Abstract
Cervical cancer remains a leading cause of cancer death in many low- and middle-income countries. Key issues that must be addressed include the obstacle of poverty, the importance of community representatives, and the credibility of the medical establishment. Better understanding of the complex layers of social ecology and the social determinants of health will allow public health planners to build sustainable programs.

Dr. Annekathryn Goodman

Dr. Nawal Nour
Despite well-known and inexpensive screening tools, cervical cancer remains a leading cause of cancer death in many low- and middle-income countries [1]. There are barriers and challenges to universal screening both in low-resource countries and among the poor, minority, immigrant, and indigenous populations of many high-income countries. Understanding the skills of and resources available to women’s health care clinicians will help tailor cervical cancer screening education and training programs for providers.
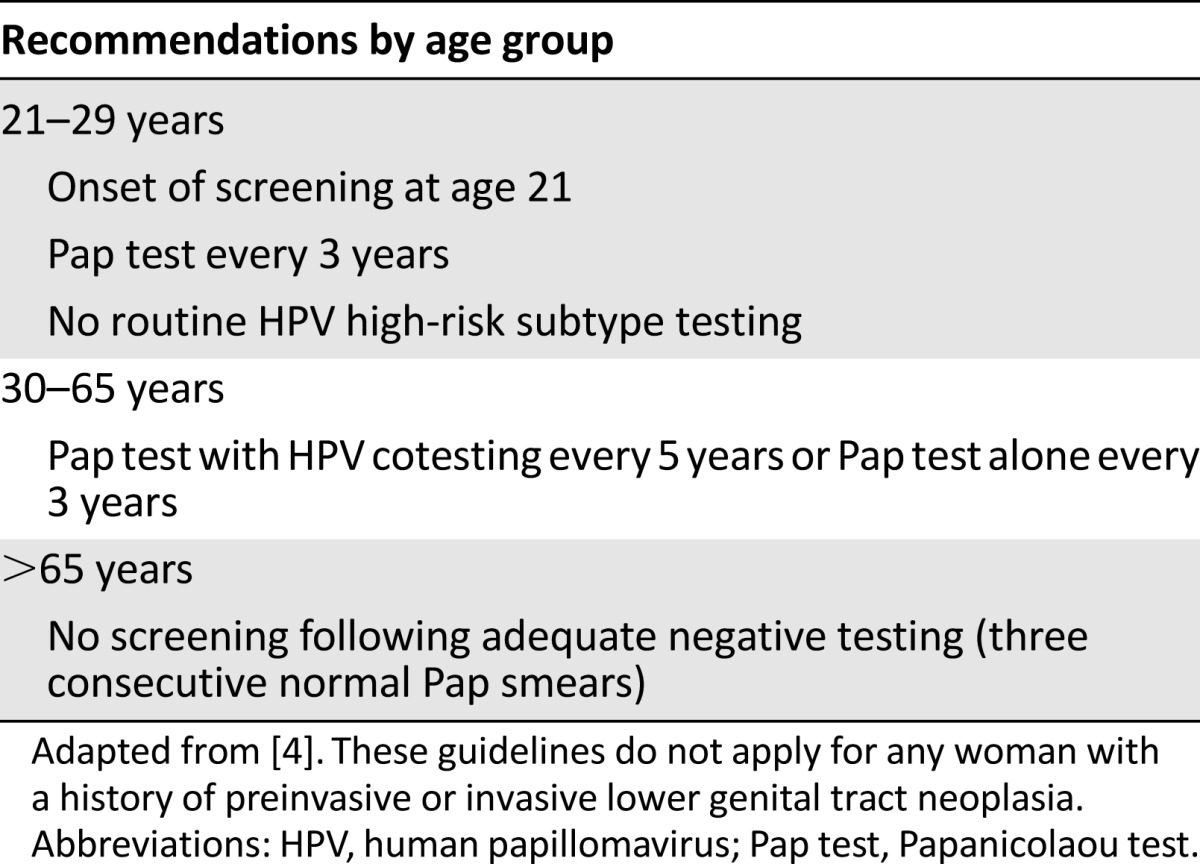
Using standardized telephone surveys, Stormo et al. [2] and Townsend et al. [3] report on the screening knowledge and practices of two separate regions with extremely high cervical cancer rates: Brazil and the U.S. Affiliated Pacific Island Jurisdictions (USAPIJ). Both surveys took place in 2011, prior to the institution of the new combined American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology guidelines for cervical cancer screening (Table 1) [4]. In Brazil, national guidelines recommend a focus on women aged 25–59 years with Papanicolaou (Pap) tests every 3 years after two consecutive yearly normal results [2]. In the USAPIJ, the older annual Pap test screening guidelines were generally followed [3]. The Brazilian and USAPIJ studies found that the majority of nurses and physicians in the surveyed health centers—94% and 76.4%, respectively—had a sound understanding of the importance of screening for the prevention of cervical cancer. These surveys offer further insights into components of the underlying infrastructures of the health care systems of these two regions.
