Abstract
Objective
On 7 April 2012, a recently returned traveller from Thailand to Australia was confirmed to have measles. An outbreak of measles subsequently occurred in the state of New South Wales, prompting a sustained and coordinated response by public health authorities. The last confirmed case presented on 29 November 2012. This report describes the outbreak and its characteristics.
Methods
Cases were investigated following Australian protocols, including case interviews and assessment of contacts for post-exposure prophylaxis.
Results
Of the 168 cases identified, most occurred in south-western and western Sydney (92.9%, n = 156). Notable features of this outbreak were the disproportionately high number of cases in the 10–19-year-old age group (29.2%, n = 49), the overrepresentation among people of Pacific Islander descent (21.4%, n = 36) and acquisition in health-care facilities (21.4%, n = 36). There were no reported cases of encephalitis and no deaths.
Discussion: This was the largest outbreak of measles in Australia since 1997. Its occurrence highlights the need to maintain vigilant surveillance systems for early detection and containment of measles cases and to maintain high population immunity to measles through routine childhood immunization. Vaccination campaigns targeting susceptible groups may also be necessary to sustain Australia’s measles elimination status.
Introduction
Measles is a highly infectious disease caused by a paramyxovirus of the genus Morbillivirus. Globally it is the most important cause of vaccine-preventable death.1 In Australia, two doses of measles-mumps-rubella (MMR) vaccine were introduced to the routine childhood vaccination schedule in 1998 for all children at 12 months and four years of age and for all adults born after 1966 who were not immune or had one dose of MMR.2 Since July 2013, the second dose has been administered at 18 months of age as the measles-mumps-rubella-varicella (MMRV) vaccine.3 A measles control campaign was also adopted in 1998, targeting children aged five to 12 years, resulting in high two-dose vaccination rates for this group. A national serological survey in 2002 estimated that the cohort born between 1978 and 1982 (aged 30–34 years in 2012) had lower immunity, having only received one dose of measles vaccine and being born in a period when natural measles infection was less common; the cohort born before 1978 had better immunity.4 Those born before 1966 were assumed to have been naturally infected.
Measles elimination has been discussed since the development of an effective measles vaccine in the 1960s. In 2005, the World Health Organization Regional Committee for the Western Pacific, of which Australia is a member, formally declared a goal of measles elimination in the region by 2012.5 It has been suggested that this had been achieved in Australia as early as 1999,4 due to high population immunity achieved through the 1998 measles control campaign and ongoing high two-dose vaccination rates among children since then,4,6 as well as a low incidence rate of measles in Australia with no endemic genotypes of the virus found in Australia since the early 1990s.4,7
However, measles cases acquired overseas are still detected in Australia which occasionally results in small outbreaks with ongoing transmission occurring in underimmunized populations. A large measles outbreak began in April 2012, with the index case being a 25-year-old male traveller from Thailand. During the next eight months, a further 167 cases were identified in the Australian state of New South Wales (NSW), constituting the largest measles outbreak in Australia since 1997 and illustrating the challenges in maintaining Australia’s measles elimination status. We report on the characteristics of this outbreak.
Methods
Under the NSW Public Health Act 2010,8 patients with measles must be notified to the local Public Health Unit by doctors and laboratories. NSW is divided into eight Local Health Districts with each district containing a Public Health Unit. Local Health Districts are subdivided into Local Government Areas (LGAs) and further subdivided into suburbs.
All confirmed cases, as defined in the Australian national guidelines,9 with a symptom onset between 7 April and 29 November 2012, an epidemiological link to South Western Sydney or Western Sydney Local Health Districts, no history of overseas travel and a laboratory specimen that was of either unknown or D8 genotype were considered part of the outbreak. Clinical specimens from measles cases occurring in this period with no clear epidemiological link to outbreak cases underwent genotyping at a reference laboratory.
Routine case investigation and the public health response followed the Australian national guidelines.9 Where possible, vaccination status was validated on the Australian Childhood Immunization Register (ACIR) established in 1996 to record immunizations administered to children under the age of seven. ACIR is considered to be a reliable record of all immunizations received in Australia by Australian residents currently aged 16 and under. Contacts of cases were assessed for timely post-exposure prophylaxis, either MMR or human normal immunoglobulin, as indicated.
