Abstract
Background:
It is unclear whether there is an association between chronotype and nonremission of depression, and whether the association is related to the confounding effect of insomnia.
Method:
A cohort of patients with major depressive disorder were assessed for chronotype (by Morningness-Eveningness Questinnaire [MEQ]), depressive symptoms, insomnia severity and clinical outcomes in a naturalistic follow-up study.
Results:
Of the 253 recruited subjects (age 50.8 ± 10.2 y; female: 82.6%; response rate 90.0%), 19.4%, 56.1% and 24.5% patients were classified as eveningness, intermediate, and morningness, respectively. Evening-type subjects had higher insomnia severity, more severe depressive symptoms, and higher suicidality. Eveningness was associated with nonremission of depression with an odds ratio (OR) of 3.36 (95% confidence interval [CI] 1.35–8.34, P < 0.01), independent of insomnia severity. In addition, insomnia was an independent significant factor in contributing to nonremission of depression (OR = 1.12; 95% CI 1.05–1.19, P < 0.001).
Conclusion:
The independent association of eveningness with nonremission of depression suggested a significant underpinning of circadian involvement in major depressive disorder. Our findings support the need for a comprehensive assessment of sleep and circadian disturbances as well as integration of sleep and chronotherapeutic intervention in the management of depression.
Citation:
Chan JWY, Lam SP, Li SX, Yu MWM, Chan NY, Zhang J, Wing YK. Eveningness and insomnia: independent risk factors of nonremission in major depressive disorder. SLEEP 2014;37(5):911-917.
Keywords: chronotype, depression, insomnia, nonremission
INTRODUCTION
Depression is a common mental illness associated with significant mortality and morbidity. Persistent symptoms in depression are associated with adverse clinical outcomes1–3 and a more chronic course of illness.4 Thus, the treatment goal of depression is a complete remission.5 Various clinical and psychosocial factors were found to predict nonremission of depression, including socioeconomic factors (i.e., female sex, lower education, divorce, unemployment, lower family income),6 concurrent anxiety,7 poor initial response to treatment,8 and personality disorders.9 Residual sleep symptoms, especially insomnia, were associated with poorer depression outcomes, including increased symptoms severity,10 higher risk of suicide,11–13 and greater risk of recurrence.14 However, there is increasing evidence suggesting a correlation of circadian rhythm with depression.15–17 Chronotype, which represents the individual circadian types of the diurnal preference for rest and activity, has been suggested to be implicated in depression. The evening chronotype was found to be associated with more depressive symptoms18–21 and a higher suicidal risk22,23 in both community subjects and clinically depressed patients. Nonetheless, the relationship between circadian typology and nonremission of depression was barely investigated. Because eveningness was associated with poorer sleep quality,23 a careful consideration of the role of insomnia in mediating the outcome of depression is needed. Thus, this study was designed to investigate the influence of eveningness on the nonremission outcome of depression while addressing the confounding effect of insomnia.
METHOD
This study was a naturalistic follow-up study of a cohort of patients with depression. Recruitment procedures have been described elsewhere.24 To summarize, patients with major depressive disorder (MDD) according to the International Classification of Disease, 10th Revision (ICD-10) criteria were recruited in 2006 by consecutive sampling at a university-affiliated regional psychiatric clinic. This cohort of patients (n = 371) was followed up in 2010 for the assessment of residual sleep disturbances in depression13 and served as the target study population of the current study, which was conducted in 2011. The study was approved by the local ethics board.
Subject Recruitment
Eligible subjects of the current study included those age 18 y or older and who had MDD, according to the ICD-10 criteria. Patients with a history of bipolar disorders, schizophrenic spectrum disorders, dementia, and alcohol or substance misuse/ dependence were excluded. Shift workers, subjects who were not able to provide valid informed consent, and those who had a significant physical condition that rendered them unable to complete the clinical interview also were excluded from the study.
Data Collection and Assessment
Each subject was interviewed using the Mini-International Neuropsychiatric Interview (MINI),25 and the severity of depression was assessed by the Hamilton Rating Scale for Depression (HRSD)-17 item version.26 They also completed a battery of questionnaires. All the subjects were instructed to complete a prospective 1-w sleep diary and to return it using a prepaid envelope. Clinical information, including the follow-up status, number of psychiatric admissions, and prescriptions of medications at the time of assessment were retrieved from the case notes and the Clinical Management System (CMS), which is a computerized clinical workstation with detailed documentation of the clinical history of any patient who have received the public health care services in Hong Kong.
Measurements
The MINI25 was administered by the clinician to ascertain and confirm the diagnosis of MDD. Suicidality was determined by the suicidality section in the MINI. Suicidal ideation in the most recent 1 mo was deemed present if any of the following items was coded yes: “Over the past 1 mo (1) Have you wished you were dead? (2) Have you wanted to harm yourself? (3) Have you thought of committing suicide? (4) Have you had any plan of suicide?” Lifetime suicidality was deemed present if a positive answer was given to the question: “In your lifetime, have you ever attempted suicide?”
