Abstract
Background
The purpose of this study is to report the safety and efficacy of a new application of collagen cross-linking using a novel device to achieve predictable refractive myopic changes in virgin corneas.
Methods
Four cases were treated with a novel device employing very high-fluence collagen cross-linking applied in a myopic pattern. Prior to treatment, riboflavin solution was applied to the intact epithelium. The collagen cross-linking device was then engaged for a total of 12 J/cm2, to be applied transepithelially in a predetermined pattern. Cornea clarity, corneal keratometry, and corneal topography were evaluated by both Placido disc and Scheimpflug imaging, along with cornea anterior segment optical coherence tomography and endothelial cell counts.
Results
An average of 2.3 diopters was achieved in the first week in all four cases treated with the very high-fluence myopic collagen cross-linking intervention. There was a slight regression to 1.44 diopters at 1 month, which remained stable at 6-month follow-up. The mean keratometry change was from 44.90 diopters to 43.46 diopters. There was no significant change in endothelial cell counts or corneal clarity. There was some mild change in epithelial thickness distribution, with the treated area showing a slight but homogeneous reduction in mean thickness from 52 μm to 44 μm.
Conclusion
This report describes the novel application of very high-fluence collagen cross-linking with a predictable well defined myopic refractive (flattening) corneal effect. This technique has the advantages of essentially no postoperative morbidity, immediate visual rehabilitation, and the potential for tapering until the desired result is achieved.
Keywords: myopia, refractive correction, high-fluence collagen cross-linking, clinical results
Video abstract
Introduction
Collagen cross-linking has been used for many years as a means of stabilizing cornea ectasia.1–5 Although a multitude of treatments and techniques are available, it has been well documented that the procedure almost invariably results in some central anterior corneal flattening,1–5 which has often been interpreted as “disease regression.” As our understanding and the technology available for collagen cross-linking has progressed, it has been theorized that differential application of collagen cross-linking in specific areas of the cornea may produce predictable refractive changes. Several aspects of this theory need further investigation. Is it possible to achieve predictable refractive changes? Can this be achieved through an intact epithelium? Can the human cornea tolerate higher fluence of ultraviolet light? This paper describes the use of a novel device employing very high-fluence collagen cross-linking, applied with a customizable pattern, in order to achieve myopic refractive changes.
Materials and methods
The study included four partially sighted volunteers with vision less than 20/400 (count fingers and worse), due to end-stage wet age-related macular degeneration, myopic refraction from −3 to −6 diopters, and astigmatism from −0.25 to −2.5 diopters. None had previously undergone cornea surgery. All patients signed informed consent forms, and the study received approval from the ethics committee. All eyes were imaged using Placido disc corneal topography (Vario Topolyzer; Oculus, Wetzlar, Germany), Scheimpflug topography (Pentacam®; Oculus), autorefraction and keratometry (Speedy-K®; Nikon, Tokyo, Japan), and anterior segment imaging and mapping by spectral domain anterior segment optical coherence tomography (RtVue-100; Optovue, Irvine, CA, USA). Given that manifest refractions are extremely challenging in these cases, only autorefraction data are reported. Corneal endothelial cell counts were evaluated by confocal microscopy (Robo K; Konan Medical Inc., Hyogo, Japan).
Surgical technique
A “myopic” treatment plan was designed to employ a 4 mm diameter ultraviolet A application that would deliver 30 mW/cm2 of surface fluence on the pupillary aperture by the KXL II device (Avedro Inc., Waltham, MA, USA) for a total exposure time of 4 minutes (12.4 J/cm2 of total energy). The surgical technique involved positioning an eyelid speculum in a sterile environment after the eyelids had been swabbed with 5% povidone iodine solution and draped with Tegaderm™ (3M, Neuss, Germany). A series of drops of ParaCel™ (Avedro Inc.), a specially formulated mildly abrasive 0.25% riboflavin solution, was applied every 30 seconds for 4 minutes, followed immediately by VibeX Xtra™ (Avedro Inc.), a 0.25% riboflavin solution and normal saline. The latter was applied again every 30 seconds for 6 minutes, so total riboflavin application took 10 minutes. The KXL II device was then placed immediately over the eye, which was kept open by the lid speculum. Following appropriate alignment and focusing by the surgeon, the pupillary aperture of each eye being treated was captured and tracked using the KXL II device. Application of ultraviolet A was directed at the 4 mm diameter area centered at the apex of the cornea.
