Abstract
Aims
To examine the efficacy of a brief intervention delivered by a therapist (TBI) or a computer (CBI), in preventing cannabis use among adolescents in urban primary care clinics.
Design
A randomized controlled trial comparing: CBI and TBI versus control.
Setting
Urban primary care clinics in the United States.
Participants
Research staff recruited 714 adolescents (ages 12-18) who reported no lifetime cannabis use on a screening survey for this study, which included a baseline survey, randomization (stratified by gender and grade) to conditions (control; CBI; TBI), and 3, 6, and 12 month assessments.
Measurements
Using an intent to treat approach, primary outcomes were cannabis use (any, frequency); secondary outcomes included frequency of other drug use, severity of alcohol use, and frequency of delinquency (among 85% completing follow-ups).
Findings
Compared with controls, CBI participants had significantly lower rates of any cannabis use over 12 months (24.2%, 16.8%, respectively, p<.05), frequency of cannabis use at 3 and 6 months (p<.05) and other drug use at 3 months (p<.01). Compared with controls, TBI participants did not differ in cannabis use or frequency, but had significantly less other drug use at 3 months (p<.05), alcohol use at 6 months (p<.01), and delinquency at 3 months (p<.01).
Conclusions
Among adolescents in urban primary care in the United States, a computer brief intervention appeared to prevent and reduce cannabis use. Both computer and therapist delivered brief interventions appeared to have small effects in reducing other risk behaviors, but these dissipated over time.
Introduction
Although in the U.S. alcohol is the most prevalent substance used by adolescents, cannabis is the most prevalent illicit drug, with rates increasing with age.1 Non-medical use of prescription drugs is the next most commonly reported substance.1 Earlier age of cannabis use increases the risk for other drug use, psychosocial problems (e.g., delinquency), and the development of substance use disorders.2-4
Traditionally, multi-session substance use prevention programs have been delivered in schools, with evidenced-based programs for alcohol, cannabis and illicit drug use.5-12,13 Findings from a meta-analysis suggest that universal programs were more effective for low base rates of use (e.g., tobacco, marijuana) and selective or indicated programs were more effective for high base rates of use (e.g., alcohol).13 School-based prevention programs have limited ability to reach youth who have dropped out of school or attend sporadically.
A visit to a primary care clinic increases the reach of prevention programs and may provide a “teachable moment” for brief interventions (BIs), increasing adolescents’ receptively to interventions.14 In order to reduce health disparities in access to primary care services among socio-economically disadvantaged populations, the U.S. government has established federally-qualified health clinics (FQHCs). BIs encompass principles of harm reduction and motivational interviewing, which may be particularly well-suited for adolescents.14,15
The application of BIs focused on universal prevention among non-using youth is generally lacking. Prior BI research has taken a selective or indicated approach, with meta-analyses demonstrating efficacy.16 For example, among adolescents drinkers in primary care, therapist BIs decrease alcohol misuse.17-21 Among drug users, there are a few promising pilot studies of therapist BIs 18,22-24 and an effective trial in the Czech Republic.21 A prior paper from the study described in this paper showed that among youth using cannabis, a therapist BI reduced driving under the influence of cannabis, but did not affect use.25 A recent study found a universal prevention focused therapist BI for adolescent substance use was not efficacious, despite the fact that content was adapted from a previously demonstrated efficacious selective prevention focused therapist BI.26-28
Using computers for assessment and delivery of universal prevention focused BIs could have a considerable public health impact. Although such studies are lacking among adolescents in primary care, among adolescents in the ED29 and college students,30,31 universal prevention focused, computer delivered alcohol BIs are effective in the short term and/or with at-risk subgroups of participants. A prior manuscript from the study described in this paper examining cannabis users showed that a selective computer BI decreased other drug use and cannabis-related consequences but not cannabis use.25
This paper presents data from a randomized controlled trial (RCT) examining the efficacy of universal prevention focused BIs (therapist or computer delivered) in comparison to a control condition among adolescents (ages 12-18) who had not initiated cannabis use presenting to urban FQHCs. Preliminary outcome variables measured at post-test included perceived risk, self-efficacy, and intention to use. The primary outcome measure was initiation and frequency of cannabis use; the secondary outcome measures were frequency of other drug use, severity of alcohol use, and frequency of delinquency. Hypotheses were that participants in the BIs would report less cannabis, alcohol, other drug use (illicit and non-medical prescription), and delinquency than controls at 3, 6, and 12 month follow-ups.
Method
Design
Project Chill was conducted at seven urban FQHCs in the Midwest (4/2007 – 12/2009). Adolescents (ages 12-18) self-administered a computerized screening survey (with audio). Participants who had not initiated cannabis use were enrolled in the RCT, consisting of a baseline assessment, randomization to one of three conditions (computer BI, therapist BI, or control), and follow-up assessments at 3, 6, and 12 months. Participants reporting past year cannabis use were enrolled in a parallel trial reported on elsewhere.25 The study was approved by the University of Michigan's Institutional Review Board (IRB) for Human Subjects and we obtained a Certificate of Confidentiality.
Procedures
On days containing greater concentration of adolescent appointments, research staff recruited patients in treatment or waiting rooms. A two phase written assent (youth ages 12-17) and/or consent (youth age 18, parents of youth ages 12-17) procedure was used for the screening and RCT. Participants self-administered the 10-minute computer screening survey and received a token $1.00 gift. Initially (April 2007 - July 2008), participants who reported no lifetime cannabis use were eligible for the RCT. In order to increase the proportion of males in the RCT and slow participant accrual, half way through the study (7/ 2008-12/ 2009), 50% of the males and 10% of the females with no prior cannabis use were randomly selected for the RCT, after which time enrollment ended as planned based on funding. Then, youth completed a 25 minute baseline computer survey ($20 remuneration) and provided a urine sample for drug testing ($5). Participants were randomly assigned to conditions by research staff using a computerized algorithm, which was monitored by the project coordinator and data manager to ensure staff could not manipulate assignment. Randomization was stratified by gender (in blocks of 21; 7 per group) and grade (6th – 8th; 9th and up including dropouts). The computerized post-test was administered following the BIs. Research staff contacted youth (e.g., phone call, text, email, or private messaging via social networking sites) to schedule follow-ups, which occurred at primary care offices (85%), homes (7%), other community locations (6%), or by phone (2%). Youth received remuneration of $25, $30, and $35 at each assessment, respectively (and $5 for a urine sample at each follow-up). Follow-up staff was blinded to condition assignment.
Measures
In addition to demographic items [i.e., age, gender, race, ethnicity, grade level (6th – 8th; 9th and up including dropouts), grades in school (mostly A's, A's and B's, Mostly B's, B's and C's, Mostly C's, C's and D's, Mostly D's, D's and F's, Mostly F's)]32-33 validated measures are described below.
