Abstract
Aims:
Primary cysts and tumors of the ovary alongwith torsion are often regarded as an indication for open oophorectomy because of the fear of leaving an ischemic organ inside and chances of recurrence. We wish to report our experience of both modalities of management where we initially removed adenexal torsion by either laparoscopic salpingo-oophorectomy or oophorectomy, but later followed a more conservative approach of adenexal lesion removal with ovarian preservation.
Materials and Methods:
Retrospective review of clinical records of patients with ovarian pathology who were managed laparoscopically.
Results:
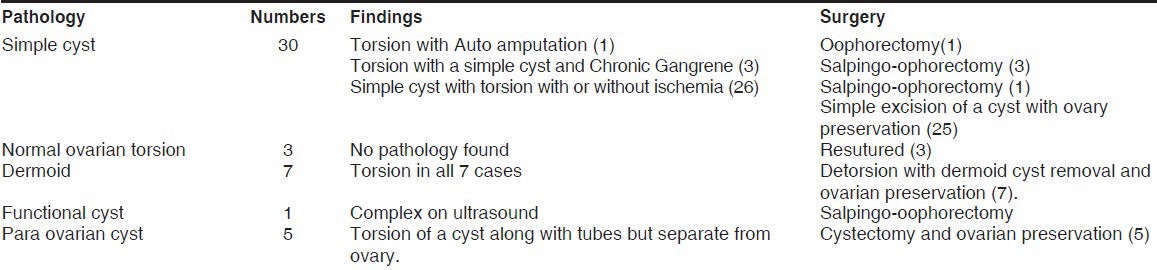
46 cases of pediatric ovarian pathology were managed between March 2006 and March 2013 in two centers by a team of surgeons. The age ranged from 1 days to 18 years (average 14.3 years) and the pathology varied from 30 cases of a simple ovarian cyst with torsion, 3 cases of ovarian torsion without any cyst, 7 cases of a dermoid cyst with torsion in all, 1 case of secreting ovarian tumor and 5 cases of a paraovarian cyst with torsion. All patients had a normal tumor marker except 1 girl with a functional ovarian tumor who had elevated LDH and estrogen levels alongwith suppressed LH and FSH. In the initial period of our study we did 1 salpingo-oophorectomy for a suspected complex lesion and two oophorectomies for torsion with a simple cyst. In the later part of our study we performed laparoscopic cystectomy and ovarian preservation in 40 cases, including 7 cases of dermoid, where we performed laparoscopic detorsion with dermoid cystectomy and ovarian preservation in the same sitting. In three cases of chronic torsion who presented to us late, we could not preserve the ovary and had to resort to salpingo-ophorectomy. Histology showed a simple corpus luteal and follicular ovarian cyst in 31 cases, a paraovarian cyst in 5 cases with mature teratoma in 7 cases. Twenty-five patients with ovarian preservation following detorsion were subjected to follow-up ultrasound, who were found to have normal shape, size and blood flow compared to the contra lateral side.
Conclusion:
We outline our experience from the management of 46 cases of various ovarian pathologies with and without ischemia and found that ovarian torsion with a benign pathology and ischemia is not a contraindication for ovarian preservation, as pointed out in the current literature.
KEY WORDS: Laparoscopic management, ovarian cyst, pediatric, torsion
INTRODUCTION
Primary cysts and tumors of the ovary are uncommon in children, are usually simple cysts or teratomas and usually benign. Collectively teratomas constitute half of all ovarian neoplasms and only 1% of these are malignant immature teratomas. Furthermore, up to 12% of cases involve both ovaries bringing into question recommendation of salpingo-oophorectomy for these lesions in children risking their long-term fertility.[1]
Adnexal torsion accounts for upto 2.7% of all cases with acute abdominal pain in children. The treatment of ovarian torsion is controversial. Although several studies suggest that untwisting the ischemic adenexal is safe and successful most of the time,[2,3] many surgeons believe that by the time the patient comes to medical attention, it is too late to salvage the twisted ovary[2,4] and advocate resection, risking their long-term fertility. Among the reasons for this are the risk of malignancy associated with torsed ovaries,[5] fear of blood clots release into the circulation after untwisting of thrombosed veins, and, most importantly, the belief that a grossly black hemorrhagic adnexa is irreversibly damaged. The aim of this study was to review our experience with ovarian torsion and to evaluate and compare the results of our initial experience with oophorectomy against the later ovary conserving approach.
MATERIALS AND METHODS
The medical records of all children who underwent laparoscopic surgery for ovarian pathology in two separate hospitals under a group of surgeons over a 7 year period were reviewed retrospectively. Information concerning patients’ demographics, diagnostic modality, intraoperative findings, postoperative complication and review of pathology reports were obtained.