Data were analysed using Microsoft Excel 2010 and Epi InfoTM 7. Age-specific notification rates were calculated using 2012 mid-year NSW population data from the Australian Bureau of Statistics. Crude notification rates for Aboriginal and/or Torres Strait Islander people and people of Samoan ancestry were calculated using NSW population data obtained in the 2011 national census. Data on MMR vaccination coverage by postcode and LGA were obtained from the NSW Ministry of Health. Mapping of cases was performed using ArcGIS 10.1.
Results
Temporal and geographic distribution
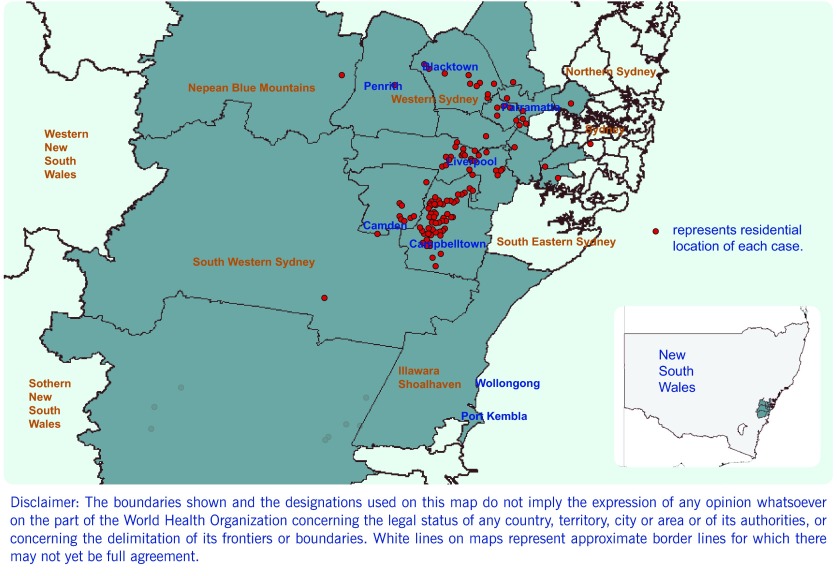
Between April and November 2012, over a period of 36 weeks, 168 confirmed cases of measles occurred in NSW (Fig. 1) – the majority (n = 126, 75.0%) in South Western Sydney Local Health District (Fig. 2). Western Sydney Local Health District had the next highest number of cases (n = 30, 17.9%), with the remaining cases distributed among several other districts. LGAs with the highest notification rates were Campbelltown, Camden and Liverpool (Table 1), all located in South Western Sydney Local Health District. The suburb of Claymore, located within Campbelltown LGA, had a particularly high notification rate (Table 1).
Fig. 1.
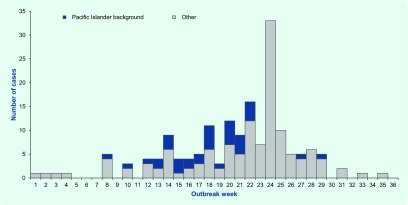
Number of measles cases by outbreak week and Pacific Islander status by symptom onset date, New South Wales, Australia, April to November 2012 (n = 168)
Fig. 2.
Measles cases by residence, New South Wales, Australia, April to November 2012 (n = 168)
Table 1. Measles case notification rates and immunization coverage rates with MMR1 and MMR2 in 2012 in Local Government Areas in New South Wales with greater than 10 outbreak cases, April to November 2012.