The HRSD26 was administered by the same clinician to score the severity of depression. A cutoff score of 8 or higher in the HRSD and the presence of a current major depressive episode) as ascertained by MINI interview was indicative of depression nonremission at the time of assessment. The cutoff score of 8 or higher was used because it was a widely accepted definition27 and has been used in other large-scale multicenter studies, for example, the STAR*D trial.6
The Morningness-Eveningness Questionnaire (MEQ),28 the most widely used chronotype questionnaire, consists of 19 questions. Individuals scored higher than 58 and lower than 42 are classified as morningess- and eveningness-type, respectively, whereas those who scored between 42 to 58 are classified as intermediate-type. MEQ has been validated locally with good psychometric properties.29
The Insomnia Severity Index (ISI)30 is composed of seven questions concerning the nature, severity, and effect of insomnia in the past 2 w. The Chinese version of ISI has been validated locally.31
The Hospital Anxiety and Depression Scale (HADS)32 is a locally validated self-reported questionnaire for detecting the severity of anxiety and depressive symptoms in psychiatric patients.33,34
The General Sleep Questionnaire (GSQ) is designed to collect information on the sleep-wake habits and to screen for sleep problems on a lifetime and 1-y basis. The questionnaire has been validated by clinical interview in the baseline study of this cohort,24 and the English version is available in our previous publication.12 In addition to the ISI score, subjects with frequent insomnia were identified by the GSQ if they reported having difficulty in initiating sleep, difficulty in maintaining sleep, or early morning awakening for at least three times per week.
A prospective 1-w sleep diary records the bedtime, wake time, number of nocturnal awakenings, and daytime naps on both weekdays and weekends. Time in bed was defined by the time elapsed from bedtime to wake time.
Statistical Analysis
Independent t-test and one-way analysis of variance were used to evaluate the differences in continuous variables. The chi-square and Kruskal-Wallis tests were used for comparing nonparametric variables. To further delineate the relationships among insomnia, depression, and chronotypes, a crude model; a logistic regression model adjusted for age, sex, and ISI; and a fully adjusted model were established with “nonremission of depression” as the dependent variable to test whether eveningness is an independent risk factor of nonremission of depression. All data analyses were carried out by Statistical Package for Social Science (SPSS Inc, Chicago, IL) version 17.0 for Windows.
RESULTS
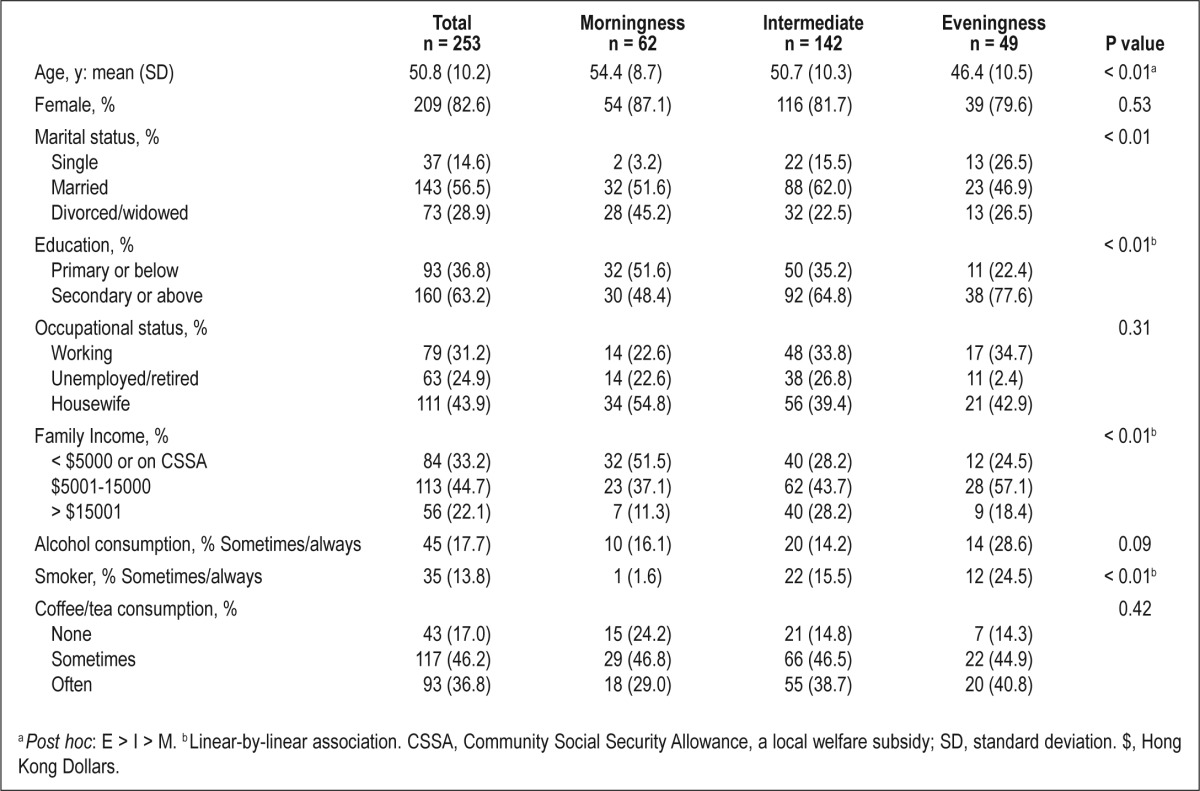
Of the 371 subjects in the cohort, two patients were deceased and 45 patients were excluded (Figure 1). The total number of eligible patients for the current study was 340. Finally, 253 patients were successfully recruited into the study, attaining a response rate of 90.0%. According to the MEQ, 19.4%, 56.1%, and 24.5% of subjects were classified as eveningness, intermediate, and morningness types, respectively. The characteristics of the subjects are presented in Table 1.