Inclusion criterion for this study was all children who were diagnosed to have an adenexal lesion on ultrasonography were subjected to laparoscopy and the procedure carried out in either center by any one individual surgeon.
Surgery was performed using laparoscopic approach with a 10 mm port placed in the umbilicus through which a 10 mm or 5 mm 0 degree telescope was used and later this port was used for retrieval of the specimen. Two 5 mm working ports were used in the right and left iliac fossae. Initially, the whole peritoneal cavity was inspected as a whole to confirm the diagnosis, exclude malignancy and inspect the contra-lateral ovary. If the ovary was twisted it was untwisted and after stabilizing the ovary a superficial incision was made with diathermy on the anti-mesenteric border. The incision was gently enlarged to separate the cyst from the surrounding ovarian tissue. Hemostasis was achieved and the cyst was retrieved through a custom made bag through the 10 mm umbilical port after changing the camera to another port site. No attempt was made to pex the ovary in any case and when no cyst was found the opened-up ovary tissue was resutured back.
RESULTS
A total of 46 patients were found to have ovarian pathology who underwent laparoscopic surgery. The average age of the patient at presentation was 14.3 years (1 day-18 years).
A total of six patients underwent oophorectomy of which three patients underwent oophorectomy during the initial period of our study. One girl who underwent salpingo-oophorectomy for a suspected complex lesion was 2 year old and had a secreting simple ovarian cyst with features of precocious puberty [Figure 1]. Her LDH and estrogen levels were high with suppressed FSH and LH level. After surgery all the parameters came to normal and features of precocious puberty subsided. One patient had totally black looking ovary with torsion on laparoscopy for which it was removed [Figure 2]. One of the oophorectomy patients was a newborn in whom the ovarian cyst had undergone chronic torsion and auto-amputation. The other three patients in the later part of our study underwent salpingo-ophorectomy as they were chronic torsion of long standing. On laparoscopy they had omental and bowel adhesions. Separation of the omentum and bowel from the mass and untwisting the gangrenous friable ovary led to detachment at the point of torsion, hence could not be preserved and had to be removed. In the remaining 40 patients where the ovary was preserved, detorsion of the ovary was done in all cases with resection of the simple cyst in 25 and dermoid cyst in 7. Five patients had a paraovarian cyst where the ovary was separate from the cyst but had torsion of the tube [Figure 3] along with a cyst [Table 1]. Three patients had torsion of ovary without any pathology inside and had to be resutured after opening the ovarian tissue. A total of 46 patients had torsion with or without ischemia, of which 30 were cases of simple cyst, 7 cases of dermoid cyst, 5 cases of fimbrial cyst, 3 cases of non-pathological ovary and 1 functioning ovarian tumor. Total six patients underwent salping-ophorectomy.
Figure 1.

Signs of precocious puberty due to a secreting simple ovarian cyst in a 2 year old girl
Figure 2.
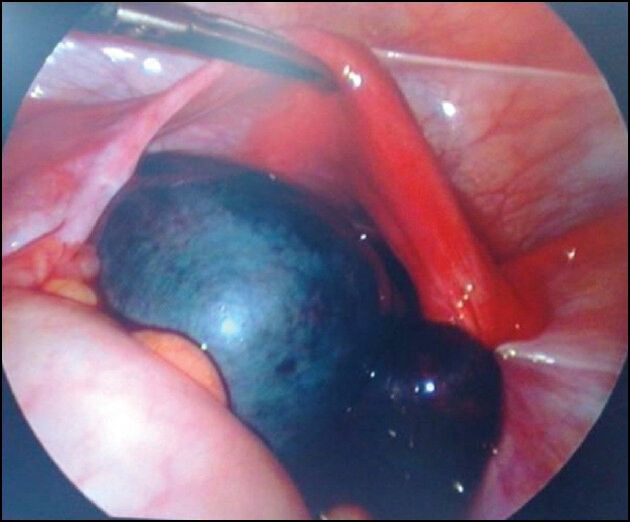
Laparoscopic view of the torsion ovary which looked totally gangrenous and was removed laparoscopically
Figure 3.

Paraovarian cyst with torsion of the tube and separate ovary seen
Table 1.
Summary of results
The presentation was that of pain, nausea and vomiting suggestive of torsion or a palpable mass. All patients underwent ultrasonography in which the diagnosis was picked up. Few patients underwent CT scan for confirmation. All patients were discharged within 48 hours of surgery. One patient had spillage of the dermoid cyst material during dissection but removed with copious saline wash. She recovered satisfactorily and had no post-operative problems. Histology was a simple ovarian corpus luteal or follicular cyst in 30 cases, a simple secreting functional cyst in 1 case, a paraovarian cyst in 5 cases with mature teratoma in 7 cases.