| Local Government Area | Incidence rate (per 100 000 population) | MMR1 vaccination coverage at two years of age in 2012 (%) | MMR2 vaccination coverage at five years of age in 2012 (%) |
|---|---|---|---|
| Blacktown LGA | 3.2 | 93.7 | 91.0 |
| Camden LGA | 17.4 | 96.8 | 94.1 |
| Campbelltown LGA | 47.2 | 94.8 | 92.3 |
| Claymore (suburb) | 393.0 | 92.6 | 88.2 |
| Liverpool LGA | 16.4 | 93.9 | 92.1 |
| Parramatta LGA | 5.7 | 93.2 | 91.0 |
| NSW (total) | 2.3 | 93.8 | 91.2 |
MMR – measles-mumps-rubella
Case characteristics
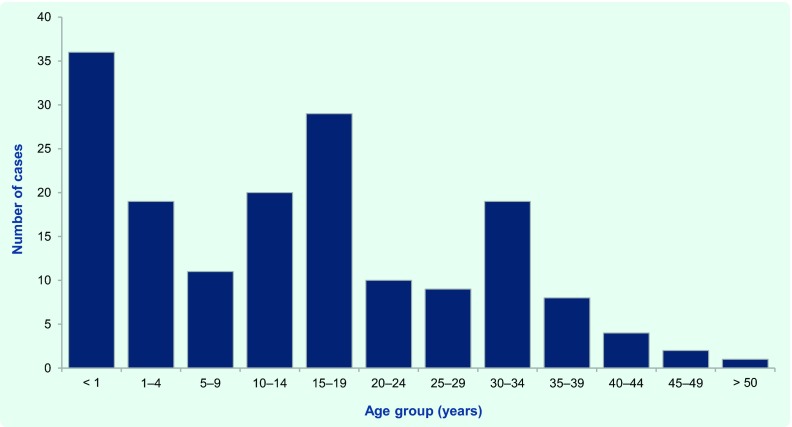
Approximately half the cases were male (n = 87, 51.8%), with the age ranging from four months to 61 years and a median age of 14 years (Fig. 3). Measles case notification rates were highest in the less-than-one-year age group (n = 36, 37.3 per 100 000 population) followed by 15–19-year-olds (n = 29, 6.2 per 100 000 population), one- to four-year-olds (n = 19, 5.0 per 100 000 population) and 10–14-year olds (n = 20, 4.5 per 100 000 population). Among children aged less than one year (n = 36), 28% were aged less than nine months (n = 10).
Fig. 3.
Number of measles cases by age group, New South Wales, April to November 2012 (n = 168)
Of the 168 cases, 12 (7.1%; 5.8 per 100 000 population) were identified as being Aboriginal and/or Torres Strait Islander people. Thirty-six cases (21.4%) were of Pacific Islander descent with 29 Samoan (17.3%; 188.7 per 100 000 population). The Pacific Islander cases were particularly overrepresented in the first half of the outbreak, with all but two occurring before week 23 (Fig. 1). They also comprised 29% (n = 14) of the 10–19-year-old age group.
Clinical course of illness
The most common symptoms recorded were rash (n = 168, 100%), fever (n = 165, 98.2%), cough (n = 158, 94.0%), coryza (n = 143, 85.1%) and conjunctivitis (n = 101, 60.1%). Koplik’s spots were identified in 43 cases (25.6%), with other symptoms including lethargy, malaise, vomiting, sore throat and headache. Most cases (n = 130, 77.4%) had fever at the time of rash onset.
Forty-nine cases (29.2%) were hospitalized; seven (4.2%) developed complications – five developed bronchiolitis, one pneumonia and one pregnant case miscarried at eight weeks during the prodrome of her measles illness. There were no reported cases of encephalitis and no deaths.
Laboratory diagnosis
Most cases (n = 157, 93.5%) were laboratory-confirmed with the remaining 11 cases (6.5%) confirmed based on clinical and epidemiological evidence. Of the 148 cases with available laboratory test results, most were confirmed through serological assay for measles virus-specific IgM antibodies (n = 123), followed by antigen detection on a respiratory specimen by immunofluorescence (n = 51) and nucleic acid testing on a respiratory or urine sample (n = 43). Negative test results were not reported to Public Health Units. Genotyping identified measles virus genotype D8 in 55 outbreak cases and genotype B3 in one case that was excluded from the outbreak.
