Abstract
Introduction
Abnormalities in maternal serum marker levels and fetal measurements obtained during the first trimester screening can be a marker not only for certain chromosomal disorders and anomalies in the fetus but also for specific pregnancy complications. In particular, low maternal serum pregnancy-associated plasma protein-A (PAPP-A), at 11–13 weeks of gestation, is associated with stillbirth, infant death, intrauterine growth restriction, preterm birth, and pre-eclampsia in chromosomally normal fetuses, while a raised nuchal translucency is associated with specific structural abnormalities and genetic syndromes. We have studied the serum Papp-A level in 560 pregnant patients (11–13 weeks gestation) registered at Bharati Hospital and Research Centre, Pune. All patients undergoing testing were followed till the delivery and their neonatal outcome was also taken into consideration.
Aims and Objectives
Our aim is to study the pregnancy outcome in relation to the variations of Papp-A level in the first trimester of pregnancy.
Materials and Methods
Every patient visiting the antenatal OPD was counseled for testing of First Trimester Screening to assess fetal well-being. Patients who were registered for delivery at our hospital were taken into the trial. Blood samples were taken at 11–13 weeks of pregnancy and sent to the PerkinElmer lab for analysis. Results were expressed in Multiple of Median and patients having MOM value less than 0.5 were carefully observed till the delivery, and a thorough neonatal examination was done by a pediatrician.
Observations
524 patients were included in the trial out of which 452 patients were found to have a normal Papp-A level of >0.5 MOM. All these patients were followed further during the antenatal period where 18 patients developed preterm labor and few patients developed pregnancy-induced hypertension. The obstetric outcome of patients with a normal Papp-A level was fairly uneventful as compared to others with a low Papp-A level.
Conclusions
Though Papp-A level in the first trimester of pregnancy (11–13 weeks) is an important predictor of future obstetric outcome, it has poor positive predictive value. Patients having a Papp-A level less than 0.5 MOM have a high risk for preterm delivery, fetal growth restriction, and stillbirths along with increased incidence of hypertensive disorders of pregnancy. A low Papp-A level is a useful indicator of risk of preterm delivery and future chance of development of pregnancy-induced hypertension.
Keywords: Papp-A in pregnancy, Preterm delivery, Fetal growth restriction
Introduction
Abnormalities in maternal serum analyte levels and fetal measurements obtained during the first trimester screening can be a marker not only for certain chromosomal disorders and anomalies in the fetus but also for specific pregnancy complications. In particular, low maternal serum pregnancy-associated plasma protein-A (PAPP-A), at 11–13 weeks of gestation, is associated with stillbirth, infant death, intrauterine growth restriction (IUGR), preterm birth, and pre-eclampsia in chromosomally normal fetuses, while a raised nuchal translucency is associated with specific structural abnormalities and genetic syndromes [1, 2].
A low PAPP-A is defined as a maternal serum PAPP-A value <0.4 MOM, with increased frequency of adverse obstetrical outcomes noted below this level [2].
PAPP-A is a large glycoprotein produced by the placenta and decidua thought to have several functions, including prevention of recognition of the fetus by the maternal immune system, matrix mineralization, and angiogenesis. A low PAPP-A is therefore descriptive of poor early placentation resulting in complications such as fetal growth restriction, fetal demise, preterm birth, and pre-eclampsia in the third trimester.
Aims and Objectives
Our aim is to study the pregnancy outcomes in relation to the variations of Papp-A level in the first trimester of pregnancy.
Materials and Methods
Every patient visiting the antenatal OPD was counseled for the testing of First Trimester Screening to assess fetal well-being. Patients who were registered for delivery at our hospital were taken into the trial. Blood sample were taken at 11–13 weeks of pregnancy and sent to the PerkinElmer lab for analysis. Results were expressed in Multiple of Median and patients having MOM value less than 0.5 are carefully observed till the delivery, and a thorough neonatal examination was done by a pediatrician.
Observations
We could study 524 patients in the first trimester of pregnancy by doing their Papp-A level. A Papp-A level more than or equal to 0.5 MOM is considered normal, while levels less than 0.5 MOM are marked as low.
