The authors surveyed coordinators and health professionals from 1,600 primary health care units across Brazil regarding their knowledge, attitudes, and practices related to cervical cancer and human papillomavirus vaccination. Results showed that overscreening may be impeding efforts to increase cervical cancer screening coverage among the eligible target population of women aged 25–64 years and that educational efforts may be needed to increase knowledge about targeting age-appropriate groups for human papillomavirus vaccination.
Keywords: Cervical cancer screening in Brazil, Global health, HPV vaccination, Cervical cancer knowledge
Abstract
Introduction.
Brazil’s national strategy for cervical cancer screening includes using the Papanicolaou (Pap) test every 3 years among women aged 25–64 years. Comprehensive primary care services are provided through a network of primary health units, but little is known about cervical cancer-related knowledge, attitudes, and practices among health professionals and coordinators working in these facilities.
Methods.
In 2011, we conducted a cross-sectional nationally representative phone survey of 1,600 primary health care units to interview one unit coordinator and one health care professional per unit (either nurse, physician, or community health worker). Responses were obtained from 1,251 coordinators, 182 physicians, 347 nurses, and 273 community health workers. Questionnaires were administered to assess health units’ characteristics and capacity for cervical cancer-related services as well as health professionals’ perceived effectiveness of the Pap test, preparedness to talk to women about cervical cancer, adherence with screening guidelines, and willingness to recommend human papillomavirus (HPV) vaccination to females.
Results.
Most units conducted screening (91.9%), used home visits to conduct recruitment and outreach (83.4%), and provided follow-up to women who did not return to discuss Pap test results (88.1%). Approximately 93% of health professionals stated that Pap testing was effective in decreasing death rates from cervical cancer and 65% stated that national guidelines for cervical cancer screening are very influential; 93% of nurses and physicians reported screening women annually and 75% reported beginning to screen women younger than 25 years old. Regarding HPV vaccination, almost 90% of nurses and physicians would recommend the HPV vaccine to their females patients if it were available. A larger proportion of physicians and nurses recommended the HPV vaccine to older girls (13–18 years) and women (19–26 years and even older than 26 years) than to younger girls (12 years or younger).
Conclusion.
Although Brazil’s network of primary care units has significantly increased access to cervical cancer screening, effective strategies are needed to ensure that women get screened at the appropriate ages and intervals. Additionally, this study’s baseline data on HPV vaccination may be useful as Brazil embarks on a national HPV vaccination program in 2014.
Implications for Practice:
Data on cervical cancer-related knowledge, attitudes, and practices among health professionals in Brazil’s network of primary care units are key to developing effective strategies for the promotion of evidence-based practices and inform the incorporation of human papillomavirus (HPV) vaccination on Brazil’s National Program of Immunizations in 2014. This study suggests that overscreening may be impeding efforts to increase the screening coverage among the eligible target population of women aged 25–64 years. Furthermore, increasing knowledge about the importance of targeting age-appropriate groups for HPV vaccination will be essential to maximize the benefits of this new strategy for cervical cancer prevention.
Introduction
With the consolidation of the Sistema Único de Saúde (SUS) in 1988, Brazil has shifted its model of health care delivery, moving from a curative model structured around urban areas to one that emphasizes prevention and decentralization in the provision of services, in addition to comprehensive health care without fees or copayments [1]. Since the implementation of the SUS, cervical cancer mortality has also steadily declined [2]. In 1998, access to cervical cancer screening was further improved by (a) increasing recruitment, (b) focusing on the target population of women aged 25–59 years, and (c) establishing a 3-year screening interval (after two consecutive negative tests) using the Papanicolaou (Pap) test as the main screening method [3]. In 2011, the national cervical cancer strategy was modified to further emphasize increased access to screening services, improved quality assurance, and increased capacity in the north and northeast regions of Brazil [4]. Beginning in 2014, Brazil will also implement a national human papillomavirus (HPV) vaccination program for girls 10–11 years of age [5].
The network of primary health care units is the gateway to the cervical cancer-related services offered as part of Brazil’s plan for cervical cancer control. These health units, particularly those that are part of the Family Health Program [1], offer comprehensive primary care services, and are composed of multidisciplinary teams of one or more physicians, nurses, nurse assistants, and four to six community health workers, who play a crucial role in conducting recruitment and follow-up of patients with abnormal Pap test results [6]. Despite significant improvements in access with the implementation of Brazil’s Family Health Program and the overall decline in cervical cancer mortality, the burden from cervical cancer is still high and recruitment of women at higher risk for cervical cancer continues to be a challenge [1, 2]. The purpose of this study was twofold: to assess the health care units’ capacity and type of services offered to increase the uptake of cervical cancer screening, and to examine cervical cancer-related knowledge, attitudes, and practices among physicians, nurses, and community health workers in Brazil’s network of primary care units.