Post-test Preliminary Outcomes
Perceived Risk
Two items34 were summed to indicate perceived risk of occasional and regular cannabis use (r = 0.54). Response choices included: No (0), Slight (1), Moderate (2), and Great (3).
Self-efficacy
Confidence in refusing cannabis use in three situations (i.e., party, home alone and feeling sad or bored, hanging out at a friend's house)35 was assessed by summing responses to a 5-point Likert scale [ranging from “not at all sure I could say no” (1) to “completely sure I could say no” (5) (α= 0.86)].
Intention to Use
A single item assessed intention to use cannabis in the next 3 months, with responses ranging from “strongly disagree” (1) to “strongly agree” (4).35
Primary Outcomes
Cannabis
Cannabis (e.g., marijuana, weed, pot) use frequency (past 3 months) was measured using a question from the Add Health study. 32,33 Response choices were: never, 1-2 days, once a month or less, 2-3 days per month, 1-2 days per week, 3-5 days per week, every day or almost every day. Variables included any cannabis use and frequency of use (range 0-6).
Secondary Outcomes
Alcohol
The Alcohol Use Disorder Test (AUDIT-C)36 was used to assess frequency, quantity, and heavy drinking (5 or more)37 in the past 3 months. During piloting, youth indicated that question #1 response options [Never (0), monthly or less (1), 2-4 times a month (2), 2-3 times a week (3), 4 or more times a week(4)] were confusing; thus, we substituted the response options for question 3 [Never (0), less than monthly (1), monthly (2), weekly (3), daily or almost daily (4)]. For quantity, the responses were: (0) none, (1) 1-2, (2) 3-4, (3) 5-6, (4) 7-9, (5) 10 or more. Items were summed to create an alcohol use severity scale (range 0 -13).
Other Drugs
Illicit and non-medical prescription drug use (on your own without a doctor telling you to take them) in the past 3 months was measured using questions from the Add Health study.32,33 Illicit drugs included: inhalants, cocaine, heroin, and other hallucinogens (e.g., ecstasy). Non-medical prescription drugs included: painkillers/opiates (e.g., Codeine); stimulants (e.g., Ritalin); and, sedatives (e.g., Xanax). Response options ranged from 0-6: never, 1-2 days, once a month or less, 2-3 days per month, 1-2 days per week, 3-5 days per week, every day or almost every day. Items were summed to create a frequency of other drug use variable (range 0-42).
Delinquency
Ten items assessing frequency of violent and non-violent delinquency in the past 3 months38 (e.g., physical fighting, stealing, selling drugs) were summed, with responses ranging from 0 to 10 or more times (α = 0.85; range 0-100).
Project Chill BIs
BIs were conducted in a private room and could be paused to allow for medical care. The BIs integrated motivational interviewing (MI) spirit and techniques, 14,15,39 emphasizing personal responsibility, supporting self-efficacy, eliciting commitment talk for avoiding cannabis use and change talk for reducing alcohol, other drugs and delinquency (see Table 1). The BIs also included normative resetting and role play scenarios. Cultural relevance to address the study population (~50% African American) was incorporated into the content based on feedback from focus testing, including providing diversity in language (key messages, scripts for CBI), items listed check boxes (e.g., goals, reasons to avoid using), and scenario topics.
Table 1.
Key Elements of Project CHILL Prevention Interventions.
| Key Elements | Goal of Element | Computer (C) and Therapist (T) Specific Content or Both (B) |
|---|---|---|
| What are we going to do | • Establish rapport • Explain purpose to talk about cannabis use |
C: Virtual therapist; Participant selects Buddy T: Therapist introduction |
| What's Important to You: Goals and Values | • Review and elaborate on goals and values. • Begin to develop discrepancy between goals/values and current behavior by exploring how cannabis use fits in with goals/values. |
B: 3 goals listed C: Summary of goals T: Brief discussion of goals |
| Where Do I Fit In: Normative Feedback | • Compare survey responses for use of cannabis and alcohol to norms for age and gender. • Raise concern by providing feedback about the association between cannabis and other risk behaviors (e.g., alcohol, other drugs) and consequences (e.g., violence, injury, delinquency, arrests). • Explore potential impact of use on goals/values, strengthening commitment talk for avoiding/reducing use. |
B: Gender/age appropriate graphs shown on screen. B: Reviewed in a matter-of-fact, non-judgmental manner. T: Discuss how currently or in the future could impact goals. C: Ask if think affects goals, check response on screen; reflective summary statements provided. C: Pictorial illustrations fading in and out to increase salience during messages. |
| You Decide: Reasons for Avoiding using/Reasons for using | • Elicit reasons to avoid using cannabis. • Explore reasons why other kids use cannabis. • Elicit and affirm commitment talk. • Support self-efficacy for avoiding use. • Support avoiding use by exploring potential impact of use on future goals/values. • Roll with resistance. • Emphasize participant responsibility for making choices. |
B: Reasons for avoiding cannabis use (long list) and reasons for using (short list) presented on screen for participant to check. T: Use MI strategies to make a connection between reasons to avoid these behaviors and goals. C: Summaries of the reasons checked on the screen. Participant checks which of goals could be affected by use, which is summarized. |
| What's Next: 6 Role Plays | • Practice 6 scenarios which were selected by the computer based on gender and risk profile obtained from assessment. • Role plays focus on: refusal skills with low peer pressure, refusal skills with high peer pressure, driving high/drunk or riding with someone high/drunk, delinquency, coping with boredom, refusal skills focusing on consequences of use. |
B: Parallel role play scenarios. T: Options are discussed to provide tools for risky scenarios. C: Animated video situations viewed with Buddy. Decision points where participant chooses the next action. If participants “choose” a negative choice (use), the buddy gives feedback on consequences in relation to goals. Participant chooses a better option, which is then animated. Scenarios show progression in consequences for characters who use and don't use. |
| What we Covered: Summary of session | • Provide participant with summary of goals, behaviors, reasons to stay away from cannabis. • Strengthen commitment to avoid using. • Support self-efficacy. • Review key messages and community resources handout (e.g., mentor, psychological services, leisure activities). • Identify one next step in avoiding cannabis. |
T: Summary to reinforce commitment talk; support/ advice for their “plan”. Review community resources with an emphasis on risk profile. C: Summaries of goals and reasons checked to stay away from cannabis. Review of key prevention messages; encourages review of the community resources handout. |
TBI
Therapists were trained in MI14,15, including use of rulers to increase self-efficacy and commitment talk for abstinence/reduction of other risk behaviors (average length =38 minutes, standard deviation =14). A computer displayed tailored feedback and prompt content. Fidelity was monitored by audio taping and providing feedback via regular individual and group supervision. A random sample of tapes was coded (25.8%, n=61) for Therapist Competence (Global Rating of MI Therapist; GROMIT; 18 items; α=0.94)40 and Content Adherence (15-items, α=0.80; developed for this study) using a 7-point Likert scale (ranging from 1 “Very Poor” to 7 “Expert Mastery”). Mean scores were generally acceptable for the GROMIT, indicating MI spirit and skill (4.95; SD=0.58; range 4-6), and content adherence (3.85; SD=0.40; range 3-6), indicating delivery of sections.
