Abstract
Recent research indicates that protective behavioral strategies (PBS)—previously established as effective self-regulating tools for reducing alcohol risk among college students—may be especially useful for students with poor mental health, who are shown to be at heightened risk for alcohol-related harm. The current study examined the moderating influence of mental health (depression and anxiety severity), gender, and race (White, Asian) in the relationship between PBS use and alcohol-related negative consequences. Participants were 1,782 undergraduate students from two West Coast universities who reported past month incidence of heavy episodic drinking. Students reported on their drinking, experience of alcohol-related consequences, use of PBS, and depression and anxiety symptomatology. Overall, results demonstrated that among participants experiencing depression or anxiety, greater PBS utilization was associated with significantly lower levels of alcohol-related consequences, even after controlling for drinking and other predictors. However, findings also revealed important distinctions in the potential effectiveness of PBS by depression/anxiety severity and racial-gender subgroup, such that Asian men with poor mental health appeared to garner unique and substantial benefit (i.e., lesser consequences) from increased PBS use. Further, PBS were found to offer substantial protective benefit for White females, irrespective of mental health. This study points to the potential for targeted PBS-specific skills training and interventions to minimize alcohol-related risks faced by the growing subpopulation of college students experiencing psychological distress, and further highlights important race-gender differentials.
Keywords: alcohol, college students, protective behavioral strategies, anxiety, depression, gender, race
The relatively high overall prevalence of poor mental health on U.S. college campuses is well-established (American College Health Association, 2008, 2011; Blanco et al., 2008; Eisenberg, Gollust, Golberstein, & Hefner, 2007; Hunt & Eisenberg 2010). Nationally representative data show that almost 11%, 12%, and 18% of college students meet DSM-IV criteria for mood, anxiety and personality disorders, respectively (Blanco et al., 2008). A recent nationwide survey found that within the past year, 31.1% of the college students surveyed reported having felt depressed at levels that caused functional impairment and a majority reported experiencing overwhelming anxiety (American College Health Association, 2011). Moreover, studies indicate substantial increases in the number of students with severe and chronic psychological problems (Barr, Rando, Krylowicz, & Winfield, 2010; Benton, Robertson, Tseng, Newton, & Benton, 2003; Gallagher, 2009; Kadison & DiGeronimo, 2004). These trends are particularly concerning since poor mental health may exacerbate a variety of challenges already experienced by college students.
Poor Mental Health and Alcohol Outcomes
Alcohol use, especially heavy episodic drinking (HED; 4+/ 5+ drinks per drinking occasion for women/men), is a significant health and safety concern among both college administrators and public health officials. Not only do more than 40% of college students report engaging in HED within the past two-week period (Hingson, Heeren, Winter, & Wechsler, 2005; Wechsler & Nelson, 2008), but these students are four times more likely than peers to meet DSM-IV criteria for alcohol abuse or dependence (Knight et al., 2002). The consequences of collegiate alcohol misuse, such as problematic physical, academic, legal, and sexual outcomes, have been widely documented (Hingson et al., 2005; Hingson, Zha, Weitzman, 2009). The risk for encountering negative alcohol-related outcomes, including alcohol use disorders, is higher among students experiencing depression (Camatta & Nagoshi, 1995; Martens et al., 2008; Miller, Miller, Verhegge, Linville, & Pumariega, 2002; Weitzman, 2004), anxiety (Geisner, Larimer, & Neighbors, 2004; Kushner, Sher & Erickson, 1999; Litt, Lewis, Blayney, & Kaysen, 2013), and poor overall mental health (Geisner, Larimer, & Neighbors, 2004; LaBrie, Kenney, & Lac, 2010). Students experiencing psychological distress may consume alcohol for several reasons (e.g., avoidant coping, lowered drinking refusal self-efficacy, increased salience of alcohol cues) that exacerbate risks for alcohol consequences (Ham & Hope, 2003; Kuntsche, Knibbe, Gmel & Engels, 2005; Park, Armeli, & Tennen, 2004; Park & Grant, 2005; Simons, Gaher, Correia, Hansen, & Christopher, 2005).
In order to more effectively inform targeted harm reduction efforts, previous researchers studying the comorbidity of poor mental health and substance misuse have commented on the need for both increased focus on college populations and further exploration of subgroup (i.e., gender, racial-ethnic status) differences (Cranford, Eisenberg, & Serras, 2009; O’Brien et al., 2004). For example, not only are college women more likely to experience psychological distress than college men (Pace & Trapp, 1995; Silverman, 2004; Weitzman, 2004), but women suffering from depression face an elevated risk for alcohol-related harms, over and above drinking, compared to both their same-sex peers as well as men experiencing depression (Harrell & Karim, 2008; Weitzman, 2004). Similarly, among males, higher levels of depressive symptoms correspond with greater daily alcohol use (Pedrelli et al., 2011), and generalized anxiety disorder is associated with frequent HED more strongly in men than women (Cranford, Eisenberg, & Serras, 2009). These studies indicate that the intersection of gender and particular mental health challenges may play an important role in college students’ alcohol behaviors and associated outcomes.
With regard to racial-ethnic differences, Asians are of particular interest since their representation is rapidly growing at American colleges (Astin, Oseguera, Sax, & Korn, 2002; U.S. Department of Education, 2011). Asian American students’ enrollment at 4-year undergraduate institutions increased 40.1% from 1994 to 2004 (Cook & Cordova, 2007). Further, compared to other ethnic groups, Asian Americans have higher levels of psychological distress but lower rates of mental health treatment utilization (Atkinson & Gim, 1989; Eisenberg & Chung, 2012; Kearney, Draper, & Baron, 2005; Lee, Law, Eo, & Oliver, 2002; Okazaki, 1997; Sue, Fujino, Hu, Takeuchi, & Zane, 1991). Moreover, depressive symptoms are linked to alcohol behaviors in this population (Iwamoto, Liu, & McCoy, 2011).
Evidence shows escalations in heavy alcohol use and problems among Asian college students (Grant, Dawson, Stinson, Chou, Dufour, & Pickering, 2004; Wechsler, Dowdall, Maenner, Gledhill-Hoyt, & Lee, 1998; Lee, Kuo, Seibring, Nelson, & Lee, 1998, 2002). Despite traditional conceptualizations of Asians as low risk drinkers, recent research has documented that Asians who do drink exhibit trajectories of increasing HED and alcohol problems during their college years (Iwamoto, Corbin, & Fromme, 2010). In fact, rates of alcohol dependence increased exponentially from 1991–1992 to 2001–2002 among young adult Asian American males (4.09–10.22%) and females (0.74 – 3.89%) (Grant, Dawson, Stinson, Chou, Dufour, & Pickering, 2004). Yet despite the increasing prevalence of alcohol abuse and high rates of poor mental health among Asian American college students, research examining these factors as they relate to alcohol risk among this subgroup is lacking.
Protective Behavioral Strategies
A significant body of research indicates that students utilizing protective behavioral strategies (PBS; Martens et al., 2005; e.g., determining not to exceed a set number of drinks, using a designated driver) tend to drink less and experience fewer consequences than peers not employing PBS (Araas & Adams, 2008; Benton et al., 2004; Borden et al., 2011; Haines, Barker, & Rice, 2006; Martens et al., 2004; Patrick, Lee, & Larimer, 2011). PBS use also varies by gender; PBS are more likely to be used, and implemented more effectively by college women than men (Benton et al., 2004; Delva et al. 2004; Frank, Thake, & Davis, 2012; Haines et al., 2006; Nguyen, Walters, Wyatt, & DeJong, 2011; Walters, Roudsari, Vader, & Harris, 2007). However, the vast majority of these studies have been conducted using college samples heavily comprised of White students. Although research examining the effectiveness of PBS among Asians is limited, evidence indicates that race plays a role in overall PBS use as well as types of PBS endorsed. White students, for instance, tend to utlize PBS focused on serious harm reduction, whereas Asian students are found more likely to use PBS that emphasize stopping or limiting alcohol consumption (LaBrie, Lac, Kenney, & Mirza, 2011). Nonetheless, research examining the extent to which PBS use and effectiveness may differ by distinct racial-gender subgroups is necessary.
