Abstract
Purpose
The purpose of this study was to compare clinical outcomes of patients with full-thickness small to large sized tears undergoing all-arthroscopic versus mini-open rotator cuff repair.
Method
A literature search for electronic databases and references for eligible studies was conducted through Medline, Embase and Cochrane library between 1969 and 2013.
Results
A total of 12 comparative studies (n = 770 patients) were included. Pooled results showed: there were no differences in function outcome, pain scores, retear rate or the incidence of adhesive capsulitis between all arthroscopic and mini-open repair groups.
Conclusions
There were no differences in outcomes between the arthroscopic and mini-open rotator cuff repair techniques, they should be considered alternative treatment options.
Level of Evidence
Level IV, Meta analysis.
Introduction
Repair of the rotator cuff was first described nearly a century ago by Codman [1]. The most frequently used methods for rotator cuff repair include the open, mini-open, and arthroscopic techniques. Currently, there is a growing trend toward a more minimally invasive approach facilitated by advances in the use of arthroscopy [2]–[5]. Both the mini-open and all-arthroscopic techniques maintain the integrity of the deltoid origin with minimal incision. The arthroscopic approach offers several advantages, including a smaller incision, easy access to the glenohumeral joint for treatment of intra-articular pathology, less soft tissue dissection, and less potential harm to the deltoid. However, a purely arthroscopic rotator cuff repair requires advanced arthroscopic skills. One of the main advantages of the mini-open rotator cuff repair is deltoid preservation thereby eliminating the risk of postoperative deltoid dehiscence. Several systematic reviews [2]–[5], including one meta-analysis [5] have demonstrated that no significant differences existed in mid- and long-term clinical outcomes between arthroscopic and mini-open repair. However, all the five studies included in that meta-analysis by Morse published in 2008 were not randomized clinical trials (RCTs) and the follow-up was retrospective in nature. This meta-analysis involved 12 studies including 3 RCTs published in 2011, 2012, 2013 respectively comparing the results of both methods on the treatment for rotator cuff tears aimed at investigating whether there were any clinical and radiographic differences between these two methods.
Materials and Methods
Identification and Selection of Studies
We carried out a literature search using Medline, Embase and Cochrane databases to identify all articles published between 1969 and 2013 that evaluated the outcomes of patients undertaking either AA (all atthroscopic repair) or MO (mini open repair). The language of the publications was limited in English. Comparative reports relating to both AA and MO were included. The following Medical Subject Headings (MeSH) and terms were used in searching: “rotator cuff tear”, “supraspinatus tendon”, “arthroscopic”, “arthroscopy”, “mini open” and “clinical trials”. The reference lists of each comparative study and previous reviews were manually examined to find additional relevant studies. We also contacted each author of the included studies to identify some more details of the clinical outcomes and further studies on the same topic by e-mail. To minimize any possible selection bias, criteria for inclusion were as follows: English reported papers; a clinical trial comparing AA and MO with a clear description of at least one of the indexes analyzed in this study. Two reviewers independently assessed each of the studies for eligibility for inclusion. Firstly, the title and the abstract were judged by either reviewer and then if it was potentially eligible, the full article would be examined. All disagreements were resolved and a final consensus was reached.
Data Extraction
Data were extracted independently by two authors subsequently after all the eligible studies were recruited. All pertinent information regarding participants and clinical outcomes were recorded. Participants’ information included the number of patients, age, gender (the rate of males in all participants). The principal outcomes of interest included details of operative time, postoperative functional outcomes (ASES, American Shoulder and Elbow Surgeons; UCLA, University of California at Los Angeles; Constant-Murley score), range of motion, pain score as well as reported complications (retear rate, adhesive capsulitis).
Study Quality
Based on the Cochrane Bone, Joint and Muscle Trauma Group [6], assessment of the methodological quality of each included study was made by the 2 reviewers who were blinded with respect to the journal, the authors and the source institution. Any controversy was cross-checked and resolved by a third author to reach a final consensus.