Materials and Methods
Data Source and Study Population
From a list of 42,000 units provided by the Ministry of Health, we conducted a stratified random sample that was proportionally allocated by region. In total, 1,600 health care units were selected, and one coordinator and one health professional were interviewed per unit (either physician, nurse, or community health worker). This sampling scheme was used to ensure that the number of units sampled was proportional to the total number of units per region (Fig. 1). The original sample included 1,600 unit coordinators, 533 nurses, 533 physicians, and 533 community health workers. Units that appeared on the list but no longer existed (approximately 3%) were replaced. Replacement was not used for those that refused to participate. Responses were obtained from 1,251 coordinators, 347 nurses, 182 physicians, and 273 community health workers (response rates of 78%, 65%, 34%, and 51%, respectively). Response rates for the overall sample were similar across regions. This study was approved by the Institutional Review Board of the Centers for Disease Control and Prevention (CDC), the Federal University of Pelotas, and Washington University in St. Louis, Missouri.
Figure 1.
Number of health care units sampled per region (n = 1,600)—Primary Care Survey, 2011.
Measures
A questionnaire was administered to coordinators to assess the health units’ capacity to provide cervical cancer-related services, type of services offered to increase uptake of cervical cancer screening, regional distribution of the units within the five regions of Brazil, and units’ population coverage. Another questionnaire was administered to nurses, physicians, and community health workers to examine perceived effectiveness of the Pap test to decrease death rates from cervical cancer, level of preparedness to talk to women about cervical cancer, familiarity and adherence with screening guidelines, and knowledge and acceptability of HPV vaccination for females (Table 1). Both questionnaires were part of a larger survey developed by CDC, the University of Pelotas, and Washington University in St. Louis examining knowledge, attitudes, and practices related to physical activity, diet, and other types of cancer [7].
