Eosinophilic gastrointestinal disorders (EGIDs) are being recognized with an increasing frequency. They are characterized by prominent eosinophilic infiltration in the absence of parasitic infection, vasculitis, neoplasm, or other known causes of eosinophilia.1,2 They are routinely classified according to anatomic location or depth of inflammation and can have a variety of presentations and symptoms.3,4 We report an unusual case of eosinophilic gastroenteritis (EG) in a middle-aged woman who presented with severe dysphagia and associated weight loss.
Case Report
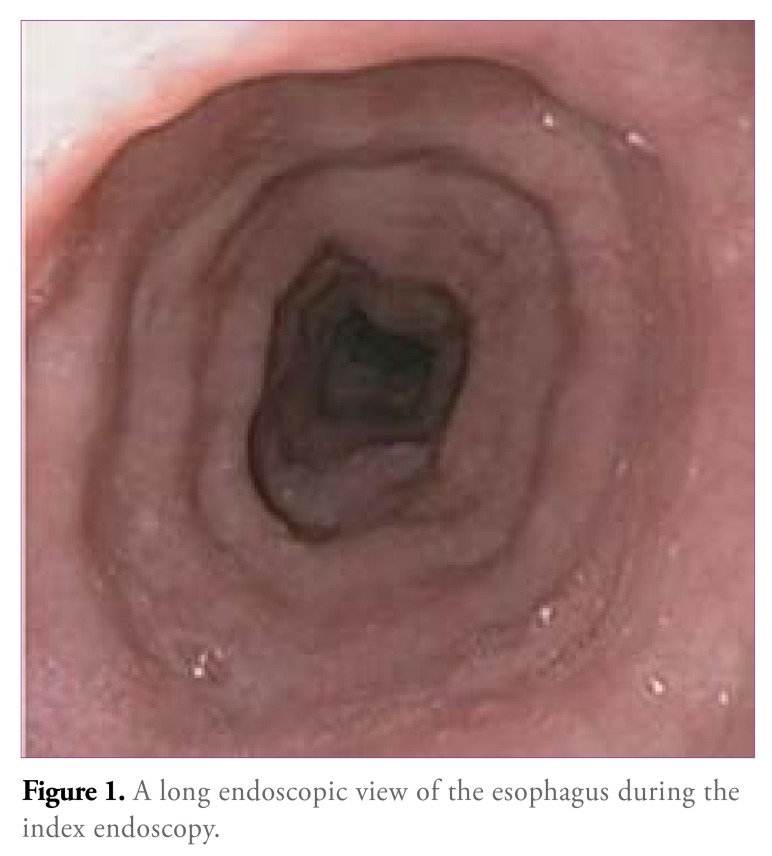
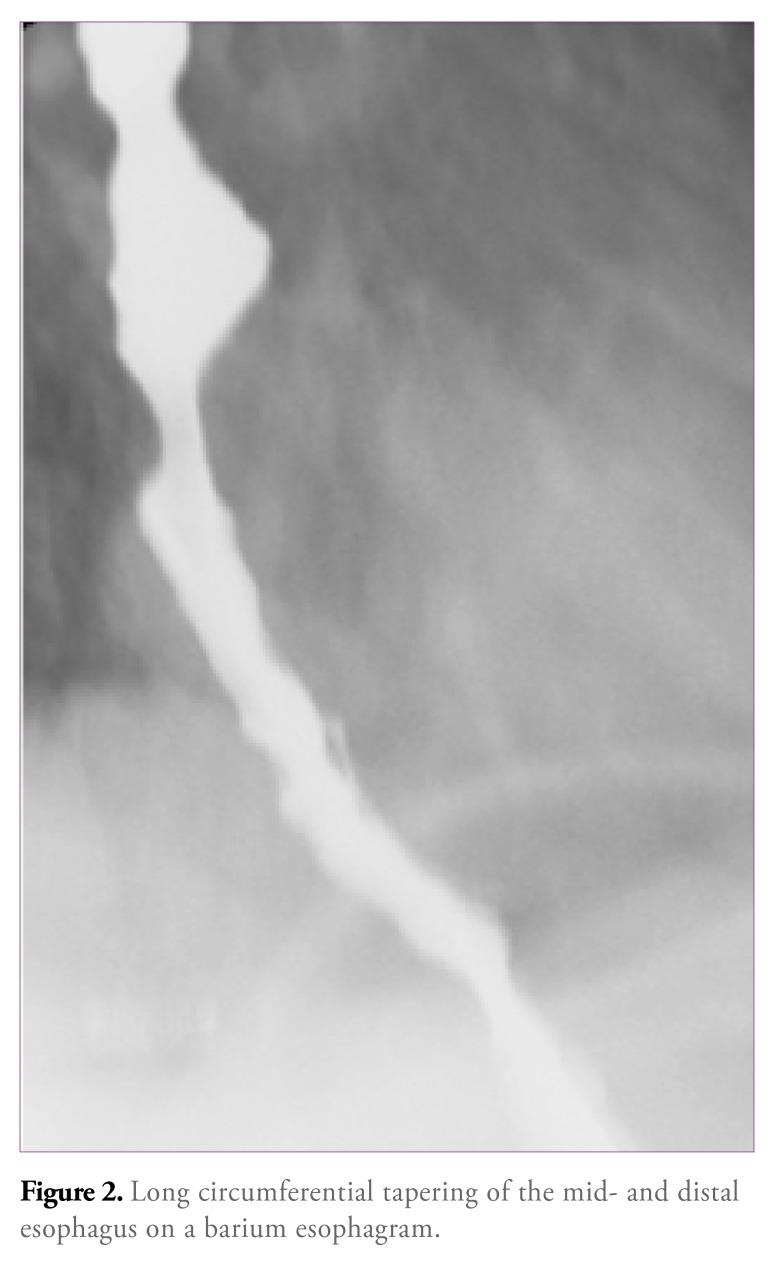
A previously healthy Haitian woman, age 50 years, was referred for symptoms of severe dysphagia to solids and liquids and a 15-lb weight loss over 4 weeks. Her medical history was significant for childhood asthma. She had no other relevant personal or medication history. Findings