Table 1.
Current cervical cancer screening guidelines
Cervical cancer is the second most common cause of cancer death for women in Brazil and in nearly all USAPI jurisdictions. Over the past 25 years, reorganization of Brazil’s health care system into 42,000 units staffed by physicians, nurses, and community health workers (CHWs) has broadened health care access and improved cervical cancer screening. The survey revealed that the challenges now faced by Brazilian health care units include the limited number of health care providers, loss to follow-up of a large percentage of patients, and a need to increase training and education about cervical cancer and the interventions appropriate for use by CHWs. Community health workers in Brazil have been effectively utilized to educate the community and to make home visits to women who are normally lost to follow-up. Although the issue of how to treat cervical cancer when it is identified was not addressed in this survey, resources outside of urban centers to manage advanced cancer are limited.
In contrast, in the USAPIJ, Pap test access varies considerably across the different islands, ranging from 15% of women in the Federated States of Micronesia to a complete lack of services in the outer atolls of the Republic of the Marshall Islands. The major challenges identified in the survey include lack of health care facilities and providers, limited access to clinics, lack of equipment, and limited infrastructure for care in response to abnormal findings. Providers at health centers must refer patients to a hospital, or even off-island, for both diagnostic procedures and therapeutic interventions.
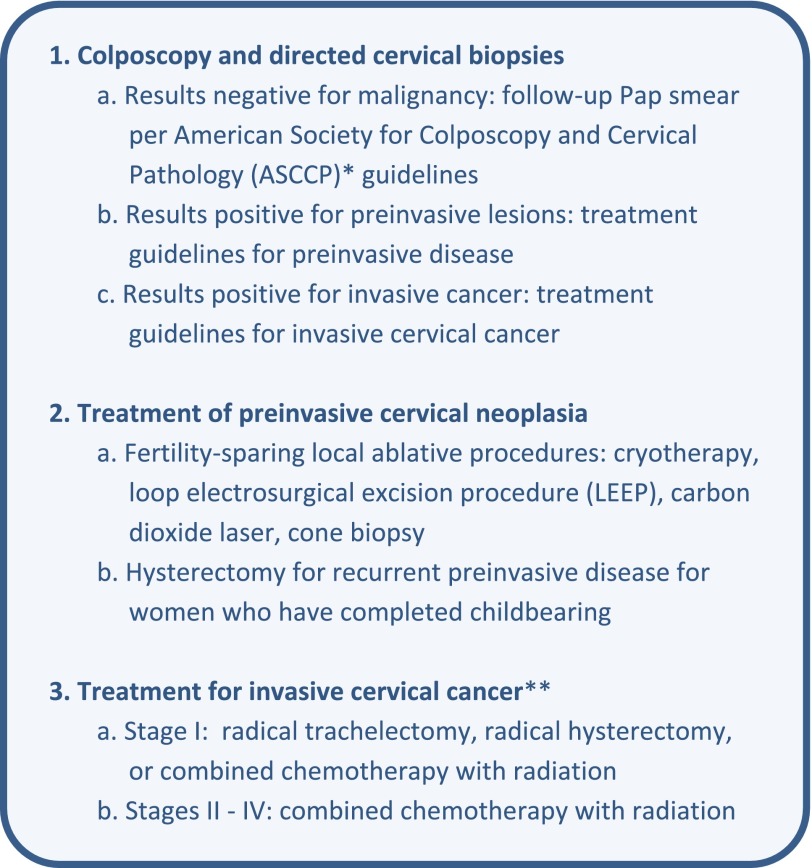
Effective secondary prevention of cervical cancer, the screening for preinvasive and early invasive disease, can occur only when two broad components of health care are in place: one is medical infrastructure to perform screening and evaluation of abnormal results and the other is acceptance and demand for these interventions by both individual women and their communities. One solution would be to expand existing programs such as HIV treatment networks with cervical cancer screening. The standard protocol for the follow-up, evaluation, and treatment of abnormal Pap smear results is outlined in Figure 1. In LMICs, there has been a growing interest in low-cost cervical cancer screening using visual inspection with acetic acid (VIA), which bypasses the use of Pap smear testing, colposcopy, and directed cervical biopsies altogether. In 11 major studies and 4 meta-analyses of programs in LMICs that evaluated the accuracy of VIA, the sensitivity and specificity of VIA to detect high-grade preinvasive cervical disease ranged from 52%-93% (mean 73%) and 49%-98% (mean 80%), respectively [5].
Figure 1.
Evaluation and treatment of abnormal Pap smears.
The core challenge for the creation of programs and for overcoming the barriers to screening is the “cause of causes”: poverty [6]. A World Health Organization survey from 15 developing countries reported a 4.1% cervical cancer-screening rate and identified the leading determinants of screening: household socioeconomic status and the percent of gross domestic product allotted to health expenditures [7].