Statistical Analysis
Study-specific RR (Ratio Risks) and associated 95% CI (confidence intervals) accounting for discontinuous variables within the study were pooled using a random-effects model, which considered both within-study and between-study variation. Standardized mean difference (SMD) was used for continuous variables for which a fixed effect model was used initially. Heterogeneity is expressed as P and I2. This value of I2 ranges from 0% (complete consistency) to 100% (complete inconsistency). If the P value of heterogeneity test was <0.1 or I2>50% [7], the random-effect model replaced the fixed modality. Sensitivity analysis was performed to evaluate the stability of the results if necessary. Subgroup analysis was conducted to get some more concrete conclusions if the data was present. Forest plots were used to graphically present the results of individual studies and the respective pooled estimate of effect size. All statistical analyses were performed with Review Manager (version 5.0.0 for Windows, The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, 2008).
Results
Study Characteristics
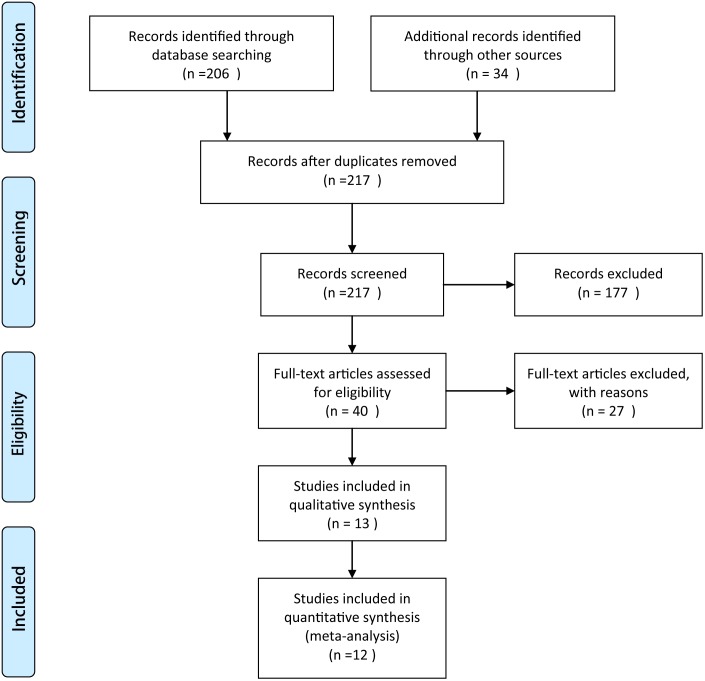
A flow chart of the studies recruited in our review was shown in Figure 1 (Fig. 1). We identified 240 potential citations (162 from Pubmed; 26 from Embase; 18 from the Cochrane Randomized Trials Databases; and 34 from relevant journals) aiming at comparing AA and MO in the treatment of rotator cuff tears. After reading the articles, as well as communicating with the first author to get additional studies or data, 13 of the 240 citations were selected for application. There was one study belonging to the same institution with different follow-up and only the recent study was selected. As a result, 12 articles [8]–[19] including a total of 770 patients (422 in the AA group and 348 in the MO group) were identified in the final analysis. Demographic information for members of each group was provided in Table 1. The 12 studies on the two different treatment choices for rotator cuff tears were published between 2003 and 2013 (Table 1). Preoperative patient characteristics did not show any significant difference between these two groups with respect to the number of patients, gender and age.
Figure 1. Flow chart of the studies recruited in this meta-analysis.
