To the Editor
Although early reports of exposure to synthetic cannabinoids described a benign course,1 with little need for emergency care, on August 24, 2013, patients began to present to Denver emergency departments with severe symptoms after exposure to a novel synthetic cannabinoid known locally as “black mamba.” The Colorado Department of Public Health and Environment (CDPHE) was notified on September 3. Medical toxicologists and CDPHE epidemiologists developed a case definition and began prospective monitoring with assistance from the Centers for Disease Control and Prevention. Records from poison control centers, care providers in nonhospital settings, and law enforcement were reviewed. A total of 263 cases of possible exposure to the synthetic cannabinoid that met the CDPHE definition were identified statewide for the period August 21 to September 19. Among these cases, only 15 had been identified by the state poison control call-in centers.
Among the 263 cases identified, there were 76 patients who presented to the emergency departments at two teaching hospitals in Denver and Aurora. Exposure was confirmed by means of patient history, bedside consultation, or laboratory analyses of products recovered from patients. The majority of cases involved single-agent ingestions; most patients were young men, and symptoms included altered mental status, tachycardia followed by bradycardia, and seizures (for additional details see the Supplementary Appendix, available with the full text of this letter at NEJM.org). The care of most patients was managed in the emergency department, but 7 patients required admission to intensive care units. The outbreak then ended abruptly; only 10 cases were reported at these two hospitals from September 13 to October 25.
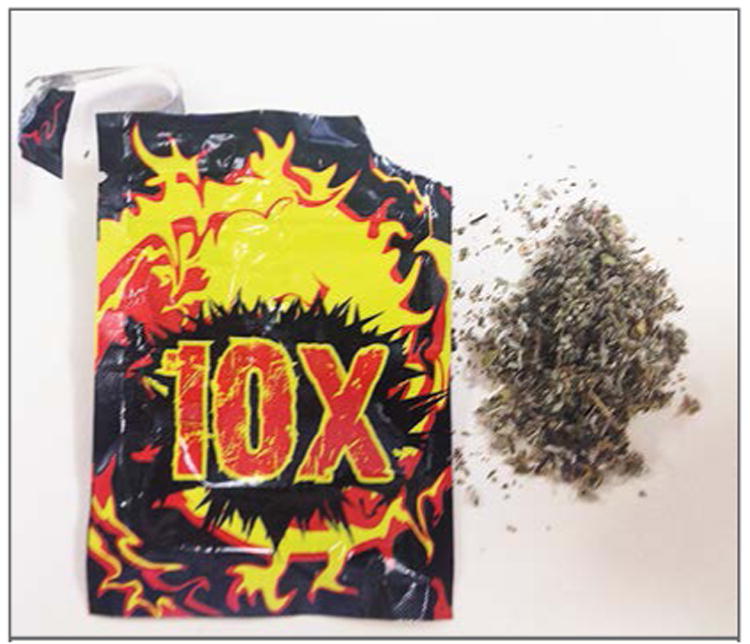
Multiple product brands (Fig. 1) were recovered from patients through a joint effort by hospital staff and law enforcement officials, and a consistent molecule was identified by the Denver Police Crime Laboratory with the use of mass spectrophotometry. The molecule, known as ADB-PINACA (N-[1-amino-3,3-dimethy-1-oxobutan-2-yl]-1-pentyl-1H-indazole-3-carboxamide), was a novel synthetic cannabinoid. We are not aware of any laboratory that can detect ADB-PINACA in blood or urine.
Figure 1. Representative Sample of Synthetic Cannabinoid Recovered from an Intoxicated Patient.
During this outbreak, exposure to ADB-PINACA was associated with neurotoxicity and cardiotoxicity. Although the effects of exposures to first-generation synthetic cannabinoids are largely benign,1 newer products have been associated with seizures,2 ischemic stroke,3 and cardiac toxicity,4 possibly due to increased potency.5 Keys to this investigation included the recognition by providers of a novel drug of abuse, coordination with the CDPHE to develop a case questionnaire, and rapid analysis of recovered products. Educational efforts included case management guidelines disseminated by the poison center, public health outreach through local news broadcasts, and informational fliers placed on buses and in the bathrooms of local clubs and bars. Medical toxicologists, public health officials, and law enforcement officials worked together to determine the cause of symptoms, develop the most effective treatment, and limit the distribution of this novel and potentially dangerous synthetic cannabinoid.
Supplementary Material
Acknowledgments
Supported by an EMF Research Training Fellowship and a grant from the NIH, National Center for Advancing Translational Sciences, to the Colorado Clinical and Translational Sciences Institute (UL1 TR000154, to Dr. Monte) and the Rocky Mountain Poison and Drug Center.
Footnotes
The contents of this work are the sole responsibility of the authors and do not necessarily represent the views of the Emergency Medicine Foundation (EMF), the National Institutes of Health (NIH), or the Rocky Mountain Poison and Drug Center.
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Andrew A. Monte, Email: andrew.monte@ucdenver.edu, University of Colorado School of Medicine Aurora, CO.
Alvin C. Bronstein, Rocky Mountain Poison and Drug Center Denver, CO
Dazhe J. Cao, Rocky Mountain Poison and Drug Center Denver, CO
Kennon J. Heard, University of Colorado School of Medicine Aurora, CO
Jason A. Hoppe, University of Colorado School of Medicine Aurora, CO
Christopher O. Hoyte, University of Colorado School of Medicine Aurora, CO
Janetta L. Iwanicki, Rocky Mountain Poison and Drug Center Denver, CO
Eric J. Lavonas, Rocky Mountain Poison and Drug Center Denver, CO
References
- 1.Hoyte CO, Jacob J, Monte AA, Al-Jumaan M, Bronstein AC, Heard KJ. A characterization of synthetic cannabinoid exposures reported to the National Poison Data System in 2010. Ann Emerg Med. 2012;60:435–8. doi: 10.1016/j.annemergmed.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Harris CR, Brown A. Synthetic cannabinoid intoxication: a case series and review. J Emerg Med. 2013;44:360–6. doi: 10.1016/j.jemermed.2012.07.061. [DOI] [PubMed] [Google Scholar]
- 3.Bernson-Leung ME, Leung LY, Kumar S. Synthetic cannabis and acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013 Oct 8; doi: 10.1016/j.jstrokecerebrovasdis.2013.07.030. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Young AC, Schwarz E, Medina G, et al. Cardiotoxicity associated with the synthetic cannabinoid, K9, with laboratory confirmation. Am J Emerg Med. 2012;30:1320.e5–1320.e7. doi: 10.1016/j.ajem.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Kronstrand R, Roman M, Andersson M, Eklund A. Toxicological findings of synthetic cannabinoids in recreational users. J Anal Toxicol. 2013;37:534–41. doi: 10.1093/jat/bkt068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