Social determinants of health encompass the greater societal, political, and economic reasons for inadequate health care facilities [8]. As Townsend et al. demonstrate in their survey of the USAPIJ providers, these social and geographical determinants are at play in this area where cervical cancer screening is inadequate because of lack of trained providers, scarce funds, lack of facilities and equipment, and a geographically diverse region of 2,194 sparsely populated islands (with the majority of people living on 658 islands) over five time zones [3].
Even in an ideal world of adequate medical providers, supplies, and infrastructure to treat abnormalities, additional barriers prevent women from seeking care. Social ecology, an early model for the complex interplay of intra- and interpersonal, community, and societal factors in human development, can be used to analyze the cultural and social barriers to health care [9]. The barriers to cervical cancer screening include personal barriers (home safety, educational status, and cultural beliefs can hinder care) and community and societal factors such as the built environment of neighborhoods that lack roads, traffic safety, or public transportation and thus discourage travel to clinics [10]. In developing countries, rural residence is a significant impediment to seeking care [7].
Personal barriers can include mental illness or lack of language fluency [11, 12]. One study from Indonesia addressed the issue of persuading women to go for screening [13]. Interviews with women, their husbands, and staff members of public health centers revealed that knowledge and perceptions were the most important barriers to screening. Women were both ignorant of the risks of cervical cancer and fatalistic about its outcome. Religious guilt and the cultural belief that they were being punished for sexual behavior can prevent minority women from seeking free and accessible cervical cancer screening [12]. Other cultures felt that Papanicolaou test screening itself was associated with shame and stigma [8]. In countries with colonial histories, indigenous women may avoid conventional medical care. One of the structural barriers to screening identified among First Nations women in Canada was a mistrust of authority related to the colonial legacy [14].
The social stigma of having cancer and fear of rejection by their husbands and communities can also prevent women from seeking medical intervention [15]. In Peru, one significant predictor of a woman’s participation in cervical cancer screening was a supportive male partner [16]. Many studies have confirmed the need for social cohesion and collective encouragement for women to venture into clinics [8].
Stormo et al. showed that community health workers have been used effectively to both educate the community and to follow up with home visits when women do not return to the clinic [2]. A 1998 landmark report on community workers identified key roles to facilitate access and care in health care systems [17]. These include cultural mediation, counseling and education, social support, advocacy for community needs, and even the development of community health service capacity.
