Abstract
Objectives
To evaluate race-related differences in depression onset and recovery in older persons, overall and by sex, and examine race-related differences in mortality according to depression.
Design
Prospective cohort study.
Setting
General community in pre-designated zip code areas in Memphis, Tennessee, and Pittsburgh, Pennsylvania.
Participants
3,075 persons age 70-79 at baseline in the Health, Aging, and Body Composition study.
Measurements
Depression was assessed at 8 time points over 10 years using the 10-item Center for Epidemiologic Studies – Depression (CES-D) scale; scores of <8 and ≥8 denoted nondepressed and depressed, respectively. We created variables for transitions across each 18-month time interval, namely, from nondepressed or depressed to nondepressed, depressed, or death, and determined the association between race and the average likelihood of these transitions over time.
Results
A higher percentage of blacks than whites were depressed at nearly all time points. Adjusting for demographics, common chronic conditions, and body mass index, blacks had a higher likelihood of experiencing depression onset than whites (odds ratio, 1.22; 95% confidence interval, 1.03-1.43); among men, blacks were more likely to experience depression onset than whites (odds ratio, 1.44; 95% confidence interval, 1.24-2.89). Blacks also had a higher likelihood of transitioning from nondepressed to death (odds ratio, 1.79; 95% confidence interval, 1.30-2.46). Overall and in sex-stratified analyses, race was not associated with recovery from depression or with the transition from depression to death.
Conclusion
Our findings highlight race differences in depression in older persons and encourage further research on the course of depression in older blacks.
Keywords: Aging, Depression, Depressive symptoms, Race differences, Epidemiology, Prospective studies
OBJECTIVE
Depression is a significant clinical and public health problem for older persons. Whereas major depression affects 1%–2% of community-living persons age 65 and older(1), 8%–30% of this population experiences clinically significant depressive symptoms(1, 2). Clinically significant depressive symptoms, often referred to simply as “depression,” are associated with negative outcomes including high health services utilization, disability, dementia, and mortality (3-8). What we know about the course of depression in older persons, however, has come largely from overwhelmingly white samples (9-11).
Older Americans are becoming increasingly diverse, with blacks projected to account for at least 12% of persons ≥65 living in the U.S. by 2050(12). Despite growing numbers of blacks living to older ages, and the national public health goal of reducing health disparities between minority and non-minority populations (13), whether or not race differentially influences the course of depression in older persons remains uncertain.
Depression is highly variable over time, with periods of chronicity, remission and recurrence (14, 15). Yet, most studies evaluating race-related differences in depression have been cross-sectional, focusing on prevalence estimates or number of symptoms at one time point as outcomes (16-19). Furthermore, the few longitudinal studies evaluating race-related differences in the course of depression in older persons have focused on symptom trajectories and average symptom levels rather than transitions into and out of clinically meaningful states of depressive symptoms (20-23). Of these, only two considered the potential impact of mortality on race differences in depression over time (20, 23). Additionally, the same non-modifiable factors that predict depression onset may not predict the course of depression. For example, low educational attainment and female sex have been found to be associated with depression onset (24-26) but not remission (27). Relatedly, female sex has been found to be associated with more severe depressive symptoms (28) and a higher likelihood of receiving treatment for depression (29), while black race is associated with a lower likelihood of initiation and adherence to depression treatment(30). Consequently, whether there are race-related differences in the onset of and recovery from depression in older persons, or whether race is similarly associated with these outcomes in men and women, remains unknown.
The objectives of this prospective study were to determine whether there are race-related differences, overall and by sex, in the onset of depression (i.e., first or recurrent episodes) and recovery from depression in older persons over time and to examine race-related differences in mortality according to depression. To achieve these objectives, we evaluated possible transitions between three states—not depressed, depressed, and death— over 10 years in a large cohort of older men and women. Improved understanding of these race-related differences will support efforts to identify and subsequently reduce racial disparities in depression treatment and prevention.
METHODS
Study Population
Participants were members of the Health, Aging, and Body Composition (Health ABC) study. Assembly of the cohort (N=3,075) has been described elsewhere(31). In brief, participants constitute a random sample of white Medicare beneficiaries and all age-eligible black community-dwelling residents in pre-designated zip code areas in Memphis, Tennessee, and Pittsburgh, PA, who were aged 70 to 79 years at time of enrollment between April 1997 and June 1998. At baseline, all participants reported no difficulty walking 0.25 miles, walking up ten steps without resting, and performing basic activities of daily living. Participants signed a written informed consent and protocols were approved by the study site institutional review boards.