Table 1. Demographic information for members of each group.
| author | year | Type of study | Group | No | F/M | Age | Follow-up | OT | UCLA S | ASES S | Consant S | VAS S | Flextion | Rotation | Abduction | Retear | AC | Evidence |
| Zwaal et al | 2013 | RCT | ASR | 47 | 18/29 | 57.2y | 56w | 73.5±17.6 | NG | NG | 73.5±17.6 | NG | 170±2.6 | 80±2.0 | NG | 8 | 5 | III |
| MOP | 48 | 20/28 | 57.8y | 56w | 53.8±13.7 | 53.8±13.7 | 159±4.3 | 72±2.9 | 6 | 6 | ||||||||
| Cho et al | 2012 | RCT | ASR | 30 | 13/17 | 55.5y | 6m | 57.67±11.04 | NG | NG | NG | 1.07±1.08 | 159.50±8.74 | 52.83±7.39 | NG | NG | 5 | III |
| MOP | 30 | 13/17 | 56.2y | 6m | 61.0±14.65 | 1.13±1.07 | 157.67±15.8 | 53.0±11.11 | 4 | |||||||||
| Kasten et al | 2011 | RCT | ASR | 17 | 8/9 | 60.1y | 6m | NG | NG | 81±20 | NG | 2.0±1.5 | 160±15 | 86±10 | NG | 3 | NG | III |
| MOP | 17 | 5/12 | 60.1y | 6m | 86.9±16.3 | 1.2±0.8 | 164±7 | 75±18 | 3 | |||||||||
| Stone et al | 2009 | prospective | ASR | 92 | 48/44 | 57y | 24m | NG | NG | NC | 76.58 | NG | NG | NG | NG | NG | NG | II |
| MOP | 31 | 15/16 | 62y | 24m | 69.14 | |||||||||||||
| Kose et al | 2008 | retrospective | ASR | 25 | 18/7 | 55y | 31.20m | NG | 29.76±4.5 | NG | 83.56±11.45 | NG | NG | NG | NG | NG | NG | II |
| MOP | 25 | 21/4 | 62y | 21.56m | 28.8±3.42 | 79.56±13.64 | ||||||||||||
| Liem et al | 2007 | retrospective | ASR | 19 | 3/16 | 61.9y | 25.0m | NG | NG | NG | 83.9 | NC | 176 | 59 | 173 | NG | 4 | II |
| MOP | 19 | 3/16 | 62.1y | 17.6m | 83.7 | 175 | 56 | 175 | 2 | |||||||||
| Verma et al | 2006 | retrospective | ASR | 38 | 16/22 | 59.4y | 24m | NG | NG | 94.6±8.9 | NG | 0.7±1.2 | 170.5±6.9 | 68.2±16.7 | 169.6±7.5 | 9 | 1 | II |
| MOP | 33 | 10/23 | 60.7y | 24m | 95.1±5.3 | 0.4±1.0 | 169.4±6.9 | 70.2±14. | 168.9±8.4 | 9 | 0 | |||||||
| Andreas et al | 2005 | retrospective | ASR | 26 | 10/16 | 56y | 19m | NG | NG | 86(43–100) | NG | NG | NG | NG | NG | NG | 16 | II |
| MOP | 28 | 12/16 | 57y | 33m | 89(56–100) | 15 | ||||||||||||
| Warner et al | 2005 | retrospective | ASR | 9 | 4/5 | 53y | 44m | NG | NG | NG | NG | NG | 160 (130–170) | 50 (30–60) | NG | NG | NG | II |
| MOP | 12 | 4/8 | 55y | 44m | 155 (110–170) | 50 (25–60) | ||||||||||||
| Youm et al | 2005 | retrospective | ASR | 42 | NG | 60 | 37.6m | NG | 33.2±2.5 | 91.1±15.4 | NG | NG | NG | NG | NG | NG | NG | II |
| MOP | 42 | 59 | 37.6m | 32.3±3.3 | 90.2±14.8 | |||||||||||||
| Kim et al | 2003 | retrospective | ASR | 42 | 15/27 | 55 | 39m(24–72) | NG | NG | 95±7.2 | NG | 0.7±1.1 | NG | NG | NG | 0 | 0 | II |
| MOP | 34 | 22/12 | 39m(24–72) | 95±7.3 | 1.0±1.5 | 1 | 4 | |||||||||||
| Severud et al | 2003 | retrospective | ASR | 35 | NG | NG | 44.6m | NG | 32.6 | 91.7 | NG | NG | NG | NG | NG | NG | NG | II |
| MOP | 29 | 44.6m | 31.4 | 90 |
Abbreviations: Year = year of publication; OT = operative time; RCT = randomized clinical trials; ASR = arthroscopic repair; MOP = mini open repair; UCLA S = University of California at Los Angeles Score; ASES S = American Shoulder and Elbow Surgeons index Score; Constant S = Constant-Murley score; VAS = visual analog scale pain score;AC = adhesive capsulitis; NG = not given.