Vaccination
Forty cases (23.8%) reported a vaccination history of at least one dose of MMR. Of the 22 that were eligible for inclusion on ACIR, only seven were located on ACIR; three of the seven cases had received two doses of MMR vaccine. For the remaining 33 cases with no records on ACIR, only one provided alternate documentation of immunization status; the remaining 32 were based on self-report (six reported receiving two doses of MMR vaccine).
Most of the 128 cases that were not sure or reported no history of vaccination were aged more than one year (n = 95) and therefore were not vaccinated appropriately for their age. For the 52 cases that provided a reason for this non-vaccination, the most common reasons included being a vaccine refuser (n = 32) forgetting to get vaccinated (n = 5) or being born overseas (n = 3).
In 2012, the five LGAs with more than 10 outbreak cases (Table 1) had immunization coverage of at least 93% for the first dose of MMR vaccine and at least 91% for the second dose. The same was found by suburb, with the exception of Claymore in Campbelltown LGA which had coverage of 88.2% for the second dose of MMR.
Health service presentations
There were 355 separate health service presentations by the 168 cases; 197 (55.5%) presented to general practitioners and 158 (44.5%) to emergency departments. In 80 emergency department (50.6%) and 33 general practitioner (16.8%) visits, isolation procedures were adopted, and no contact follow-up was required. There were 16 instances of transmission occurring in the waiting rooms of general practices and emergency departments, and in hospital wards, resulting in 36 secondary cases (21.4% of all cases).
Public health response
Case and contact follow-up
A total of 4786 contacts of cases not correctly isolated in waiting rooms of emergency departments and general practitioners were contacted by telephone and letter. Of these, 621 were advised to have MMR vaccine and 442 to have normal human immunoglobulin as post-exposure prophylaxis. An additional 415 personal contacts of cases were identified for follow-up; 80 were advised to have MMR vaccine and 85 to have normal human immunoglobulin.
The volume of cases and large number of susceptible contacts identified required additional staffing within some Public Health Units, and in South Western Sydney Local Health District Public Health Unit an Incident Command System structure was adopted. In addition, the NSW Health Computer Assisted Telephone Interviewing service was engaged to assist with contact follow-up.
Prevention measures
Multiple methods of communicating with both health practitioners and the community were used. Alerts were sent to general practitioners and emergency departments, local Public Health Units placed posters in areas believed to see a high volume of people within the most affected communities and multiple media releases were broadcast.
MMR vaccination clinics were established in seven high schools that either had confirmed cases or high enrolments of students of Pacific Islander descent. A community vaccination clinic was also established in a local club. In addition, Samoan churches were visited by public health staff and community leaders, and educational materials about measles were distributed in both English and Samoan.
Discussion
Despite high vaccination coverage and timely public health control measures, this measles outbreak continued for 35 weeks. In Australia, unvaccinated young adults have been linked to outbreaks and pose a particular risk because of their mobility, high contact rates and the increasing ease of overseas travel.10 The D8 genotype in this outbreak is known to be circulating in Thailand and has been exported to Australia and Europe previously.11,12 Key features of this outbreak were the disproportionately high notification rates in people of Pacific Island descent and teenagers. Other notable features included the number of infants affected and nosocomial transmission in health-care settings.
In the era of measles elimination, underimmunized minority groups are a major component of measles epidemiology; however, interventions to increase immunity in these groups remain a challenge.13–15 In Australia, Pacific Islanders are a high-risk group for ongoing transmission of measles,16 as shown in this outbreak, where people of Pacific Island, particularly Samoan descent, were overrepresented. In 2006, there were approximately 100 000 Pacific Islanders living in Australia, predominantly in Sydney, Melbourne and Brisbane.17 This figure, however, is likely to be an underestimate as many Pacific Islanders arrive via New Zealand, with which Australia has special mutual migration arrangements whereby citizens can visit, live and work in either country.18 In the 2011 national census, Campbelltown LGA had a population of 145 967 with 2.1% reporting speaking Samoan in their households19; in Claymore, within Campbelltown LGA, this was 13.0% of the 3308 population, one of the highest proportions in NSW.20 Official immunization data by ethnicity are not available, but staff that conducted the MMR clinics in high schools during the outbreak reported that many students of Pacific Islander background appeared to have missed routine childhood vaccinations both before and after their arrival in Australia.