of an initial endoscopy performed by a community physician suggested extrinsic esophageal obstruction but were ultimately nondiagnostic. At our hospital, we repeated the endoscopic examination (Figure 1) and found a distensible lumen without any specific segmental stricture, although there was an impression that the overall caliber of the esophagus was narrowed. This finding was supported by results of a barium esophagram (Figure 2). Biopsies of the midesophagus revealed only occasional eosinophils (1 to 2 eosinophils per high-power field [eos/HPF]).
Figure 1.
A long endoscopic view of the esophagus during the index endoscopy.
Figure 2.
Long circumferential tapering of the mid- and distal esophagus on a barium esophagram.
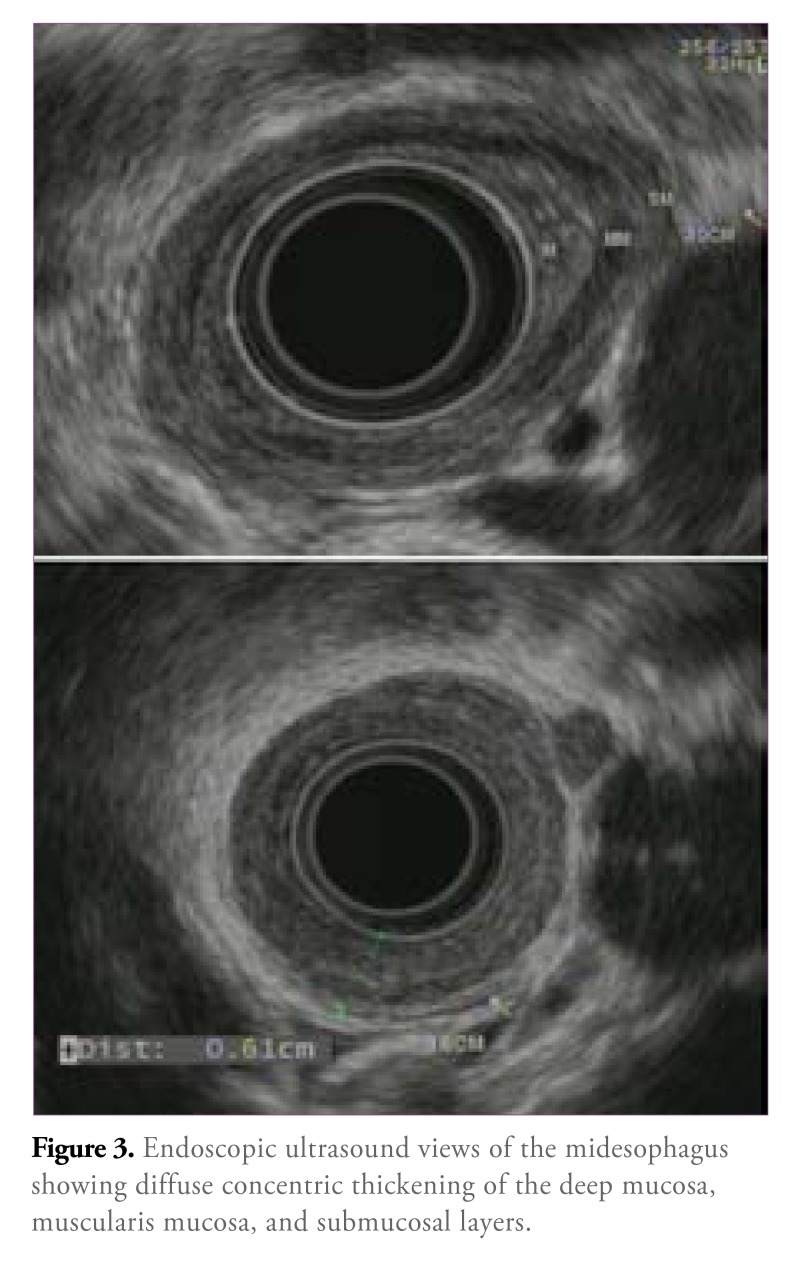
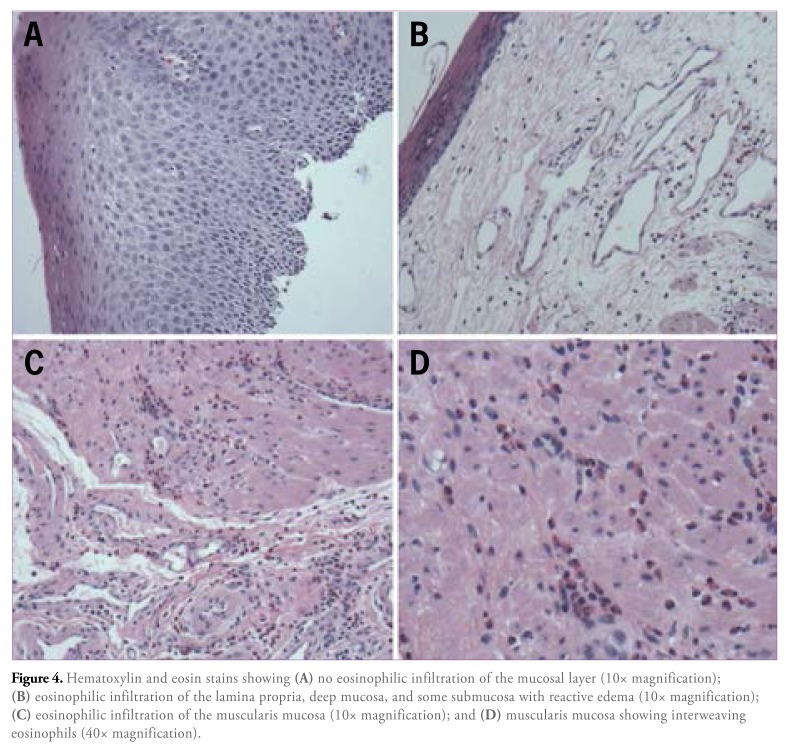
We also performed an endoscopic ultrasound (EUS), which revealed a diffuse thickening of the mucosal and submucosal layers throughout the entire esophagus without evidence of extraluminal compression or lymphadenopathy (Figure 3). To exclude a diffusely infiltrating process, we performed an endoscopic mucosal resection (EMR) using a band ligation and snare technique. Histologic analysis revealed greater than 60 eos/HPF limited to the deep mucosa, muscularis mucosa, and parts of the submucosal layer (Figure 4). Significant edema and some eosinophils dissecting the muscle layers were found. The epithelial layer, however, was devoid of any significant eosinophilia. No other types of inflammatory cells were present, and there was no evidence of malignancy. The pattern of inflamma-tion was consistent with what has been described in EG when it extends to the esophagus.
Figure 3.
Endoscopic ultrasound views of the midesophagus showing diffuse concentric thickening of the deep mucosa, muscularis mucosa, and submucosal layers.
Figure 4.