Table 1.
Questionnaire on cervical cancer-related attitudes, knowledge, and practices administered to physicians, nurses, and community health workers working in Brazil’s network of primary care units (n = 802)—Primary Care Survey, Brazil, 2011
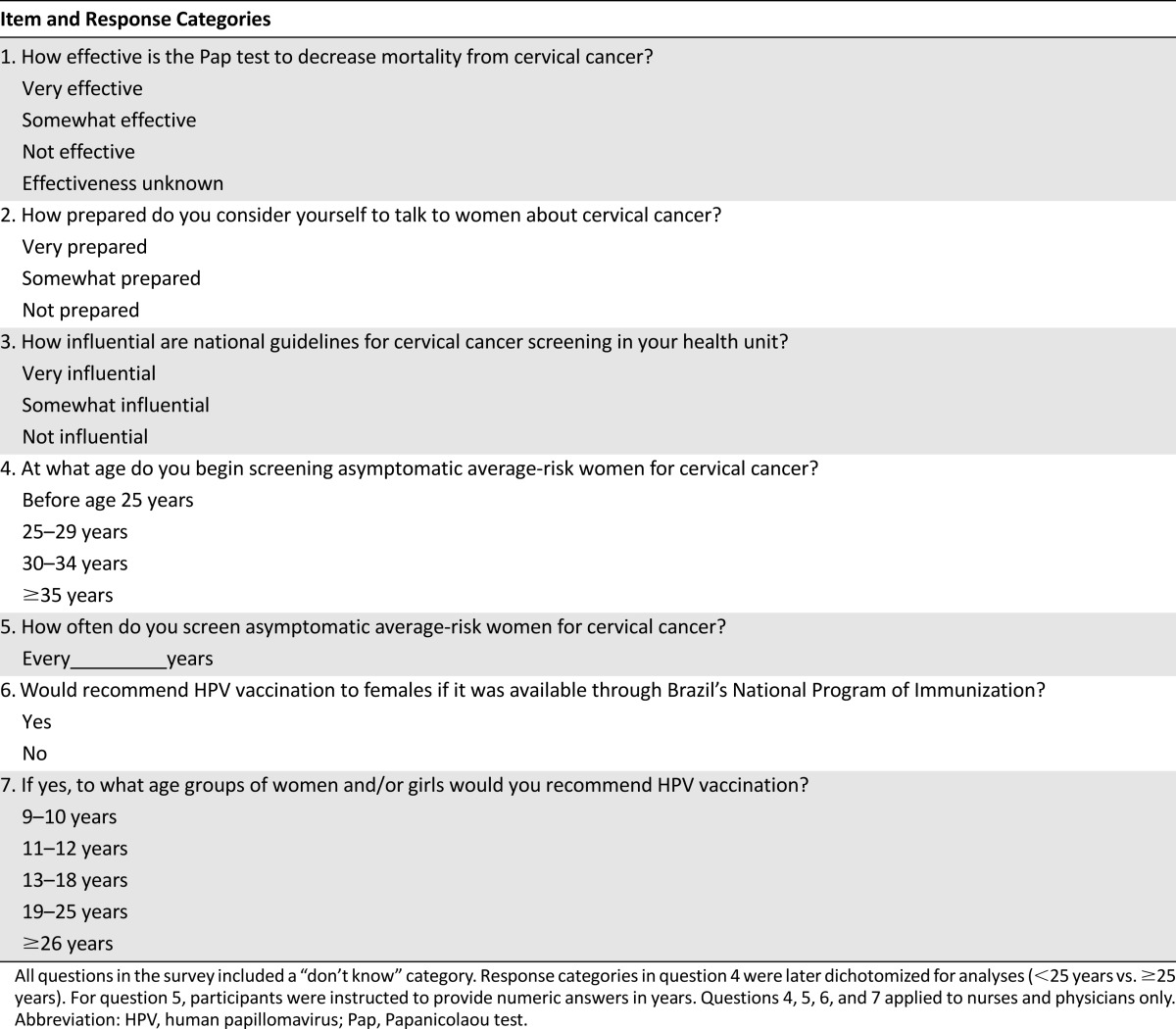
Questions were drafted in English, translated to Portuguese by native speakers, and back-translated to English. The final Portuguese version of the questionnaire was piloted among a small group of participants in Brazil to assess the instrument’s validity and reliability. In January 2011, phone surveys were conducted by a team of six trained interviewers attending graduate programs at the University of Pelotas in Brazil. Data collection was completed in June 2011. Informed consent was read to participants before the questionnaire was administered. Interviews for both coordinators and health professionals lasted, on average, 40 minutes.
Statistical Analyses
From the coordinator survey, we conducted bivariate analyses of health care units’ characteristics and capacity to provide services for cervical cancer prevention and early detection. Using the health professional survey, we compared knowledge, attitudes, and practices related to cervical cancer screening and HPV vaccination by provider type. We limited our analyses of screening practices and intentions to recommend HPV vaccination to physicians and nurses. We used Pearson chi-square tests (where applicable) to compare responses by health professional type. Staff at the University of Pelotas used EpiData statistical software version 3.1 (http://www.epidata.dk) to input the raw data and then transferred it into SPSS 16 (SPSS, Chicago, IL). All data received by CDC and Washington University were deidentified.
Results
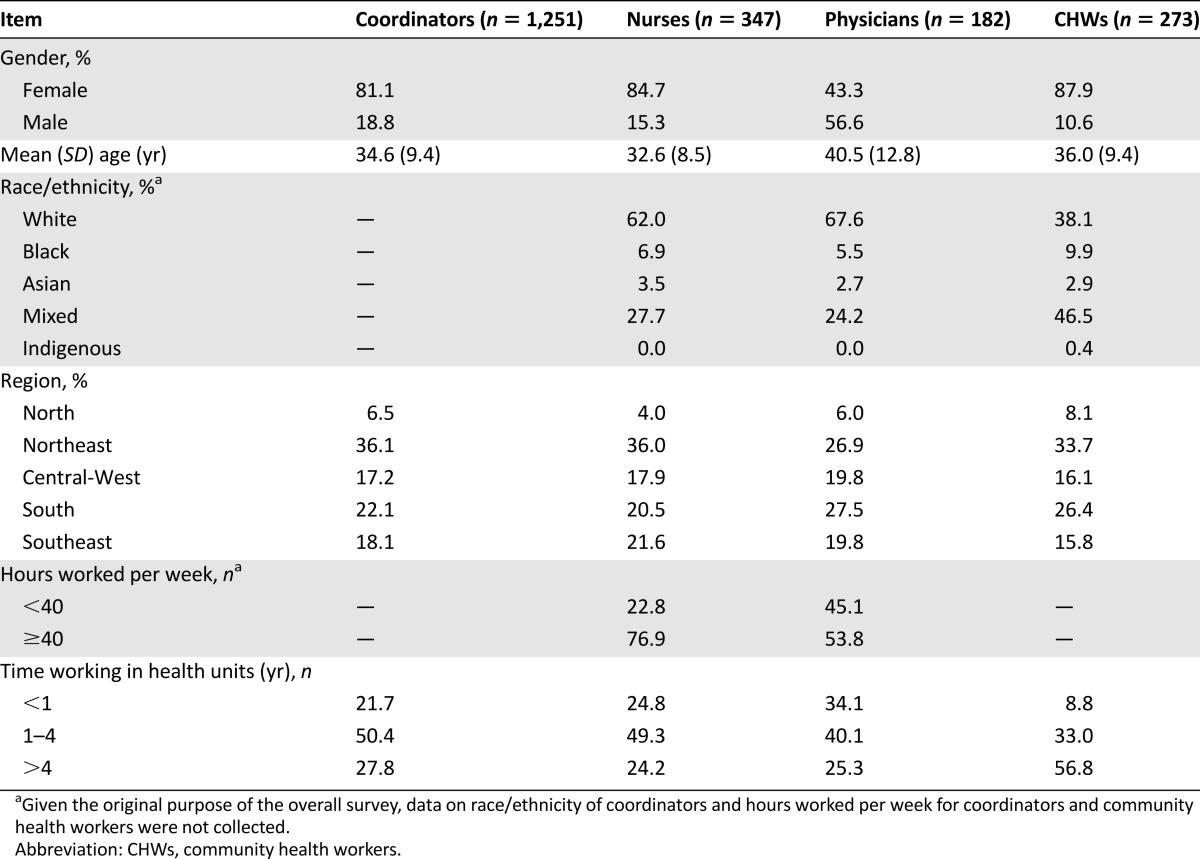
Demographic and Professional Characteristics
More than 80% of unit coordinators and health professionals (except physicians) were women (Table 2). More than half (56.8%) of community health workers had worked in their specific health unit for more than 4 years, compared with coordinators (27.8%), nurses (24.2%), and physicians (25.3%).