Data Collection
Health ABC data were collected using both face-to-face interviews and clinic visits that occurred over 10 years of follow-up. Because depressive symptoms were not assessed during years 2, 7 and 9, data from years 1, 3, 4, 5, 6, 8, 10, and 11 were included in the present study. Participants unable to attend their clinic visit were offered a home visit or a telephone follow-up. Deaths were ascertained by proxy report and were confirmed by obtaining death certificates. A total of 1,160 (37.7%) participants died after a mean (SD) follow-up of 5.7 (±2.6) years.
Demographic data, including race, age, sex, years of education, and poverty status were collected during the Year 1 (i.e., baseline) face-to-face interview. Participants self-identified their race as either white or black. Education was categorized as less than high school and high school or more. Poverty was determined by applying a set of income thresholds that vary by family size and composition issued in 1998 by the U.S. Census Bureau to reported annual income levels. Every participant was assigned a value representing a percentage of the federal poverty level. Participants with an income level at or below 150% of the federal poverty level were considered to have low socioeconomic status (SES). This indicator, commonly used in determining eligibility for federal and state public assistance programs, has been used previously with these data (32). Presence of coronary heart disease (CHD), stroke, diabetes, and cancer were ascertained at baseline and during subsequent face-to-face interviews by asking participants if a doctor told them that they had each of these conditions. Body mass index (BMI), reported as kg/m2, was calculated from measured weight and height collected during the clinic assessments.
Assessment of depressive symptoms and transition states
Depressive symptoms were assessed during the face-to-face interviews at years 1, 3, 4, 5, 6, 8, 10, and 11 using the 10-item Center for Epidemiologic Studies – Depression (CES-D) scale. Participants were asked about the frequency of depressive symptoms in the past week. Total scores range from 0 to 30, and participants scoring ≥8 were considered as “depressed” (33). Data on depression were complete for 99% of the participants at baseline and 96%, 94%, 94%, 94%, 76%, 78%, and 80% of the 3075 participants at years 3, 4, 5, 6, 8, 10, and 11, respectively. Because the CES-D was not administered to study participants at all visit types in years 8, 10 (i.e., home visit, telephone interview), and 11 (e.g., home visit), the total percent with depression data was lower than in previous years. However, of the participants who could have completed the CES-D in years 8, 10, and 11, less than 1% were missing depression data.
We then created variables for six possible transitions that could occur across each of the 18-month time intervals. The transitions were nondepressed to nondepressed, nondepressed to depressed (i.e., depression onset), or nondepressed to death; and depressed to nondepressed (i.e., recovery), depressed to depressed; or depressed to death. We have used this approach previously to evaluate transitions into and out of depression states over time (24). Because there were seven time intervals over the 10-year study period (e.g., years 1 to 3; years 3 to 4), each participant had an opportunity to contribute up to a total of seven transitions.
Statistical Analyses
We compared baseline participant characteristics by race using χ2 or t test statistics. We then used the χ2 statistic to determine if the percentage of whites and blacks with depression at each time point was significantly different. To determine whether the observed transitions into and out of depression were clinically meaningful, we calculated the percentage of transitions that represented absolute changes in the CES-D scores ≥4 points for each of the 18-month time intervals. We subsequently determined whether the distribution of these percentages differed by race using the χ2 statistic.
Given the likely intracorrelation between estimates over time, running a polytomous logistic regression model at each time interval would likely yield biased results. Consequently, we used longitudinal statistical methods to determine if, on average over time, race was associated with depression onset (i.e., transition from a nondepressed to a depressed state) and recovery from depression (i.e., transition from a depressed to a nondepressed state) and to examine race-related differences in the average likelihood of transitioning from a nondepressed or a depressed state to death. Specifically, we ran generalized multinomial logit models for nominal outcomes that were estimated with a generalized estimating equation (GEE) and used exchangeable correlation structures. We ran one longitudinal model which included all participants who were nondepressed at the beginning of any of the 7 time intervals. Participants who remained nondepressed during an interval (i.e., at two consecutive time points) were used as the reference group. Consequently, the parameter estimates for the model reflected the population values averaged across the respective strata; nondepressed to depressed and nondepressed to death versus remaining nondepressed. The second model included participants who were depressed at the beginning of any of the 7 time intervals. Participants who remained depressed during an interval were used as the reference group and the parameter estimates reflected the population values averaged across the respective strata; depressed to nondepressed and depressed to death versus remaining depressed. Final models were adjusted for age, sex, race, education, poverty, chronic conditions, BMI, and study site. We then ran the above models with a Race X Sex interaction term, and subsequently conducted sex-stratified analyses. Because the CES-D was not administered to study participants at all visit types in years 8, 10, and 11, we re-ran the models using only the data from years 1, 3, 4, 5, and 6 for comparison purposes. Finally, to complement the aforementioned analyses, and confirm the findings from prior studies, we repeated these analyses after considering depression as a continuous variable. We used generalized estimating equations to fit multivariate, marginal, linear regression models to determine if the average depression score over time differed by race.
