee TA, Shields AE, Vogeli C, Gibson TB, Woong-Sohn M, Marder WD, Weiss KB. Mortality Rates in Veterans with Multiple Chronic Conditions. Journal of General Internal Medicine. 2007;22(Suppl 3):403–407. doi: 10.1007/s11606-007-0277-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner KA, Cox CS. Chronic Conditions Among Medicare Beneficiaries. Preventing Chronic Disease. doi: 10.5888/pcd10.120137. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BJ, Paschall CB, Svendsen DP. Mortality and Medical Comorbidity among Patients with Serious Mental Illness. Psychiatric Services (Washington, DC) 2006;57(10):1482–1487. doi: 10.1176/appi.ps.57.10.1482. [DOI] [PubMed] [Google Scholar]
- Singh JA. Accuracy of Veterans Affairs Databases for Diagnoses of Chronic Diseases. Preventing Chronic Disease. 2009;6(4):A126. Retrieved from http://www.cdc.gov/pcd/issues/2009/oct/08_0263.htm. [PMC free article] [PubMed] [Google Scholar]
- Steinman MA, Lee SJ, Boscardin WJ, Miao Y, Fung KZ, Moore KL, Schwartz JB. Patterns of Multimorbidity in Elderly Veterans. Journal of the American Geriatrics Society. 2012;60(10):1872–1880. doi: 10.1111/j.1532-5415.2012.04158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Multiple Chronic Conditions—A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. 2010 Retrieved from http://www.hhs.gov/ash/initiatives/mcc/mcc_framework.pdf.
- Wennberg JE, Fisher ES, Goodman DC, Skinner JS. Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care. 20082008 Retrieved from http://www.dartmouthatlas.org/downloads/atlases/2008_Chronic_Care_Atlas.pdf. [PubMed]
- Wolff JL, Starfied B, Anderson G. Prevalence, Expenditures, and Complication s of Multiple Chronic Conditions in the Elderly. Archives of Internal Medicine. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]