Table 2.
Health professionals’ and unit coordinators’ demographic and professional characteristics (n = 2,053)—Primary Care Survey, Brazil, 2011
Coordinators’ Survey: Health Unit Characteristics
Overall, the majority of health units were part of the Family Health Program (60.7%) and had a population coverage of 6,000 or fewer inhabitants (Table 3). The Northeast region had the highest percentage of health units that are part of the Family Health Program (71.4%), whereas the South region had the lowest percentage of this type of units (51.6%). With regard to the units’ composition, most had one physician (60.5%), one nurse (72.7%), and a team of four or more community health workers (72.5%).
Table 3.
Primary health care units’ characteristics, by region (n = 1,251)—Primary Care Survey, Brazil, 2011
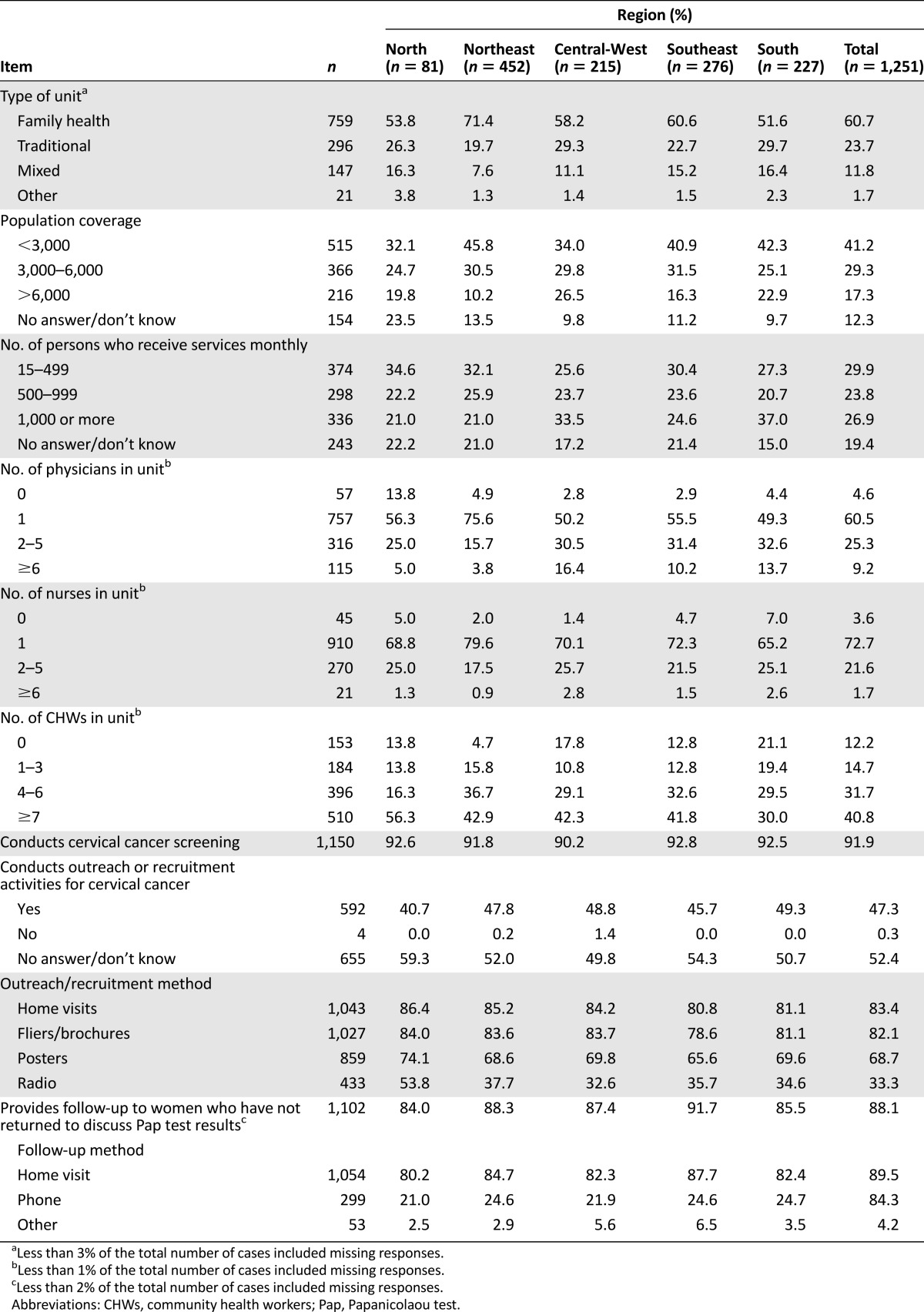
A total of 91.9% units conducted cervical cancer screening, 47.3% conducted outreach or recruitment activities, and 88.1% provided follow-up for patients who had not returned to discuss Pap test results. Home visits were the most common type of outreach or recruitment activity (83.4%) and the main follow-up method for women who had not returned to discuss Pap test results (89.5%).
Health Professionals’ Survey: Attitudes, Knowledge, and Screening Practices
Most health professionals (>90%) stated that Pap testing is very effective in decreasing mortality rates from cervical cancer (Table 4). Among health professional type, community health workers (57.6%) were the least likely to report being very prepared to talk to women about cervical cancer, compared with nurses (89.3%) and physicians (70.3%) (p < .001).
Table 4.
Cervical cancer related attitudes, knowledge, and practices of health professionals working in health units, by professional type (N=802)—Primary Care Survey, Brazil, 2011
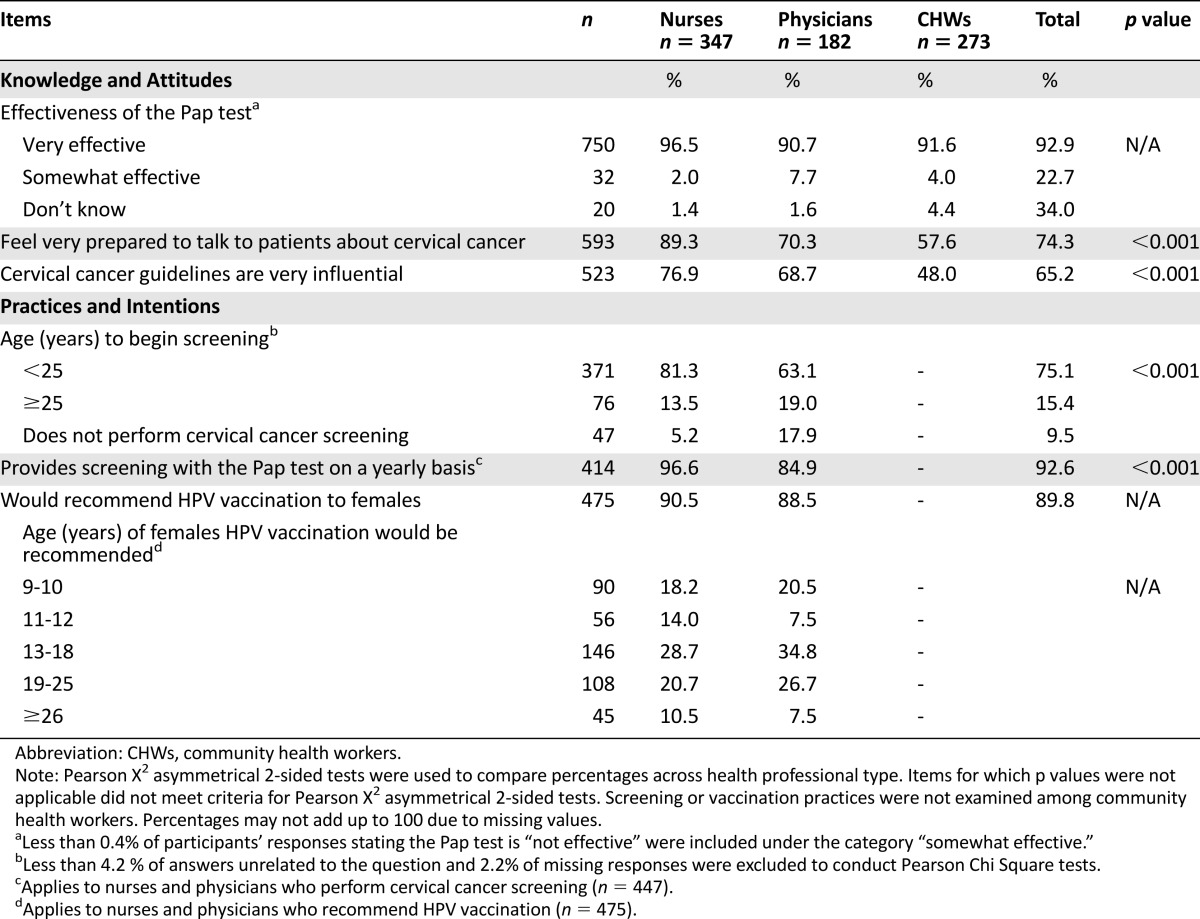