Data were analyzed using SAS version 9.3 (SAS Institute, Inc., Cary, NC). Longitudinal models were performed using SUDAAN statistical software version 11.0 (RTI Institute, Research Triangle Park, NC). The threshold for statistical significance was α ≤0.05 (two-tailed).
RESULTS
Baseline Characteristics
Table 1 provides the baseline characteristics of the sample overall and according to race. The average age of the 3,075 participants was 73.6 (±2.9) years and approximately half were female and half were recruited from each site. Approximately one quarter of the sample did not graduate from high school and 46.2% were at or below the 150% poverty level. Cancer was the most prevalent chronic condition, reported by approximately 18% of the sample, followed by diabetes, CHD, and stroke. The average BMI was 27.4 (±4.8). Differences by race were observed for all characteristics with the exception of CHD. Blacks’ average age was older and BMI was higher than whites’ average age and BMI, and a higher percentage of blacks were female, were at or below the 150% poverty level, reported having stroke and diabetes, and lived in Pittsburgh. A higher percentage of whites reported having cancer. These race differences were largely observed within men and women, with the exception of age and CHD; average age did not differ by race for men, and among women a higher proportion of blacks had CHD (data not shown).
Table 1.
Baseline Characteristics of Participants According to Race; Health, Aging, and Body Composition Study 1998-1999.
| Characteristic | Overall (N=3,075) | White (n=1,794) | Black (n=1,281) | Wald Chi-square or ta | P-value |
|---|---|---|---|---|---|
| Age, mean (SD) | 73.6 (2.9) | 73.8 (2.9) | 73.4 (2.9) | t=3.19 | <0.001 |
| Female, n (%) | 1584 (51.5) | 855 (47.7) | 729 (56.9) | 25.60 | <0.001 |
| Not a high school graduate, n (%) | 775 (25.2) | 219 (12.2) | 556 (43.6) | 162.08 | <0.001 |
| At or below 150% poverty level, n (%) | 1421 (46.2) | 569 (31.7) | 852 (66.5) | 405.90 | <0.001 |
| Coronary Heart Disease, n (%) | 357 (11.6) | 207 (11.5) | 150 (11.7) | 0.027 | 0.87 |
| Stroke, n (%) | 72 (2.3) | 25 (1.4) | 47 (3.7) | 17.15 | <0.001 |
| Diabetes, n (%) | 460 (15.0) | 191 (10.7) | 269 (21.0) | 63.17 | <0.001 |
| Cancer, n (%) | 579 (18.8) | 439 (24.5) | 140 (11.0) | 89.37 | <0.001 |
| Body Mass Index, mean (SD) | 27.4 (4.8) | 26.5 (4.1) | 28.6 (5.4) | t=−11.38 | <0.001 |
| Pittsburgh, n (%) | 1527 (49.7) | 859 (47.9) | 668 (52.2) | 5.44 | 0.02 |
Wald chi-square tests have df = 1, t-statistics have df = 3073
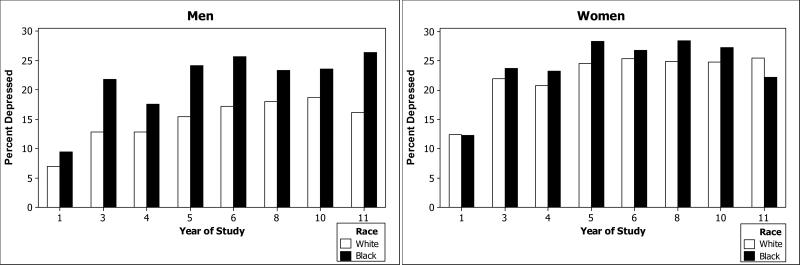
A total of 310 (10.1%) participants were depressed at baseline (i.e., CES-D≥8), with no difference according to race (chi-square test statistic = 1.69; df=1; P=0.19). There were 19.5%, 18.4%, 22.5%, 23.6%, 23.1%, 23.2%, and 21.9% depressed participants at years 3, 4, 5, 6, 8, 10, and 11, respectively and a significantly higher percentage of blacks than whites were depressed at each time point, with the exception of years 10 and 11 where there was no race difference. Of the nondepressed at baseline, 1,030 (37.6%) experienced depression at some other point during the study. Whereas there were no race-related differences in the percentage of depressed women at any time point, black men were significantly more likely to be depressed than white men at nearly all time points (Figure 1).
Figure 1.