Figure 1.
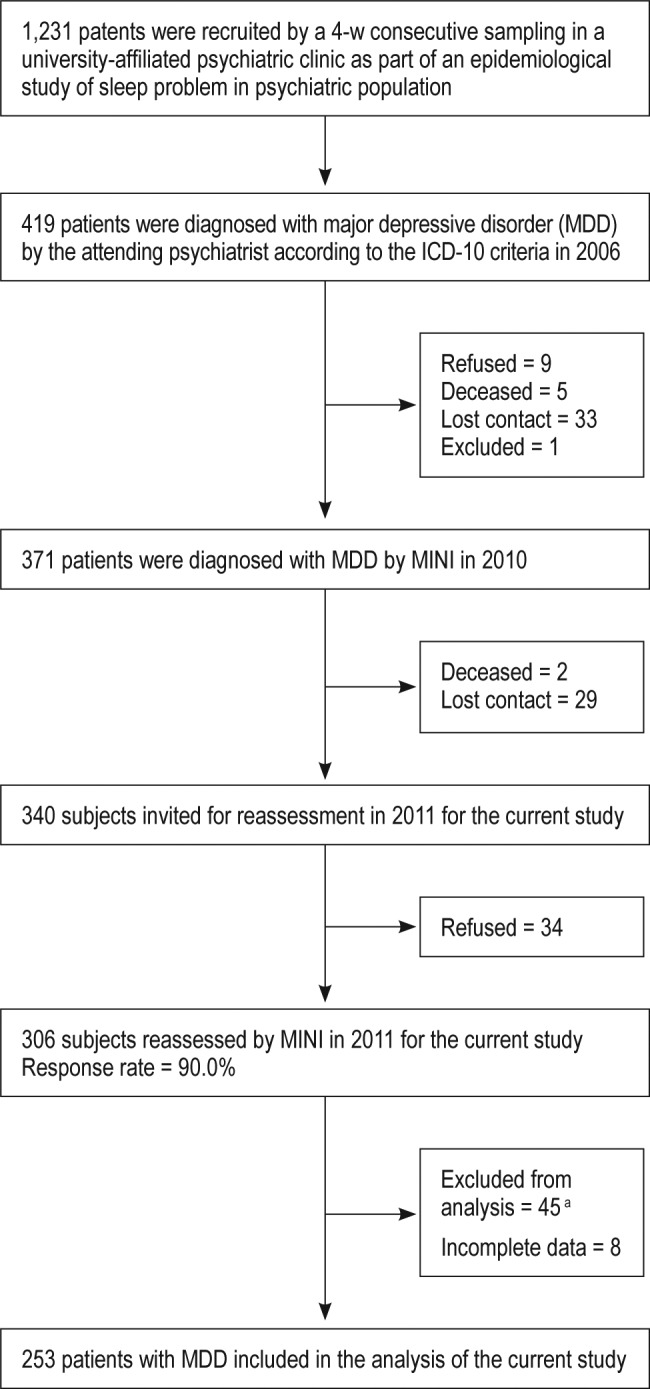
Flow chart indicating recruitment procedures. aBipolar affective disorder = 18, schizophrenia spectrum = 2, dementia = 4, substance abuse = 7, alcohol dependence = 4, significant hearing impairment not able to complete interview = 1, shift-worker = 9.
Table 1.