The cornea was moistened once every minute with a drop of balanced salt solution. After completion of collagen cross-linking, the eyelid speculum was removed and treatment was started with a combination of antibiotic (Dispersadron-C®; Alcon, Fort Worth, TX, USA) and corticosteroid (Vigamox®; Alcon) eye drops for 10 days.
All patients were examined on the first day, after the first week, and monthly thereafter for 6 months. Visual acuity assessment, Placido disc topography, Scheimpflug imaging, and anterior segment optical coherence tomography were performed at each visit, along with an endothelial cell count and autorefraction keratometry.
Results
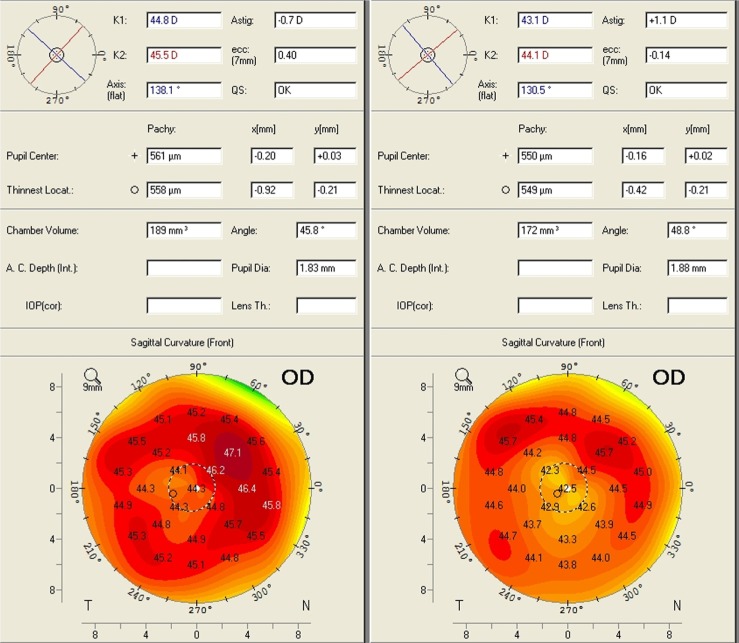
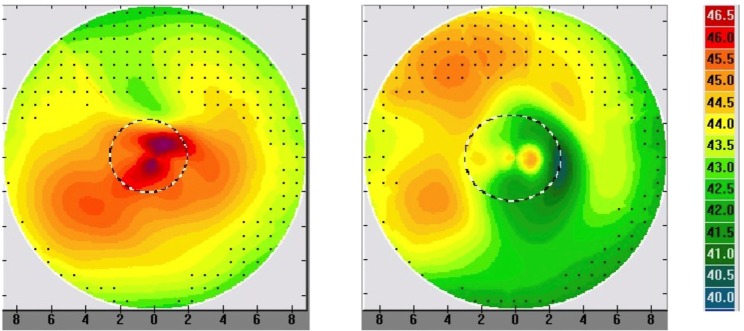
The data for preoperative and postoperative keratometry, flattening at 1 week and 6 months, corneal endothelial cell counts, and subject age are summarized in Table 1. All eyes showed significant, predictable, and very regular flattening over the central cornea. After the first week, a mean flattening of 2.3 diopters was documented by keratometry, Placido disc topography (Figure 1), and Scheimpflug tomography (Figure 2). By 1 month, flattening had regressed to a mean of 1.44 diopters. These values remained stable through to follow-up at 6 months, establishing stability of the effect.
Table 1.