Hematoxylin and eosin stains showing (A) no eosinophilic infiltration of the mucosal layer (10x magnification); eosinophilic infiltration of the lamina propria, deep mucosa, and some submucosa with reactive edema (10x magnification); eosinophilic infiltration of the muscularis mucosa (10x magnification); and (D) muscularis mucosa showing interweaving eosinophils (40x magnification).
Subsequently, we performed an EMR of the patient’s stomach and obtained deep biopsies of the duodenum, which did not identify eosinophilia. Tests for parasites, autoimmune disorders, and HIV infection were all negative. Given the severity of the patient’s symptoms, a course of twice-daily prednisone was initiated. In addition, serum allergy testing was performed for food and environmental allergens, which did not identify any specific allergic trigger. The patient’s oral intake of solids and liquids improved within 48 hours, and follow-up at 2, 4, and 6 weeks suggested that the patient’s symptoms had completely resolved with an associated return to baseline weight. A repeat EUS performed at 8 weeks showed a marked improvement in the thickness of the mucosal and submucosal layers (Figure 5). Given the patient’s symptomatic resolution and evidence of improvement via EUS, therapy was discontinued at 8 weeks, and the patient has continued to do well.
Figure 5.
An endoscopic ultrasound view of the midesophagus showing decreased thickening of the deep mucosal and submucosal layers after treatment.
Discussion
Eosinophilic esophagitis (EoE) is the most commonly recognized form of EGIDs, with a prevalence of 5 per 10,000 persons.5,6 Other EGIDs, such as EG and eosinophilic colitis, are far less common, with an unknown prevalence.7 As opposed to EoE, these disorders vary significantly in the extent and depth of gastrointestinal involvement, resulting in a wide range of symptoms.3 Despite this spectrum in presentation, all EGIDs share eosinophilic infiltration as a common feature, perhaps implicating an allergic mechanism. A strong personal or family history of allergy can be found in more than 50% of patients.4 In addition, genetic factors have been implicated, with case reports of similar disease processes in monozygotic twins,8 but, overall, there is a lack of firm evidence to support a hereditary component.
EG, specifically, can involve 1 or more segments from the esophagus to the rectum. In 1970, Klein and colleagues arbitrarily classified patients according to the depth of involvement (ie, those with predominantly mucosal, muscular, or serosal disease).1-4,9 Since its first description in 1937, less than 300 cases of EG have been reported, most of which have been single case reports or small case series.7,8,10,11 EG is most commonly reported in the small bowel, particularly the second portion of the duodenum. Rarely, it has been described in the esophagus as part of a larger systemic disorder.3,4 Patients typically present in the third through fifth decades of life, but the disease can affect any age group and probably has an equal gender distribution.4 Symptoms are directly related to the extent of the gastrointestinal involvement. Patients with predominantly mucosal disease have symptoms of diarrhea, malabsorption, and abdominal pain, whereas those with muscular involvement present more commonly with bowel thickening and symptoms of pyloric or intestinal obstruction. When the disease extends to the serosal layer, ascitic fluid accumulation can occur.4,10
Our patient presented with symptoms of esophageal obstruction secondary to severe eosinophilic infiltration with reactive edema. Although manometry was not performed in our case, dysmotility is a common finding,6 which was evident in the narrow caliber and spasmodic appearance of the patient’s esophagus during the esopha-gram (Figure 2). Although the patient’s symptoms were directly related to esophageal eosinophilia, her disease is distinct from the more commonly encountered EoE, particularly because there was preferential infiltration of eosinophils in the deep mucosal and submucosal layers of the esophagus. In adults, EoE is entirely mucosal, resulting in an epithelial surface layering of eosinophils. Occasionally, deeper layers can be affected but to a lesser extent than the epithelium, setting it apart from mucosal EG, which involves multiple layers equally. In this case, the epithelium showed no eosinophilia (Figure 4A), supporting our diagnosis of EG rather than EoE. It is also notable that the 2 disorders can occur in the same individual as distinct processes, albeit not concurrently.11
For EGIDs, the main therapeutic options include oral or topical corticosteroids, montelukast, sodium cromogly-cate, and restrictive diets. For EG, the results of each of these therapies are variable; however, it is clear that cortico-steroids are associated with faster resolution of symptoms.3 Our patient had complete symptomatic resolution within 8 weeks on a tapered corticosteroid regimen. Serum allergy testing did not identify a particular food trigger that could be avoided, and for most patients, long-term avoidance of foods can be impractical. A repeat EUS confirmed an improvement in the mucosal and submucosal edema associated with symptom resolution. Our diagnostic approach to this patient, overall, has been unique, incorporating a combination of EUS and EMR for diagnosis and follow-up. This highlights the diagnostic challenge for this disease and the limitation of traditional biopsies, which only sample small sections of the superficial mucosa.