In the U.S., where cervical cancer outcome disparities have significant links with racial and ethnic minority status, lay health promoters have been used to educate communities about health risks and appropriate interventions for chronic diseases and cancer screening [18, 19]. There has been a move to improve community collaboration in these screening programs. One program in Peru empowered CHWs to develop a program to implement screening in their communities [20]. Another program targeting Mexican American women used “promotoras” (i.e., CHWs) to develop a curriculum to train other CHWs about cervical cancer and to identify relevant social determinants of health in their communities [21]. The use of community health workers to educate the community and improvements in health literacy, beliefs, and attitudes of the community increased screening uptake in rural India [22]. Criticism of community workers or “patient navigators” in the U.S. includes the concern that such programs add costs but may not identify cancers at an earlier stage [23]. While there has been a growing use of midlevel providers such as midwives, nurse practitioners, and physician assistants for clinical outreach and patient education in the United States, the significant nursing shortage in many LMICs makes CHWs a more feasible and economic model for screening programs [24].
An analysis of successful population-wide screening programs identifies several recurring themes that are important both in low- and middle-income countries and in high-income countries where segments of the population are underserved. In addition to robust medical infrastructure and financial stability, the society at large must support and promote screening efforts. Leadership and education come not only from the medical community but also from representatives of civil society. Key issues that must be addressed include the obstacle of poverty, the importance of community representatives, and the credibility of the medical establishment. Poverty and the lack of food and shelter are serious obstacles to cancer screening and cancer care; therefore, public health programs must address basic survival before cervical cancer screening can be improved. The lessons learned from CHWs include the importance of programmatic activism and integration of community and medical goals. Medical providers must create a safe, predictable, and private environment where women feel respected. Better understanding of the complex layers of social ecology and the social determinants of health will allow public health planners to build sustainable programs.
Footnotes
Editor’s Note: See the related articles in this month's issue: Analía Romina Stormo et al., “Cervical Cancer-Related Knowledge, Attitudes, and Practices of Health Professionals Working in Brazil's Network of Primary Care Units,” on pages 375–382 and Julie Townsend et al., “Current Cervical Cancer Screening Knowledge, Awareness, and Practices Among U.S. Affiliated Pacific Island Providers: Opportunities and Challenges,” on pages 383–393.
Disclosures
The authors indicated no financial relationships.
References
- 1.GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Available at http://globocan.iarc.fr/Default.aspx Accessed February 16, 2014.
- 2.Stormo AR, de Moura L, Saraiya M. Cervical cancer-related knowledge, attitudes, and practices of health professionals working in Brazil’s network of primary care units. The Oncologist. 2014;19:375–382. doi: 10.1634/theoncologist.2013-0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Townsend JS, Stormo AR, Roland KB, et al. Current cervical cancer screening knowledge, awareness, and practices among United States Affiliated Pacific Island providers: Opportunities and challenges. The Oncologist. 2014;19:383–393. doi: 10.1634/theoncologist.2013-0340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012;16:175–204. doi: 10.1097/LGT.0b013e31824ca9d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradford LS, Goodman A. Cervical cancer screening and prevention in low resource settings. Clinical Obstet Gynecol. 2013;56:76–87. doi: 10.1097/GRF.0b013e31828237ac. [DOI] [PubMed] [Google Scholar]
- 6.Vineis P, Wild CP. Global cancer patterns: Causes and prevention. Lancet. 2014;383:549–557. doi: 10.1016/S0140-6736(13)62224-2. [DOI] [PubMed] [Google Scholar]