The few studies examining the role of mental health in the PBS use and alcohol outcomes relationship indicate that PBS may offer unique benefits to students experiencing psychological distress. For instance, although college students and young adults experiencing mental distress or possessing poor self-regulation abilities have demonstrated a lower likelihood of employing PBS, PBS use among these individuals appears especially effective in reducing alcohol-related harms (D’Lima, Pearson, & Kelley, 2012; LaBrie, Kenney, Lac, Garcia, & Ferraiolo, 2009; Litt, Lewis, Blayney, & Kaysen, 2013; Martens et al., 2008), even over and above alcohol use (LaBrie, Kenney, & Lac, 2010). These findings suggest that students experiencing mental health challenges may lack the cognitive or self-regulation resources to protect themselves against alcohol-related harm, and hence equipping them with easy-to-implement PBS may greatly reduce their overall alcohol risk. Examination of subgroup differences (e.g., gender and race/ethnicity) is needed to inform PBS-based alcohol harm reduction initiatives that seek to target students suffering from poor mental health.
The Current Study
The current study extends previous research by examining the differential impact of both depression and anxiety symptomatology, as well as exploring gender and race differences in the relationship between PBS use and alcohol-related consequences. Overall, we expected greater PBS use to be associated with lower levels of alcohol consumption and consequences, and greater utilization of PBS to be most protective for students reporting greater levels of depression or anxiety. The central aim of this study, however, was to examine the extent to which the interaction of mental health, gender, and race moderated the relationship between PBS use and alcohol consequences while controlling for alcohol consumption. Based on previous research, we anticipated that greater use of PBS would be particularly effective in reducing alcohol consequences among women (White or Asian) experiencing higher levels of depression or anxiety. Finally, given the lack of existing research examining factors that may protect Asians from alcohol-related risk, we also sought to explore how PBS may buffer alcohol-related consequences as a function of mental health, gender, and race. This integrative examination of these interrelationships will provide insight into the subgroups that may benefit most from protective strategies and, in turn, potentially inform targeted alcohol harm reduction interventions.
Method
Participants and Procedures
Participants were 1,782 undergraduate students from two West Coast universities, a large public university enrolling approximately 30,000 students and a medium-sized private university with an enrollment of about 6,000 students. Participants were part of a larger intervention study. A total of 11,069 students were randomly selected and invited via mail and email to participate in a study about alcohol use among college students. Participants accessed the screening survey via a designated URL provided within the invitation and consented to participate by signing an IRB-approved online consent form.
Of the 4,983 (45.0%) students who completed the screening survey, 2,032 (40.8%) met screening criteria—reporting White or Asian racial status and having had at least one past month heavy episodic drinking (HED) experience—and were immediately invited to participate in a baseline survey. Participants were paid a nominal stipend upon completion of both the screening and baseline surveys. The current sample is comprised of 1,782 (87.7% of those meeting screening criteria) students who completed the subsequent baseline survey. The current sample differed somewhat from participants who met screening criteria but did not complete the baseline survey: on average, non-completers reported more weekly drinking (t = −2.42, p = .016), and were more likely to be female [X2 (1, N = 2,032) = 6.51, p = .011] and attend the large public university [X2 (1, N = 2,032) = 4.24, p = .039]. No significant differences emerged with respect to alcohol-related negative consequences, mental health measures or race. Participants in the present sample had a mean age of 19.94 years (SD = 1.33), and 56.4% were female. The sample’s racial breakdown was 76.3% White and 23.7% Asian. Racial-gender subgroups were as follows: White men (n = 581), White women (n = 778), Asian men (n = 196), and Asian women (n = 227).
Measures
The current study examined students’ reported sex, race, alcohol consumption and consequences, depression and anxiety, and use of PBS.
Weekly drinks
Alcohol consumption was assessed using the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985; Dimeff, Baer, Kivlahan, & Marlatt, 1999). Participants were instructed to “consider a typical week within the past month” before answering, “How many drinks did you typically consume on a Monday? Tuesday?” and so on. Students’ open-ended responses across the seven week days were summed to form an average total weekly drinks variable.
Weekly HED occasions
HED was measured using students’ responses to the DDQ measure. The number of week days in which participants reported typically consuming at least four (women) or five (men) drinks were summed to calculate a weekly heavy episodic drinking variable used in the ANOVA and correlation tables only.
Alcohol-related negative consequences
The 23-item Rutgers Alcohol Problems Inventory (RAPI; White & Labouvie, 1989) (α = .89) measured alcohol-related negative consequences encountered in the past month. Participants used a four-point scale (0 = Never to 4 = 10 or more times) to report frequency of experiencing a problematic drinking outcome during this time period. Items included, “Neglected your responsibilities,” “Had a fight, argument or bad feelings with a friend,” and “Missed out on other things because you spent too much money on alcohol.” Responses were summed to yield an “alcohol-related negative consequences” variable.
Depression
Participants’ past-week symptoms of depression were assessed using the psychometrically validated 20-item Center for Epidemiologic Studies Depression Scale, (CES-D; Radloff, 1977) (α = .90). Items included, “I had crying spells,” “I felt that everything I did was an effort,” and “I felt sad” and were measured on a four-point scale (0 = Rarely or none of the time [less than 1 day] to 3 = Most or all of the time [5–7 days]). The CES-D has been demonstrated as a valid and reliable measure in general populations of adolescent and young adults (Cuijpers, Boluijt, & van Straten, 2008; Radloff, 1991), and has been shown to be particularly effective is assessing depressive severity among college students (Santor, Zuroff, Ramsay, Cervantes, & Palacios, 1995). Summed scores greater or equal to 16 indicate clinically significant depressive symptomatolgy.
Anxiety
The 21-item Beck Anxiety Inventory (BAI; Beck and Steer, 1993) (α = .90) assessed cognitive and behavioral symptoms of anxiety experienced in the past three months. Symptoms include “numbness or tingling,” “fear of dying,” and “fear of losing control” and were assessed on a scale ranging from 0 (Not at all) to 3 (Severely). The BAI has previously been found to have acceptable reliability and validity (Beck, Epstein, Brown, & Steer; 1988; Fydrich, Dowdall, & Chambless, 1992). Summed BAI scores indicate anxiety severity as follows: minimal (0–7), mild (8–15), moderate (16–25), and high (26–63).
Protective Behavioral Strategies
Participants’ frequency of PBS use in drinking contexts was assessed using the 15-item Protective Behavioral Strategies Scale (PBSS; Martens, et al. 2005) (α = .81), a psychometrically validated measurement of alcohol-related protective behaviors (Benton et al., 2004; Martens et al., 2005; Martens, Ferrier, & Cimini, 2007; Martens, Pedersen, LaBrie, Ferrier & Cimini, 2007; Walters et al. 2007). The questionnaire assesses PBS use on a scale of 1 (never) to 5 (always) across three subscales: stopping/limiting drinking (7 items; α = .80; e.g., “Determine not to exceed a set number of drinks”), manner of drinking (5 items; α = .62; e.g., “Drink slowly, rather than gulp or chug,”), and serious harm reduction (3 items; α = .69; e.g., Know where your drink has been at all times”).
Analyses
Prior to analyses, we explored the distributional properties of all variables. Alcohol-related negative consequences was positively skewed, and thus its square-root transformation was used in the regression analyses (Cohen, Cohen, West, & Aiken, 2003). None of the composites used in analyses exceeded skewness levels of 1.4 or kurtosis levels of 1.7.