CBI
Using touch screens and headphones for audio, the CBI was an animated, interactive program (average length=33 minutes, standard deviation=13) delivered by a virtual therapist, who provided affirmations and summaries. Guided by a buddy chosen by participants, the role-play scenarios showed characters in risky situations, with progression over time in various consequences, eliciting participant interaction and role modeling positive choices.
Control
Participants in the control (and the BIs) were given a brochure containing warning signs of problems with cannabis and community resources (e.g., substance use, mental health, and leisure activities).
Data analysis
SAS Version 9.2 was used for analyses. Descriptive data is presented regarding enrollment and baseline characteristics by condition assignment; bivariate analyses were conducted to examine equivalence of groups at baseline (chi-square; t-tests). Preliminary outcome analyses examined within condition (TBI, CBI) changes from baseline to posttest on perceived risk, self-efficacy, and intentions (using paired Wilcoxon signed rank test due to skewed variable distributions).
Study aims were to prevent or delay initiation of cannabis use and reduce the extent of involvement with cannabis use, alcohol use, other drug use, and delinquency. Although 97% received their assigned condition, an intent to treat approach was used (e.g., all randomized participants included regardless of whether condition was received). Participants missing at follow-up are not included in analyses; however, follow-up rates exceeded 85% for all conditions over time and attrition analyses showed that baseline variables were not significantly related to follow-up completion, suggesting the data was missing at random. First, the percentage point difference for any cannabis use was compared by conditions (TBI, CBI) versus control at each time pint (3, 6, 12) as well as cumulatively, over 12 months using Fishers Exact Test (with 95% confidence intervals). Second, regression analyses (i.e., negative binominal or Poisson models based on distribution) were conducted to predict continuous primary (cannabis use frequency) and secondary (i.e., other drug use frequency, alcohol use severity, and delinquency frequency) outcomes at 3, 6, and 12 months. Independent variables included baseline levels of the variable examined and condition (TBI vs. control, CBI vs. control). The study was not powered to detect differences between BIs. Third, for conservative purposes, we repeated the regression analyses described above, controlling for baseline variables: gender, grade level (6th – 8th; 9th and up including dropouts), Hispanic ethnicity, race (African-American vs. other), and failing grades (D and below or dropped out). Age was not included as it was correlated 0.91 with grade level.
To achieve 80% power, n=199 per group were needed to detect a 10% difference in outcomes. Cohen's effect sizes38 were calculated for significant effects. Effect sizes of d=0.10 are considered clinically meaningful in prevention literature.42
Results
Participants
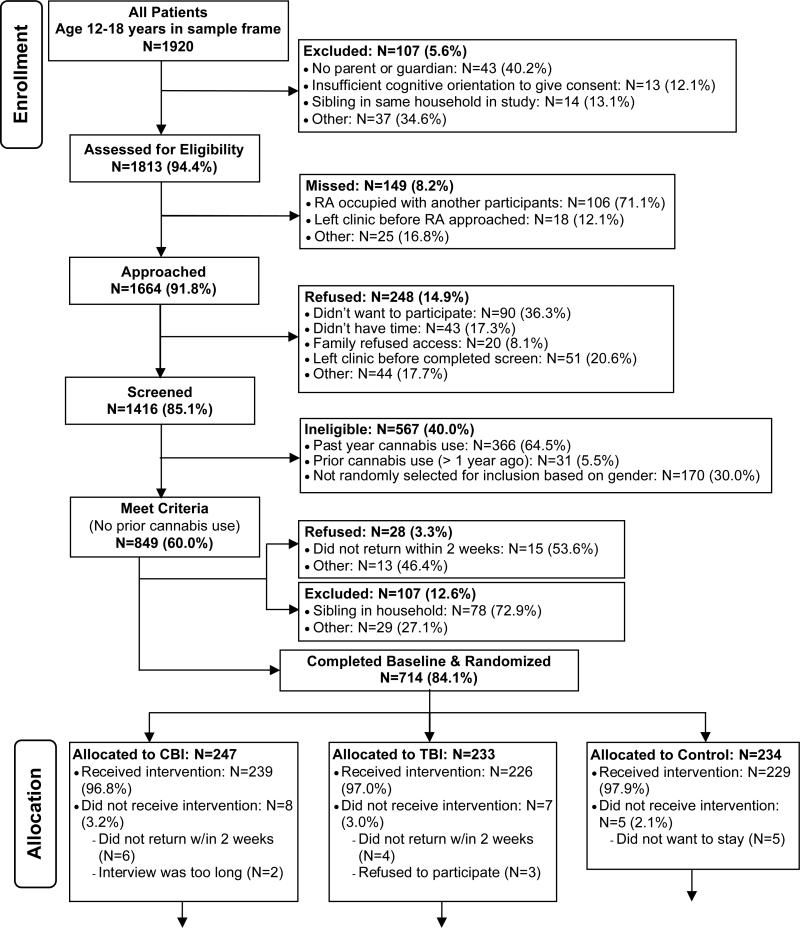
Overall, 1416 youth were screened (Figure 1). Males were more likely to refuse participation in the screening than females (18.0% and 12.9%, respectively; χ2(1) =8.18, p<.05). Also, Caucasians were more likely to refuse than African-Americans and other races (21.9%, 12.8%, and 15.6%, respectively; χ2(2) =14.72 , p<.001).
Figure 1.
Study Enrollment
Among those screened, 714 reported no prior cannabis use, completed the baseline, and were enrolled in the RCT. Although no gender differences were observed for participation in the baseline (3.6% male, 3.7% female; χ2(1) =0.0157, p>0.05), Caucasians were more likely to refuse than African-Americans and other races (6.0%, 3.9%, 1.3%, respectively; χ2(2)=6.86 and p<.05). No other information could be gathered on those who refused without written informed consent. Baseline characteristics were examined for equivalence by condition; age and grade level were significantly different by condition assignment (Table 2). Note that participants reporting past year cannabis use (n=366; see Walton et al., 2013) or cannabis use that occurred greater than 1 year ago (n=31) were excluded from the prevention study.