Comparison of the demographics among the three chronotypes
Clinical Correlates
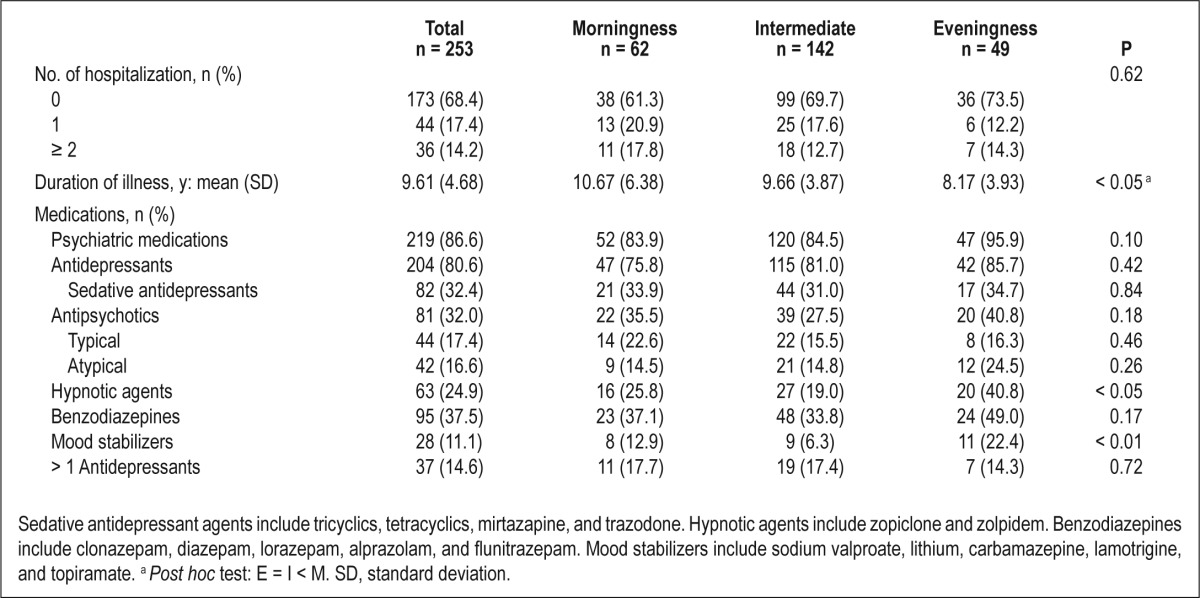
The duration of illness, hospitalization records, and prescription of psychiatric medications were compared among the chronotypes. Morning-type had a significantly longer duration of illness (10.67 ± 6.38 y, P < 0.05), but the association between morningness and duration of illness became insignificant after adjusting for age (P = 0.6). There was no difference in the number of previous hospitalizations among different chronotypes. There were also no significant differences in the prescription of antidepressants, antipsychotic agents, and benzodiazepines among the chronotypes, but a higher percentage of evening-type patients was prescribed hypnotic agents (P < 0.05) and mood stabilizers (P < 0.01; Table 2)
Table 2.
Clinical correlates among chronotypes
Association Between Insomnia and Chronotype
As reflected by the sleep diary, evening-type subjects had a more delayed bedtime and wake time, for approximately 2–3 h later than the morning-type both on weekdays and weekends (Table 3). There was an increasing prevalence of frequent insomnia in the most recent 1 y across the spectrum of circadian preference, with 19.4%, 35.2%, and 46.9% in morningness, intermediate, and eveningness subjects, respectively (P < 0.01). Evening-type had the highest score on the ISI (16.02 ± 5.61, P < 0.01), compared with the morning-type (11.17 ± 6.81) and intermediate-type (14.01 ± 7.07).
Table 3.
Sleep and depression outcomes among the three chronotypes
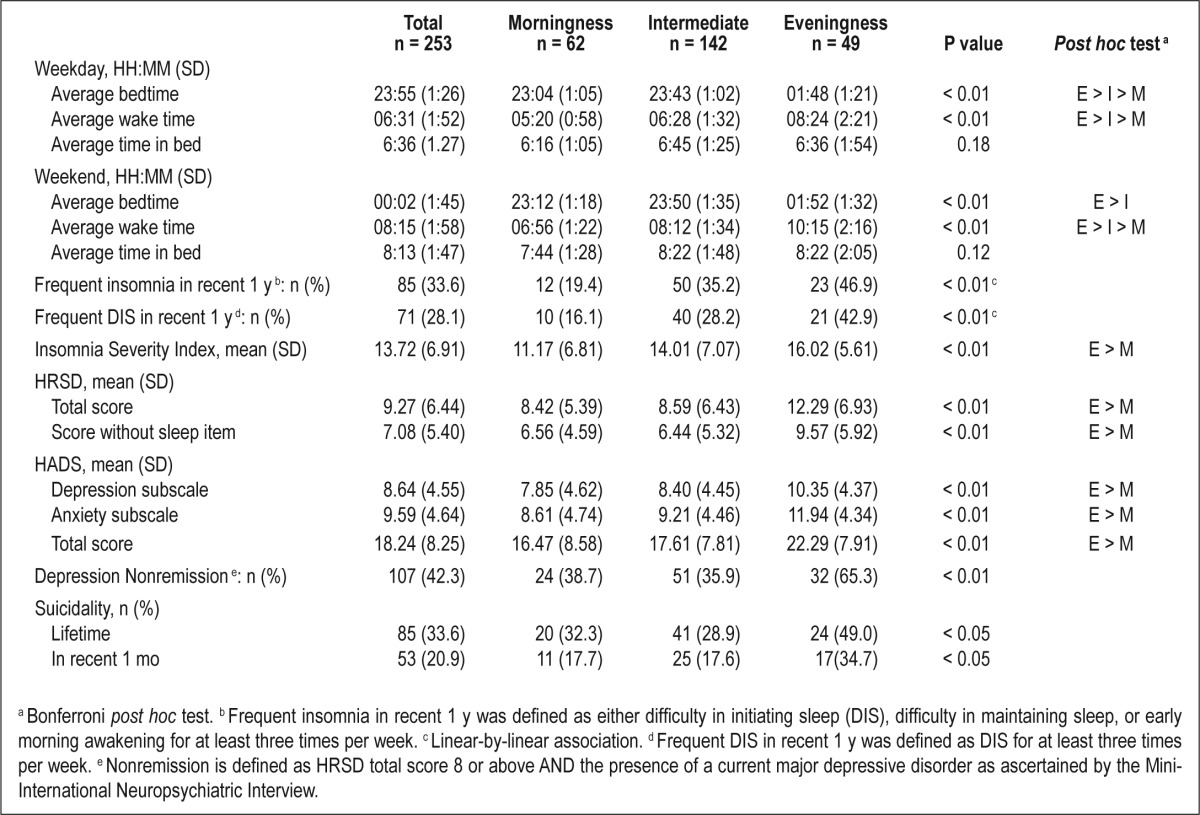
Association Between Chronotype and the Outcome of Depression
Evening-type was associated with more severe depressive symptoms (HRSD scores: 12.9 ± 6.93, P < 0.01), compared with the morning-type (8.42 ± 5.39) and intermediate-type (8.59 ± 6.43). Because insomnia was more severe in the evening-type, a HRSD score without sleep items was calculated. The modified score remained significantly higher in the evening-type (9.57 ± 5.92, P < 0.01). The self-reported HADS depression score showed a similar pattern with a higher severity toward eveningness (10.35 ± 4.37, P < 0.01). Anxiety symptoms, likewise, were significantly worse in the evening-type (11.94 ± 4.34, P < 0.01). Post hoc tests of the HRSD and HADS scores did not reveal any significant differences between the morning- and intermediate-types. In addition, the nonremission rate of depression was highest among the evening-type (65.3%, P < 0.01). They also had the highest prevalence of lifetime suicide attempts (P < 0.05) and a higher level of suicidality in the most recent 1 mo (P < 0.05). Sleep and depression variables are depicted in detail in Table 3.
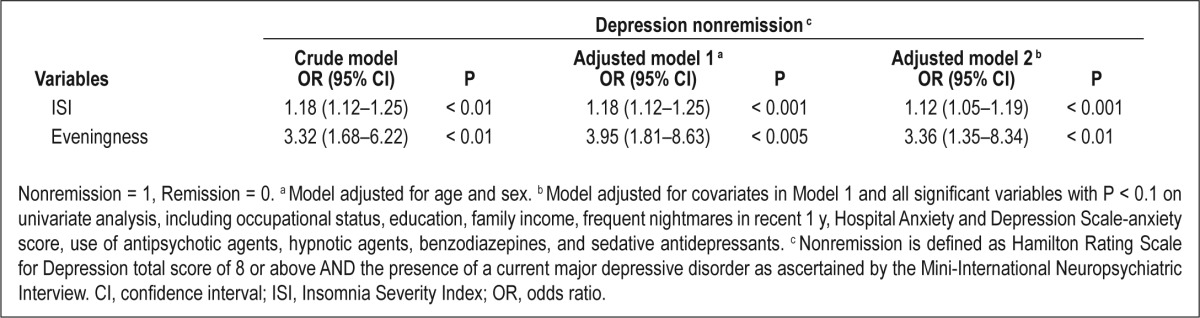