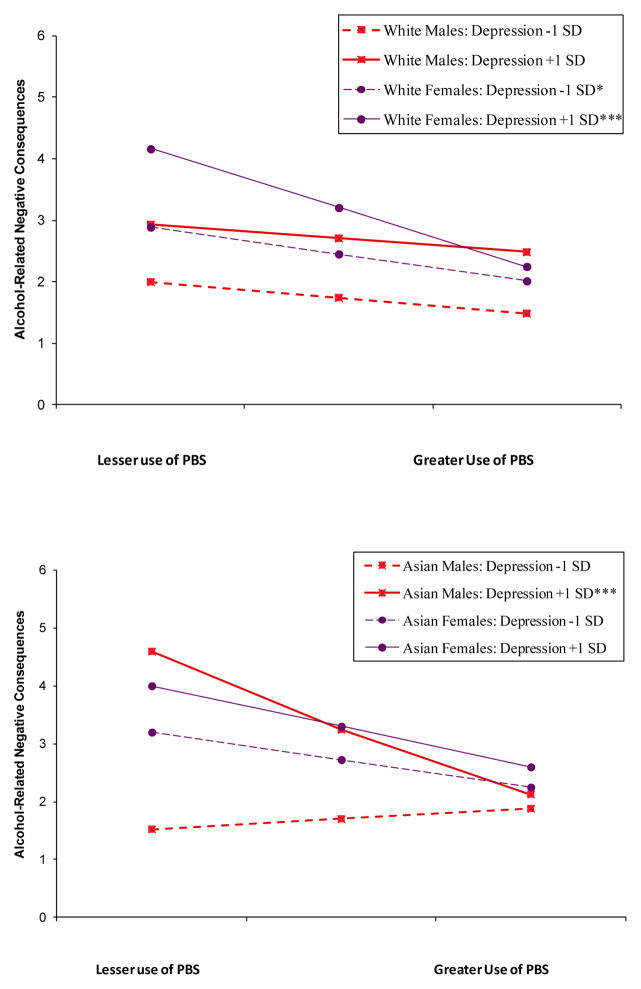
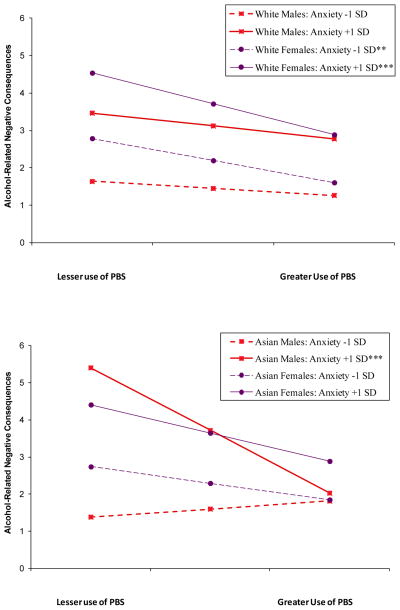
First, we examined mean differences in drinking, alcohol-related consequences, mental health, and PBS using a 2 × 2 (Gender [male, female] × Race [White, Asian]) analysis of variance (ANOVA) (see Table 1). Next, a full sample correlation matrix is presented (Table 2). Finally, we performed two hierarchical multiple regression models incorporating four-way interactions to assess the extent to which mental health status (depression or anxiety), gender, and race statistically moderated the use of PBS on the outcome of alcohol-related negative consequences experienced in the past month (Table 3). Interpretation of the four-way interactions controlled for all other effects in the model, including nested lower-order two- and three-way interaction effects (Aiken & West, 1991; Cohen, Cohen, West, & Aiken, 2002). All predictors were standardized prior to computation of interaction terms to avoid statistical artifacts associated with multicollinearity, and no issues with tolerance were encountered. As displayed in Figures 1 and 2, higher-order interactions were graphed according to established guidelines (Aiken & West, 1991); all continuous predictor and moderator variables (PBS and mental health) were plotted at one standard deviation below (low) and above (high) the respective mean and dichotomous variables (gender and race) were plotted using their meaningful categorical levels.1 The use of interaction terms was deemed superior to split subgroup analyses in examining how the PBS-consequences relationship varied across severity of mental health, gender, and race (including the interrelationship of the moderating variables). However, in order to explicate the effects across race and sex, significant four-way interactions were decomposed to examine respective three- and two-way models restricted by respective subgroup.
Table 1.
Mean Differences in Drinking, Alcohol-Related Consequences, Depression, Anxiety, and Use of Protective Behavioral Strategies (PBS) as a Function of Gender and Race
| Measure | Gender
|
Race
|
Gender × Race | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n = 777) | Female (n = 1,005) | White (n = 1,359) | Asian (n = 423) | ||||||||||||
|
|
|
|
|||||||||||||
| Mean | SD | % | Mean | SD | % | F-test | Mean | SD | % | Mean | SD | % | F-test | F-test | |
|
|
|
|
|||||||||||||
| Alcohol-related | |||||||||||||||
| Weekly drinks | 13.90 | 10.26 | 8.57 | 6.51 | 113.68*** | 11.63 | 9.03 | 8.54 | 7.37 | 53.70*** | 4.57* | ||||
| Weekly HED occasions | 1.49 | 1.33 | 0.73 | 1.06 | 120.78*** | 1.15 | 1.27 | 0.77 | 1.08 | 41.56*** | 1.63 | ||||
| Past month consequences | 4.23 | 5.67 | 3.68 | 4.39 | 3.85 | 3.96 | 4.87 | 3.81 | 5.36 | 0.37 | 0.01 | ||||
| Mental Health | |||||||||||||||
| Depression | 12.45 | 8.97 | 14.51 | 9.28 | 25.99*** | 12.99 | 8.97 | 15.61 | 9.64 | 26.65*** | 2.90 | ||||
| Low | 70.9 | 62.8 | 69.7 | 55.3 | |||||||||||
| High | 29.1 | 37.2 | 30.3 | 44.7 | |||||||||||
| Anxiety | 6.90 | 6.89 | 8.72 | 6.91 | 26.73*** | 7.77 | 6.68 | 8.43 | 7.77 | 3.26 | 0.61 | ||||
| Minimal | 66.0 | 51.8 | 58.4 | 56.7 | |||||||||||
| Mild | 23.3 | 31.7 | 28.5 | 26.6 | |||||||||||
| Moderate | 6.8 | 13.5 | 10.2 | 11.8 | |||||||||||
| Severe | 3.9 | 3.0 | 2.9 | 4.9 | |||||||||||
| PBS use | |||||||||||||||
| Overall | 43.69 | 7.88 | 48.35 | 8.30 | 111.20*** | 46.21 | 8.16 | 46.66 | 9.29 | 1.74 | 0.22 | ||||
| Stopping/limiting drinking | 17.87 | 5.06 | 19.88 | 5.47 | 54.28*** | 18.67 | 5.14 | 20.07 | 5.97 | 24.47*** | 0.58 | ||||
| Manner of drinking | 13.79 | 3.25 | 14.92 | 3.26 | 43.38*** | 14.50 | 3.24 | 14.17 | 3.46 | 2.75 | 0.60 | ||||
| Serious harm reduction | 12.04 | 2.28 | 13.56 | 1.89 | 153.28*** | 13.04 | 2.09 | 12.42 | 2.48 | 23.16*** | 1.71 | ||||
Note. Weekly drinks and HED (heavy episodic drinking) occasions assess typical weekly drinking behaviors in the past month; Depression (CESD) severity is low (0–15) or high (≥16); anxiety (BAI) severity is minimal (0–7), mild (8–15), moderate (16–25), or severe (>25).
p < .05.
p < .01.
p < .001.
Table 2.