Table 2.
Baseline Demographic and Substance Use Characteristics by Condition.
| Background Characteristics | Total n= 714 | TBI n=233 | CBI n=247 | Control n=234 |
|---|---|---|---|---|
| % / M (SD) | % / M (SD) | % / M (SD) | % / M (SD) | |
| Demographics | ||||
| Male | 43.0% | 45.5% | 44.5% | 38.9% |
| African-American Race | 63.7% | 64.0% | 62.4% | 65.0% |
| Hispanic ethnicity | 9.2% | 10.8% | 7.0% | 9.8% |
| Age* | 14.9 (1.9) | 15.2 (1.8) | 14.7 (1.9) | 14.9 (2.1) |
| Grade Level 6-8* | 36.5% | 30.1% | 40.1% | 39.3% |
| Failing grades | 17.1% | 14.6% | 16.6% | 20.1% |
| Drug Use Behaviors | ||||
| Other Illegal Drug Use (ever) | 6.9% | 7.7% | 7.3% | 5.6% |
| Frequency | 0.2 (1.0) | 0.2 (1.0) | 0.2 (0.8) | 0.2 (1.1) |
| Alcohol Use (ever) | 12.0% | 12.0% | 10.5% | 13.7% |
| Frequency | 0.2 (0.5) | 0.2 (0.5) | 0.2 (0.6) | 0.2 (0.5) |
| Delinquency (any) | 47.5% | 51.5% | 47.4% | 43.6% |
| Frequency | 1.9 (4.3) | 1.9 (3.5) | 2.0 (4.9) | 1.8 (4.3) |
p ≤0.05
Note: CBI=Computer Brief Intervention; TBI=Therapist Brief Intervention; M=Mean; SD=Standard Deviation
Note the following variables definitions: 1) Race = African-American vs. other; 2) Grade Level = 6th - 8th; 9th and up including dropouts; and 3) Failing grades = D's and below or dropped out.
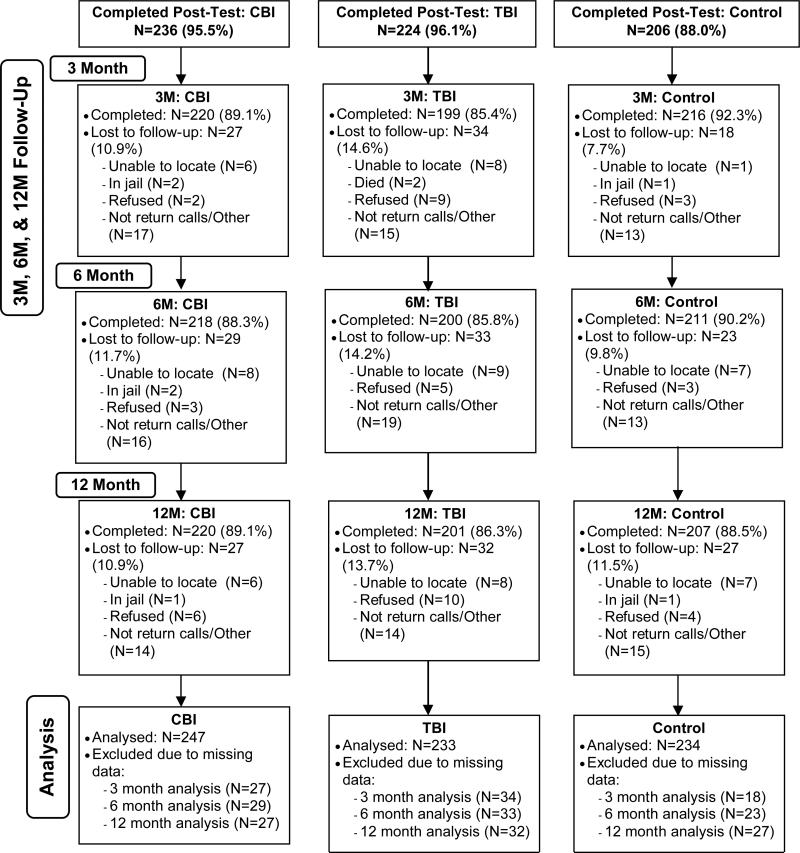
Most youth (93.4%; 667/714) completed their condition immediately or within two weeks (n= 24); youth who did not receive their BI (n=23) were included in follow-ups. Follow-up rates exceeded 85% at 3, 6, and 12-months. Chi-square analyses comparing attrition rates by group showed no evidence of differential drop-out by condition at 6 or 12 months (p values >.05). At 3-months, the TBI group had significantly lower follow-up rates than the control (85.4% vs. 92.3%; X2(1)=5.61, p<.05); attrition did not differ at 3 months for the CBI vs. control. Comparisons of those completing follow-ups at 3, 6 and 12 months with those who did not complete follow-ups were not significant for variables shown in Table 1.
Concordance between past 3 month self-report and urine drug screen for cannabis was excellent at baseline (99.4%). At 3, 6, and 12 months, agreement remained high (99.0%); thus, self-report was used for analyses.
Preliminary Outcomes
At post-test, significant increases were noted in perceived risk (for the CBI but not TBI) and in self-efficacy (for the CBI and TBI). No significant changes were found for behavioral intentions, likely because at baseline most adolescents reported “strongly disagree” for intention to use.
Primary and Secondary Outcomes
Cannabis Use
Table 4 shows the point prevalence of any cannabis use by condition over time. For the CBI, although the point prevalence did not differ at each time point, the cumulative prevalence over 12 months was significantly lower in the CBI as compared to the control. The point prevalence of cannabis use did not differ for the TBI versus the control.
Table 4.
