Abstract
Study Objectives:
To examine the patterns of insomnia and sleep-related movement from ages 4.5 to 9 years, their concurrent associations with mental health symptoms in childhood, and the longitudinal associations of sleep-problem persistence with mental health symptoms at ages 9 and 18 years.
Design:
A 14-year prospective follow-up study. Assessments included maternal report on the Children's Sleep Habits Questionnaire at ages 4.5 and 9, and child mental health symptoms via maternal report at age 4.5, multi-informant (child, teacher, mother) report at age 9, and adolescent report at age 18.
Setting:
Community.
Participants:
A total of 396 children (51% female).
Interventions:
N/A.
Measurements and Results:
Sleep problems were more common at age 4.5 than 9; symptoms of insomnia and abnormal sleep movement both had persistence rates of 9–10%. At age 4.5, insomnia was associated with hostile-aggressive and hyperactive-distractible behavior, but there were no significant associations for sleep movement. At age 9, both insomnia and sleep movement were associated with symptoms of depression, externalizing, and attention deficit hyperactivity disorder (ADHD). Insomnia persistence was associated with symptoms of depression, externalizing, and ADHD at age 9 and anxiety and externalizing at age 18; sleep- movement persistence was associated with externalizing and ADHD at age 9, and ADHD at age 18. The age 18 persistence effects for insomnia and anxiety and for sleep movement and ADHD were significant when controlling for earlier mental health.
Conclusions:
Childhood insomnia and sleep movement are common and associated with mental health symptoms. Their persistence from middle to late childhood predicts associations with specific types of mental health symptoms at age 18.
Citation:
Armstrong JM, Ruttle PL, Klein MH, Essex MJ, Benca RM. Associations of child insomnia, sleep movement, and their persistence with mental health symptoms in childhood and adolescence. SLEEP 2014;37(5):901-909.
Keywords: adolescence, anxiety, attention deficit hyperactivity disorder, childhood, depression, externalizing, insomnia, longitudinal, sleep-related movement
INTRODUCTION
Child sleep difficulties have been associated with emotional and behavioral problems,1–3 echoing findings in adolescents4–6 and adults.7–10 Sleep problems are prevalent in childhood, and aspects of insomnia, such as difficulties with sleep onset, nighttime awakening, and morning awakening, are among the most common nonrespiratory sleep problems during the preschool and early school years.11,12 Sleep-related movements are often observed among children as well.13,14 In contrast, the prevalence of parasomnias, such as night terrors and enuresis, is lower and diminishes further with age13,14; hypersomnia is also uncommon in childhood.15 Prior research has linked prevalent child sleep difficulties to a range of mental health problems. For example, childhood insomnia has been linked to anxiety,16 depression,17,18 conduct problems and aggression,19 and attention deficit hyper-activity disorder (ADHD).20,21 Similarly, associations have been found for sleep-related movement, with restless sleep associated with mood and anxiety disorders22 and ADHD,20,21 and bruxism related to internalizing13,23,24 as well as bad temper and hyperactivity.25
Most of this work, though, has been cross-sectional or occasionally retrospective, with little prospective longitudinal research examining the links between childhood sleep problems and mental health later in life. There is some shorter-term longitudinal work, linking persistent sleep problems at age 4–5 years to emotional and behavioral problems 2 years later26 and connecting sleep problems at age 8 to depression and/or anxiety at age 10.27,28 Longer-term research includes several studies led by Gregory. In one, persistent sleep problems across childhood (ages 5 and/or 7 and age 9) predicted increased rates of anxiety—but not depressive—disorders in early adulthood.29 In two others, preschool sleep problems predicted elevated anxiety, conduct problems, and hyperactivity at age 730 and similar emotional problems at age 15.31 Echoing this work, two studies led by Wong found that sleep problems in preschool and later childhood predicted internalizing and externalizing problems during childhood and early adolescence.32,33
Although this work suggests that childhood sleep problems, especially persistent ones, may have implications for later mental health problems, each of these prior studies has been limited by reliance on nonspecific, global measures of sleep difficulties. Rather than assessing particular types of sleep problems, these studies used items about unspecified “sleep problems,” “sleeping difficulties,” and/or “trouble sleeping,” sometimes combined with additional questions about insomnia, hypersomnia, somnambulism, somniloquy, and/or nightmares. Only one recent longitudinal study focused specifically on insomnia, linking persistent insomnia to poorer mental health at its second assessment (average age 14) while controlling for mental health at baseline (average age 9).34 The mental health measures in that study were limited, however, with an undifferentiated global mental health score examined alongside single items for hyperactivity and temper outbursts.