Most nurses and physicians (76.9% and 68.7%, respectively) stated that national guidelines for cervical cancer screening are very influential in their specific health unit; however, 92.6% reported screening women on an annual basis and 75.1% reported beginning to screen women before the age of 25 years, with nurses the more likely to report both of these practices (p < .01). A total of 5.2% of nurses reported not performing cervical cancer screening, which was lower than the percentage of physicians (17.9%) (p < .001). A total of 90.5% of nurses and 88.5% of physicians reported that they would recommend HPV vaccination to their female patients. When asked to indicate specific age groups, most nurses and physicians reported that they would recommend it to females aged ≥13 years. Across age groups, the highest percentage of both nurses and physicians would recommend it to females aged 13–18 years (28.7% and 34.8%, respectively) followed by those aged 19–25 years (20.7% and 26.7%, respectively).
Conclusion
In this study, the practices of physicians and nurses in Brazil’s network of primary health care units were not consistent with national guidelines for cervical cancer screening initiation and frequency, suggesting that overscreening may be impeding efforts to increase the screening coverage among the eligible target population of women aged 25–64 years. These findings are consistent with previous work in the city of Campiñas [8] and the southern city of Pelotas [9] showing that most Pap tests were performed in women outside the eligible target population or in those who had been screened within the past 3 years. Both the World Health Organization and Brazilian national screening guidelines do not recommend screening women under age 25 years because treatment of precancerous lesions is rarely needed among younger women as these lesions are usually cleared. Screening on an annual basis is also not recommended [3, 10]. Although a significantly higher percentage of nurses than physicians stated that national guidelines for cervical cancer screening are very influential, nurses were less likely to follow them in practice. These findings highlight the need to develop effective and possibly separate interventions for physicians and nurses about the importance of prioritizing women in the target-age population and the harms associated with overscreening. Provider assessment and feedback interventions have been found effective in increasing cervical cancer screening with the Pap test [11]; however, determining whether these or other strategies are effective in reducing overscreening and increasing adherence with screening guidelines remains an important research need.