Efficacy of CBI and TBI (vs. Control) on Any Cannabis Use Over Time.
| Outcome | CBI % (n) | Control % (n) | Percentage-Point Difference (95% CI) | Relative Rate (95% CI) |
|---|---|---|---|---|
| Point prevalence at 3 months | 5.00 (11)a | 7.87 (17)i | −2.87 (−7.47-1.73) | 0.64 (0.30-1.32) |
| Point prevalence at 6 months | 5.96 (13)b | 9.01 (19)j | −3.05 (−8.02-1.94) | 0.66 (0.34-1.31) |
| Point prevalence at 12 months | 10.91 (24)c | 14.01 (29)k | −3.10 (−9.37-3.17) | 0.78 (0.47-1.29) |
| Any use over 12 months | 16.82 (37)d | 24.16 (50)l | −7.34 (−14.98-0.00)* | 0.70 (0.48-1.00) |
| Outcome | TBI % (n) | Control % (n) | Percentage-Point Difference (95% CI) | Relative Rate (95% CI) |
|---|---|---|---|---|
| Point prevalence at 3 months | 6.53 (13)e | 7.87 (17)i | −1.34 (−6.31-3.63) | 0.83 (0.42-1.66) |
| Point prevalence at 6 months | 9.00 (18)f | 9.00 (19)j | 0.00 (−5.54-5.54) | 1.00 (0.54-1.85) |
| Point prevalence at 12 months | 10.95 (22)g | 14.01 (29)k | −3.06 (−9.46-3.34) | 0.78 (0.46-1.31) |
| Any use over 12 months | 20.90 (42)h | 24.16 (50)l | −3.26 (−11.36-4.84) | 0.87 (0.60-1.24) |
Note: The relative rate is the percentage in the BI group divided by control group. Use rates were calculated by participants who used cannabis among those completing follow-up. CBI=Computer Brief Intervention; TBI=Therapist Brief Intervention. CI=Confidence Interval.
220
218
220
220
199
200
201
201.
216
211
207
207
p<.05
Frequency Outcomes: Cannabis, Other drugs, Alcohol, Delinquency
Models are presented that do not control for demographics (Table 5). As compared to controls, participants in the CBI showed significantly less cannabis use at 3 and 6 months (d = 0.12, 0.14, respectively) and other drug use at 3 months (d= 0.09); the CBI did not affect alcohol use or delinquency (Table 5). Although participants in the TBI did not significantly differ from controls in cannabis use, participants in the TBI showed significantly less other drug use at 3 months (d= 0.03), delinquency at 3 months (d= 0.36), and alcohol use at 6 months (d= 0.14) as compared to controls. No significant effects were observed at 12 months.
Table 5.
Regression Analyses: Efficacy of TBI and CBI (vs. Control) on Extent of Substance Use and Delinquency Over Time.
| Variable | 3Ma IRR (95%CI) | 6Mb IRR (95%CI) | 12Mc IRR (95%CI) |
|---|---|---|---|
| Cannabis Use Frequency | |||
| Computer | 0.55 (0.30,0.99)* | 0.56 (0.34,0.91)* | 0.89 (0.60,1.31) |
| Therapist | 0.92 (0.55,1.54) | 0.65 (0.41,1.04) | 0.90 (0.61,1.33) |
| Other Drug Use Frequency | |||
| Baseline Other Drug Use | 1.20 (1.09,1.32)*** | 1.20 (1.09,1.32)*** | 1.42 (1.31,1.53)** |
| Computer | 0.48 (0.29,0.79)** | 0.94 (0.60,1.48) | 0.75 (0.38,1.49) |
| Therapist | 0.52 (0.31,0.87)* | 0.61 (0.36,1.04) | 0.86 (0.39,1.92) |
| Alcohol Use Severity | |||
| Baseline Alcohol Use | 3.00 (2.15,4.19)*** | 2.27 (1.73,2.99)*** | 2.32 (1.73,3.11)*** |
| Computer | 0.86 (0.48,1.55) | 0.63 (0.39,1.01) | 0.82 (0.50,1.34) |
| Therapist | 1.23 (0.70,2.18) | 0.52 (0.32,0.85)** | 0.69 (0.42,1.34) |
| Delinquency Frequency | |||
| Baseline Delinquency | 1.25 (1.17,1.32)*** | 1.23 (1.14,1.33)*** | 1.19 (1.12,1.26)*** |
| Computer | 0.91 (0.63,1.33) | 1.15 (0.72,1.84) | 0.88 (0.55,1.41) |
| Therapist | 0.54 (0.36,0.80)** | 0.92 (0.58,1.48) | 0.98 (0.61,1.57) |
Note: 3M=3 Month follow-up; 6M=6 Month follow-up; 12M=12 Month follow-up; TBI= Therapist Brief Intervention; CBI=Computer Brief Intervention; IRR= Incident Rate Ratio; CI=Confidence Interval. IRR values >1.0 indicate variables positively associated with the outcome variable and values <1.0 indicate variables negatively associated with the outcome variable. Effect Sizes: 1) Cannabis Use: CBI = 0.12 (3M) and 0.14 (6M); 2) Other Drug Use: CBI = 0.09 (3M); 3) Alcohol Use: TBI = 0.14 (3M); and 4) Delinquency: TBI =0.36 (3M).
n=635
n=629
n=628.
p < 0.05
p < 0.01
p < 0.001.
Additional models controlled for demographics (i.e., gender, grade level, race, failing grades, ethnicity; Table 6). Findings for the CBI were identical as reported above. Findings for the TBI were similar, with the exception that the efficacy of the TBI on other drug use was not significant. Regarding demographics, in general, cannabis use, other drug use, and delinquency was positively related to male gender, high school grade level or dropping out, African-American race, and failing grades. Alcohol use was significantly related to high school grade level or dropping out. African-American race was positively associated with marijuana use and delinquency whereas Other race was positively associated with other drug use and alcohol use.
Table 6.
Regression Analyses: Efficacy of TBI and CBI (vs. Control) on Extent of Substance Use and Delinquency Over Time: Controlling for Baseline Characteristics.