Percentage of depressed (CES-D score >8) White and Black men (Panel A) and White and Black women (Panel B) over 10 years of follow-up, in the Health, Aging, and Body Composition Study. Visit year: year 1, 1997–1998; year 3, 1999-2000; year 4, 2000–2001; year 5, 2001-2002; year 6, 2002–2003; year 8, 2004-2005; year 10, 2007-2008; year 11, 2008-2009. Among men, a significantly higher percentage of Blacks were depressed at years 3, 4, 5, 6, and 11; among women, the percentage of those who were depressed did not differ between Whites at Blacks any year during the study.
The majority of transitions from a nondepressed state to a depressed state, or vice versa, were based on absolute changes in CES-D scores of ≥4 points. Of the participants who transitioned from a nondepressed to a depressed state, 86%; 69%; 77%; 66%; 69%; 66%; and 58% had a ≥4-point absolute change in their CES-D score over each time interval, respectively. Of those who transitioned from a depressed to a nondepressed state, 70%; 74%; 67%; 67%; 70%; 72%; and 75% had a ≥4-point absolute change in their CES-D score over each time interval, respectively. There were no differences in the distribution of change scores by race for either transition.
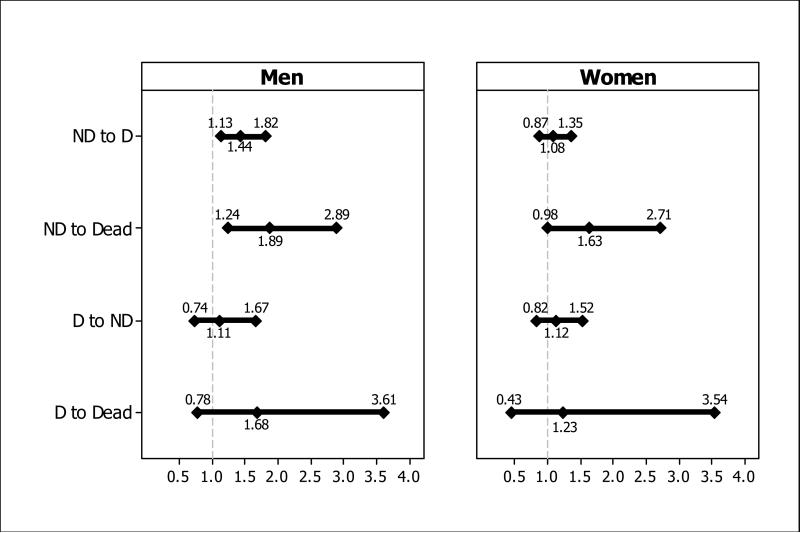
Table 2 presents the results from the longitudinal models evaluating the association between race and the likelihood of each of the six possible transitions over 10 years. Among the nondepressed, blacks were significantly more likely to transition to a depressed state (i.e., onset) and to death. Among the depressed, there were no race-related differences in transition to a nondepressed state (i.e., recovery) or death. The Race X Sex interaction term was statistically significant in the model evaluating the association between race and transitions among those who were nondepressed (Wald chi-square test statistic = 3.87; df=2; P=0.02), but was not significant in the model evaluating the association between race and transitions among those who were depressed (Wald chi-square test statistic = 0.20, df=2; P=0.82). Figure 2 provides the odds ratios and 95% confidence intervals from the sex-stratified models. In comparison to white men, black men had a higher likelihood of depression onset (t statistic=2.99; df=1402; P=0.003) and of transitioning from nondepressed to death (t statistic=2.97; df=1402; P=0.003). In contrast, there were no race-related differences in the likelihood of depression onset (t statistic=0.71; df=1464; P=0.48) or in the transition from a nondepressed state to death (t statistic=1.88; df=1464; P=0.06) among women. In both men and women, there were no race differences in the likelihood of recovery from depression or transitioning from depression to death. After rerunning the models using only the data from years 1, 3, 4, 5, and 6, the results were similar. Finally, results from modeling CES-D as a continuous variable indicate that, on average, blacks’ CES-D scores were 0.50 (SE 0.12) points higher than whites’ scores (Chi-square score test statistic 15.76; df=1; P<0.001). Among men, blacks’ average CES-D scores were 0.79 (SE 0.17) points higher than whites’ scores (Chi-square score test statistic 20.2; df=1; P<0.001), whereas there was no race difference in average CES-D scores over time among women (Chi-square score test statistic 2.3; df=1; P=0.14).
Table 2.