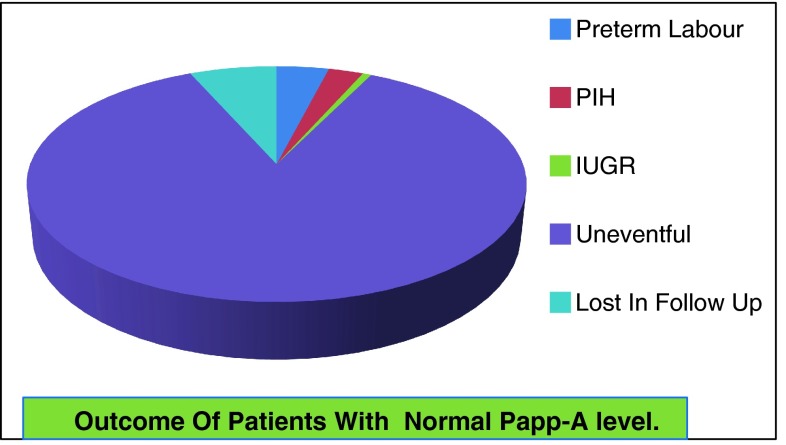
Normal MOM >0.5
452 patients were found to have normal levels and were further followed till delivery. 18 patients developed preterm labor (Fig. 1) on their successive follow-up, while 12 patients had good neonatal outcome. 6 babies had extreme prematurity which required prolonged NICU admission and repeated surfactants.
Fig. 1.
Outcome of patients having Papp-A level >0.5 MOM
12 patients in the normal MOM study arm developed pregnancy-induced hypertension, which in most of the patients was well controlled with treatment, but 2 patients required termination of pregnancy in the 8th month of pregnancy.
No isolated fetal growth restriction was documented in the study arm, except in two to three patients where it was associated with pregnancy-induced hypertension.
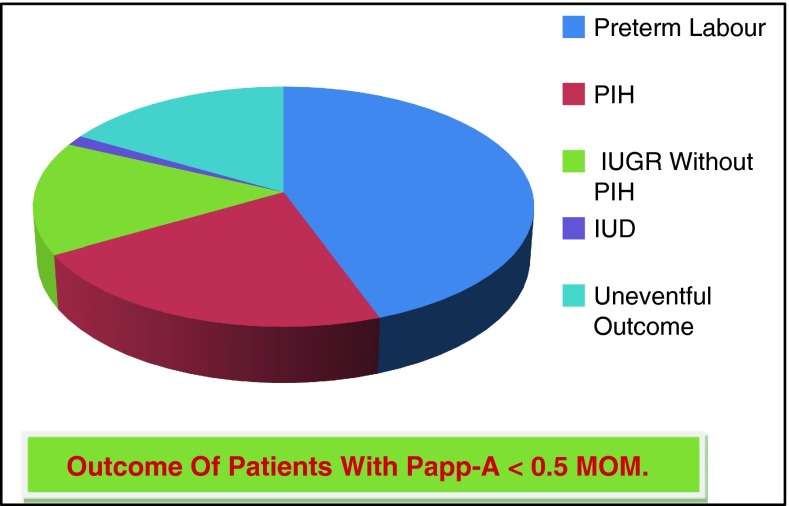
Low Papp-A Level <0.5 MOM
72 patients in the study group had a Papp-A level <0.5 MOM. All of these patients were followed till the delivery. A significant number of patients in the study arm developed preterm labor—32 patients (Fig. 2). 21 patients delivered during the 32–36 weeks of pregnancy where the outcome was comparatively better, while 11 patients delivered during the 28–32 weeks of pregnancy. Interestingly, most of the patients who developed preterm labor did not respond to the tocolytic agents and we could hardly buy any time for the antenatal steroids to act and to enhance the fetal lung maturity.
Fig. 2.
Outcome of patients having Papp-A <0.5 MOM
16 patients in this study arm developed pregnancy-induced hypertension and 7 patients required termination of pregnancy for the severe pre-eclampsia.
11 patients in the study group had developed Fetal Growth Restriction and did not have simultaneous PIH. Most of the patients had asymmetrical FGR suggesting increased uteroplacental resistance as a cause of Fetal Growth Restriction.
So, the positive predictive value of low Papp-A level in our study is 52 % to anticipate future obstetrical complications such as preterm deliveries, fetal growth restrictions, and stillbirths.
While those patients having a Papp-A level more than 0.5 MOM also had preterm deliveries but the incidence is comparable to the general population. The incidence of gestational hypertension and preterm labor was relatively high in patients with a Papp-A level less than 0.5 MOM.