Cervical cancer incidence and mortality in Latin America and the Caribbean is characterized by regional variations within countries, including Brazil [12]. Through its novel patient-centered approach, the SUS has increased access by bringing primary care services to the communities. Community health workers in Brazil’s network of primary health units are in charge of conducting outreach, recruitment, and follow-up of women who have not returned to discuss Pap test results. Thus, these professionals play a pivotal role in increasing patient-provider communication and access to cervical cancer-related services, especially in the North and Northeast regions of Brazil where the screening coverage is low [6]. Coordinators in charge of health units in both of these regions reported having the highest percentage of community health workers in their multidisciplinary teams of health professionals; however, only a little over half of community health workers reported being very prepared to talk to women about cervical cancer. Community health workers were also the least likely to state that guidelines for cervical cancer screening were very influential. Previous studies have found that home visits by community health workers are an effective strategy to increase screening, especially among vulnerable groups [13, 14]. Women in these groups also have the least knowledge about cervical cancer screening and the lowest access to services [12]. In this study, home visits were the most commonly used method to conduct outreach, recruitment, and follow-up, with very minimal variations across regions (6%–7%). Thus, it is critical that community health workers are equipped with the communication skills and health knowledge needed to properly conduct outreach, increase recruitment, and conduct follow-up of women who have not returned to the health unit to discuss their Pap test results.