Longitudinal Assessment of Transitions Over 10 Years Among Blacks Relative to Whites: Health, Aging, and Body Composition Study.
| Transition | Unadjusted Data | Adjusted Dataa | ||||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | t Statisticb | P-value | Odds Ratio | 95% Confidence Interval | t Statisticb | P-value | |
| Non-depressed | ||||||||
| To non-depressed | 1.00 | Reference | NA | NA | 1.00 | Reference | NA | NA |
| To depressed | 1.48 | 1.30, 1.70 | 5.74 | <0.001 | 1.22 | 1.03, 1.43 | 2.38 | 0.02 |
| To death | 1.48 | 1.27, 1.74 | 4.86 | <0.001 | 1.79 | 1.30, 2.46 | 3.58 | <0.001 |
| Depressed | ||||||||
| To depressed | 1.00 | Reference | NA | NA | 1.00 | Reference | NA | NA |
| To non-depressed | 1.07 | 0.88, 1.30 | 0.72 | 0.47 | 1.14 | 0.90, 1.45 | 1.08 | 0.28 |
| To death | 1.40 | 1.03, 1.90 | 2.15 | 0.03 | 1.62 | 0.89, 2.94 | 1.59 | 0.11 |
Abbreviations: NA, data Not Applicable.
Multinomial logit models that were estimated with Generalized Estimating Equations adjusted for age, sex, education (high school graduate versus did not graduate from high school), socioeconomic status, coronary heart disease, stroke, diabetes, cancer, body mass index, and site.
Transitions from Non-depressed df=2967; Transitions from Depressed df=1220
Figure 2.
Adjusted odds ratios and 95% confidence intervals derived from sex-stratified multinomial logit models, estimated with Generalized Estimating Equations (GEE), that evaluate the association between race (Blacks versus Whites) and the likelihood of the following transitions: Nondepressed to depressed; Nondepressed to death; Referent group, Nondepressed to nondepressed (odds ratio = 1.0); and Depressed to nondepressed; Depressed to death, Referent group, Depressed to depressed (odds ratio = 1.0).
CONCLUSIONS
In this longitudinal study, which included multiple assessments of depressive symptoms in older persons over 10 years, we found that blacks were more likely than whites to experience depression onset over time and to transition from a non-depressed state to death. Yet, race was not associated with recovery from depression, nor was it associated with a transition from a depressed state to death. Sex-stratified analyses revealed that black men may be more likely than white men to transition from a non-depressed state to either a depressed state or to death. Among women, however, race was not associated with depression onset or recovery, nor was it associated with a transition to death from either a nondepressed or depressed state.
It is uncertain if race is differentially associated with depression in older people. Mixed findings regarding the cross-sectional relationship between race and depression contribute to this uncertainty. Whereas major depression has been found to be more prevalent among older whites than blacks (34), some studies report that blacks have a significantly higher number of depressive symptoms than whites, even after controlling for factors such as SES (16, 19). Other studies report the opposite or have found no association (17, 18). At nearly all time points in the present study, we found that a significantly higher percentage of black participants were depressed as compared with white participants. The stability of this finding, over a long period of follow-up, indicates that the burden of experiencing clinically significant depressive symptoms in older persons may be greater for blacks than whites.
The association between race and depression onset offers additional support for a race-related difference in depression in older persons. We found that blacks were 22% more likely to experience depression onset as compared with whites, even after controlling for important confounders such as number of years of education and poverty. Blacks’ increased likelihood of transitioning from a nondepressed to a depressed state may help to explain the previously reported increase in depressive symptoms over time among older blacks (21) and may also help to explain our finding that blacks have higher average CES-D scores over time as compared with whites. In addition, because older blacks, more so than whites, live in areas with lower-quality healthcare (35), neighborhood characteristics may contribute to the race-related difference in depression onset. The moderate to large changes in the CES-D scores regardless of race, however, are indicative of clinically meaningful transitions from a nondepressed to a depressed state.
In contrast, we found that race was not associated with recovery from depression. This finding was somewhat surprising given recent reports that mental health services use and antidepressant use in older persons is lower among blacks than whites (36-38) and that blacks are less likely to initiate or adhere to treatment for mental health conditions (30, 39). Likelihood of recovery, however, is a function of both diagnosis and appropriate treatment. Consequently, it is possible that racial disparities in recovery from depression may have emerged had we been able to distinguish (and control for) participants who had been diagnosed with depression by a clinician and subsequently received treatment from those who were undiagnosed. The lack of a race difference in recovery from depression also challenges prior research indicating a higher likelihood of persistent depression among blacks (40). Only 10% of the sample in this prior study, however, included blacks age 60 and older. Future research is needed to verify our findings and evaluate if race differentially influences the effect of diagnosis and initiation of treatment on recovery from depression in older persons. Furthermore, given that 50% of the depressed participants in this study were depressed during at least two consecutive time points, there is still a substantial need for effective recognition and prevention of depression in older persons regardless of race.