Preoperative and postoperative keratometry, flattening at 1 week, and keratometric flattening results at 6 months along with corneal endothelial cell counts and age of each subject
| PreK1 (D) |
PreK2 (D) |
PostK1 (D) |
PostK2 (D) |
1 w flat (D) |
6 m flat (D) |
Pre-ECC (counts/mm2) |
Post-ECC (counts/mm2) |
Age (years) |
|
|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 44.50 | 44.75 | 42.75 | 43.50 | 2.25 | 1.45 | 1,800 | 1,800 | 72 |
| Patient 2 | 44.25 | 45.50 | 42.75 | 44.50 | 1.75 | 1.25 | 1,500 | 1,500 | 68 |
| Patient 3 | 44.80 | 45.50 | 43.10 | 44.10 | 2.10 | 1.55 | 1,650 | 1,650 | 71 |
| Patient 4 | 44.50 | 45.50 | 43.25 | 43.75 | 1.90 | 1.50 | 1,450 | 1,550 | 73 |
| Mean | 44.50 | 45.30 | 42.96 | 43.96 | 2.30 | 1.44 | 1,600 | 1,625 | 71.25 |
Abbreviations: D, diopters; PreK1, flattest preoperative keratometry meridian value; PreK2, steepest preoperative keratometry meridian value; PostK1, flattest postoperative keratometry meridian value at 6 months; PostK2, steepest postoperative keratometry meridian value at 6 months; 1 w flat, mean keratometric flattening noted at 1 week; 6 m flat, mean keratometric flattening noted at 6 months; Pre-ECC, preoperative endothelial cell count (cells/mm2); Post-ECC, postoperative endothelial cell count (cells/mm2); age, age of each patient studied at the start of the trial.
Figure 1.
Placido disc topography for patient 3 preoperatively (left) and 6 months postoperatively (right) depicting the significant and regular central corneal flattening effect.
Figure 2.
Scheimpflug imaging data for patient 3 preoperatively (left) and 6 months postoperatively (right) depicting the significant and regular central corneal flattening effect.
Abbreviations: D, diopters; OD, right eye.
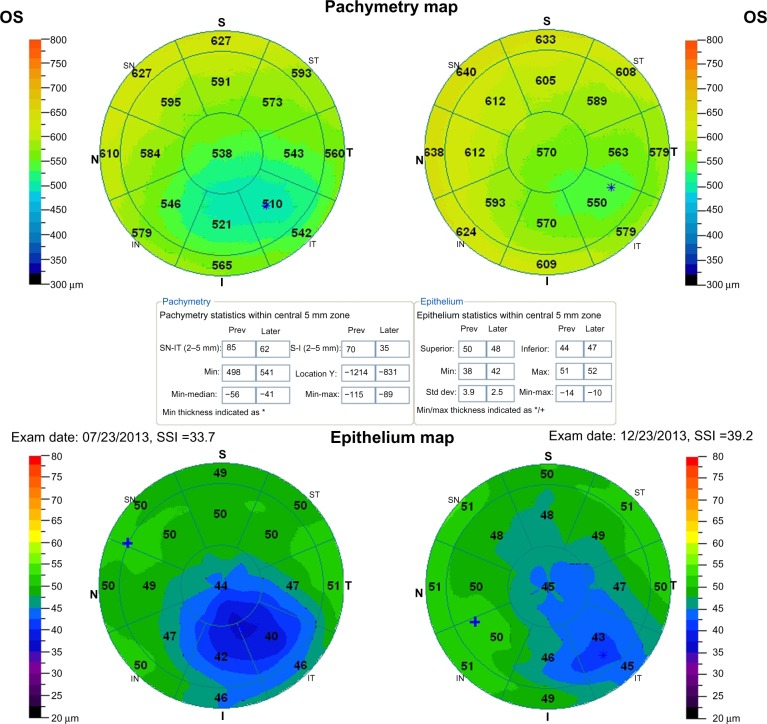
Anterior segment optical coherence tomography imaging showed mild epithelial changes, with the treated area showing a slight but homogeneous reduction in mean epithelial thickness over the treated area (Figure 3). The average epithelial thickness was 49 μm preoperatively, which decreased to 44 μm at 1 month postoperatively, and then increased to 48 μm at 5 months postoperatively.
Figure 3.
Anterior segment optical coherence tomography derived preoperatively and 5 months postoperatively showing corneal thickness and epithelial maps of the central 6 mm of the cornea in patient 3 (all units in microns [um]).