Chronotype and Insomnia in Relation to the Outcome of Depression
In Model 1, eveningness was significantly associated with nonremission after adjusting for age, sex, and ISI (odds ratio [OR] = 3.95, 95% confidence interval [CI] 1.81–8.63, P < 0.005; Table 4). In Model 2, after adjusting for confounding variables including demographics, nightmares, concurrent anxiety, and psychotropic prescriptions, eveningness remained a significant risk factor leading to a threefold risk of depression nonremission compared with the noneveningness group (OR = 3.36, 95% CI 1.35–8.34, P < 0.01). In both models, insomnia severity was an independent predictor of nonremission status of depression (Model 1: OR = 1.18, 95% CI 1.12–1.25, P < 0.001; Model 2: OR: 1.12; 95% CI 1.05–1.19, P < 0.001).
Table 4.
Logistic regression analysis of factors contributing to nonremission of depression
DISCUSSION
In this prospective cohort of patients with MDD, nonremission was common (42.3%) in psychiatric practice. Both insomnia and evening chronotype emerged to be independent risk factors of nonremission in depression.
Sleep Disturbances in MDD
Insomnia is increasingly recognized as a significant factor associated with poor outcomes of depression.12,35 In our study, 33.6% of the subjects complained of frequent insomnia in the most recent 1 y, a percentage that was much higher than the prevalence of insomnia in the local general population (10–12%) using similar defining criteria.36,37 The prevalence rate of insomnia as reported in our cohort, however, was slightly lower than that of the other posttreatment studies (48–51%).38,39 It was likely related to a more stringent criterion that we used to define insomnia. Similarly to previous studies, we have demonstrated that the presence of insomnia independently and negatively affected depression outcomes.12–14 The high prevalence of insomnia in our study highlighted the importance of a comprehensive assessment of both depressive symptoms and concomitant sleep disturbances in the routine clinical settings.13 Various pharmacological and behavioral treatments have been used in treating insomnia in depressed patients, and the adjuvant cognitive-behavioral therapy for insomnia (CBT-I) seems to have yielded some promising results.40 For instance, a recent randomized controlled trial with a modest sample size showed that the addition of CBT-I to antidepressants led to a higher remission rate of depression than antidepressants plus control therapy, albeit the result was not significant (P = 0.08).41 With the ultimate target to achieve complete remission of symptoms, it is imperative to address the high rate of residual insomnia with an effective sleep-targeted treatment to improve the outcomes of depressed patients.