| Variable | 3Ma IRR (95%CI) | 6Mb IRR (95%CI) | 12Mc IRR (95%CI) |
|---|---|---|---|
| Cannabis Use Frequency | |||
| Computer | 0.53 (0.29, 0.95)* | 0.61 (0.37, 0.99)* | 0.86 (0.58, 1.27) |
| Therapist | 0.84 (0.49, 1.42) | 0.66 (0.41, 1.06) | 0.94 (0.21, 4.18) |
| Gender | 1.60 (1.00, 2.56) | 1.63 (1.08, 2.46) | 1.07 (0.77, 1.50) |
| Education | 0.86 (0.53, 1.40) | 0.41 (0.25, 0.67) | 0.58 (0.40, 0.85) |
| Race Group | 2.61 (1.04, 6.56)* | 4.85 (1.75, 13.45) | 1.75 (0.97, 3.15) |
| Failing Grade | 0.44 (0.27, 0.73)** | 0.30 (0.20, 0.45) | 0.61 (0.42, 0.88) |
| Ethnicity | 1.05 (0.35, 3.15) | 1.43 (0.67, 3.08) | 1.03 (0.57, 1.86) |
| Other Drug Use Frequency | |||
| Baseline Other Drug Use | 1.26 (1.14, 1.39)*** | 1.23 (1.12, 1.36)*** | 1.32 (1.20, 1.46)*** |
| Computer | 0.52 (0.31, 0.86)* | 0.97 (0.61, 1.55) | 0.78 (0.38, 1.58) |
| Therapist | 0.65 (0.39, 1.08) | 0.63 (0.37, 1.07) | 0.90 (0.39, 2.04) |
| Gender | 0.23 (0.14, 0.41)*** | 1.13 (0.73, 1.74) | 1.27 (0.69, 2.33) |
| Education | 2.56 (1.66, 3.94)*** | 1.93 (1.19-3.16)* | 1.92 (1.02, 3.59)* |
| Race Group | 0.32 (0.19, 0.54)*** | 0.40 (0.24, 0.66)*** | 0.86 (0.30, 2.48) |
| Failing Grade | 0.41 (0.26, 0.66)*** | 0.36 (0.23, 0.55)*** | 0.74 (0.31, 1.79) |
| Ethnicity | 0.73 (0.37, 1.41) | 0.64 (0.31, 1.32) | 0.70 (0.23, 2.20) |
| Alcohol Use Severity | |||
| Baseline Alcohol Use | 3.06 (2.15, 4.36)*** | 2.05 (1.59, 2.65)*** | 2.20 (1.67, 2.90)*** |
| Computer | 0.93 (0.52, 1.68) | 0.66 (0.42, 1.04) | 1.22 (0.75, 1.99) |
| Therapist | 1.38 (0.78, 2.43) | 0.57 (0.36, 0.91)* | 1.36 (0.84, 2.23) |
| Gender | 0.84 (0.51, 1.36) | 0.90 (0.61, 1.34) | 0.78 (0.52, 1.18) |
| Education | 0.97 (0.58, 1.62) | 0.53 (0.34, 0.84)** | 0.46 (0.28, 0.76)** |
| Race Group | 0.76 (0.40, 1.44) | 0.47 (0.29, 0.76)** | 0.75 (0.43, 1.30) |
| Failing Grade | 0.58 (0.33, 1.02) | 0.73 (0.47, 1.15) | 0.94 (0.55, 1.60) |
| Ethnicity | 1.75 (0.74, 4.15) | 1.80 (0.96, 3.38) | 1.57 (0.77, 3.18) |
| Delinquency Frequency | |||
| Baseline Delinquency | 1.20 (1.13, 1.27)*** | 1.21 (1.12, 1.31)*** | 1.13 (1.06, 1.20)*** |
| Computer | 0.90 (0.62, 1.31) | 0.94 (0.60, 1.48) | 0.85 (0.53, 1.36) |
| Therapist | 0.53 (0.36, 0.79)** | 0.81 (0.51, 1.30) | 1.03 (0.64, 1.65) |
| Gender | 1.46 (1.07, 2.00)* | 1.55 (1.07, 2.25)* | 1.84 (1.24, 2.72)** |
| Education | 1.75 (1.28, 2.40)** | 0.92 (0.62, 1.37) | 1.49 (1.01, 2.21)* |
| Race Group | 1.86 (1.10, 3.16)* | 0.76 (0.44, 1.31) | 0.99 (0.55, 1.78) |
| Failing Grade | 0.83 (0.56, 1.22) | 0.74 (0.46, 1.19) | 0.60 (0.36, 1.00)* |
| Ethnicity | 1.19 (0.67, 2.09) | 1.34 (0.66, 2.71) | 1.05 (0.48, 2.30) |
Note: 3M=3 Month follow-up; 6M=6 Month follow-up; 12M=12 Month follow-up; TBI= Therapist Brief Intervention; CBI=Computer Brief Intervention; IRR= Incident Rate Ratio; CI=Confidence Interval. IRR values >1.0 indicate variables positively associated with the outcome variable and values <1.0 indicate variables negatively associated with the outcome variable.
p<0.05
p<0.01
p<0.001
n=635
n=629
n=628.
Discussion
To our knowledge, this study is the first to use a universal prevention approach to examine the potential efficacy of BIs among adolescents in primary care who have yet to initiate cannabis use. Reflecting the increased use and subsequent salience of technology among adolescents, the CBI was efficacious in preventing cannabis use and reducing involvement with cannabis and other drugs, with small but clinically meaningful effect sizes (0.12-0.14). Given demands placed upon medical staff, using computers for delivery of BIs could facilitate translation into routine practice at FQHCs. The TBI was efficacious in attenuating risk behaviors associated with cannabis use in the short term, namely alcohol, other drug use, and delinquency, with effect sizes ranging from 0.11 to 0.36; however, the TBI did not prevent cannabis use. These findings are consistent with a prior paper from this study among cannabis users, which showed greater evidence for the CBI than the TBI.25 Conclusions regarding BIs efficacy vary based on substance, problem severity, setting, and delivery mechanism. For example, a universal prevention focused, computerized, alcohol BI among college freshman showed greater effects for non-drinkers than low risk drinkers;30 however, other studies have found greater effects for selective or indicated prevention samples (substance users) than universal prevention samples. 43 Further, a recent review concluded TBIs were more effective than CBIs among college students who misused alcohol.44
Variation in BI content may also explain differences in findings across studies. Although our BIs were conceptualized to have parallel content, in practice the delivery mechanism affected the content. Therapists were given autonomy to focus the TBI based on participant interaction; thus, the therapist may have placed greater emphasis on risk behaviors other than cannabis (e.g., half of the youth reported a least one act of delinquency) while the CBI more consistently focused on cannabis use. In contrast, although tailored, the CBI the content was set apriori, with greater emphasis on cannabis and the connection to other risk behaviors, which was reflected in significant increases at post-test in ratings of perceived risk. Alternatively, although both BI's aimed to increase self-efficacy and commitment talk for abstinence by presenting hypothetical risk situations, the TBI was presented in discussion format whereas the CBI included interactive videos modeling how youth could handle risk situations to avoid potential consequences (e.g., health, social, legal).
Future studies are needed to delineate the essential elements of computer and therapist BIs addressing universal substance use prevention among adolescents. For instance, decisional balance exercises are associated with poorer outcomes in one review and better outcomes in another, 44,45 perhaps reflecting differences in therapist skills than specific content. Identification of therapist behaviors that are associated with worse outcomes is another important area of future research, with review studies suggesting simple reflections and directiveness are counterproductive45,46 among substance using samples. In our study, it is unknown whether such behaviors occurred in the TBI; whereas the CBI was programmed so that it did not include such behaviors.
Although findings for this study showed short-term benefits of BIs, consistent with conclusions from reviews regarding the efficacy of motivational interviewing based BIs, 47 effects were generally not sustained. Given that the American Medical Association (AMA) recommends that adolescents be asked at least annually about substance use48, additional boosters could be delivered during subsequent visits. In order to optimize effects, a multi-modal approach could be utilized in which the computer program could be initially provided for universal prevention, followed by therapist BIs to further explore changes in risk behaviors over time.