Outcome Measurements
The results of RR/SMD and 95% CI for each comparison were shown in Table 2. Because of lacking consistency in the way the outcomes were acquired (e.g. the time points when the measurements were conducted differed among the studies), almost all the results were obtained directly from the pooling of data without stratifying by different periods. Moreover, not all studies provided necessary data, so we only compared with the limited articles which might contribute bias to our final results.
Table 2. Outcome measures in the meta-analysis of comparisons between all arthrosopic and mini-open cuff tear repair.
| Outcome | Risk ratio (95% CI) | P | STD (95% CI) | Heterogeneity | I 2% | Number of patients | Nubmer of studies |
| UCLA score | 0.11 | 0.28 (−0.06, 0.62) | 0.85 | 0 | 134 | 2 | |
| AESE score | 0.74 | −0.04(−0.28, 0.20) | 0.83 | 0 | 270 | 4 | |
| Consant score | 0.12 | 0.91 (−0.24, 2.05) | 0.002 | 90 | 145 | 2 | |
| VAS score | 0.59 | −1.55(−2.01, 0.53) | <0.00001 | 91 | 336 | 5 | |
| Forward flextion | 0.29 | 0.76 (−0.66, 2.17) | <0.00001 | 96 | 260 | 4 | |
| External rotation | 0.21 | 0.94 (−0.53, 2.40) | <0.00001 | 96 | 260 | 4 | |
| Retear | 0.99(0.57, 1.73) | 0.97 | 0.76 | 0 | 280 | 4 | |
| Adhesive capsulitis | 1.12 (0.76, 1.64) | 0.57 | 0.52 | 0 | 394 | 6 |
Abbreviation: STD = Std Mean Difference; VAS = visual analog scale pain score; ASES = American Shoulder and Elbow Surgeons; UCLA = University of California at Los Angeles.
Functional Results (UCLA Score, AESE Score, Constant Score)
7 studies [8]–[10], [12], [14], [17], [18] using different score systems were involved when comparing the function score between two groups. There was no difference in the function outcome scores between the two groups. Even though at different periods of follow-up, patients got the similar function score measured as UCLA (STD = 0.28 95% CI −0.06, 0.62), AESE (STD = −0.04 95% CI −0.28, 0.20) and Constant (STD = 0.91 95% CI −0.24, 2.05). Several studies in which only mean value was provided were not included. However, authors in these studies gave homologous results as our outcome.