Thus, as outlined above and noted recently by others,27,35 most of the research on childhood sleep problems and mental health is limited to cross-sectional or retrospective studies, and existing prospective longitudinal work has used relatively nonspecific sleep measures and/or more global mental health measures. Further, these studies typically consider a limited number of assessment times that often cover short periods of development. As a result, the prevalence and patterns of persistence of child sleep problems over time and the connections between specific childhood sleep problems and specific current, and especially later, mental health symptoms are not well understood.
The current study seeks to begin addressing these gaps in the literature by using a well-established measure of specific, common child sleep problems alongside well-validated measures of specific child and adolescent mental health problems; by employing data analytic strategies that minimize measurement artifacts and consider possible confounding variables; and by utilizing assessments that extend from middle and late childhood into adolescence. The current study considers three main questions. First, what are the patterns of insomnia and sleep-related movement from ages 4.5 to 9 in a community sample? Second, what are the concurrent associations of these specific sleep problems with specific types of mental health symptoms at each age? Third, what are the associations of longitudinal patterns (i.e., persistence) of these sleep problems with mental health symptoms at ages 9 and 18?
METHODS
Participants
Subjects were drawn from the Wisconsin Study of Families and Work (originally called the Wisconsin Maternity Leave and Health Project36), a community sample of 570 families recruited from health care clinics in the Milwaukee (80%) and Madison (20%) areas and followed from mothers' second trimester of pregnancy through child age 18 years. Based on the study's original focus on work and parental leave, eligible mothers were cohabiting with the baby's father, either working for pay/profit or full-time homemakers, and older than 18. The current study includes the 396 families with complete childhood sleep data, 341 of whom also have mental health data at age 18. At each assessment, children selected a toy as a thank-you gift, and adolescents and adults were paid for completing study activities. Informed consent and parental permission for minors were obtained at each assessment. All procedures were reviewed and approved by the University of Wisconsin Institutional Review Board.
Insomnia and Sleep Movement
At child ages 4.5 and 9 years, childhood sleep problems were measured via mother-report with a version of the widely used and well-validated37,38 Children's Sleep Habits Questionnaire.39 Sleep problems covered included insomnia, sleep movement, hypersomnia, and a range of parasomnias, and a single question assessed snoring (“Child snores loudly”). However, the prevalence of persistent hypersomnia (4.5%) and persistent parasomnias (2.8%) was too low for consideration here, because of problems related to limited power and imbalanced cell sizes.
For each item, mothers reported how often children exhibited the sleep behavior during the most recent typical week. Five symptoms of insomnia and three types of sleep-related movement were assessed (Tables 1 and 2). Responses were scored as 1 (“Usually, 5–6 times a week” or “Always, 7 times a week”) or 0 (“Never, less than once a week”; “Rarely, once a week”; or “Sometimes, 2–4 times a week”). At each age, cases of insomnia were defined as the presence of one or more symptoms, as were cases of sleep movement. Insomnia persistence was then defined based on whether children had exhibited insomnia at neither, either, or both ages 4.5 and 9, and sleep-movement persistence was similarly defined.
Table 1.