Twenty-five patients with ovarian preservation following detorsion were subjected to follow-up ultrasound, 5 years to 4 months after surgery and were found to have normal shape, size and blood flow compared to the contra lateral side. In two patients where the gangrenous ovary was preserved, the ovary could not be located of two subsequent scans at 6 months and 1 year follow up. Remaining patients were lost to follow up.
DISCUSSION
Our results show safety and complete functional recovery after untwisting the ischemic adnexa, regardless of the gross appearance. This was suggested in a large series of 214 cases of adnexal torsion with successful conservative treatment and no serious complications.[2]
Conservative ovarian surgery in childhood and adolescence is important for the development of normal puberty and future fertility.[7]
In large simple cysts and mature ovarian teratomas, there is little or no tendency for malignant degeneration or coexistence of malignant cells hence conservative therapy would seem more appropriate than open or laparoscopic salpingo-oophorectomy.[8]
Only the time lapse from presentation to surgery and the physician's specialty correlated with the choice of treatment. Probably with longer time, the adnexa is more likely to appear necrotic, and the surgeon is therefore likely to excise it. Recuperation of the ovary has been reported for upto 72 hours after the torsion.[9] The laparoscopic removal of these lesions has been well documented in large adult series[10] and small adolescent series.[11] It is clear from our series and from others[2,12] that a black-bluish ischemic appearance is not proof of irreversible necrosis, because the patients judged as having severely ischemic ovaries intraoperatively had normal follicular development later on.[13]
While concerns over peritonitis secondary to spillage have been raised, neither ours nor the previously mentioned studies experienced any such incidence of chemical peritonitis.[1] It has been shown that the use of an endoscopic retrieval bag significantly decreased the risk of spillage. If spillage occurs peritonitis can be minimized by adequate lavage.[14]
In addition to the clinical picture, ultrasound scan can be useful diagnostic tool. In our series it almost always reported ovarian pathology such as enlargement, cyst or mass. The diagnosis of a dermoid cyst was suggested by several sonographic findings. Although Doppler ultrasound scan has been frequently used in recent years, it can be misleading. The flow can be normal with torsion[15] leading to delay in management. Alternatively, the ovary can be viable despite no evidence of arterial or venous blood flow on Doppler ultrasound scan.[12] If torsion is suspected clinically but the ultrasound cannot establish a definitive diagnosis, laparoscopic exploration is emerging as the recommended diagnostic and therapeutic tool.[16]
When a tentative diagnosis has been reached, serum concentration of ovarian tumors, alpha-fetoprotein (AFP), B-human chorionic gonadotrophin (B-HCG) and CA 125 were obtained in order to further rule out possible malignancy. In our series all the patients had normal tumor markers and one patient with a secreting cyst had high level of estrogen and suppressed FSH and LH but her tumor markers were normal. Abnormal pathology is associated with most cases of torsion and is one reason why many Pediatric surgeons choose to resect the ovary. Descargues et al.[16] reported that normal ovaries or ovaries with benign pathology are responsible for 97% of adenexal torsions. Malignant lesions cause more inflammation and fibrosis leading to adherence to surrounding structures[4] and therefore have less chance of torsion. The most frequent etiologies of adenexal torsion are benign cystic teratomas, tubal cysts, follicular cysts and serous or mucinous cystadenomas.[2]
The presence of torsion should not deter one from ovarian cystectomy with gonadal preservation. In our series 17 patients presented with acute torsion. In 14 the ovary looked significantly ischemic where oophorectomy was done in one and the other had auto-amputated, the rest 12 ovaries were preserved. Despite appearance, we were able to dissect off the lesion from the ovary. If cystectomy is difficult in case of an ischemic edematous ovary, the patient can be reexamined in 6 to 8 weeks and secondary surgery performed at that time.[1,2] There is significant evidence to support detorsion and ovarian conservation, regardless of the ovary at operation.[2] None of our patients underwent second-look surgery and none of our patients underwent pexy to fix the ovary.