Table 1 shows a significant rise in the incidence of preterm labor, fetal growth restriction, and PIH in patients with low Papp-A level in the first trimester of pregnancy.
Table 1.
A comparison between the outcomes of patients with normal Papp-A and low Papp-a levels is shown
| Preterm labor | Fetal growth restriction | Pregnancy-induced hypertension | Stillbirths | |
|---|---|---|---|---|
| Normal Papp-A >0.5 MOM : 425 patients | 18 (4.2 %) | 12 (2.8 %) | 3 (Associated with PIH) | Nil |
| Low Papp-Av <0.5 MOM : 72 patients | 32 (47 %) | 11 (Unrelated to the PIH) (15 %) | 16 (22 %) | 01 |
Discussion
A low PAPP-A level is poorly sensitive; although these associations exist at the lower end of the PAPP-A distribution, a majority of patients with these adverse outcomes do not have a low PAPP-A. In addition, it has a low positive predictive value as few patients with a low PAPP-A actually have an adverse outcome [3]. However, the likelihood of an adverse outcome does increase as the PAPP-A level decreases, with extremely low levels of PAPP-A having very high positive predictive values as follows: < .45 MoM (5th percentile).
1 to 4 % risk of pregnancy loss before 20 weeks;
increased risk of IUGR, positive predictive value 14 % (OR 2.7, 95 % CI 1.9–3.9);
increased risk of preterm delivery before 34 weeks (OR 2.3, 95 % CI 1.1–4.7).
<0.29 MoM (1st percentile) significantly increased risk of IUGR, with positive predictive values of 24 % [4, 5].
Studies have shown that in combination with a low PAPP-A level, second trimester monitoring of fetal growth, placental size, and Doppler indices can help to identify women at high risk of adverse obstetric outcomes [1, 2, 5–7] and improve accuracy. In addition, a normal ultrasound examination does not rule out an adverse pregnancy outcome [6].
PAPP-A is produced by the placental trophoblasts, especially by the extravillous cytotrophoblasts [8]. It is a “protease” for insulin-like growth factor (IGF)-binding proteins 4 and 5 [9]. This means it has the ability to help release IGF from these binding proteins so that it is free to interact with its cell receptor [10]. IGF is thought to play an important role in trophoblast invasion and hence the early development and vascularization of the placenta and the placental bed. These early events in the formation of the placenta are critical to the pregnancy outcome and, when abnormal, are associated with miscarriage, IUGR of the baby, pregnancy-induced hypertensive disorders, fetal death in utero, premature delivery, and even cesarean section for indications of fetal or maternal compromise. It has been postulated that low levels of PAPP-A, resulting in less release of IGF, could be a pathway by which placentation abnormalities occur that culminate in these poor pregnancy outcomes.
Recent studies would support this association between low PAPP-A levels in the first trimester and risk for poor pregnancy outcome. Spencer and colleagues [11] evaluated first trimester markers in 54,722 chromosomally normal singleton pregnancies. At the 5th percentile of PAPP-A (0.415 MoM), the odds ratios for fetal loss before 24 weeks, at or above 24 weeks, and at any gestational age were 3.3, 1.9, and 2.8, respectively. In other words, there was about a threefold risk of losing a baby with low PAPP-A levels. Cowans and Spencer [12] recently confirmed the association between low PAPP-A and low for gestational age birth weight babies as well. Indeed, they found a linear relationship between the severity of growth restriction and the decrease in PAPP-A levels—in other words, the lower the PAPP-A, the smaller the babies at any gestational age.
Several other studies confirm the association of the other “pregnancy complications” noted above with low levels of PAPP-A. For example, as a spin-off of the results in the First and Second Trimester Evaluation of Risk (FASTER) trial, it was found that women with PAPP-A at or below the 5th percentile “were significantly more likely to experience fetal loss at less than or equal to 24 weeks, low birth weight, preeclampsia, gestational hypertension, preterm birth (P < 0.001) and stillbirth, preterm premature rupture of membranes, and placental abruption (P < 0.02)” [13].