Prior research consistently reports that older women are more likely to experience depression than men (24, 41, 42). The under-representation of blacks in these studies, however, has largely precluded the ability to evaluate whether race is differentially associated with depression onset and recovery in men and women separately. Our sex-specific analyses revealed that black men were 44% more likely to experience depression onset than their white counterparts. The difference in depression onset that we observed by sex was marked, with more than a 5-fold difference in the odds ratio for men as compared with women. Relatedly, we also found that average depression scores over time were significantly higher for blacks than for whites among men, yet race was not associated with CES-D score over time among women. Although we controlled for CHD, stroke, diabetes, cancer, and BMI over the study period, it is possible that race differences in other somatic indicators of health, such as kidney disease or tobacco use, which are over-represented in black men (12, 43), may account for the positive association between race and depression onset in men. More research is needed to confirm our finding that black men have a higher likelihood of experiencing depression onset than white men and to identify potentially modifiable factors that may explain this race difference. Additional research may also help to determine the utility of developing preventative efforts that target and are tailored to black men, thereby ultimately supporting the effort to achieve Healthy People 2020's goals of improving mental health through prevention and treatment and reducing health disparities between minority and non-minority populations (13, 44).
By including mortality as an outcome, we addressed the often overlooked issue of competing risk of death in longitudinal studies of older persons (45) that has been found to influence trajectories of depression in a study of adults age 51 and older (20). Blacks in our study were 79% more likely to transition from a nondepressed state to death than were whites. These findings persisted in men, with black men 89% more likely to transition from nondepressed to death as compared with white men. Blacks were also 62% more likely to transition from a depressed state to death than were whites. Although this latter relationship did not reach statistical significance, these substantial effect sizes further reinforce blacks’ mortality disadvantage. The substantial effect sizes among both the nondepressed and depressed groups also warrant additional research to confirm whether or not depression is akin to conditions like flu and pneumonia which confer no race difference in mortality in late life (46).
Use of data from the Health ABC study, a large, racially-diverse study of community-dwelling older adults with excellent retention, provided a unique opportunity to evaluate race differences in depression over a 10-year period. We used longitudinal methods that enhanced statistical power and accounted for potential correlation among depression scores. Furthermore, we not only controlled for important demographic covariates, such as education and poverty status, but we also controlled for time-varying chronic conditions which also have been found to be associated with both race and depression(47, 48). However, several potential limitations should be acknowledged. All participants were well-functioning at baseline, therefore potentially limiting the generalizability of the findings. We were unable to confirm clinical depression using the CES-D-10. Yet, we used a cut point of ≥8 which has been used previously to indicate clinically significant depressive symptoms (33, 47) that are associated with deleterious health outcomes in older persons (3-6). Because information regarding participants’ depression status before the baseline interview was not available, we could not determine if participants’ first transition from a nondepressed to a depressed state represented incident depression. It is possible that our findings reflect continued race-related patterns of depression established earlier in life. Future studies should evaluate whether race differences in the onset of and recovery from depression during youth and middle age influence depression patterns in older age. Finally, because data on depression was collected at discrete time points, study participants may have experienced additional transitions into and out of depressive states that we could not capture. However, the availability of up to seven waves of follow-up data over 10 years provides the best information, to date, on race-related differences in the onset of and recovery from depression in late life.
Detailed information on the natural history of depression is important to advance efforts in the prevention and treatment of depression in late life. The present research provides new evidence supporting a race difference in the onset of depression, but not recovery, in older persons and further underscores blacks’ mortality disadvantage. We also found evidence to suggest that the relationship between race and depression onset may be stronger in men than in women. Overall, our findings highlight race differences in depression in older persons and reinforce the need for depression prevention strategies. In addition, our findings encourage further research on the course of depression in older blacks, who have historically been under-represented in longitudinal studies of depression in later life.
Acknowledgements
This work was supported in part by the Intramural Research Program of the National Institute on Aging (NIA) contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; the National Institute on Aging at the National Institutes of Health research grants R01-AG028050 and K01-AG-03-1324 (to L.C.B); the National Institute of Nursing research grant R01-NR012459; and National Institute of Mental Health research grant R01-MH086498.
The National Institutes of Health provided funding for research on which this article is based.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: None declared.
This paper was initially presented as a talk at the 2012 Annual Meeting of the Gerontological Society of America.
Contributor Information
Lisa C. Barry, Center on Aging, University of Connecticut, Farmington, Connecticut 06030-5215, US
Roland J. Thorpe, Jr., Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, US
Brenda W.J.H. Penninx, Department of Psychiatry, VU University Medical Center in Amsterdam, The Netherlands
Kristine Yaffe, Department of Psychiatry, University of California, San Francisco, California, US.
Dorothy Wakefield, Center on Aging, University of Connecticut, Farmington, Connecticut, US.
Hilsa N. Ayonayon, Department of Epidemiology and Biostatistics, University of California, San Francisco, California, US
Suzanne Satterfield, Department of Preventive Medicine, University of Tennessee Health Science Center, Memphis, Tennessee, US.