The three LGAs with the highest notification rates in 2012, Campbelltown, Camden and Liverpool, also had higher vaccination coverage rates than the NSW average. This suggests that high coverage rates at the LGA level may not represent complete coverage within the LGA, as there may be pockets of underimmunized populations in these areas, as evidenced by the lower vaccine coverage in Claymore. Therefore, as well as ensuring childhood vaccination targets of 95% for the first dose and 90% for the second dose,21 geographically targeted strategies towards susceptible minority groups are also required to increase overall measles immunity.
There was also a high number of cases aged between 10 and 19 years in this outbreak – a group that should have received routine childhood vaccinations. A measles outbreak in England in 2012 showed a similar pattern, attributed to the dramatic fall in MMR vaccinations in the United Kingdom in the late 1990s following a link made between the MMR vaccine and autism, which was subsequently discredited.22 However, this does not explain the high number of cases in this age group in this outbreak, as according to ACIR data, Australia did not suffer the same decline in MMR coverage at that time.23 As ACIR data were not consistently reported until the late 1990s,24 historical immunization coverage of teenagers (aged 14 and over in 2012) is not available. Also, the immunization status of children who migrate to Australia is not captured by ACIR, especially those over the age of four who have missed all routinely scheduled immunizations. These factors may partially explain why this potentially susceptible group that should have received routine childhood vaccinations may have been undetected before the outbreak. Despite this, that over two thirds of cases in this age group were born in Australia and should have received two doses of MMR vaccine as part of routine childhood immunizations introduced in 1998 is a concern.
Two other age groups at high risk of measles infection25 were also overrepresented in this outbreak – infants and adults aged 30–34. Infants aged less than 12 months are too young to have been vaccinated. That a significant proportion of this group were aged less than nine months suggests earlier waning natural protection offered by maternal antibodies than previously thought.26 Adults aged 30–34 years grew up in a period when measles was not endemic in Australia, but due to their age, they may have missed out on the 1998 vaccination programme and measles control campaign.
Nosocomial transmission in health-care settings formed a significant component of the outbreak burden, also seen in previous outbreaks,27 as these settings are ideal for transmission of measles due to their closed spaces and susceptible occupants.28 The large number of multiple presentations by cases to health-care facilities contributed to nosocomial transmission, as did the lack of isolation of cases presenting with a fever and rash, despite significant communication between public health authorities and clinical services. A high turnover of staff and the nature of shift work in emergency departments where staff were not always present to access the communications from public health authorities, as well as a lack of diagnostic experience among younger clinicians who often had never seen a case of measles, may explain these oversights.
There are some limitations to this outbreak investigation. Small surveillance gaps between generations of cases illustrated that not all cases of measles were being identified. Reporting of negative test results are not required in the established surveillance system, and cases that were initially notified but later discarded due to incomplete or poor-quality laboratory test results made it difficult to draw conclusions about the effectiveness of the surveillance system. Data quality was at times incomplete, including for ethnicity status and whether a contact received their recommended intervention. Cases were not followed up after initial interview and contact tracing; information about complications from measles was also incomplete and may underestimate the true burden of disease. The sensitive case definition used may have included cases not truly part of the outbreak; however, this number is likely to be small as all cases with no clear epidemiological links underwent genotyping with only one non-D8 case identified.
This outbreak, although the largest in Australia since 1997, was relatively modest in size, limited in geographical spread and of moderate duration compared with other recent outbreaks from industrialized countries throughout Europe.29 However, its duration is cause for concern, particularly as recent modelling suggests that based on declining measles seropositivity, the effective reproductive number (R) may exceed one in Australia in the next few years.30 Australia’s measles elimination status was not affected by this outbreak; however, the circulation of a single measles virus genotype for 35 weeks highlights the need to maintain vigilant surveillance systems for early detection and containment of measles cases and to maintain high population immunity to measles. This outbreak also highlighted susceptibility of measles in Pacific Islanders living in Australia and that young travellers can cause measles outbreaks in non-endemic countries; a vaccination programmme targeting these at-risk groups needs to be implemented in conjunction with the routine childhood immunization programme, to which no change is required.