Conclusions
Though Papp-A level in the first trimester of pregnancy (11–13 weeks) is an important predictor of future Obstetric outcome, it has poor positive predictive value. Patients having Papp-A level less than 0.5 MOM have a higher risk for preterm delivery, fetal growth restriction, and stillbirths along with increased incidence of hypertensive disorders of pregnancy. The lower the MOM Value of Papp-A, the more the chances of adverse obstetrical outcome. In our study, we have found an increased incidence of preterm labor and pregnancy-induced hypertension in patients having a Papp-A level <0.5 MOM. While patients having a Papp-A level >0.5 MOM had fairly uneventful obstetric outcome except for a few of them who had preterm labor and PIH, which is comparable to the population mean. So, further larger studies will be required involving large subgroups of pregnant patients to determine the association of Papp-A level and its outcome.
References
- 1.Proctor LK, Toal M, Keating S, et al. Placental size and the prediction of severe early-onset intrauterine growth restriction in women with low pregnancy-associated plasma protein-A. Ultrasounds Obstet Gynecol. 2009;34(3):274–282. doi: 10.1002/uog.7308. [DOI] [PubMed] [Google Scholar]
- 2.Gagnon A, Wilson RD, Audibert F, et al. Obstetrical complications associated with abnormal maternal serum marker analytes. J Obstet Gynaecol Can. 2008;30(10):918–949. doi: 10.1016/S1701-2163(16)32973-5. [DOI] [PubMed] [Google Scholar]
- 3.Jacob A, Canick JA, Messerlian GM et al (2010) Pregnancy outcomes predicted by serum markers assayed in Down syndrome screening.
- 4.Krantz D, Goetzl L, Simpson JL. Association of extreme first-trimester free human chorionic gonadotropin-beta, pregnancy-associated plasma protein A, and nuchal translucency with intrauterine growth restriction and other adverse pregnancy outcomes. Am J Obstet Gynecol. 2004;191(4):1452. doi: 10.1016/j.ajog.2004.05.068. [DOI] [PubMed] [Google Scholar]
- 5.Spencer K, Cowans NJ, Chefetz I, et al. First-trimester maternal serum PP-13, PAPP-A and second-trimester uterine artery Doppler pulsatility index as markers of pre-eclampsia. Ultrasound Obstet Gynecol. 2007;29(2):128–134. doi: 10.1002/uog.3876. [DOI] [PubMed] [Google Scholar]
- 6.Filippi E, Staughton J, Peregrine E, et al. Uterine artery Doppler and adverse pregnancy outcome in women with extreme levels of fetoplacental proteins used for down syndrome screening. Ultrasound Obstet Gynecol. 2011;37(5):520–527. doi: 10.1002/uog.8901. [DOI] [PubMed] [Google Scholar]
- 7.Cnossen JS, Morris RK, Riet G, et al. Use of uterine artery Doppler ultrasonography to predict pre-eclampsia and intrauterine growth restriction: a systematic review and bivariable meta-analysis. CMAJ. 2008;178(6):701–711. doi: 10.1503/cmaj.070430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Handschuh K, et al. Low PAPP-A: what are the clinical implications? Placenta. 2006;27(Suppl A):S127–S134. doi: 10.1016/j.placenta.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Bowman CJ, Streck RD, Chapin RE. Maternal-placental insulin-like growth factor (IGF) signaling and its importance to normal embryo-fetal development. Birth Defects Res B. 2010;17:10–18. doi: 10.1002/bdrb.20249. [DOI] [PubMed] [Google Scholar]
- 10.Kirkegaard I, Uldbjerg N, Oxvig C. Biology of pregnancy-associated plasma protein-A in relation to prenatal diagnostics: an overview. Acta Obstet Gynecol Scand. 2010;89(9):1118–1125. doi: 10.3109/00016349.2010.505639. [DOI] [PubMed] [Google Scholar]
- 11.Ultrasound Obstet Gynecol 2006;28:637-43. [DOI] [PubMed]
- 12.Cowans NJ, Spencer K. First-trimester ADAM12 and PAPP-A as markers for intrauterine fetal growth restriction through their roles in the insulin-like growth factor system. Prenat Diagn. 2007;27(3):264–271. doi: 10.1002/pd.1665. [DOI] [PubMed] [Google Scholar]
- 13.Dugoff L, Hobbins JC, Malone FD, et al. First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: a population-based screening study (the FASTER Trial) Am J Obstet Gynecol. 2004;191(6):1446–1451. doi: 10.1016/j.ajog.2004.06.052. [DOI] [PubMed] [Google Scholar]