Anne B. Newman, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, US
Eleanor M. Simonsick, Clinical Research Branch, National Institute on Aging, Baltimore, Maryland, US
REFERENCES
- 1.Blazer DG. Depression in late life: review and commentary. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 2.Forlani C, Morri M, Ferrari B, et al. Prevalence and Gender Differences in Late-Life Depression: A Population-Based Study. Am J Geriatr Psychiatry. 2013 doi: 10.1016/j.jagp.2012.08.015. doi: 10.1016/j.jagp.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Geerlings SW, Beekman AT, Deeg DJ, et al. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychol Med. 2001;31:1361–1371. doi: 10.1017/s0033291701004639. [DOI] [PubMed] [Google Scholar]
- 4.Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 5.Meeks TW, Vahia IV, Lavretsky H, et al. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129:126–142. doi: 10.1016/j.jad.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unutzer J, Patrick DL, Marmon T, et al. Depressive symptoms and mortality in a prospective study of 2,558 older adults. Am J Geriatr Psychiatry. 2002;10:521–530. doi: 10.1097/00019442-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Saczynski JS, Beiser A, Seshadri S, et al. Depressive symptoms and risk of dementia: the Framingham Heart Study. Neurology. 2010;75:35–41. doi: 10.1212/WNL.0b013e3181e62138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gracia-Garcia P, de-la-Camara C, Santabarbara J, et al. Depression and Incident Alzheimer Disease: The Impact of Disease Severity. Am J Geriatr Psychiatry. 2013 doi: 10.1016/j.jagp.2013.02.011. doi: 10.1016/j.jagp.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beekman AT, Deeg DJ, Geerlings SW, et al. Emergence and persistence of late life depression: a 3-year follow-up of the Longitudinal Aging Study Amsterdam. J Affect Disord. 2001;65:131–138. doi: 10.1016/s0165-0327(00)00243-3. [DOI] [PubMed] [Google Scholar]
- 10.Beekman ATF, Geerlings SW, Deeg DJH, et al. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatry. 2002;59:605–611. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 11.Harris T, Cook DG, Victor C, et al. Onset and persistence of depression in older people--results from a 2-year community follow-up study. Age Ageing. 2006;35:25–32. doi: 10.1093/ageing/afi216. [DOI] [PubMed] [Google Scholar]
- 12.Older Americans 2012: Key Indicators of Well-Being, Hyattsville, Federal Interagency Forum on Aging-Related Statistics. 2012.
- 13.HHS Action Plan to Reduce Racial and Ethnic Health Disparities. U.S. Department of Health and Human Services; Washington, D.C.: 2011. [Google Scholar]
- 14.Mueller TI, Kohn R, Leventhal N, et al. The course of depression in elderly patients. Am J Geriatr Psychiatry. 2004;12:22–29. [PubMed] [Google Scholar]
- 15.Mackenzie CS, El-Gabalawy R, Chou KL, et al. Prevalence and Predictors of Persistent Versus Remitting Mood, Anxiety, and Substance Disorders in a National Sample of Older Adults. Am J Geriatr Psychiatry. 2013 doi: 10.1016/j.jagp.2013.02.007. doi: 10.1016/j.jagp.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blazer DG, Landerman LR, Hays JC, et al. Symptoms of depression among community-dwelling elderly African-American and white older adults. Psychol Med. 1998;28:1311–1320. doi: 10.1017/s0033291798007648. [DOI] [PubMed] [Google Scholar]
- 17.Cohen CI, Magai C, Yaffee R, et al. Racial differences in syndromal and subsyndromal depression in an older urban population. Psychiatr Serv. 2005;56:1556–1563. doi: 10.1176/appi.ps.56.12.1556. [DOI] [PubMed] [Google Scholar]
- 18.Gallo JJ, Cooper-Patrick L, Lesikar S. Depressive symptoms of whites and African Americans aged 60 years and older. J Gerontol B Psychol Sci Soc Sci. 1998;53:P277–286. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- 19.Jang Y, Borenstein AR, Chiriboga DA, et al. Depressive symptoms among African American and white older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:P313–P319. doi: 10.1093/geronb/60.6.p313. [DOI] [PubMed] [Google Scholar]
- 20.Xiao X, Liang J, Bennett JM, et al. Ethnic differences in the dynamics of depressive symptoms in middle-aged and older Americans. J Aging Health. 2010;22:631–652. doi: 10.1177/0898264310370851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60:P136–142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 22.Beard JR, Cerda M, Blaney S, et al. Neighborhood characteristics and change in depressive symptoms among older residents of New York City. Am J Public Health. 2009;99:1308–1314. doi: 10.2105/AJPH.2007.125104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sutin AR, Terracciano A, Milaneschi Y, et al. The Trajectory of Depressive Symptoms Across the Adult Life Span. JAMA Psychiatry. 2013:1–9. doi: 10.1001/jamapsychiatry.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barry LC, Allore HG, Guo Z, et al. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psychiatry. 2008;65:172–178. doi: 10.1001/archgenpsychiatry.2007.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiske A, Wetherell JL, Gatz M, et al. Depression in older adults. Ann Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dalle Carbonare L, Maggi S, Noale M, et al. Physical disability and depressive symptomatology in an elderly population: a complex relationship. The Italian Longitudinal Study on Aging (ILSA). Am J Geriatr Psychiatry. 2009;17:144–154. doi: 10.1097/jgp.0b013e31818af817. [DOI] [PubMed] [Google Scholar]