Discussion
A multitude of reports have established the significant refractive changes that accompany classic collagen cross-linking1–8 utilizing the classic Dresden protocol (3 mW/cm2 for 30 minutes), as well as collagen cross-linking utilizing higher fluence,9 and even cross-linking delivered in eyes that have had riboflavin placed within a femtosecond laser-created pocket or intrastromal corneal ring segment channels.10,11 Over the years, most clinicians have referred to this process as “flattening,” which has often been interpreted as “disease regression.” We have long theorized that this flattening is a refractive effect resulting from differential cross-linking between different segments of the cornea, resulting in a dissimilar stiffening effect, which macroscopically is interpreted as a refractive change. Our group has reported previously on the use of higher-fluence collagen cross-linking as a prophylactic refractive stability modulator in both myopic and hyperopic laser-assisted in situ keratomileusis.12–14 We have also recently reported impressive refractive changes in astigmatic keratotomy when “flash” collagen cross-linking is applied just at the incision margins.15
With the research and development of an appropriate device done by the Avedro team and the ability to perform feasibility studies with the KXL II device, it appears that this promise holds true. In a population of elderly patients, we were able to achieve an impressively regular and predictable central cornea flattening effect, consistent with a correction of myopia of about 2.5 diopters.
Of note, the initial refractive effect was slightly greater, appeared to regress between the first week and the first month, then remained stable thereafter. No cornea clarity or endothelial cell changes (the noted difference of 25 cells/mm2 may well be attributed to instrumentation-measurement precision and centration accuracy) were noted in this study group, despite application of much higher energy than that used in the “standard” Dresden protocol.16
Although longer follow-up will be necessary to determine the long-term stability of the present data, these findings are compelling with regard to the correction of small myopic refractive errors of the cornea without incision or tissue removal in an excimer-like fashion or other previously described thermal techniques combined with collagen cross-linking.17
This novel procedure appears to be extremely simple for both patient and surgeon, and is essentially performed through intact epithelium. The interim epithelial remodeling in the first 6 months, when compared with normal eyes,18 appears to flatten slightly in a homogeneous way (average 8 microns). It appears to require extremely minor postoperative lifestyle adjustment on the part of the patient, and essentially no pain or discomfort occurs, even within the first few hours following the procedure. The topographic changes seen on Placido and Scheimpflug imaging as well as on anterior segment optical coherence tomography are compelling evidence of the specificity and topography-guided precision of the KXL II device. This application may have greater efficacy in younger corneas, given that the corneas studied here were from older patients and possibly less sensitive to collagen cross-linking. In patients with early keratoconus where stabilization and correction of myopic refractive error is desired, the potential advantages of this procedure would be another possible future application. These cases were specifically chosen for an initial feasibility study that would establish the safety and possible efficacy of this procedure. We introduce herein the clinical use of ultra high fluence transepithelial CXL for refractive corneal change. The dose-effect relationship of this treatment is currently under investigation. Minimal patient discomfort compared to laser refractive surgery makes this procedure a possible future alternative for lower refractive errors. Hyperopic and toric corrections are novel applications currently being investigated. The ease of this procedure and the essentially zero associated morbidity it offers may also allow the possibility of titrating the effect over two or more treatments. Hyperopic and toric corrections may be other novel applications that could be attempted using this technology.
Conclusion
This paper introduces a novel technique based on refractive collagen cross-linking on virgin corneas as an alternative refractive correction technique for mild myopia. In the follow-up time evaluated, these patients showed an impressive and stable reduction in their myopia. This pilot work may represent a landmark study of a potentially revolutionary new refractive procedure.
Acknowledgments
The novel concept of refractive CXL named PiXL was designed and implemented as concept and technology design by David Muller, PhD.
Footnotes
Disclosure
This work was presented in part at the International Society of Refractive Surgery subspecialty day, New Orleans, LA, USA, November 15–17, 2013. The author has no other conflicts of interest in this work.