Eveningness as an Independent Risk Factor for Nonremission
In line with previous studies, evening-type depressed patients were found to have more severe depressive symptoms, a higher prevalence of lifetime history of suicidal attempts and current suicidal ideations.18,20,21,23 Furthermore, eveningness was associated with a threefold increased risk of nonremission of depression independent of sociodemographic variables, psychotropic medications, insomnia severity, and concurrent anxiety in our study. Although the overall nonremission rate in our study population was 42.3%, the nonremission rate became higher, reaching 65.3% in the evening-type. Although a lower income and educational attainment were factors that were associated with a lower remission rate,6 eveningness was associated with a higher nonremission rate despite higher family income and educational attainment in our study.
A possible explanation for the association between poorer depression outcomes and eveningness might be related to the contributing effect of insomnia, as shown by a higher ISI score and a more prevalent usage of hypnotic agents in the evening-type subjects in our study. Evening-type individuals were shown to have greater sleep variability42 and more dysfunctional sleep beliefs43 that might contribute to the development of insomnia. Clinically, these potential risk factors could be amenable to sleep intervention through the reinforcement of sleep hygiene and sleep education. In addition, evening-type depressed subjects were shown to have higher suicidality, higher prevalence of smoking, nearly significantly higher rate of alcohol use, and higher use of mood stabilizers. Because the design of the study has excluded the subjects with comorbid alcohol and substance abuse at the intake interview, the weak association with alcohol and substance misuse in the current study was expected. These results were compatible with previous literature suggesting that evening-type subjects tended to exhibit a higher degree of neuroticism44 and impulsivity,45 and to have a higher prevalence of substance abuse.46 The higher percentage of mood stabilizers prescription could be related to the higher impulsivity as reflected by the higher suicidality or presence of agitated or atypical depression, conditions that are not specifically diagnosed by our current diagnostic instruments.
It is worth noting that, however, eveningness was found to be associated with an increased risk of depression nonremission even after adjusting for insomnia severity. This further supports the significant and independent role of circadian factor in contributing to the depressive symptomatology and argues for the development of circadian-focused treatment in depression. There has been increasing evidence showing that circadian interventions, such as light therapy, sleep deprivation, and melatonergic antidepressants, were efficacious in reducing depressive symptoms.17,47 These circadian-focused treatments also have been shown with some initial promising results in enhancing remission in patients with depression.48 It was postulated that disturbances in social rhythm or routines might promote disruptions in circadian rhythms, which in turn precipitate the affective episodes in vulnerable persons.49 The interpersonal and social rhythm therapy proposed for stabilizing the social rhythm was found to lengthen the time to recurrence of both mania and depressive episodes in patients with bipolar affective disorder.50 Research on the treatment of depression that directly addresses the circadian typology is limited, but a study on healthy subjects suggested that the effect of sleep deprivation could differ significantly among different chronotypes (morning-type reported worsening of their depressed mood, whereas evening-types had an improved mood state).51 Thus, chronotype might serve as an important clinical marker to identify vulnerable individuals with a higher risk of nonremission, and there is a need of developing personalized treatment according to one's circadian typology.
In summary, nonremission of depression is very common in clinical practice. Sleep disturbances and eveningness were both implicated in the nonremission of depression. Our findings suggested the importance of a comprehensive and systematic assessment of sleep-wake habits and circadian preference in the routine clinical management, and argued for the need for integrating appropriate sleep and chronotherapeutic treatment in the management of depression.
Limitation
First, the primary limitation of our study was the cross-sectional measurement of chronotype, which precluded us from differentiating the state versus trait nature of chronotype and its causal relationship with depression. It is also possible that there were undetected status change (remitted or relapsed) in between the two time points of assessment. Second, as the definition of remission in our study is tied to the cutoff HRSD score of 8 and absence of major depressive episode by MINI, a different remission rate and results might be produced by other definitions of nonremission. Nonetheless, our current study used the most widely accepted HRSD cutoff for remission. Third, this study was limited by a lack of objective circadian biological markers, such as the measurements of core body temperature or melatonin levels. Previous studies have consistently demonstrated that there was a close association of circadian preference with these biological markers.52,53 In addition, the evening chronotype of the subjects was corroborated by their 1-w prospective sleep diary data, suggesting that the self-reported chronotype would be a valid proxy marker of the circadian preference.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENT
The authors thank the staffs of the sleep assessment unit of Shatin Hospital and Li Ka Shing Psychiatric Centre, Prince of Wales Hospital in supporting this research. This paper was partly based on the data collected for the Part III Examination of the Hong Kong College of Psychiatrists for the author CJW.