Beginning in 2014, the quadrivalent HPV vaccine will be available through Brazil’s SUS for girls 10–11 years of age [15]. This target population was identified as the most age-appropriate group for immunization based on the Brazilian Ministry of Health 2012 study, which found that 18.3% of 13- to 15-year-old girls nationwide had already engaged in sexual activity [5]. This study examined providers’ and nurses’ willingness to recommend HPV vaccination to their female patients for specific age groups of patients prior to the announcement of this policy. Although we found that the majority of nurses and physicians would recommend HPV vaccination, our findings indicate that educational efforts may be needed to increase knowledge about targeting age-appropriate groups given that vaccination provides protection against HPV types if exposure has not yet occurred through sexual activity. Our findings are consistent with previous research in the United States showing that a greater percentage of physicians recommend the vaccine to older age groups outside the target age of 11–12 years [16]. Initial advocacy efforts addressing the importance of targeting girls in appropriate age groups will be key to ensuring that vaccination is effective in providing protection against HPV types. Finally, the development of a comprehensive communication plan with ample support from immunization partners should be considered as another possible mechanism to ensure that girls in the eligible target population receive HPV vaccination [17].
The present study has limitations. The beliefs and practices reported in this study are based on self-reported data and may be influenced by social desirability and recall bias. As in many provider surveys [18], the response rate of physicians was lower than that of other groups and did not allow for a comparison of knowledge, attitudes, and practices by covariates of interest across health professional type. Despite these limitations, the overall sample of 1,251 units is representative of the network of units in each of the five regions of Brazil. To our knowledge, this is also the first study to provide an assessment from a national perspective of the knowledge, attitudes, and practices related to cervical cancer prevention and screening in Brazil’s network of health units. Lastly, this study provides baseline data on HPV vaccination that may be helpful to inform Brazil’s strategy to incorporate HPV vaccination in its National Program of Immunization in 2014.
Brazil’s network of health units is a prominent example of successful comprehensive primary care, with accomplishments, challenges, and lessons learned that can be useful for the United States and other high- and middle-income countries attempting to shift their paradigm of health care delivery to a patient-centered approach. Our study, however, points out the need for increased knowledge of national guidelines and emphasis on evidence-based screening practices to make a significant impact in the long term and maximize the benefits of this comprehensive primary care strategy for cervical cancer prevention and control.
Acknowledgments
This article was supported by Cooperative Agreement U48/DP001903 from the Centers for Disease Control and Prevention with the Prevention Research Center at Washington University in St. Louis, Missouri. This research was supported in part by an appointment to CDC's Research Participation Program administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and CDC. Findings from this study were previously presented at the 28th International Papilloma Virus Conference, December, 2012 and at the 2012 CDC National Cancer Conference. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Editor's Note: See the related article, “Current Cervical Cancer Screening Knowledge, Awareness, and Practices Among U.S. Affiliated Pacific Island Providers: Opportunities and Challenges,” by Julie S. Townsend et al. on page 383 of this issue, and the commentary by Annekathryn Goodman and Nawal Nour, which discusses the context surrounding the global disparities in cervical cancer, on page 315.
For Further Reading: Suneeta Krishnan, Emily Madsen, Deborah Porterfield et al. Advancing Cervical Cancer Prevention in India: Implementation Science Priorities. The Oncologist 2013;18:1285–1297.
Implications for Practice: Considerable research has been conducted on the prevention of cervical cancer in India. The majority of studies have focused on the feasibility, acceptability, and impact of secondary prevention of cancer through screening, early detection, and treatment. Despite this evidence, there have been few government-led public health programs to prevent and control cervical cancer. The primary goals of this review are to summarize the lessons learned from cervical cancer prevention research and pilot programs in India and to identify research priorities to facilitate the translation of existing knowledge into policies and programs that advance cervical cancer prevention.
Author Contributions
Conception/design: Lenildo de Moura, Mona Saraiya
Provision of study material or patients: Analía Romina Stormo, Lenildo de Moura
Collection and/or assembly of data: Lenildo de Moura
Data analysis and interpretation: Analía Romina Stormo, Mona Saraiya
Manuscript writing: Analía Romina Stormo, Lenildo de Moura, Mona Saraiya
Final approval of manuscript: Analía Romina Stormo, Lenildo de Moura, Mona Saraiya
Disclosures
The authors indicated no financial relationships.