Correlation Matrix Using Full Sample
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 9a | 9b | 9c | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sex (female)a | -- | |||||||||||
| 2 | Race (Asian)b | −.03 | -- | ||||||||||
| 3 | Campus (private)c | .07** | −.28*** | -- | |||||||||
| 4 | Weekly drinks | −.30*** | −.15*** | .10*** | -- | ||||||||
| 5 | Weekly HED occasions | −.30*** | −.13*** | .08*** | .88*** | -- | |||||||
| 6 | Alcohol-related consequences | −.06* | −.01 | .10*** | .40*** | .35*** | -- | ||||||
| 7 | Depression | .11*** | .12*** | .04 | −.05 | −.04 | .26*** | -- | |||||
| 8 | Anxiety | .13*** | .04 | .05 | .00 | −.01 | .32*** | .62*** | -- | ||||
| 9 | PBS Use | .27*** | .02 | .06* | −.34*** | −.35*** | −.25*** | −.05 | −.03 | -- | |||
| PBS Subscales | |||||||||||||
| 9a | Stopping/limiting drinking | .19*** | .11*** | .02 | −.22*** | −.24*** | −.15*** | .01 | .01 | .88*** | -- | ||
| 9b | Manner of drinking | .17*** | −.04 | .04 | −.35*** | −.37*** | −.21*** | −.05* | −.05* | .74*** | .42*** | -- | |
| 9c | Serious harm reduction | .34*** | −.12*** | .13*** | −.23*** | −.22*** | −.26*** | −.12*** | −.08*** | .57*** | .31*** | .29*** | -- |
Note. N = 1,782. Weekly drinks and HED occasions assessed typical weekly drinking in past month. Alcohol-related negative consequences assessed for the past month.
For Sex, reference level is male.
For Race, reference level is White.
For Campus, reference level is large public university.
p < .05.
p < .01.
p < .001.
Table 3.
Hierarchical Mulitple Regression Models Predicting Past Month Alcohol-Related Negative Consequences by Mental Health, PBS Use, Sex, and Race
| Model 1: Depression | Model 2: Anxiety | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | Δ R2 | Step 1
|
Step 2
|
Step 3
|
Step 4
|
Step 5
|
Predictor | Δ R 2 | Step 1
|
Step 2
|
Step 3
|
Step 4
|
Step 5
|
||||
| β | β | β | β | B | SE | β | β | β | β | β | B | SE | β | ||||
| Step 1: | .29*** | .27*** | |||||||||||||||
| Campusa | .05* | .06** | .06** | .06** | .07 | .02 | .06** | Campus | .05* | .06** | .06** | .06** | .07 | .02 | .06** | ||
| Weekly drinks | .44*** | .43*** | .43*** | .43*** | .51 | .03 | .43*** | Weekly drinks | .45*** | .43*** | .43*** | .43*** | .51 | .03 | .43*** | ||
| Anxiety | .30*** | .22*** | .21*** | .21*** | .25 | .03 | .21*** | Depression | .27*** | .12*** | .12*** | .11*** | .14 | .03 | .11*** | ||
| Step 2: | .03*** | .05*** | |||||||||||||||
| Depression | .12*** | .12*** | .11*** | .13 | .03 | .11*** | Anxiety | .22*** | .21*** | .21*** | .25 | .03 | .21*** | ||||
| PBS use | −.13*** | −.13*** | −.13*** | −.15 | .03 | −.13*** | PBS use | −.13*** | −.13*** | −.13*** | −.16 | .03 | −.13*** | ||||
| Sexb | .08*** | .08*** | .08*** | .10 | .03 | .08*** | Sex | .08*** | .08*** | .08*** | .09 | .03 | .08*** | ||||
| Racec | .02 | .02 | .01 | .02 | .03 | .02 | Race | .02 | .02 | .01 | .02 | .03 | .02 | ||||
| Step 3: | .01* | .01 | |||||||||||||||
| D × Pd | −.05* | −.04 | −.04 | .02 | −.03 | A × P | −.05* | −.03 | −.04 | .02 | −.03 | ||||||
| P × S | −.03 | −.03 | −.05 | .03 | −.04 | P × S | −.03 | −.03 | −.04 | .03 | −.03 | ||||||
| P × R | .01 | .01 | .00 | .02 | .00 | P × R | .00 | .00 | −.01 | .02 | −.01 | ||||||
| D × S | −.04 | −.03 | −.05 | .03 | −.04 | A × S | −.03 | −.03 | −.04 | .02 | −.03 | ||||||
| D × R | .02 | .02 | .01 | .02 | .01 | A × R | .01 | .01 | −.00 | .02 | −.00 | ||||||
| S × R | −.02 | −.01 | −.01 | .03 | −.01 | S × R | −.02 | −.02 | −.02 | .02 | −.01 | ||||||
| Step 4: | .004 | .01** | |||||||||||||||
| D × P × S | .01 | .00 | .02 | .00 | A × P × S | .05* | .03 | .02 | .03 | ||||||||
| D × P × R | −.04 | −.03 | .02 | −.03 | A × P × R | −.05* | −.05 | .02 | −.05* | ||||||||
| D × S × R | −.03 | −.03 | .02 | −.02 | A × S × R | −.01 | −.01 | .02 | −.01 | ||||||||
| P × S × R | .03 | .02 | .02 | .02 | P × S × R | .03 | .03 | .02 | .03 | ||||||||
| Step 5: | .002* | .003** | |||||||||||||||
| D × P × S × R | .05 | .02 | .05* | A × P × S × R | .05 | .02 | .06** | ||||||||||
| Total R2 | .34 | .34 | |||||||||||||||
Note. N = 1,782. Δ R2 = R-square change; Betas reported at each step, and unstandardized coefficients (Bs and Standard Errors) reported at the final step with all predictors entered.
For Campus, 0 = large public university and 1 = medium-sized private university.
For Sex, 0 = male and 1 = female.
For Race, 0 = White and 1 = Asian.
For interaction terms, D = Depression, A = Anxiety, P = PBS, S = Sex, and R = Race.
p < .05.
p < .01.
p < .001.
Figure 1.
Four-way interaction illustrating Depression × PBS Use × Sex × Race on alcohol-related negative consequences, controlling for drinking. Plots illustrate use of PBS by depression (low versus high) as a function of gender among Whites and Asians on consequences.
Figure 2.
Four-way interaction illustrating Anxiety × PBS Use × Sex × Race on alcohol-related negative consequences, controlling for drinking. Plots illustrate use of PBS by anxiety (low versus high) as a function of gender among Whites and Asians on consequences.
Note. Alcohol-related negative consequences was square root transformed for statistical analyses. For interpretability, values in the figures are depicted in their original metric.
*p < .05, **p < .01, and ***p < .001 denote significant slopes.
Results
Mean Differences as a Function of Gender and Race
Over one-third of the current sample reported levels of psychological distress deemed clinically significant. Among Asians, nearly half (44.7%) met the criteria for clinically significant depression. As shown in Table 1, main effects for gender show that women reported higher depressive and anxiety symptoms, and greater use of PBS (overall and by PBS subscale) compared to men. Men reported greater typical weekly drinks and HED than women, although no significant mean differences in the experience of past month alcohol consequences emerged. Main effects for race demonstrated that Whites, relative to Asians, reported greater weekly drinking and HED (but not alcohol-related consequences), and Asians reported higher depressive (but not anxiety) symptomatology. Although there were no significant mean differences on overall PBS use, Asians reported higher use of stopping/limiting drinking and Whites reported higher serious harm reduction PBS. A statistically significant interaction effect between gender and race was found for reported weekly drinking, such that White males drank significantly more than other racial-gender subgroups.
Correlations
As shown in Table 2, a full sample correlation matrix exhibits bivariate associations between sex, race, campus, weekly drinks, weekly HED, past month alcohol-related consequences, depression, anxiety, and use of PBS (overall and subscales). As expected, all drinking-related variables (weekly, HED, and consequences) were positively correlated (all ps < .001), and each was negatively correlated with PBS and PBS subscales (all ps < .001). Depression and anxiety were intercorrelated (p < .001), positively correlated with experience of alcohol consequences (both ps < .001), and inversely correlated with manner of drinking (p = .033 and p = .049, respectively) and serious harm reduction PBS (both ps < .001).
Hierarchical Multiple Regression Models
Each model was estimated as follows: Step 1 included all covariates: campus, weekly drinks, and mental health (anxiety in the model examining depression; depression in the model examining anxiety). Given the high correlation between anxiety and mental health, each model controlled for the other mental health index. Main effects were entered in Step 2: mental health (depression or anxiety), PBS use, sex, and race. Step 3 included all two-way interaction terms: Mental Health (depression or anxiety) × PBS; PBS × Sex; PBS × Race; Mental Health × Sex; Mental Health × Race; and Sex × Race. Next, three-way interactions were added at Step 4: Mental Health × PBS × Sex; Mental Health × PBS × Race; Mental Health × Sex × Race; and PBS × Sex × Race. For each model, the four-way interaction term, Mental Health × PBS × Sex × Race, was entered at the final step (Step 5).