Conflicts of interest
None declared.
Funding
None.
References
- 1.Moss WJ, Griffin DE. Measles. Lancet. 2012;379:153–64. doi: 10.1016/S0140-6736(10)62352-5. [DOI] [PubMed] [Google Scholar]
- 2.National Centre for Immunisation Research & Surveillance Immunisation Schedules. Sydney: University of Sydney; 2000. http://www.ncirs.edu.au/immunisation/schedules/ updated 18 June 2012. accessed 30 August 2013. [Google Scholar]
- 3.Australian Technical Advisory Group on Immunisation. The Australian Immunization Handbook. 10th ed. Canberra: Australian Government Department of Health and Ageing; 2013. [Google Scholar]
- 4.Heywood AE, et al. Elimination of endemic measles transmission in Australia. Bulletin of the World Health Organization. 2009;87:64–71. doi: 10.2471/BLT.07.046375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Progress toward the 2012 measles elimination goal–Western Pacific Region, 1990–2008. MMWR Morbidity and Mortality Weekly Report. 2009;58:669–73. [PubMed] [Google Scholar]
- 6.National Centre for Immunisation Research & Surveillance. Coverage Estimates. Sydney: University of Sydney; 2002. http://www.ncirs.edu.au/immunisation/coverage/estimates/index.php updated 18 July 2013. accessed 30 August 2013. [Google Scholar]
- 7.Rosewell A, Reinten-Reynolds T, Spokes PJ. EpiReview: Measles in NSW, 2002–2011. New South Wales Public Health Bulletin. 2012;23:201–7. doi: 10.1071/NB12085. [DOI] [PubMed] [Google Scholar]
- 8.Public Health Act 2010 (New South Wales), Schedule 1. Canberra: Ministry of Health; 2012. http://www.legislation.nsw.gov.au/maintop/view/inforce/act+127+2010+cd+0+Nhttp://www.legislation.nsw.gov.au/maintop/view/inforce/act+127+2010+cd+0+N accessed 30 August 2013. [Google Scholar]
- 9.Measles. National guidelines for public health units. Canberra: Australian Government, Department of Health; 2009. http://www.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-measles.htm updated 19 February 2009. accessed 7 November 2013. [Google Scholar]
- 10.Martin N, Foxwell AR. Measles status in Australia, and outbreaks in the first quarter of 2009. Communicable Diseases Intelligence. 2009;33:225–31. [PubMed] [Google Scholar]
- 11.Rota PA, et al. Global distribution of measles genotypes and measles molecular epidemiology. Journal of Infectious Diseases. 2011;204(Suppl 1):S514–23. doi: 10.1093/infdis/jir118. [DOI] [PubMed] [Google Scholar]
- 12.Kantele A, et al. Travellers returning with measles from Thailand to Finland, April 2012: Infection Control Measures. Euro Surveillance: European Communicable Disease Bulletin. 2012;17(22):pii=20184. doi: 10.2807/ese.17.22.20184-en. [DOI] [PubMed] [Google Scholar]
- 13.Mayoral Cortés JM, et al. Measles outbreak in Andalusia, Spain, January to August 2011. Euro Surveillance: European Communicable Disease Bulletin. 2012;17(42):pii=20300. [PubMed] [Google Scholar]
- 14.Cohuet S, et al. Outbreak of measles among Irish Travellers in England, March to May 2007. Euro Surveillance: European Communicable Disease Bulletin. 2007;12(24):pii=3216. doi: 10.2807/esw.12.24.03216-en. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3216 accessed 30 August 2013. [DOI] [PubMed] [Google Scholar]
- 15.Review of outbreaks and barriers to MMR vaccination coverage among hard-to-reach populations in Europe. Stockholm: European Centre for Disease Prevention and Control; 2013. [Google Scholar]