- 7.Akinyemiju TF. Socio-economic and health access determinants of breast and cervical cancer screening in low-income countries: Analysis of the World Health Survey. PLoS One. 2012;7:e48834. doi: 10.1371/journal.pone.0048834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams-Brennan L, Gastaldo D, Cole DC, et al. Social determinants of health associated with cervical cancer screening among women living in developing countries: A scoping review. Arch Gynecol Obstet. 2012;286:1487–1505. doi: 10.1007/s00404-012-2575-0. [DOI] [PubMed] [Google Scholar]
- 9.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 10.Goodman A. The social ecology of cervical cancer: The challenges to Pap smear screening. Int J Clin Med. 2013;4:16–20. [Google Scholar]
- 11.Aggarwal A, Pandurangi A, Smith W. Disparities in breast and cervical cancer screening in women with mental illness: A systematic literature review. Am J Prev Med. 2013;44:392–398. doi: 10.1016/j.amepre.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Watts L, Joseph N, Velazquez A, et al. Understanding barriers to cervical cancer screening among Hispanic women. Am J Obstet Gynecol. 2009;201:199.e1–199.e8. doi: 10.1016/j.ajog.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Kim YM, Ati A, Kols A, et al. Influencing women’s actions on cervical cancer screening and treatment in Karawang District, Indonesia. Asian Pac J Cancer Prev. 2012;13:2913–2921. doi: 10.7314/apjcp.2012.13.6.2913. [DOI] [PubMed] [Google Scholar]
- 14.Maar M, Burchell A, Little J, et al. A qualitative study of provider perspectives of structural barriers to cervical cancer screening among first nations women. Womens Health Issues. 2013;23:e319–e325. doi: 10.1016/j.whi.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregg JL. An unanticipated source of hope: Stigma and cervical cancer in Brazil. Med Anthropol Q. 2011;25:70–84. doi: 10.1111/j.1548-1387.2010.01137.x. [DOI] [PubMed] [Google Scholar]
- 16.Winkler J, Bingham A, Coffey P, et al. Women’s participation in a cervical cancer screening program in northern Peru. Health Educ Res. 2008;23:10–24. doi: 10.1093/her/cyl156. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal EL. Summary of the National Community Health Advisor Study: Weaving the future. Available at http://crh.arizona.edu/sites/crh.arizona.edu/files/pdf/publications/CAHsummaryALL.pdf Accessed February 16, 2014.
- 18.Rauh-Hain JA, Clemmer JT, Bradford LS, et al. Racial disparities in cervical cancer survival over time. Cancer. 2013;119:3644–3652. doi: 10.1002/cncr.28261. [DOI] [PubMed] [Google Scholar]
- 19.Gwede CK, Ashley AA, McGinnis K, et al. Designing a community-based lay health advisor training curriculum to address cancer health disparities. Health Promot Pract. 2013;14:415–424. doi: 10.1177/1524839912458675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levinson KL, Abuelo C, Chyung E, et al. The Peru Cervical Cancer Prevention Study (PERCAPS): Community-based participatory research in Manchay, Peru. Int J Gynecol Cancer. 2013;23:141–147. doi: 10.1097/IGC.0b013e318275b007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore-Monroy M, Wilkinson-Lee AM, Verdugo L, et al. Addressing the information gap: Developing and implementing a cervical cancer prevention education campaign grounded in principles of community-based participatory action. Health Promot Pract. 2013;14:274–283. doi: 10.1177/1524839912454141. [DOI] [PubMed] [Google Scholar]
- 22.Isaac R, Finkel M, Olver I, et al. Translating evidence into practice in low resource settings: Cervical cancer screening tests are only part of the solution in rural India. Asian Pac J Cancer Prev. 2012;13:4169–4172. doi: 10.7314/apjcp.2012.13.8.4169. [DOI] [PubMed] [Google Scholar]
- 23.Bensink ME, Ramsey SD, Battaglia T, et al. Costs and outcomes evaluation of patient navigation after abnormal cancer screening: Evidence from the Patient Navigation Research Program. Cancer. 2014;120:570–578. doi: 10.1002/cncr.28438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds J, Wisaijohn T, Pudpong N, et al. A literature review: The role of the private sector in the production of nurses in India, Kenya, South Africa and Thailand. Hum Resour Health. 2013;11:1–14. doi: 10.1186/1478-4491-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology. Cervical Cancer version 1. 2014 Available at http://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed March 13, 2014.