Prompt diagnosis and early intervention cannot be overemphasized, especially among pediatric surgeons who perform more oophorectomies and fewer detorsions compared with a gynecologist. This was one reason why we had performed oophorectomy in one case of gangrenous torsion and one case of simple secreting cyst. This observation underlines how important it is for surgeons to consider this diagnosis in a prepubertal girl with abdominal pain, especially in the context of similar repeated episodes suggesting recurrent torsion/detorsion.[2]
In conclusion, laparoscopic cystectomy of benign ovarian tumors with gonadal preservation is safe in children. It offers benefits of normal puberty and future fertility. The previous concerns of recurrence, spillage and malignancy seem not to be significant as previously thought in our own series or in the preceding literature.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Karpelowsky JS, Erik R, La Hei. Laparoscopic resection of benign ovarian tumors in children with gonadal preservation. Pediatr Surg Int. 2009;25:251–4. doi: 10.1007/s00383-009-2336-8. [DOI] [PubMed] [Google Scholar]
- 2.Aziz D, Davis V, Allen L, Langer JC. Ovarian Torsion in Children: Is Oophorectomy Necessary? J Pediatr Surg. 2004;39:750–3. doi: 10.1016/j.jpedsurg.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 3.Rody A, Jackisch C, Klockenbusch W, Heinig J, Coenen-Worch V, Schneider HP. The conservative management of adenexal torsion — case report and review of literature. Eur J Obstet Gynecol Reprod Biol. 2002;101:83–6. doi: 10.1016/s0301-2115(01)00518-8. [DOI] [PubMed] [Google Scholar]
- 4.Kolonska ER, Keller MS, Weber TR. Acute ovarian torsion in children. Am J Surg. 2000;180:462–5. doi: 10.1016/s0002-9610(00)00503-1. [DOI] [PubMed] [Google Scholar]
- 5.Sommerville M, Grimes DA, Koonings PP, Campbell K. Ovarian neoplasms and the risk of adnexal torsion. Am J Obstet Gynecol. 1991;164:577–8. doi: 10.1016/s0002-9378(11)80024-4. [DOI] [PubMed] [Google Scholar]
- 6.Templeman CL, Fallat ME, Lam AM, Perlman SE, Hertweck SP, O’Connor DM. Managing mature cystic teratomas of the ovary. Obstet Gynecol Surv. 2000;55:738–45. doi: 10.1097/00006254-200012000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Comerci JT, Licciardi F, Bergh PA, Gregori C, Breen JL. Mature cystic teratoma: A clinic-pathological evaluation of 517 cases and review of the literature. Obstet Gynecol. 1994;84:22–8. [PubMed] [Google Scholar]
- 8.Chen M, Chen CD, Yang YS. Torsion of the previously normal uterine adnexa. Evaluation of the correlation between the pathological changes and the clinical characteristics. Acta Obstet Gynecol Scand. 2001;80:58–61. doi: 10.1034/j.1600-0412.2001.800111.x. [DOI] [PubMed] [Google Scholar]
- 9.Chapron C, Dubuisson JB, Samouh N, Foulot H, Aubriot FX, Amsquer Y, et al. Treatment of ovarian dermoid cysts. Place and modalities of operative laparoscopy. Surg Endosc. 1994;8:1092–5. doi: 10.1007/BF00705727. [DOI] [PubMed] [Google Scholar]
- 10.Templeman CL, Hertweck SP, Scheetz JP, Perlman SE, Fallat ME. The management of mature cystic teratomas in children and adolescents: A retrospective analysis. Hum Reprod. 2000;15:2669–72. doi: 10.1093/humrep/15.12.2669. [DOI] [PubMed] [Google Scholar]
- 11.Templeman C, Hertweck SP, Fallat ME. The clinical course of unresected ovarian torsion. J Pediatr Surg. 2000;35:1385–7. doi: 10.1053/jpsu.2000.9347. [DOI] [PubMed] [Google Scholar]
- 12.Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. Minimal surgery for the twisted ischemic adnexa can preserve ovarian function. Hum Reprod. 2003;18:2599–602. doi: 10.1093/humrep/deg498. [DOI] [PubMed] [Google Scholar]
- 13.Felder EP, Guzick DS, Guido R, Kanbour-Shakir A, Krasnow JS. Adhesion formation from release of dermoid contents in the peritoneal cavity and effect of copious lavage: A prospective, randomized, blinded, controlled study in a rabbit model. Fertil Steril. 1996;65:852–9. doi: 10.1016/s0015-0282(16)58225-9. [DOI] [PubMed] [Google Scholar]
- 14.Ozcan C, Celik A, Ozok G, Erdener A, Balik E. Adnexa torsion in children may have catastrophic sequel: Asynchronous bilateral torsion. J Pediatr Surg. 2002;37:1617–20. doi: 10.1053/jpsu.2002.36195. [DOI] [PubMed] [Google Scholar]
- 15.Pansky M, Abargil A, Dreazen E, Golan A, Bukovsky I, Herman A. Conservative management of adnexal torsion in premenarchal girls. J Am Assoc Gynecol Laparosc. 2000;7:121–4. doi: 10.1016/s1074-3804(00)80021-3. [DOI] [PubMed] [Google Scholar]
- 16.Descargues G, Tinolt-Mauger F, Gravier A, Lemoine JP, Marpeau L. Adnexal torsion: A report on forty five cases. Eur J Obstet Gynecol Reprod Biol. 2001;98:91–6. doi: 10.1016/s0301-2115(00)00555-8. [DOI] [PubMed] [Google Scholar]