Limitations
Several study limitations require attention. Self-report data were collected, which may be prone to response bias. To increase the accuracy of self-report, we included a urine drug screen (with excellent concordance), participants’ self-administered data on computers, and follow-up staff were “blinded” to condition assignment.49,50 Although regular supervision was provided and a computer was used to prompt section content for therapists, a challenge inherent to delivery of TBIs is fidelity. Although follow-up rates were excellent (>85%), substance use among those not completing follow-ups was unknown; thus, analyses were limited to those completing follow-ups. Also, higher rates of attrition in the TBI at 3 months could have affected findings. Replication is required to determine generalizability to other samples (e.g., Hispanics) and settings.
Conclusions
From a public health standpoint, findings from this universal prevention study suggest that a computer BI may be particularly promising in deterring the use of cannabis and other drug in the short term. Findings for a therapist BI were mixed, with no effects on cannabis use but short term effects on other risk behaviors. Future studies are needed to identify critical components of BIs, including the optimal combination of therapist and computer BIs and timing of delivery of boosters at subsequent visits.
Table 3.
Within Condition (TBI, CBI) Changes in Perceived Risk, Self-efficacy, and Intention to Use.
| Variable | TBI (n=236) | CBI (n=247) |
|---|---|---|
| Perceived Risk | ||
| Baseline Mean (SD) | 2.21 (0.97) | 2.33 (0.90) |
| Post-Test Mean (SD) | 2.24 (0.90) | 2.54 (0.72) |
| Difference in Mean (SD) | 0.03 (0.85) | 0.21 (0.74) |
| % Change in Mean | 1.4% | 9.0%*** |
| Self-Efficacy | ||
| Baseline Mean (SD) | 3.82 (1.59) | 3.91 (1.51) |
| Post-Test Mean (SD) | 4.17 (1.47) | 4.36 (1.28) |
| Difference in Mean | 0.43 (1.32) | 0.49 (1.32) |
| % Change in Mean | 9.2%*** | 11.5%*** |
| Intention to Use | ||
| Baseline Mean (SD) | 1.21 (0.49) | 1.23 (0.55) |
| Post-Test Mean (SD) | 1.20 (0.55) | 1.23 (0.55) |
| Difference in Mean | 0.01 (0.59) | 0.01 (0.65) |
| % Change in Mean | 0.8% | 0.8% |
p≤0.001.
Note: n shown is for baseline; 3 TBI participants did not complete the post-test and 3 CBI participants did not complete the post-test.
Acknowledgements
This project was funded by a grant (#DA020075) from the National Institute on Drug Abuse (NIDA). We would like to thank project staff as well as the patients and medical staff at Hamilton Community Health Centers and Health Delivery Inc., and Mott Children's Health Center for their support of this project.
Footnotes
Declarations of Interest: None.
References
- 1.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2011. Volume I: Secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan. 2012 [Google Scholar]
- 2.Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry. 2002;59(11):1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- 3.Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, et al. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289(4):427–33. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 4.McCabe SE, West BT, Cranford JA, Ross-Durow P, Young A, Teter CJ, et al. Medical misuse of controlled medications among adolescents. Arch Pediatr Adolesc Med. 2011;165(8):729–35. doi: 10.1001/archpediatrics.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tobler NS, Stratton HH. Effectiveness of school-based drug prevention programs: A meta-analysis of the research. J Prim Prev. 1997;18(1):71–128. [Google Scholar]
- 6.D'Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, Green JHD. Preventing alcohol use with a voluntary after-school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prev Sci. 2012;13(4):415–25. doi: 10.1007/s11121-011-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hecht ML, Marsiglia FF, Elek E, Wagstaff DA, Kulis S, Dustman P, et al. Culturally grounded substance use prevention: An evaluation of the keepin' it R.E.A.L. curriculum. Prev Sci. 2003;4(4):233–48. doi: 10.1023/a:1026016131401. [DOI] [PubMed] [Google Scholar]
- 8.Catalano RF, Berglund ML, Ryan JAM, Lonczak HS, Hawkins JD. Positive youth development in the United States: Research findings on evaluations of positive youth development programs. Prevention & Treatment. 2002;5:1–111. [Google Scholar]
- 9.Hanley S, Ringwalt C, Ennett ST, Vincus AA, Bowling JM, Haws SW, et al. The prevalence of evidence-based substance use prevention curricula in the nation's elementary schools. J Drug Educ. 2010;40(1):51–60. doi: 10.2190/DE.40.1.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Arch Gen Psychiatry. 2010;67(1):85–93. doi: 10.1001/archgenpsychiatry.2009.173. [DOI] [PubMed] [Google Scholar]
- 11.Sussman S, Sun P, Rohrbach LA, Spruijt-Metz D. One-year outcomes of a drug abuse prevention program for older teens and emerging adults: Evaluating a motivational interviewing booster component. Health Psychol. 2012;31(4):476–85. doi: 10.1037/a0025756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faggiano F, Vigna-Taglianti F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school-based substance abuse prevention program: 18-Month follow-up of the EU-Dap cluster randomized controlled trial. Drug Alc Dep. 2010;108:56–64. doi: 10.1016/j.drugalcdep.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 13.Shamblen SR, Derzon JH. A preliminary study of the population-adjusted effectiveness of substance abuse prevention programming: Towards making IOM program types comparable. J Prim Prev. 2009;30:89–107. doi: 10.1007/s10935-009-0168-x. [DOI] [PubMed] [Google Scholar]
- 14.Monti PM, Barnett NP, Colby SM, O'Leary TA. Motivational enhancement of alcohol-involved adolescents. In: Monti PM, Colby SM, O'Leary TA, editors. Adolescents, alcohol and substance abuse: Reaching teens through brief interventions. The Guilford Press; New York, NY: 2001. pp. 145–82. [Google Scholar]
- 15.Miller WR, Rollnick S. Motivational interviewing, third edition: Helping people for change (applications of motivational interviewing) The Guilford Press; New York, NY: 2012. [Google Scholar]
- 16.Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting & Clinical Psychology. 2011;79(4):433–40. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- 17.Bertholet N, Daeppen JB, Weitlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief intervention in primary care. Arch Intern Med. 2005;165:986–95. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 18.Mason M, Pate P, Drapkin M, Sozinho K. Motivational interviewing integrated with social network counseling for female adolescents: A randomized pilot study in urban primary care. J Subst Abuse Treat. 2011;41:148–55. doi: 10.1016/j.jsat.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Millstein SG, Marcell AV. Screening and counseling for adolescent alcohol use among primary care physicians in the United States. Pediatrics. 2003;111:114–25. doi: 10.1542/peds.111.1.114. [DOI] [PubMed] [Google Scholar]