- 16.Forrest JM, et al. Measles control in Australia. Report of the Measles Control in Australia Workshop, 5 November 1997. Communicable Diseases Intelligence. 1998;22:33–6. [PubMed] [Google Scholar]
- 17.Rose S, Quanchi M, Moore C. A national strategy for the study of the Pacific. Brisbane: Australian Association for the Advancement of Pacific Studies; 2009. http://www.uq.edu.au/hprc/docs/AAAPS%20National%20Report%20Cover%202009_Prof.Moore.pdf accessed 30 August 2013. [Google Scholar]
- 18.Ball R, Beacroft L, Lindley J. Australia’s Pacific Seasonal Worker Climate Scheme. Trends & Issues in Crime and Criminal Justice. Canberra: Australian Institute of Criminology; 2011. p. 432.http://www.aic.gov.au/documents/E/0/C/%7BE0C1EEB4-B893-489E-98F3-8FF9BAF3E8C9%7Dtandi432.pdf accessed 30 August 2013. [Google Scholar]
- 19.2011 Census Quickstats, Campbelltown. Canberra: Australian Bureau of Statistics; 2011. http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/LGA11500 updated 28 March 2013. accessed 30 August 2013. [Google Scholar]
- 20.2011 Census Quickstats, Claymore. Canberra: Australian Bureau of Statistics 2011; http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/SSC10536 updated 28 March 2013. accessed 30 August 2013. [Google Scholar]
- 21.Let’s work together to beat measles: a report on Australia’s Measles Control Campaign. Canberra: Commonwealth Department of Health and Aged Care; 2000. [Google Scholar]
- 22.Vivancos R, et al. An ongoing large outbreak of measles in Merseyside, England, January to June 2012. Euro Surveillance: European Communicable Disease Bulletin. 2012;17(29):pii=20226. doi: 10.2807/ese.17.31.20234-en. [DOI] [PubMed] [Google Scholar]
- 23.Leask J, Booy R, McIntyre PB. MMR, Wakefield and The Lancet: what can we learn? Medical Journal of Australia. 2010;193:5–7. doi: 10.5694/j.1326-5377.2010.tb03730.x. [DOI] [PubMed] [Google Scholar]
- 24.Conaty SJ, McAnulty JM. The Australian Childhood Immunisation Register: validation of the immunisation status of children who are very overdue. Australian and New Zealand Journal of Public Health. 2001;25:139–40. doi: 10.1111/j.1753-6405.2001.tb01835.x. [DOI] [PubMed] [Google Scholar]
- 25.Gidding HF, Gilbert GL. Measles immunity in young Australian adults. Communicable Diseases Intelligence. 2001;25:133–6. [PubMed] [Google Scholar]
- 26.Leuridan E, et al. Early waning of maternal measles antibodies in era of measles elimination: longitudinal study. British Medical Journal (Clinical Research Ed.) 2010;340:c1626. doi: 10.1136/bmj.c1626. [DOI] [PubMed] [Google Scholar]
- 27.Hope K, et al. Measles transmission in health care waiting rooms: implications for public health response. Western Pacific Surveillance and Response Journal. 2012;3:33–8. doi: 10.5365/wpsar.2012.3.3.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Botelho-Nevers E, et al. Nosocomial transmission of measles: an updated review. Vaccine. 2012;30:3996–4001. doi: 10.1016/j.vaccine.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 29.Cottrell S, Roberts RJ. Measles outbreak in Europe. BMJ (Clinical Research Ed.) 2011;342(jun15 1):d3724. doi: 10.1136/bmj.d3724. [DOI] [PubMed] [Google Scholar]
- 30.Wood J, et al. Declining measles seropositivity in Australia and elimination status. Canberra: 2013. https://secure.ashm.org.au/ei/viewpdf.esp?id=112&file=c%3A%5CCertain%5CEventwin%5Cdocs%5Cpdf%5CCDCASIDFinal00279%2Epdf Paper presented at: The Communicable Disease Control Conference, 19–20 Mar 2013. accessed 30 August 2013. [Google Scholar]