Overall sleep-problem prevalence and persistence (n = 396)
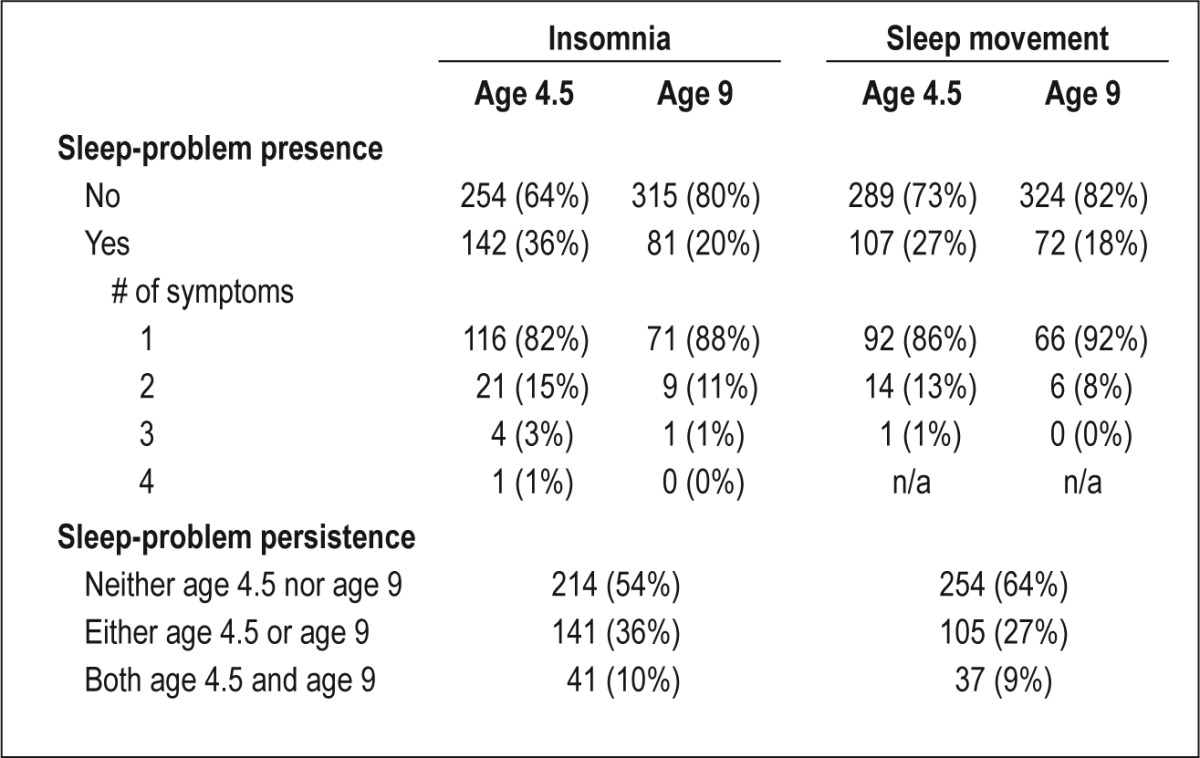
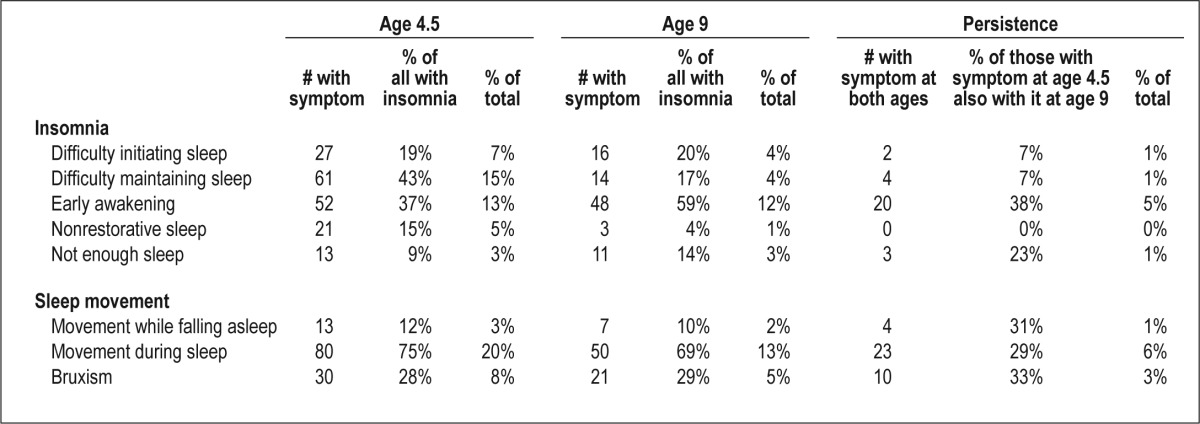
Table 2.
Item-level sleep-problem prevalence and persistence (n = 396)
Mental Health Symptoms
At child age 4.5, mothers completed the Preschool Behavior Questionnaire (PBQ),40 which yields three summed scores: anxious-fearful (nine items; e.g., “Is worried, worries about many things,” “Cries easily”), hostile-aggressive (11 items; e.g., “Is disobedient,” “Fights with other children”), and hyper-active-distractible (four items; e.g., “Has poor concentration or short attention span,” “Squirmy, fidgety child”).