- 27.Alexopoulos GS, Katz IR, Bruce ML, et al. Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162:718–724. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shanmugasegaram S, Russell KL, Kovacs AH, et al. Gender and sex differences in prevalence of major depression in coronary artery disease patients: a meta-analysis. Maturitas. 2012;73:305–311. doi: 10.1016/j.maturitas.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klap R, Unroe KT, Unutzer J, et al. Caring for mental illness in the United States: a focus on older adults. Am J Geriatr Psychiatry. 2003;11:517–524. [PubMed] [Google Scholar]
- 30.Kales HC, Nease DE, Jr., Sirey JA, et al. Racial Differences in Adherence to Antidepressant Treatment in Later Life. T Am J Geriatr Psychiatry. 2013 doi: 10.1016/j.jagp.2013.01.046. 10.1016/j.jagp.2013.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann NY Acad Sci. 2000;904:462–473. doi: 10.1111/j.1749-6632.2000.tb06501.x. [DOI] [PubMed] [Google Scholar]
- 32.Thorpe RJ, Jr., Koster A, Kritchevsky SB, et al. Race, socioeconomic resources, and late-life mobility and decline: findings from the Health, Aging, and Body Composition study. J Gerontol A Biol Sci Med Sci. 2011;66:1114–1123. doi: 10.1093/gerona/glr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 34.Byers AL, Yaffe K, Covinsky KE, et al. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67:489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baicker K, Chandra A, Skinner JS, et al. Who you are and where you live: how race and geography affect the treatment of medicare beneficiaries. Health Aff (Millwood) 2004:VAR33–44. doi: 10.1377/hlthaff.var.33. Suppl Variation. [DOI] [PubMed] [Google Scholar]
- 36.Akincigil A, Olfson M, Siegel M, et al. Racial and ethnic disparities in depression care in community-dwelling elderly in the United States. Am J Public Health. 2012;102:319–328. doi: 10.2105/AJPH.2011.300349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neighbors HW, Woodward AT, Bullard KM, et al. Mental health service use among older African Americans: the National Survey of American Life. Am J Geriatr Psychiatry. 2008;16:948–956. doi: 10.1097/JGP.0b013e318187ddd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pickett YR, Greenberg RL, Bazelais KN, et al. Depression Treatment Disparities Among Older Minority Home Healthcare Patients. Am J Geriatr Psychiatry. 2013 doi: 10.1016/j.jagp.2013.01.078. doi: 10.1016/j.jagp.2013.01.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jimenez DE, Cook B, Bartels SJ, et al. Disparities in mental health service use of racial and ethnic minority elderly adults. J Am Geriatr Soc. 2013;61:18–25. doi: 10.1111/jgs.12063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 41.Mulsant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. J Clin Psychiatry. 1999;60(Suppl 20):9–15. [PubMed] [Google Scholar]
- 42.Steffens DC, Skoog I, Norton MC, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Arch Gen Psychiatry. 2000;57:601–607. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- 43.Tarver-Carr ME, Powe NR, Eberhardt MS, et al. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: a population-based study of potential explanatory factors. J Am Soc Nephrol. 2002;13:2363–2370. doi: 10.1097/01.asn.0000026493.18542.6a. [DOI] [PubMed] [Google Scholar]
- 44. [February 12, 2013];Healthy People 2020 Objective Topic Areas and Page Numbers. http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- 45.Berry SD, Ngo L, Samelson EJ, et al. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58:783–787. doi: 10.1111/j.1532-5415.2010.02767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 47.Carnethon MR, Biggs ML, Barzilay JI, et al. Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med. 2007;167:802–807. doi: 10.1001/archinte.167.8.802. [DOI] [PubMed] [Google Scholar]
- 48.Sachs-Ericsson N, Burns AB, Gordon KH, et al. Body mass index and depressive symptoms in older adults: the moderating roles of race, sex, and socioeconomic status. Am J Geriatr Psychiatry. 2007;15:815–825. doi: 10.1097/JGP.0b013e3180a725d6. [DOI] [PubMed] [Google Scholar]