REFERENCES
- 1.Judd LL, Akiskal HS, Paulus MP. The role and clinical significance of subsyndromal depressive symptoms (SSD) in unipolar major depressive disorder. J Affect Disord. 1997;45:5–17. doi: 10.1016/s0165-0327(97)00055-4. [DOI] [PubMed] [Google Scholar]
- 2.Judd LL, Akiskal HS, Maser JD, et al. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. J Affect Disord. 1998;50:97–108. doi: 10.1016/s0165-0327(98)00138-4. [DOI] [PubMed] [Google Scholar]
- 3.Paykel ES, Ramana R, Cooper Z, Hayhurst H, Kerr J, Barocka A. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995;25:1171–80. doi: 10.1017/s0033291700033146. [DOI] [PubMed] [Google Scholar]
- 4.Judd LL, Paulus MJ, Schettler PJ, et al. Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? Am J Psychiatry. 2000;157:1501–4. doi: 10.1176/appi.ajp.157.9.1501. [DOI] [PubMed] [Google Scholar]
- 5.Nierenberg AA, Wright EC. Evolution of remission as the new standard in the treatment of depression. J Clin Psychiatry. 1999;60:7–11. [PubMed] [Google Scholar]
- 6.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 7.Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–51. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- 8.Katz MM, Meyers AL, Prakash A, Gaynor PJ, Houston JP. Early symptom change prediction of remission in depression treatment. Psychopharmacol Bull. 2009;42:94–107. [PubMed] [Google Scholar]
- 9.Grilo CM, Sanislow CA, Shea MT, et al. Two-year prospective naturalistic study of remission from major depressive disorder as a function of personality disorder comorbidity. J Consult Clin Psychol. 2005;73:78–85. doi: 10.1037/0022-006X.73.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Brien EM, Chelminski I, Young D, Dalrymple K, Hrabosky J, Zimmerman M. Severe insomnia is associated with more severe presentation and greater functional deficits in depression. J Psychiatric Res. 2011;45:1101–5. doi: 10.1016/j.jpsychires.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Agargun MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–51. doi: 10.4088/jcp.v58n0602. [DOI] [PubMed] [Google Scholar]
- 12.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–6. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 13.Li SX, Lam SP, Chan JW, Yu MW, Wing YK. Residual sleep disturbances in patients remitted from major depressive disorder: a 4-year naturalistic follow-up study. Sleep. 2012;35:1153–61. doi: 10.5665/sleep.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42:209–12. doi: 10.1016/s0165-0327(96)01411-5. [DOI] [PubMed] [Google Scholar]
- 15.Monteleone P, Maj M. The circadian basis of mood disorders: recent developments and treatment implications. Eur Neuropsychopharmacol. 2008;18:701–11. doi: 10.1016/j.euroneuro.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Pandi-Perumal SR, Moscovitch A, Srinivasan V, Spence DW, Cardinali DP, Brown GM. Bidirectional communication between sleep and circadian rhythms and its implications for depression: lessons from agomelatine. Prog Neurobiol. 2009;88:264–71. doi: 10.1016/j.pneurobio.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 17.Hickie IB, Rogers NL. Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet. 2011;378:621–31. doi: 10.1016/S0140-6736(11)60095-0. [DOI] [PubMed] [Google Scholar]
- 18.Chelminski I, Ferraro FR, Petros TV, Plaud JJ. An analysis of the “eveningness-morningness” dimension in “depressive” college students. J Affect Disord. 1999;52:19–29. doi: 10.1016/s0165-0327(98)00051-2. [DOI] [PubMed] [Google Scholar]
- 19.Hidalgo MP, Caumo W, Posser M, Coccaro SB, Camozzato AL, Chaves ML. Relationship between depressive mood and chronotype in healthy subjects. Psychiatry Clin Neurosci. 2009;63:283–90. doi: 10.1111/j.1440-1819.2009.01965.x. [DOI] [PubMed] [Google Scholar]
- 20.Hirata FC, Lima MC, de Bruin VM, Nobrega PR, Wenceslau GP, de Bruin PF. Depression in medical school: the influence of morningnesseveningness. Chronobiol Int. 2007;24:939–46. doi: 10.1080/07420520701657730. [DOI] [PubMed] [Google Scholar]
- 21.Gaspar-Barba E, Calati R, Cruz-Fuentes CS, et al. Depressive symptomatology is influenced by chronotypes. J Affect Disord. 2009;119:100–6. doi: 10.1016/j.jad.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 22.Gau SS, Shang CY, Merikangas KR, Chiu YN, Soong WT, Cheng AT. Association between morningness-eveningness and behavioral/emotional problems among adolescents. J Biol Rhythms. 2007;22:268–74. doi: 10.1177/0748730406298447. [DOI] [PubMed] [Google Scholar]
- 23.Selvi Y, Aydin A, Boysan M, Atli A, Agargun MY, Besiroglu L. Associations between chronotype, sleep quality, suicidality, and depressive symptoms in patients with major depression and healthy controls. Chronobiol Int. 2010;27:1813–28. doi: 10.3109/07420528.2010.516380. [DOI] [PubMed] [Google Scholar]