References
- 1.Rocha R, Soares RR. Evaluating the impact of community-based health interventions: Evidence from Brazil’s Family Health Program. Health Econ. 2010;19(Suppl):126–158. doi: 10.1002/hec.1607. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt MI, Duncan BB, Azevedo e Silva G, et al. Chronic non-communicable diseases in Brazil: Burden and current challenges. Lancet. 2011;377:1949–1961. doi: 10.1016/S0140-6736(11)60135-9. [DOI] [PubMed] [Google Scholar]
- 3.Instituto Nacional de Câncer (INCA). 2010. Monitoramento das acoes de controle do cancer do colo do utero e mama. Brazil, Rio de Janeiro: INCA. Available at http://www1.inca.gov.br/inca/Arquivos/inform.deteccaoprecoce.pdf Accessed January 1, 2012.
- 4.Union for International Cancer Control. 2011. Prevention and treatment of breast and cervical cancer in Brazil. Available at http://www.uicc.org/advocacy/prevention-and-treatment-cervical-and-breast-cancer-brazil Accessed October 15, 2012.
- 5.Brazilian Ministry of Health. 2013. Ministério da Saúde incorpora vacina contra HPV ao SUS [in Portuguese]. Available at http://portalsaude.saude.gov.br/portalsaude/noticia/11613/162/ministerio-da-saude-incorpora-vacina-contra-hpv-ao-sus.html Accessed July 31, 2013.
- 6.Pinto RM, da Silva SB, Soriano R. Community health workers in Brazil’s Unified Health System: A framework of their praxis and contributions to patient health behaviors. Soc Sci Med. 2012;74:940–947. doi: 10.1016/j.socscimed.2011.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Florindo AA, Mielke GI, Gomes GA, et al. Physical activity counseling in primary health care in Brazil: A national study on prevalence and associated factors. BMC Public Health. 2013;13:794. doi: 10.1186/1471-2458-13-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freitas RA, Carvasan GA, Morais SS, et al. Excessive Pap smears due to opportunistic cervical cancer screening. Eur J Gynaecol Oncol. 2008;29:479–482. [PubMed] [Google Scholar]
- 9.de Quadros CA, Victora CG, da Costa JS. Coverage and focus of a cervical cancer prevention program in southern Brazil. Rev Panam Salud Publica. 2004;16:223–232. doi: 10.1590/s1020-49892004001000001. [DOI] [PubMed] [Google Scholar]
- 10.International Agency for Research on Cancer (IARC). Cervical cancer and screening. In Handbook of Cancer Prevention. Vol. 10. Lyon, France: IARC, 2005. Available at http://www.iarc.fr/en/publications/pdfs-online/prev/handbook10/index.php Accessed March 1, 2011.
- 11.Sabatino SA, Lawrence B, Elder R, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: Nine updated systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Villa LL. Cervical cancer in Latin America and the Caribbean: The problem and the way to solutions. Cancer Epidemiol Biomarkers Prev. 2012;21:1409–1413. doi: 10.1158/1055-9965.EPI-12-0147. [DOI] [PubMed] [Google Scholar]
- 13.Mauad EC, Nicolau SM, Moreira LF, et al. Adherence to cervical and breast cancer programs is crucial to improving screening performance. Rural Remote Health. 2009;9:1241. [PubMed] [Google Scholar]
- 14.Agurto I, Arrossi S, White S, et al. Involving the community in cervical cancer prevention programs. Int J Gynaecol Obstet. 2005;89(Suppl 2):S38–S45. doi: 10.1016/j.ijgo.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 15.Pan American Health Organization. 2013. Cancer in the Americas: Country profiles 2013. Available at http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=23456&Itemid=270&lang=en Accessed November 30, 2013.
- 16.Daley MF, Crane LA, Markowitz LE, et al. Human papillomavirus vaccination practices: A survey of U.S. physicians 18 months after licensure. Pediatrics. 2010;126:425–433. doi: 10.1542/peds.2009-3500. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. 2005. Vaccine introduction guidelines: Adding a vaccine to a national immunization program. Available at http://www.who.int/immunization/hpv/plan/vaccine_introduction_guidelines_who_2005.pdf. Accessed July 31, 2013.
- 18.VanGeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: A systematic review. Eval Health Prof. 2007;30:303–321. doi: 10.1177/0163278707307899. [DOI] [PubMed] [Google Scholar]