As shown in Table 3, each of the blocks of predictors in steps 1 and 2 contributed significantly (p < .001) to the explained variance in alcohol-related consequences at its respective step of entry, over and above prior steps. In Model 1 (Depression), Step 3 (p = .019) and Step 5 (p = .013) were significant. In Model 2 (Anxiety), Step 4 (p = .007) and Step 5 (p = .007) were significant. Final models with all predictors entered were significant for depression, F(18,1763) = 49.28, p < .001 and anxiety, F(18,1763) = 49.53, p < .001. In both final models, the following variables uniquely and significantly predicted alcohol-related negative consequences over and above other predictors: being a student at a medium-sized private (versus large public) university (β = .06, p = .006); more weekly drinks (β = .43, p < .001); greater levels of anxiety (β = .21, p < .001); greater levels of depression (β = .11, p < .001); lower PBS use (β = −.13, p < .001); and being female (β = .08, p < .001). Notably, in Step 3 of each model, mental health interacted with PBS use (Depression × PBS [β = −.05, p = .027]; Anxiety × PBS [β = −.05, p = .027]) such that among participants with higher (versus lower) levels of mental distress, greater utilization of PBS was significantly related to lesser alcohol-related consequences (graphs not displayed). In Step 4 of Model 2, Anxiety × PBS × Sex (β = .05, p = .027) and Anxiety × PBS × Race (β = −.05, p = .016) were significant. In Model 1, the four-way interaction, Depression × PBS × Sex × Race, was significant (β = .05, p = .013) and is graphed in Figure 1. In Model 2, Anxiety × PBS × Sex × Race was significant (β = .06, p = .007) and is illustrated in Figure 2.
Interpreting the four-way interactions
With respect to depression, simple slope analyses revealed that slopes were significantly different from zero among White females at higher (t = −3.82, p < .001) and lower (t = −2.44, p = .015) levels of depression and among Asian males at higher levels of depression only (t = −3.40, p < .001) (Figure 1). Likewise, in the model examining anxiety, simple slope analyses were significant among White females at higher (t = −3.36, p < .001) and lower (t = −3.02, p = .003) levels of anxiety and Asian males at higher levels of anxiety (t = −4.00, p < .001) (Figure 2).
Supplemental analyses examining three-way interactions (Mental Health × PBS × Sex) within racial subgroups were conducted to decompose the significant interactions. No significant interactions emerged among Whites, but among Asians, Depression × PBS × Sex (p = .008) and Anxiety × PBS × Sex (p = .002) were significant. Further decomposition revealed a significant mental health by PBS interaction in the depression (p < .001) and anxiety (p < .001) models when restricted to Asian men but not Asian women. Consistent with tests of simple slopes, these supplemental analyses indicate that PBS are uniquely protective for White women (regardless of mental health status) and Asian men with high (as opposed to low) depression or anxiety.
Discussion
As expected, greater utilization of PBS was associated with lower levels of both alcohol consumption and consequences among heavy drinking college students. Also consistent with existing research (e.g., Barr et al., 2010; Denhardt & Murphy, 2011; Gallagher, 2009; Geisner et al., 2004; Weitzman, 2004), participants in this sample indicated relatively high prevalence rates of anxiety and depression symptoms, and greater mental distress was correlated with greater levels of alcohol-related consequences. Results support the effectiveness of PBS in reducing alcohol risk among students with poor mental health overall (LaBrie et al., 2009, 2010; Martens et al., 2008); however, this study advances prior research by revealing important distinctions in the protective benefit of PBS by mental health severity as well as racial-gender subgroup. The interaction among mental health, gender, and race significantly moderated the relationship between PBS use and alcohol consequences, even after controlling for drinking and other predictors. Results indicate that White women, but not Asian women, garnered substantial benefit (i.e., lesser consequences) from greater use of PBS, irrespective of mental health status. In addition, PBS appeared uniquely beneficial for Asian men with poor (as compared to strong) mental health. By highlighting the complexity of racial-gender influences, these findings also extend previous research that has largely considered PBS to be more effectively used by females than males (Benton et al., 2004; Delva et al. 2004; Frank et al., 2012; Haines et al., 2006; Nguyen et al., 2011; Walters et al., 2007) and those with poor mental health compared to strong mental health (D’Lima et al., 2012; LaBrie et al., 2009, 2010; Litt et al., 2013; Martens et al., 2008).
This study draws attention to the potential of PBS as important self-protection tools for Asian men in particular. While the representation of Asian males on American college campuses has increased exponentially in the past two decades (Cook & Cordova, 2007; U.S. Department of Education, 2010), so too have their rates of heavy drinking and alcohol dependence (Grant et al., 2004; Wechsler et al, 2002). Given Asian men’s disinclination towards utilizing campus mental health services and preference for using personal resources to address substance misuse (e.g., Lee, Law, Eo, & Oliver, 2002; Sue, Fujino, Hu, Takeuchi, & Zane, 1991), PBS-based alcohol interventions that screen for mental health risk may be a feasible approach by which to address co-occuring mental health-alcohol problems in this subgroup. Moreover, evidence supports that interventions integrating cultural-specific approaches may be particularly effective (Griner & Smith, 2006).
Consistent with existing research, PBS use appears to protect White women from experiencing alcohol-related negative consequences. Because PBS were shown to be effective for heavy drinking White women regardless of mental health status, PBS-based skills training broadly applied to women’s groups at risk for alcohol problems offers much potential. Equipping women’s groups (e.g., sororities, single sex residence hall floors or athletic teams) with information about PBS and how to implement them before and during drinking episodes may minimize exposure to sexual harms and other negative consequences common among heavy drinking females on college campuses (Howard, Griffin & Boekeloo, 2008; Parks & Fals-Stewart, 2004). Still, these findings are particularly noteworthy for White women with higher levels of depression or anxiety who comprise a sizable segment of the college student population in the U.S. and are susceptible to co-occuring mental health-substance use problems and associated consequences (Harrell & Karim, 2008; Kessler, Crum, Warner, & Nelson, 1997; LaBrie et al., 2009, 2010; Silverman, 2004; Weitzman, 2004). In the current sample, White women with poor mental health, relative to White men or White women with strong mental health, faced significantly greater likelihood for alcohol-related consequences; however, greater PBS use appeared to offer substantial protection in reducing this risk.
Notably, the current study assessed participants’ natural use of PBS, which may not reflect the effectiveness of PBS explicitly learned. PBS skills-training approaches may enable high risk subgroups students who do not naturally use PBS to learn strategies for effectively implementing PBS. At present, college-based alcohol prevention initiatives aimed at the high-risk and growing subpopulation of students with poor mental health are lacking. PBS skills training, which has demonstrated efficacy as one facet of multi-component alcohol interventions aimed at broader student populations (Barnett, Murphy, Colby, & Monti, 2007; Larimer et al., 2007), offers an easy-to-use and cost-effective approach for reducing alcohol-related harm among multiple subgroups of students with poor mental health. Facilitator-led PBS-based interventions, both group and individual, that screen for depression or anxiety may be used to target those students who may benefit most from learning PBS. Employing concrete protective strategies appears to provide substantial protection for students who may lack the emotional regulation capability, coping skills, or social resources known to safeguard them from alcohol-related harm. Counselors at psychological centers, nurses and practitioners at student health facilities, and residence hall advisors, for instance, may be valuable conduits for informing at-risk students about PBS and discussing contexts in which strategies may be best utilized.