References
- 1.Ghanem RC, Santhiago MR, Berti T, Netto MV, Ghanem VC. Topographic, corneal wavefront, and refractive outcomes 2 years after collagen cross-linking for progressive keratoconus. Cornea. 2014;33(1):43–48. doi: 10.1097/ICO.0b013e3182a9fbdf. [DOI] [PubMed] [Google Scholar]
- 2.Arora R, Jain P, Goyal JL, Gupta D. Comparative analysis of refractive and topographic changes in early and advanced keratoconic eyes undergoing corneal collagen cross-linking. Cornea. 2013 Aug 22; doi: 10.1097/ICO.0b013e3182a02ddb. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 3.Hassan Z, Szalai E, Módis L, Jr, Berta A, Németh G. Assessment of corneal topography indices after collagen cross-linking for keratoconus. Eur J Ophthalmol. 2013;23(5):635–640. doi: 10.5301/ejo.5000249. [DOI] [PubMed] [Google Scholar]
- 4.Touboul D, Trichet E, Binder PS, Praud D, Seguy C, Colin J. Comparison of front-surface corneal topography and Bowman membrane specular topography in keratoconus. J Cataract Refract Surg. 2012;38(6):1043–1049. doi: 10.1016/j.jcrs.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 5.Piñero DP, Alio JL, Klonowski P, Toffaha B. Vectorial astigmatic changes after corneal collagen cross-linking in keratoconic corneas previously treated with intracorneal ring segments: a preliminary study. Eur J Ophthalmol. 2012;22(Suppl 7):S69–S80. doi: 10.5301/ejo.5000063. [DOI] [PubMed] [Google Scholar]
- 6.Greenstein SA, Fry KL, Hersh PS. Corneal topography indices after corneal collagen cross-linking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37(7):1282–1290. doi: 10.1016/j.jcrs.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ. Post-LASIK ectasia. Ophthalmology. 2007;114(6):1230. doi: 10.1016/j.ophtha.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 8.Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen cross-linking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33(12):2035–2040. doi: 10.1016/j.jcrs.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 9.Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. doi: 10.2147/OPTH.S27170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser-created pocket: initial clinical results. J Refract Surg. 2009;25(11):1034–1037. doi: 10.3928/1081597X-20090901-02. [DOI] [PubMed] [Google Scholar]
- 11.Alió JL, Toffaha BT, Piñero DP, Klonowski P, Javaloy J. Cross-linking in progressive keratoconus using an epithelial debridement or intrastromal pocket technique after previous corneal ring segment implantation. J Refract Surg. 2011;27(10):737–743. doi: 10.3928/1081597X-20110705-01. [DOI] [PubMed] [Google Scholar]
- 12.Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen cross-linking and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013;61(8):430–432. doi: 10.4103/0301-4738.116074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanellopoulos AJ, Kahn J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012;28(Suppl 11):S837–S840. doi: 10.3928/1081597X-20121005-05. [DOI] [PubMed] [Google Scholar]
- 14.Kanellopoulos AJ. Long-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2012;6:1125–1130. doi: 10.2147/OPTH.S31256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanellopoulos AJ. Very high fluence collagen cross-linking as a refractive enhancement of a regressed previous astigmatic keratotomy. J Refract Surg. 2013;29(7):504–505. doi: 10.3928/1081597X-20130515-06. [DOI] [PubMed] [Google Scholar]
- 16.Wollensak G, Spörl E, Seiler T. Treatment of keratoconus by collagen cross linking. Ophthalmologe. 2003;100(1):44–49. doi: 10.1007/s00347-002-0700-3. German. [DOI] [PubMed] [Google Scholar]
- 17.Kanellopoulos AJ. Laboratory evaluation of selective in situ refractive cornea collagen shrinkage with continuous wave infrared laser combined with transepithelial collagen cross-linking: a novel refractive procedure. Clin Ophthalmol. 2012;6:645–652. doi: 10.2147/OPTH.S31250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanellopoulos AJ, Asimellis G. In vivo three-dimensional corneal epithelium imaging in normal eyes by anterior-segment optical coherence tomography: a clinical reference study. Cornea. 2013;32(11):1493–1498. doi: 10.1097/ICO.0b013e3182a15cee. [DOI] [PubMed] [Google Scholar]