- 24.Lam SP, Fong SY, Ho CK, Yu MW, Wing YK. Parasomnia among psychiatric outpatients: a clinical, epidemiologic, cross-sectional study. J Clin Psychiatry. 2008;69:1374–82. doi: 10.4088/jcp.v69n0904. [DOI] [PubMed] [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 26.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48:851–5. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 28.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 29.Zhang B, Hao YL, Wing YK. The reliability and validity of Chinese Version Morningness Eveningness Questionnaire. Chin J Behav Med Sci. 2006;15:856–8. (in Chinese) [Google Scholar]
- 30.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung KF, Kan KK, Yeung WF. Assessing insomnia in adolescents: comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med. 2011;12:463–70. doi: 10.1016/j.sleep.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 32.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 33.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 34.Leung CM, Wing YK, Kwong PK, Lo A, Shum K. Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison with the Hamilton Rating Scale of Depression. Acta Psychiatr Scand. 1999;100:456–61. doi: 10.1111/j.1600-0447.1999.tb10897.x. [DOI] [PubMed] [Google Scholar]
- 35.Troxel WM, Kupfer DJ, Reynolds CF, 3rd, et al. Insomnia and objectively measured sleep disturbances predict treatment outcome in depressed patients treated with psychotherapy or psychotherapy-pharmacotherapy combinations. J Clin Psychiatry. 2012;73:478–85. doi: 10.4088/JCP.11m07184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang J, Li AM, Kong AP, Lai KY, Tang NL, Wing YK. A community-based study of insomnia in Hong Kong Chinese children: Prevalence, risk factors and familial aggregation. Sleep Med. 2009;10:1040–6. doi: 10.1016/j.sleep.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 37.Zhang J, Lam SP, Li SX, et al. Long-term outcomes and predictors of chronic insomnia: a prospective study in Hong Kong Chinese adults. Sleep Med. 2012;13:455–62. doi: 10.1016/j.sleep.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 38.Carney CE, Segal ZV, Edinger JD, Krystal AD. A comparison of rates of residual insomnia symptoms following pharmacotherapy or cognitive-behavioral therapy for major depressive disorder. J Clin Psychiatry. 2007;68:254–60. doi: 10.4088/jcp.v68n0211. [DOI] [PubMed] [Google Scholar]
- 39.Iovieno N, van Nieuwenhuizen A, Clain A, Baer L, Nierenberg AA. Residual symptoms after remission of major depressive disorder with fluoxetine and risk of relapse. Depress Anxiety. 2011;28:137–44. doi: 10.1002/da.20768. [DOI] [PubMed] [Google Scholar]
- 40.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia:update of the recent evidence (1998-2004) Sleep. 2006;29:1398–414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 41.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suh S, Nowakowski S, Bernert RA, et al. Clinical significance of night-to-night sleep variability in insomnia. Sleep Med. 2012;13:469–75. doi: 10.1016/j.sleep.2011.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 2007;3:289–94. [PMC free article] [PubMed] [Google Scholar]
- 44.Tonetti L, Fabbri M, Natale V. Relationship between circadian typology and big five personality domains. Chronobiol Int. 2009;26:337–47. doi: 10.1080/07420520902750995. [DOI] [PubMed] [Google Scholar]
- 45.Adan A, Natale V, Caci H, Prat G. Relationship between circadian typology and functional and dysfunctional impulsivity. Chronobiol Int. 2010;27:606–19. doi: 10.3109/07420521003663827. [DOI] [PubMed] [Google Scholar]
- 46.Prat G, Adan A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiol Int. 2011;28:248–57. doi: 10.3109/07420528.2011.553018. [DOI] [PubMed] [Google Scholar]
- 47.Even C, Schroder CM, Friedman S, Rouillon F. Efficacy of light therapy in nonseasonal depression: a systematic review. J Affect Disord. 2008;108:11–23. doi: 10.1016/j.jad.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 48.Martiny K, Refsgaard E, Lund V, et al. A 9-week randomized trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetine. J Clin Psychiatry. 2012;73:1234–42. doi: 10.4088/JCP.11m07625. [DOI] [PubMed] [Google Scholar]
- 49.Ehlers CL, Kupfer DJ, Frank E, Monk TH. Biological rhythms and depression: The role of zeitgebers and zeitstorers. Depress Anxiety. 1993;1:285–93. [Google Scholar]
- 50.Frank E. Interpersonal and social rhythm therapy: a means of improving depression and preventing relapse in bipolar disorder. J Clin Psychol. 2007;63:463–73. doi: 10.1002/jclp.20371. [DOI] [PubMed] [Google Scholar]
- 51.Selvi Y, Gulec M, Agargun MY, Besiroglu L. Mood changes after sleep deprivation in morningness-eveningness chronotypes in healthy individuals. J Sleep Res. 2007;16:241–4. doi: 10.1111/j.1365-2869.2007.00596.x. [DOI] [PubMed] [Google Scholar]
- 52.Baehr EK, Revelle W, Eastman CI. Individual differences in the phase and amplitude of the human circadian temperature rhythm: with an emphasis on morningness-eveningness. J Sleep Res. 2000;9:117–27. doi: 10.1046/j.1365-2869.2000.00196.x. [DOI] [PubMed] [Google Scholar]
- 53.Griefahn B. The validity of the temporal parameters of the daily rhythm of melatonin levels as an indicator of morningness. Chronobiol Int. 2002;19:561–77. doi: 10.1081/cbi-120004226. [DOI] [PubMed] [Google Scholar]