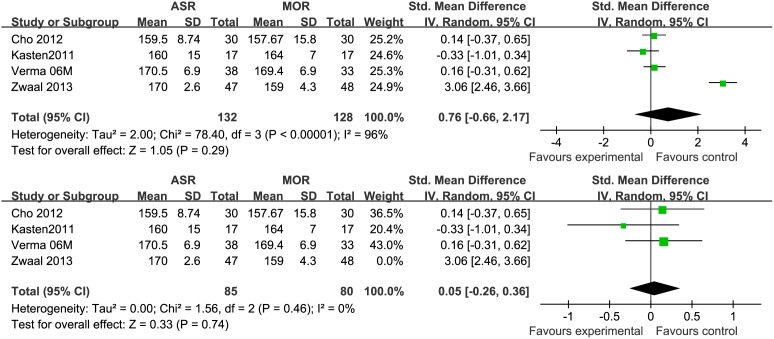
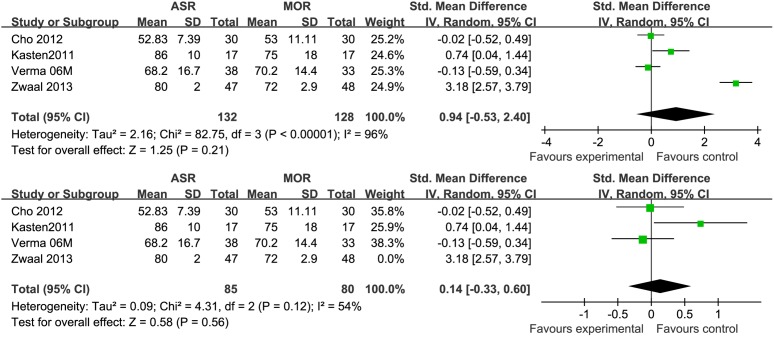
Range of Motion (Forward Flextion, External Rotation)
Based on the available data, only 4 studies [8]–[10], [14] provided the information about postoperative range of motion (Forward flextion, External rotation) with 260 patients. Among these 4 studies, only one examined the degree of abduction as mean and standard deviation. No statistical difference was observed in either forward flextion (STD = 0.76 95% CI −0.66, 2.17) or external rotation (STD = 0.94 95% CI −0.53, 2.40). During analysis, an obvious heterogeneity (p<0.0001) of the combined data was found. Each of the 4 studies was excluded respectively to do a sensitivity analysis. The result showed that the heterogeneity decreased only when the study published in 2013 by Zwaal et al [8] excluded (Fig. 2, 3). Zwaal reported a significant greater range of motion in both flextion and external rotation in AA group. We tried to find the potential difference between this one and the other three studies and found that patients with simultaneous lesions of the shoulder were excluded by Zwaal. Another possible reason was that all arthroscopic repair would provide a more rapid rehabilitation and better function with advanced techniques and skills.
Figure 2. Forest plot showing the SMD (Standardized mean difference) and 95% CI for Forward flextion after surgery with and without the study by Zwaal13 during a sensitivity analysis.
The heterogeneity decreased significantly when the study by Zwaal et al was excluded.
Figure 3. Forest plot showing the SMD (Standardized mean difference) and 95% CI for External rotation after surgery with and without the study by Zwaal13 during a sensitivity analysis.
The heterogeneity decreased significantly when the study by Zwaal et al was excluded.
VAS Score
A total of 5 studies [8]–[10], [14], [18] including 336 patients were included for analysis of pain score (visual analog scale pain score was chosen as the Uniform standards). Two studies measured this value at 6 month follow-up and the other three gave the data at 12m, 24m, 39m respectively. The 95% CI ranged from −0.21 to 0.53 and the value of Std Mean Difference was 0.59. No significant difference was seen in regards to VAS score. Like comparison of range of motion, an obvious heterogeneity (p<0.0001) occurred in VAS analysis which disappeared while excluding the study by Zwaal et al [8]. The reason might equally own to arthroscopic development.
Compliation
Seven studies [8]–[10], [13]–[15], [18] and 428 cases were available for the analysis of complications. Even though most previous studies have showed a difference between AA and MO in complications, no significant difference was seen in this meta analysis with respect to postoperative incidence of retear (OR = 0.99, 95% CI 0.57, 1.73) or adhesive capsulitis (OR = 1.12, 95% CI 0.76, 1.64) without any heterogeneity.