Although women in this sample implemented more PBS than men overall, distinct gender subgroups (i.e., White females and Asian males) were found to garner unique protective benefit from employing PBS. Indeed, students’ natural use of PBS may be reflective of cultural gender norms. For example, men may be hesitant to implement PBS perceived as weak (i.e., manner of drinking; e.g., “avoid drinking games,” “avoid trying to ‘keep up’ or ‘outdrink’ others”) whereas women may be drawn toward PBS that enable them to protect themselves from sexual harm (i.e., serious harm reduction; e.g., “make sure you go home with a friend,” “know where your drink has been at all times”). Further, differences in PBS utilization were found to differ considerably by race. Compared to White students, Asian students implemented significantly more stopping/limiting but less serious harm reduction PBS. This predilection for drinking constraint may be attributed to Asian cultural values that espouse drinking in moderation and stigmatize alcohol dependence (Lu, Engs, & Hanson, 1997; Okazaki, 2000; Yang, Phelan, & Link, 2008; Zane & Huh-Kim, 1998; Zane & Yeh, 2002), or perhaps Asians’ genetic susceptibility to the adverse effects associated with drinking-induced flushing response (e.g., facial flushing, nausea, vomiting; see Wall & Ehlers, 1995). Interestingly, recent studies using general samples of college students indicate that stopping/limiting PBS may be ineffective in reducing and may even increase risks for alcohol-related harm (Frank, Thake, & Davis, 2012; Martens et al., 2011).
In light of these findings, future research should examine how student subgroup may influence how specific PBS are optimally utilized. For instance, although some PBS may complement Asian students’ drinking practices, others may be more conducive to women’s safe drinking behaviors (e.g., “have a friend let you know when you have had enough to drink” or “know where your drink has been at all times”). Still other PBS may not resonate with certain subgroups of students; for example, some PBS may be irrelevant to depressed or anxious students who may have weak friendship networks, avoid social gatherings, or disregard serious harm to themselves. In the current results, for instance, poor mental health indices tended to be correlated with lesser use of serious harm reduction strategies (e.g., “use a designated driver,” “make sure that you go home with a friend”). Confirmatory factor analyses or student focus groups may yield important insights into the effectiveness of specific strategies with respect to race, gender or mental health that may inform PBS skills training applications.
Examining the potential moderating role of coping drinking motives, which are consistently linked to maladaptive drinking patterns, alcohol misuse, and consequences (Cooper, Agocha, & Sheldon, 2000; Karwacki & Bradley, 1996; Labouvie & Bates, 2002), in the relationship between mental health status and PBS use may be a logical next step for future research. Not only are students with psychological distress prone to consume alcohol as a means to cope with negative affect (Gonzalez, Collins, & Bradizza, 2009; Lyvers, Thorberg, Ellul, Turner, & Bahr, 2010), but recent research has shown PBS to be especially valuable in reducing alcohol abuse and dependence among students with high coping motives (Patrick et al., 2011).
Limitations
Findings are limited in a number of ways. First, self-reported data were collected using online surveys. Although participants were assured of confidentiality and self-reports are shown to be valid and reliable in evaluating alcohol use and behaviors (e.g., Maisto, Connors, & Allen, 1995), the potential for self-report bias was possible. In addition, data were cross-sectional. Research incorporating longitudinal designs may better explicate the relationships among mental health, PBS use, and both alcohol consumption and harms by assessing alcohol use and consequences prior or subsequent to PBS implementation. Specifically, PBS-based interventions that account for pre- and post-intervention assessment are warranted. Also, the current sample did not account for ethnicity beyond overall White and Asian ethnic status. Up to 15 Asian subgroups exist in the U.S., and each renders distinct alcohol-related cultural beliefs and behaviors. Korean and Filipino college students, for example, tend to endorse more positive alcohol-related expectancies and drink at higher rates than Chinese or Vietnamese peers (Chang, Shrake, & Rhee, 2008; Luczak, Wall, Shea, Byun, & Carr, 2001; Lum, Corliss, Mays, Cochran, & Lui, 2009). Further, the present analyses did not account for acculturation, which not only is a key predictor of alcohol risk (Lum et al., 2009; So & Wong, 2006) but is also associated with mental health (Miller, Yang, Hui, Choi, & Lim, 2011; Ruzek, Nguyen, & Herzog, 2011). Studies that incorporate large ethnically diverse representative samples will offer insight into the use and benefit of PBS across Asian ethnic subgroups.
Conclusion
The present study provides important implications for college administrators and clinicians interested in reducing alcohol risk among a growing segment of students experiencing mental health issues. PBS skills training and PBS-based interventions are undeveloped areas of alcohol risk prevention that appear to offer considerable promise as practical, straightforward, and cost-effective strategies for reducing alcohol-related consequences among at-risk student drinkers. Findings demonstrate that the value of PBS skills training may vary as a function of mental health, gender, and race, and thus targeted PBS-specific interventions may be warranted. More research is needed however to explicate the types of PBS as well as the processes by which PBS may be most effective among distinct subgroups of students. Nonetheless, this study lends empirical support to the potential for PBS initiatives to respond to the needs of an increasing number of college students at considerable risk for alcohol-related harm.
Acknowledgments
This research was supported by Grant R01 AA 012547-06A2 from the National Institute of Alcohol Abuse and Alcoholism (NIAAA) and a grant from ABMRF/The Foundation for Alcohol Research.
Footnotes
For example, in the final four-way interaction equation examining depression, y = b0 + b1*x1 + b2*x2 + b3*x3 + b4*x4 + b5*x1x2 + b6*x1x3 + b7*x1x4 + b8*x2x3 + b9*x2x4 + b10*x3x4 + b11*x1x2x3 + b12*x1x2x4 + b13*x1x3x4 + b14*x2x3x4 + b15*x1x2x3x4, where x1 = 1 (high PBS Use) or −1 (low PBS Use); x2 = 1 (high depression) or (low depression); x3 = −1.14 (male) or .88 (female); and x4 = −.56 (White) or 1.79 (Asian).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Astin AW, Oseguera L, Sax LJ, Korn WS. The American freshman: Thirty-five year trends, 1966–2001. Los Angeles, CA: Higher Education Research Institute, University of California, Los Angeles; 2002. [Google Scholar]
- American College Health Association. American College Health Association-National College Health Assessment: Reference Group Data Report Spring 2008. Baltimore: American College Health Association; 2008. [Google Scholar]
- American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2011. Baltimore: American College Health Association; 2011. [Google Scholar]
- Araas TE, Adams TB. Protective behavioral strategies and negative alcohol-related consequences in college students. Journal of Drug Education. 2008;38(3):211–224. doi: 10.2190/DE.38.3.b. [DOI] [PubMed] [Google Scholar]
- Atkinson DR, Gim RH. Asian-American cultural identity and attitudes toward mental health services. Journal of Counseling Psychology. 1989;36(2):209–212. [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, Monti PM. Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors. 2007;32(11):2529–2548. doi: 10.1016/j.addbeh.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr V, Rando R, Krylowicz B, Winfield E. The Association for University and College Counseling Center Directors Annual Survey. 2010 Retrieved from Association for University & College Counseling Center Directors website: http://www.aucccd.org/img/pdfs/directors_survey_2009_m.pdf.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and clinical Psychology. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. The Psychological Corporation, Harcourt Brace & Company; San Antonio, TX: 1993. [Google Scholar]
- Benton SA, Robertson JM, Tseng WC, Newton FB, Benton SL. Changes in counseling center client problems across 13 years. Professional Psychology: Research and Practice. 2003;34(1):66–72. [Google Scholar]