To our knowledge, isolated eosinophilic infiltration of the esophagus, in a pattern consistent with EG, has never been described in the literature. Previously, a handful of reports have described esophageal involvement in extensive EG of the upper gastrointestinal tract.4 In these cases, esophageal involvement occurs later in the disease process and can be a marker of severity. Our case is unique in that there was no evidence of involvement apart from the esophagus. This case may represent a variant in the spectrum of EGIDs or an early form of esophageal EG with the potential to progress to involvement at other sites. In most cases, the diagnosis can be quite difficult to establish, and treatment often must be empiric. The ability to use multiple imaging modalities, as well as techniques for tissue sampling, helped identify the patient’s condition early, and prompt treatment resulted in complete resolution of symptoms.
Summary
EG is an uncommon entity characterized by heavy eosinophilic infiltration of the gastrointestinal tract wall. Its symptoms can range from nonspecific abdominal pain to luminal obstruction. It can affect a single segment, but it more commonly affects multiple segments and causes an array of symptoms. Esophageal involvement rarely occurs, and isolated esophageal EG, as with our patient, has never been reported in the literature. EG is histologically distinct from the more common EoE, and, perhaps, the triggers and mechanisms of inflammation also may differ. Our approach to this case highlights the current diagnostic- and treatment-related obstacles regarding this disorder and emphasizes the importance of multimodality imaging and sampling techniques that are not routinely employed.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Yan BM, Shaffer EA. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58(5):721–732. doi: 10.1136/gut.2008.165894. [DOI] [PubMed] [Google Scholar]
- 2.de Chambrun GP, Gonzalez F, Canva JY, et al. Natural history of eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. 2011;9(11):950–956.e1. doi: 10.1016/j.cgh.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Lee J, Dierkhising R, Wu TT, Alexander J, Weiler C. Eosinophilic gastrointestinal disorders (EGID) with peripheral eosinophilia: a retrospective review at Mayo Clinic. Dig Dis Sci. 2011;56(11):3254–3261. doi: 10.1007/s10620-011-1754-3. [DOI] [PubMed] [Google Scholar]
- 4.Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer and subserosal tissues. Gut. 1990;31(1):54–58. doi: 10.1136/gut.31.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins MH. Histopathologic features of eosinophilic esophagitis. Gastrointest Endosc Clin N Am. 2008;18(1):59–71. doi: 10.1016/j.giec.2007.09.014. viii-ix. [DOI] [PubMed] [Google Scholar]
- 6.Furuta GT. Eosinophilic esophagitis: update on clinicopathological manifestations and pathophysiology. Curr Opin Gastroenterol. 2011;27(4):383–388. doi: 10.1097/MOG.0b013e328347bb10. [DOI] [PubMed] [Google Scholar]
- 7.Zhang L, Duan L, Ding S, et al. Eosinophilic gastroenteritis: clinical manifestations and morphological characteristics, a retrospective study of 42 patients. Scand J Gastroenterol. 2011;46(9):1074–1080. doi: 10.3109/00365521.2011.579998. [DOI] [PubMed] [Google Scholar]
- 8.Aquino A, Dòmini M, Rossi C, D’Incecco C, Fakhro A, Lelli Chiesa P. Pyloric stenosis due to eosinophilic gastroenteritis: presentation of two cases in mono-ovular twins. Eur J Pediatr. 1999;158(2):172–173. doi: 10.1007/s004310051045. [DOI] [PubMed] [Google Scholar]
- 9.Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49(4):299–319. doi: 10.1097/00005792-197007000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Lim KC, Tan HK, Rajnakova A, Venkatesh SK. Eosinophilic gastroenteritis presenting with duodenal obstruction and ascites. Ann Acad Med Singapore. 2011;40(8):379–381. [PubMed] [Google Scholar]
- 11.Le-Carlson M, Triadafilopoulos G, Pai RK, Kerner JA. An evolving case of concurrent eosinophilic esophagitis and eosinophilic gastroenteritis. Dig Dis Sci. 2012;57(4):842–844. doi: 10.1007/s10620-012-2061-3. [DOI] [PubMed] [Google Scholar]