- 20.Ozer EJ, Tschann JM, Pasch LA, Flores E. Violence perpetration across peer and partner relationships: Co-occurrence and longitudinal patterns among adolescents. J Adolesc Health. 2004 Jan;34(1):64–71. doi: 10.1016/j.jadohealth.2002.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Harris SK, Csémy L, Sherritt L, Starostova O, Van Hook S, Johnson J, et al. Computer-facilitated substance use screening and brief advice for teens in primary care: An international trial. Pediatrics. 2012;129(6):1–12. doi: 10.1542/peds.2011-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haller D, Meynard A, Lefebvre D, Tylee A, Narring F, Broers B. Brief intervention addressing excessive cannabis use in young people consulting their GP: A pilot study. Br J Gen Pract. 2009;59:166–72. doi: 10.3399/bjgp09X419529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knight JR, Sherritt L, Van Hook S, Gates EC, Levy S, Chang G. Motivational interviewing for adolescent substance use: A pilot study. J Adolesc Health. 2005;37(2):167–9. doi: 10.1016/j.jadohealth.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 24.D'Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. J Subst Abuse Treat. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 25.Walton MA, Bohnert K, Resko S, Barry KT, Chermack ST, Zucker RA, et al. Computer and Therapist Based Brief Interventions among Cannabis-using Adolescents presenting to Primary Care: One Year Outcomes. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2013.04.020. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCambridge J, Strang J. Development of a structured generic drug intervention model for public health purposes: a brief application of motivational interviewing with young people. Drug and alcohol review. 2003;22(4):391–9. doi: 10.1080/09595230310001613903. [DOI] [PubMed] [Google Scholar]
- 27.McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- 28.McCambridge J, Strang J. Deterioration over time in effect of Motivational Interviewing in reducing drug consumption and related risk among young people. Addiction. 2005;100(4):470–8. doi: 10.1111/j.1360-0443.2005.01013.x. [DOI] [PubMed] [Google Scholar]
- 29.Maio RF, Shope JT, Blow FC, Gregor MA, Zakrajsek JS, Weber JE, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med. 2005;45(4):420–9. doi: 10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 30.Bingham CR, Barretto AI, Walton MA, Bryant CM, Shope JT, Raghunathan TE. Efficacy of a web-based, tailored, alcohol prevention/intervention program for college students: 3 month follow-up. J Drug Educ. 2011;41(4):405–30. doi: 10.2190/DE.41.4.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kypri K, Langley JD, Saunders JB, Cashell-Smith ML, Herbison P. Randomized controlled trial of web-based alcohol screening and brief intervention in primary care. Arch Intern Med. 2008;168(5):530–6. doi: 10.1001/archinternmed.2007.109. [DOI] [PubMed] [Google Scholar]
- 32.Sieving RE, Beuhring T, Resnick MD, Bearinger LH, Shew M, Ireland M, et al. Development of adolescent self-report measures from the National Longitudinal Study of Adolescent Health. J Adolesc Health. 2001;28(1):73–81. doi: 10.1016/s1054-139x(00)00155-5. [DOI] [PubMed] [Google Scholar]
- 33.Harris K, Florey F, Tabor J, Bearman P, Jones J, Udry J. The national longitudinal study of adolescent health: Research design. Add Health. 2003 http://www.cpc.unc.edu/projects/addhealth/design.
- 34.Johnston LD, O'Malley PM, Bachman PM, Schulenberg JE. Monitoring the Future: National Results on Adolescent Drug Use: Overview of key findings, 2003. National Institute on Drug Abuse; Bethesda, MD: 2004. Report No. NIH Publication No. 04-5506. [Google Scholar]
- 35.Ellickson PL, Bell RM. Prospects for preventing drug use among young adolescents. The RAND Corporation; Santa Monica, CA: 1990. [Google Scholar]
- 36.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 37.Chung T, Colby SM, Barnett NP, Monti PM. Alcohol use disorders identification test: factor structure in an adolescent emergency department sample. Alcohol Clin Exp Res. 2002;26(2):223–31. [PubMed] [Google Scholar]
- 38.Zimmerman MA, Ramirez-Valles J, Zapert KM, Maton KI. A longitudinal study of stress-buffering effects for urban African American male adolescent problem behaviors and mental health. J Community Psychol. 2000;28(1):17–33. [Google Scholar]
- 39.Baer JS, Peterson PL. Adolescents and young adults. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people for change. Second edition Guilford Press; New York, NY: 2002. pp. 320–32. [Google Scholar]
- 40.Moyers TB. The Global Rating of Motivational Interviewing Therapists. Center on Alcoholism, Substance Use, and Addictions. 2004 http://casaa.unm.edu/download/GROMIT.pdf.
- 41.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. Academic Press; San Diego, CA: 1985. [Google Scholar]
- 42.Gottfredson DC, Wilson DB. Characteristics of effective school-based substance abuse prevention. Prev Sci. 2003;4(1):27–38. doi: 10.1023/a:1021782710278. [DOI] [PubMed] [Google Scholar]
- 43.McCambridge J, Hunt C, Jenkins RJ, Strang J. Cluster randomised trial of the effectiveness of motivational interviewing for universal prevention. Drug Alc Dep. 2011;114:177–84. doi: 10.1016/j.drugalcdep.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 44.Carey KB, Scott-Sheldon LAJ, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review. 2012;32(8):690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2008;104:705–15. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tollison SJ, Mastroleo NR, Witkiewitz K, Lee CM, Ray AE, Larimer ME. The relationship between baseline drinking status, peer motivational interviewing microskills, and drinking outcomes in a brief alcohol intervention for matriculation college students: A replication. Behav Ther. 2013;44(137-151) doi: 10.1016/j.beth.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smedslund G, Berg RC, Hammerstrom KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse (Review). The Cochrane Library. 2011;(11):1–128. doi: 10.1002/14651858.CD008063.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.American Medical Association . Guidelines for Adolescent Preventive Services (GAPS) American Medical Association; Chicago, IL: 1997. [DOI] [PubMed] [Google Scholar]
- 49.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. J Adolesc Health. 2003;33(6):436–57. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 50.Dennis M, Titus JC, Diamond G, Donaldson J, Godley SH, Tims FM, et al. The Cannabis Youth Treatment (CYT) experiment: Rationale, study design and analysis plans. Addiction. 2002;97:16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 51.Schulz KF, Altman DG, Moher D, for the CONSORT Group CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med. 2010:152. Epub 24 March. [PMC free article] [PubMed] [Google Scholar]