Discussion
Arthroscopy was first used in the treatment of rotator cuff tears as a diagnostic tool, enabling the surgeon to diagnose glenohumeral pathology [20]. Interest in an all-arthroscopic technique has increased in recent years as arthroscopic techniques continue to improve and advance. Mini-open repair represent an attempt to combine the advantages of arthroscopic and open repair. The ability to investigate intra-articular pathology and still repair the tendon with bone tunnels without taking down the deltoid origin has made mini open repair a popular technique. Arthroscopic technique is technically more demanding than the mini-open surgery. The mini-open technique provides direct visualization of the cuff repair and allows the surgeons to place the stitches in an open technique, which is more convenient and familiar for surgeons. The mini-open technique also allows for tension absorbing stitches to be placed in the cases where they are needed. Earlier studies published on all-arthroscopic versus mini-open rotator cuff repair did not find any significant difference between the treatment groups [14]–[17], [19], [21]. In this meta-analysis, we demonstrate similar results, with no differences noted in clinical outcomes between the arthroscopic group and the mini-open group for all scoring scales evaluated. Our analysis is the first high-quality study with the largest number and highest level of articles.
However, some studies [8], [10], [21] have demonstrated that the all-arthroscopic procedure does obtain its treatment effect faster than the mini-open procedure with respect to improvement in function score, VAS pain/impairment scores, and range of motion within 6m postoperatively. None of the other studies reported postoperative pain assessments within such a short time after surgery. This could be attributed to the greater compromise of deltoid muscle tissue in the MO group resulting from increased swelling and detachment of muscle fibers from the acromion [22]. Given that decreased postoperative pain is often associated with a quicker return to work, further study to confirm these results would be helpful in recommending all arthroscopic repair on the basis of decreased postoperative pain. For the 7 studies with a minimum follow-up of 2 years included in this meta-analysis, there were no statistically significant differences in preoperative functional or pain score between groups within each study.
In terms of postoperative adhesive capsulitis, AA offers some advantages over the MO repair. The mini-open approach requires a split in the deltoid fibers extending into the subdeltoid bursa, even though the deltoid origin is preserved. This may lead to subacromial scarring and stiffness [23].Using three to four portal sites instead of a 3to 4 cm incision, arthroscopic technique can potentially reduce the risk of this complication. Because the deltoid origin is preserved during mini open repair, rehabilitation of the shoulder can be less restricted as it is not necessary to wait until the deltoid is healed to the acromion. Currently, with the help of postoperative rehabilitation protocol made by special physical therapist, patients get a quick rehabilitation in both groups and no difference in adhesive capsulitis was detected in this analysis.
Another important issue to patients and their physicians is the recurrent rotator cuff tear. Despite many published concerns regarding long-term integrity of repair [24], [25], our study comparing all-arthroscopic methods to mini-open techniques with mixed populations (small, middle and large tears) showed no difference in incidence of recurrent tears. While exploring the incidence of retear after arthroscopic rotator cuff repair alone, some studies have shown excellent function outcome [26], [27]. The correlation of functional results with integrity of the cuff is worth attention. Liu and Baker [28] presented an interesting result after a minimum follow-up of 2 years. Patients with larger tears had a higher incidence of persistent defects, but there was no significant difference in function outcome between patients with and without defects. Therefore, they got a conclusion that function outcome was not determined by the integrity of the cuff. In a short-term follow-up, Liem et al [13], have correlated the clinical outcome of arthroscopic rotator cuff repairs with magnetic resonance imaging evidence of repair integrity and demonstrated improvements in clinical outcome, regardless of repair integrity. An interesting finding from Verma [14] was that retear rate was higher for the open group and lower for the arthroscopic group for tears smaller than 3 cm, for tears larger than 3 cm, retear rate was lower for the open group and higher for the arthroscopic group. However, this difference was not statistically significant. Although we did not compare outcomes of rotator cuff repair based on tear size in the present study, some factors influencing the high rotator cuff retear rate can’t be ignored including tear size, preoperative duration of symptoms, degeneration of cuff, fixation technique or hardware used.