- Benton SL, Schmidt JL, Newton FB, Shin K, Benton SA, Newton DW. College Student Protective Strategies and Drinking Consequences. Journal of Studies on Alcohol. 2004;65(1):115–121. doi: 10.15288/jsa.2004.65.115. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borden LA, Martens MP, McBride MA, Sheline KT, Bloch KK, Dude K. The role of college students’ use of protective behavioral strategies in the relation between binge drinking and alcohol-related problems. Psychology of Addictive Behaviors. 2011;25(2):346–351. doi: 10.1037/a0022678. [DOI] [PubMed] [Google Scholar]
- Camatta CD, Nagoshi CT. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcoholism: Clinical and Experimental Research. 1995;19(1):142–146. doi: 10.1111/j.1530-0277.1995.tb01482.x. [DOI] [PubMed] [Google Scholar]
- Chang J, Shrake E, Rhee S. Patterns of alcohol use and attitiudes toward drinking among Chinese and Korean American college students. Journal of Ethnicity and Substance Abuse. 2008;7(3):341–356. doi: 10.1080/15332640802313346. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/ correlational analysis for the behavioral science. 3. Mahwah, NJ: Routledge; 2002. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cook BJ, Cordova DI. Minorities in Higher Eduction: Twenty-Second Annual Status Report: 2007 Supplement. American Council on Education; 2007. Retrieved from http://www.acenet.edu/AM/Template.cfm?Section=CAREE&Template=/CM/ContentDisplay.cfm&ContentID=23716. [Google Scholar]
- Cooper ML, Agocha VB, Sheldon MS. A motivational perspective on risky behaviors: The role of personality and affect regulatory processes. Journal of Personality. 2000;68(6):1059–1088. doi: 10.1111/1467-6494.00126. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors. 2009;34(2):134–145. doi: 10.1016/j.addbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Boluijt P, Straten A. Screening of depression in adolescents through the Internet. European Child & Adolescent Psychiatry. 2008;17(1):32–38. doi: 10.1007/s00787-007-0631-2. [DOI] [PubMed] [Google Scholar]
- Dawson JF, Richter AW. Probing three-way interactions in moderated multiple regression: Development and application of a slope difference test. Journal of Applied Psychology. 2006;91(9):917–926. doi: 10.1037/0021-9010.91.4.917. [DOI] [PubMed] [Google Scholar]
- Delva J, Smith MP, Howell RL, Harrison DF, Wilke D, Jackson L. A Study of the Relationship Between Protective Behaviors and Drinking Consequences Among Undergraduate College Students. Journal of American College Health. 2004;53(1):19–26. doi: 10.3200/JACH.53.1.19-27. [DOI] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25(4):595–604. doi: 10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York, NY US: Guilford Press; 1999. [Google Scholar]
- D’Lima GM, Pearson MR, Kelley ML. Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in first-year college students. Psychology of Addictive Behaviors. 2012;26(2):330–337. doi: 10.1037/a0026942. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Chung H. Adequacy of depression treatment among college students in the United States. General Hospital Psychiatry. 2012 doi: 10.1016/j.genhosppsych.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77(4):534–542. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- Gallagher RP. National survey of counseling center directors. Alexandria, VA: International Association of Counseling Services; 2009. [Google Scholar]
- Geisner IM, Larimer ME, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29(5):843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Collins RL, Bradizza CM. Solitary and social heavy drinking, suicidal ideation, and drinking motives in underage college drinkers. Addictive Behaviors. 2009;34(12):993–999. doi: 10.1016/j.addbeh.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug & Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Griner D, Smith TB. Culturally adapted mental health interventions: a meta-analytic review. Psychotherapy Theory Research Practice Training. 2006;43:531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- Haines MP, Barker G, Rice RM. The personal protective behaviors of college student drinkers: Evidence of indigenous protective norms. Journal of American College Health. 2006;55(2):69–76. doi: 10.3200/JACH.55.2.69-76. [DOI] [PubMed] [Google Scholar]
- Ham LS, Hope DA. College students and problematic drinking: A review of the literature. Clinical Psychology Review. 2003;23(5):719–759. doi: 10.1016/s0272-7358(03)00071-0. [DOI] [PubMed] [Google Scholar]
- Harrell ZAT, Karim NM. Is gender relevant only for problem alcohol behaviors? An examination of correlates of alcohol use among college students. Addictive Behaviors. 2008;33(2):359–365. doi: 10.1016/j.addbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among US college students ages 18–24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18–24, 1998–2005. Journal of Studies on Alcohol and Drugs. 2009;(Supplement No. 16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard DE, Griffin MA, Boekeloo BO. Prevalence and psychosocial correlates of alcohol-related sexual assault among university students. Adolescence. 2008;43(172):733–750. [PMC free article] [PubMed] [Google Scholar]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health. 2010;46(1):3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Iwamoto D, Liu W, McCoy T. An exploratory model of substance use among Asian American women: The role of depression, coping, peer use and Asian values. Journal of Ethnicity in Substance Abuse. 2011;10(4):295–315. doi: 10.1080/15332640.2011.623494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto DK, Corbin W, Fromme K. Trajectory classes of heavy episodic drinking among Asian American college students. Addiction. 2010;105(11):1912–1920. doi: 10.1111/j.1360-0443.2010.03019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadison R, DiGeronimo TF. College of the Overwhelmed. San Francisco, CA: Jossey-Bass; 2004. [Google Scholar]
- Karwacki SB, Bradley JR. Coping, drinking motives, goal attainment expectancies and family models in relation to alcohol use among college students. Journal of Drug Education. 1996;26(3):243–255. doi: 10.2190/A1P0-J36H-TLMJ-0L32. [DOI] [PubMed] [Google Scholar]
- Kearney LK, Draper M, Barón A. Counseling utilization by ethnic minority college students. Cultural Diversity and Ethnic Minority Psychology. 2005;11(3):272–285. doi: 10.1037/1099-9809.11.3.272. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54(4):313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Knight JR, Wechsler H, Kuo M, Seibring M, Weitzman ER, Schuckit M. Alcohol abuse and dependence among U.S. college students. Journal of Studies on Alcohol. 2002;63(3):263–70. doi: 10.15288/jsa.2002.63.263. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. American Journal of Psychiatry. 1999;156(5):723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Labouvie EW, Bates ME. Reasons for alcohol use in young adulthood: Validation of three-dimensional measure. Journal of Studies on Alcohol. 2002;63:145–155. doi: 10.15288/jsa.2002.63.145. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Lac A, Kenney SR, Mirza T. Protective behavioral strategies mediate the effect of drinking motives on alcohol use among heavy drinking college students: Gender and race differences. Addictive Behaviors. 2010;36(4):354–361. doi: 10.1016/j.addbeh.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education. 2010;40(4):361–378. doi: 10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, Ferraiolo P. Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development. 2009;50(1):35–49. doi: 10.1353/csd.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, et al. Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2007;75(2):285–293. doi: 10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MY, Law FM, Eo E, Oliver E. Perception of substance use problems in Asian American Communities by Chinese, Indian, and Vietnamese American youth. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory, Research & Practice. 2002;11(3–4):159–189. doi: 10.1300/J051v11n03_02. [DOI] [Google Scholar]
- Litt DM, Lewis MA, Blayney JA, Kaysen DL. Protective behavioral strategies as a mediator of the generalized anxiety and alcohol use relationship among lesbian and bisexual women. Journal of Studies on Alcohol and Drugs. 2013;74:168–174. doi: 10.15288/jsad.2013.74.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu ZP, Engs RC, Hanson DJ. The drinking behaviors of a sample of university students in Nanning, Guangxi Province, People’s Republic of China. Substance Use & Misuse. 1997;32:495–506. doi: 10.3109/10826089709039368. [DOI] [PubMed] [Google Scholar]
- Luczak SE, Shea SH, Hsueh AC, Chang J, Carr LG, Wall TL. ALDH2*2 is associated with a decreased likelihood of alcohol-induced blackouts in Asian American college students. Journal of Studies on Alcohol. 2006;67(3):349–353. doi: 10.15288/jsa.2006.67.349. [DOI] [PubMed] [Google Scholar]