Arthroscopic repair of the rotator cuff is technically demanding and requires a long learning curve for a surgeon to become specialist in this domain [13], [29]. The mini-open surgical repair technique has a various repair choices from bone tunnels to implantable suture anchors, while only the implantable suture anchor devices can be used for all-arthroscopic surgical technique which may result in the all-arthroscopic rotator cuff repair costing more time [30]. Conversion to a mini-open or open approach is easily done if needed. Because of the technical demands of arthroscopic repair, many researchers consider one of the most obvious advantages of the mini open repair procedure is that it consumes less operative time. 2 [8], [10] of the 12 included studies gave the data about operative time. One was published in 2013 [8], the mean time of surgery were 73.5 min and 53.8 min for AA and MO repair respectively with a dominance of reduced 20 min for MO group. Another study published in 2012 [10], conversely a shorter operative duration was obtained in AA group (57.67 min versus 61.00 min). Neither of these two studies showed any significant difference about surgery time. With recent innovations and technologic advances of general arthroscopic instruments and rotator cuff repair-specific appliances, arthroscopic repair does achieve a good clinical result with shorted operative time.
Limitation
Some limitations must be recognized in this meta-analysis. First of all, in spite of this fact that we have included all the eligible comparative studies, the number of patients is relatively small. Second, some parameters (eg. Operative time, the degree of abduction, total cost) were not analyzed as a result of insufficient data. Furthermore, there were many variations of the 12 included studies. For instance, specific inclusion and exclusion criteria varied, as some studies included patients who had undergone other procedures for additional intra-articular pathology during surgery, whereas others did not. Some use bone tunnels and others use suture anchors for osseous fixation in mini open group. Future studies should address this issue.
Conclusion
This Meta analysis demonstrated that arthroscopic and mini-open repair produce equivalent clinical outcomes in the middle to long postoperative period. Overall, both arthroscopic and mini open techniques are effective and viable options for surgeons with advanced arthroscopic skills.
Supporting Information
PRISMA Checklist.
(DOC)
Funding Statement
The authors have no support or funding to report.
References
- 1.Codman EA (1990) Rupture of the supraspinatus tendon. 1911. Clin Orthop Relat Res: 3–26. [PubMed]
- 2. Nho SJ, Shindle MK, Sherman SL, Freedman KB, Lyman S, et al. (2007) Systematic review of arthroscopic rotator cuff repair and mini-open rotator cuff repair. J Bone Joint Surg Am 89 Suppl 3127–136. [DOI] [PubMed] [Google Scholar]
- 3. Lindley K, Jones GL (2010) Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead NJ) 39: 592–600. [PubMed] [Google Scholar]
- 4. MacDermid JC, Holtby R, Razmjou H, Bryant D (2006) All-arthroscopic versus mini-open repair of small or moderate-sized rotator cuff tears: a protocol for a randomized trial [NCT00128076]. BMC Musculoskelet Disord 7: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, et al. (2008) Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med 36: 1824–1828. [DOI] [PubMed] [Google Scholar]
- 6. Handoll HH, Gillespie WJ, Gillespie LD, Madhok R (2007) Moving towards evidence-based healthcare for musculoskeletal injuries: featuring the work of the Cochrane Bone, joint and Muscle Trauma Group. J R Soc Promot Health 127: 168–173. [DOI] [PubMed] [Google Scholar]
- 7. Cochran WG (1954) The combination of estimates from different experiments. Biometrics 10: 101–129. [Google Scholar]
- 8. van der Zwaal P, Thomassen BJ, Nieuwenhuijse MJ, Lindenburg R, Swen JW, et al. (2013) Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomized controlled trial in 100 patients with 1-year follow-up. Arthroscopy 29: 266–273. [DOI] [PubMed] [Google Scholar]
- 9. Kasten P, Keil C, Grieser T, Raiss P, Streich N, et al. (2011) Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop 35: 1663–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cho CH, Song KS, Jung GH, Lee YK, Shin HK (2012) Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics 35: e1347–1352. [DOI] [PubMed] [Google Scholar]
- 11. Colegate-Stone T, Allom R, Tavakkolizadeh A, Sinha J (2009) An analysis of outcome of arthroscopic versus mini-open rotator cuff repair using subjective and objective scoring tools. Knee Surg Sports Traumatol Arthrosc 17: 691–694. [DOI] [PubMed] [Google Scholar]
- 12. Kose KC, Tezen E, Cebesoy O, Karadeniz E, Guner D, et al. (2008) Mini-open versus all-arthroscopic rotator cuff repair: comparison of the operative costs and the clinical outcomes. Adv Ther 25: 249–259. [DOI] [PubMed] [Google Scholar]
- 13. Liem D, Bartl C, Lichtenberg S, Magosch P, Habermeyer P (2007) Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy 23: 514–521. [DOI] [PubMed] [Google Scholar]
- 14. Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, et al. (2006) All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy 22: 587–594. [DOI] [PubMed] [Google Scholar]
- 15. Sauerbrey AM, Getz CL, Piancastelli M, Iannotti JP, Ramsey ML, et al. (2005) Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy 21: 1415–1420. [DOI] [PubMed] [Google Scholar]
- 16. Warner JJ, Tetreault P, Lehtinen J, Zurakowski D (2005) Arthroscopic versus mini-open rotator cuff repair: a cohort comparison study. Arthroscopy 21: 328–332. [DOI] [PubMed] [Google Scholar]
- 17. Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD (2005) Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg 14: 455–459. [DOI] [PubMed] [Google Scholar]
- 18. Kim SH, Ha KI, Park JH, Kang JS, Oh SK, et al. (2003) Arthroscopic versus mini-open salvage repair of the rotator cuff tear: outcome analysis at 2 to 6 years’ follow-up. Arthroscopy 19: 746–754. [DOI] [PubMed] [Google Scholar]
- 19. Severud EL, Ruotolo C, Abbott DD, Nottage WM (2003) All-arthroscopic versus mini-open rotator cuff repair: A long-term retrospective outcome comparison. Arthroscopy 19: 234–238. [DOI] [PubMed] [Google Scholar]
- 20. Wiley AM, Older MW (1980) Shoulder arthroscopy. Investigations with a fibreoptic instrument. Am J Sports Med 8: 31–38. [DOI] [PubMed] [Google Scholar]
- 21.Kang L, Henn RF, Tashjian RZ, Green A (2007) Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy 23: 573–582, 582.e571–572. [DOI] [PubMed]
- 22. Wright RW, Baumgarten KM (2010) Shoulder outcomes measures. J Am Acad Orthop Surg 18: 436–444. [DOI] [PubMed] [Google Scholar]
- 23. Mormino MA, Gross RM, McCarthy JA (1996) Captured shoulder: a complication of rotator cuff surgery. Arthroscopy 12: 457–461. [DOI] [PubMed] [Google Scholar]
- 24. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-a: 219–224. [DOI] [PubMed] [Google Scholar]
- 25. Schneeberger AG, von Roll A, Kalberer F, Jacob HA, Gerber C (2002) Mechanical strength of arthroscopic rotator cuff repair techniques: an in vitro study. J Bone Joint Surg Am 84-a: 2152–2160. [DOI] [PubMed] [Google Scholar]
- 26. Lee E, Bishop JY, Braman JP, Langford J, Gelber J, et al. (2007) Outcomes after arthroscopic rotator cuff repairs. J Shoulder Elbow Surg 16: 1–5. [DOI] [PubMed] [Google Scholar]
- 27. Bennett WF (2003) Arthroscopic repair of full-thickness supraspinatus tears (small-to-medium): A prospective study with 2- to 4-year follow-up. Arthroscopy 19: 249–256. [DOI] [PubMed] [Google Scholar]
- 28. Liu SH, Baker CL (1994) Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy 10: 54–60. [DOI] [PubMed] [Google Scholar]
- 29. Buess E, Steuber KU, Waibl B (2005) Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy 21: 597–604. [DOI] [PubMed] [Google Scholar]
- 30. Pietschmann MF, Froehlich V, Ficklscherer A, Wegener B, Jansson V, et al. (2008) Biomechanical testing of a new knotless suture anchor compared with established anchors for rotator cuff repair. J Shoulder Elbow Surg 17: 642–646. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.
(DOC)