- Lum C, Corliss HL, Mays VM, Cochran SD, Lui CK. Differences in the drinking behaviors of Chinese, Filipino, Korean, and Vietnamese College Students. Journal of Studies on Alcohol and Drugs. 2009;70:568–574. doi: 10.15288/jsad.2009.70.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luczak SE, Wall TL, Shea SH, Byun SM, Carr, Lucinda G. Binge drinking in Chinese, Korean, and White college students: Genetic and ethnic group differences. Psychology of Addictive Behaviors. 2001 Dec;15(4):306–309. doi: 10.1037/0893-164X.15.4.306. [DOI] [PubMed] [Google Scholar]
- Lyvers M, Thorberg FA, Ellul A, Turner J, Bahr M. Negative mood regulation expectancies, frontal lobe related behaviors and alcohol use. Personality and Individual Differences. 2010;48(3):332–337. [Google Scholar]
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical and Experimental Research. 1995;19(6):1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Cimini MD. Do protective behavioral strategies mediate the relationship between drinking motives and alcohol use in college students. Journal of Studies on Alcohol and Drugs. 2007;68(1):106–114. doi: 10.15288/jsad.2007.68.106. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Korbett K, Anderson DA, Simmons A. Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol. 2005;66(5):698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, Cimini MD. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55(4):535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Littlefield AK, Murphy JG, Cimini MD. Changes in protective behavioral strategies and alcohol use among college students. Drug and Alcohol Dependence. 2011;118(2–3):504–507. doi: 10.1016/j.drugalcdep.2011.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Pederson ER, LaBrie JW, Ferrier AG, Cimini MD. Measuring alcohol-related protective behavioral strategies among college students: Further examination of the Protective Behavioral Strategies Scale. Psychology of Addictive Behaviors. 2007;21(3):307–315. doi: 10.1037/0893-164X.21.3.307. [DOI] [PubMed] [Google Scholar]
- Martens MP, Taylor KK, Damann KM, Page JC, Mowry ES, Cimini MD. Protective behavioral strategies when drinking alcohol and their relationship to negative alcohol-related consequences in college students. Psychology of Addictive Behaviors. 2004;18(4):390–393. doi: 10.1037/0893-164X.18.4.390. [DOI] [PubMed] [Google Scholar]
- Miller B, Miller M, Verhegge R, Linville H, Pumariega A. Alcohol misuse among college athletes: Self-medication for psychiatric symptoms? Journal of Drug Education. 2002;32(1):41–52. doi: 10.2190/JDFM-AVAK-G9FV-0MYY. [DOI] [PubMed] [Google Scholar]
- Miller MJ, Yang M, Hui K, Choi NY, Lim RH. Acculturation, enculturation, and Asian American college students’ mental health and attitudes toward seeking professional psychological help. Journal of Counseling Psychology. 2011;58(3):346–357. doi: 10.1037/a0023636. [DOI] [PubMed] [Google Scholar]
- Nguyen N, Walters ST, Wyatt TM, DeJong W. Use and correlates of protective drinking behaviors during the transition to college: Analysis of a national sample. Addictive Behaviors. 2011;36:1008–1014. doi: 10.1016/j.addbeh.2011.06.002. [DOI] [PubMed] [Google Scholar]
- Okazaki S. Sources of ethnic differences between Asian American and White American college students on measures of depression and social anxiety. Journal of Abnormal Psychology. 1997;106(1):52–60. doi: 10.1037/0021-843x.106.1.52. [DOI] [PubMed] [Google Scholar]
- Okazaki S. Treatment delay among Asian-American patients with severe mental illness. American Journal of Orthopsychiatry. 2000;70:58–64. doi: 10.1037/h0087751. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Charney DS, Lewis L, Cornish JW, Post RM, Woody GE, Bowden CL. Priority actions to improve the care of persons with co-occurring substance abuse and other mental disorders: a call to action. Biological Psychiatry. 2004;56:703–713. doi: 10.1016/j.biopsych.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Pace TM, Trapp MdC. A psychometric comparison of the Beck Depression Inventory and the Inventory for Diagnosing Depression in a college population. Assessment. 1995;2(2):167–172. [Google Scholar]
- Park CL, Grant C. Determinants of positive and negative consequences of alcohol consumption in college students: Alcohol use, gender, and psychological characteristics. Addictive Behaviors. 2005;30(4):755–765. doi: 10.1016/j.addbeh.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Park CL, Armeli S, Tennen H. The daily stress and coping process and alcohol use among college students. Journal of Studies on Alcohol. 2004;65(1):126–135. doi: 10.15288/jsa.2004.65.126. [DOI] [PubMed] [Google Scholar]
- Parks KA, Fals-Stewart W. The temporal relationship between college women’s alcohol consumption and victimization experiences. Alcoholism: Clinical and Experimental Research. 2004;28(4):625–629. doi: 10.1097/01.alc.0000122105.56109.70. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Lee CM, Larimer ME. Drinking motives, protective behavioral strategies, and experienced consequences: Identifying students at risk. Addictive Behaviors. 2011;36:270–273. doi: 10.1016/j.addbeh.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Farabaugh AH, Zisook S, Tucker D, Rooney K, Katz J, Fava M. Gender, depressive symptoms and patterns of alcohol use among college students. Psychopathology. 2011;44(1):27–33. doi: 10.1159/000315358. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Ruzek NA, Nguyen DQ, Herzog DC. Acculturation, enculturation, psychological distress and help-seeking preferences among Asian American college students. Asian American Journal of Psychology. 2011;2(3):181–196. doi: 10.1037/a0024302. [DOI] [Google Scholar]
- Santor DA, Zuroff DC, Ramsay JO, Cervantes P, Palacios J. Examining scale discriminability in the BDI and CES-D as a function of depressive severity. Psychological Assessment. 1995;7(2):131–139. doi: 10.1037/1040-3590.7.2.131. [DOI] [Google Scholar]
- Silverman MM. College student suicide prevention: Background and blueprint for action. Student Health Spectrum. 2004:13–20. [Google Scholar]
- Simons JS, Gaher RM, Correia CJ, Hansen CL, Christopher MS. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19(3):326. doi: 10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- So DW, Wong FY. Alcohol, drugs, and substance use among Asian-American college students. Journal of Psychoactive Drugs. 2006;38(1):35–42. doi: 10.1080/02791072.2006.10399826. [DOI] [PubMed] [Google Scholar]
- Sue S, Fujino DC, Hu L, Takeuchi DT, Zane NWS. Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology; Journal of Consulting and Clinical Psychology. 1991;59(4):533–540. doi: 10.1037//0022-006x.59.4.533. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Education, National Center for Education Statistics. Digest of Education Statistics, 2010. 2011 Retrieved from: http://nces.ed.gov/programs/digest/d10/ch_3.asp.
- Wall TL, Ehlers CL. Genetic influences affecting alcohol use among Asians. Alcohol Health & Research World. 1995;19(3):184–189. Retrieved from http://www.niaaa.nih.gov/Publications/AlcoholResearch/ [PMC free article] [PubMed] [Google Scholar]
- Wall TL, Shea SH, Chan KK, Carr LG. A genetic association with the development of alcohol and other substance use behavior in Asian Americans. Journal of Abnormal Psychology. 2001;110(1):173–178. doi: 10.1037/0021-843x.110.1.173. [DOI] [PubMed] [Google Scholar]
- Walters ST, Roudsari BS, Vader AM, Harris TR. Correlates of protective behavior utilization among heavy-drinking college students. Addictive Behaviors. 2007;32(11):2633–2644. doi: 10.1016/j.addbeh.2007.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Maenner G, Gledhill-Hoyt J, Lee H. Changes in binge drinking and related problems among American college students between 1993 and 1997. Journal of American College Health. 1998;47(2):57–68. doi: 10.1080/07448489809595621. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts: Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American college health. 2002;50(5):203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol & Drugs. 2008;69(4):481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192(4):269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50(1):30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Yang LH, Phelan JC, Link BG. Stigma and beliefs of efficacy towards traditional Chinese medicine and western psychiatric treatment among Chinese-Americans. Cultural Diversity and Ethnic Minority Psychology. 2008;14(1):10–18. doi: 10.1037/1099-9809.14.1.10. [DOI] [PubMed] [Google Scholar]
- Zane NWS, Huh-Kim J. Addictive behaviors. In: Lee LC, Zane NWS, editors. Handbook of Asian American Psychology. Thousand Oaks, CA: Sage; 1998. pp. 527–554. [Google Scholar]
- Zane N, Yeh M. The use of culturally-based variables in assessment: Studies on loss of face. In: Kurasaki KS, Sue S, editors. Asian American mental health: Assessment, methods and theories. New York, NY: Kluwer; 2002. pp. 123–138. [Google Scholar]