At child age 9, mothers, teachers, and children reported on child mental health symptoms using the MacArthur Health and Behavior Questionnaire (HBQ).41,42 At age 18, adolescents themselves completed an age-appropriate version of the HBQ. The four HBQ scales considered here are anxiety, computed as the mean of generalized anxiety (seven to 13 items; e.g., “Nervous, high-strung, or tense”) and either social inhibition at age 9 (five items; e.g., “Gets quiet around children he/she does not know”) or social anxiety at age 18 (12 items; social-inhibition items plus others, e.g., “I try to get out of doing things in front of others”); depression (11 to 13 items; e.g., “Unhappy, sad, or depressed,” “Feels worthless or inferior”); externalizing, computed as the mean of oppositional defiant (six to 10 items; e.g., “Argues a lot with adults”), conduct problems (nine to 12 items; e.g., “Lies or cheats”), and overt aggression (four to eight items; e.g., “Taunts and teases other children”); and ADHD, computed as the mean of inattention (five to nine items; e.g., “Cannot concentrate, cannot pay attention for long”) and impulsivity (six to nine items; e.g., “Impulsive or acts without thinking”).
The adult- and child-report HBQ instruments were developed in tandem to provide parallel measures across respondents. Multi-informant scores at age 9, derived using principal components analysis (PCA) for each scale, provide a measure of each characteristic that is more reliable and valid than scores based on a single reporter or a combinational approach that does not control extraneous variance.43 To retain the largest sample, subjects were included in analyses at age 9 if HBQ data were available from at least two reporters. Thus, as in earlier work,44 multi-informant scores comprising mother-, teacher-and child-reports were used where available (n = 354), and PCA-derived scores employing data from mother and teacher (n = 7) or mother and child (n = 28) were used for cases with one missing reporter; seven cases with neither teacher- nor child-report data were excluded from age 9 analyses.
Items potentially confounded with the sleep problems examined here were omitted from scale scores to avoid inflated associations due to measurement overlap, i.e., insomnia-related items were dropped from the measures of generalized anxiety (e.g., “I have trouble sleeping”) and depression (e.g., “Underactive, slow-moving, or lacks energy”). Additionally, in secondary analyses reported below, consideration was given to potential connections between sleep movement and daytime movement-related symptoms of ADHD assessed on the HBQ impulsivity subscale (two items per reporter, e.g., “Fidgets” and “Cannot stay seated when required to do so”).
Psychostimulant Use
At age 9, mothers reported on children's current medication use, and open-ended responses were double-coded by investigators and trained research assistants. Regular use of psychostimulants (i.e., amphetamine and dextroamphetamine [Adderall]; methylphenidate [Ritalin]) was coded as yes (1) or no (0). In secondary analyses reported below, consideration was given to the possible role of psychostimulants in the association of sleep problems and mental health symptoms.
Analytic Plan and Preliminary Analyses
Item-level missing data were minimal; scores were computed for respondents who answered at least 75% of the items on a given scale. Descriptive statistics were produced, and data were inspected to screen for violations of statistical assumptions. Four multivariate analyses of variance (MANOVAs) were run to examine the overall associations of (1) age 4.5 concurrent sleep problems and mental health symptoms; (2) age 9 concurrent sleep problems and mental health symptoms; (3) sleep-problem persistence and age 9 mental health symptoms; and (4) sleep-problem persistence and age 18 mental health symptoms. Univariate analyses of variance (ANOVAs) were examined to probe significant multivariate findings, and post hoc comparisons used Bonferroni correction for multiple testing as appropriate. In addition, for significant univariate findings at age 18, ANCOVAs were conducted to ascertain whether effects persisted when controlling for age 9 levels of the outcome of interest.
After examining descriptive statistics, all outcome variables were transformed with a base-10 logarithm to normalize positively skewed distributions and ensure the homogeneity of variance and equality of variance-covariance matrices. Multivariate outliers were screened by computing Mahalanobis distance for each case on the outcome variables, and two potential outliers were identified at age 18; although the overall pattern of results was unchanged with their inclusion or omission, these cases were excluded from age 18 analyses to limit the influence of extreme values.
In a set of secondary analyses, primary analyses were repeated as MANCOVAs to separately rule out possible effects of snoring and psychostimulants and moderation by child sex, and analyses were re-run with the ADHD daytime movement items omitted given their similarity to some of the sleep movement items. Including snoring in the models described below did not produce significant associations between snoring and outcomes, nor did it change the pattern of other results. The pattern of results was also unchanged when childhood psycho-stimulant use was included as a covariate, with all major findings remaining significant or nearly so; e.g., all univariate associations between ADHD and sleep movement or sleep-movement persistence were significant at P ≤ 0.056. Further, multivariate analyses found no significant moderation by child sex of the associations between sleep problems and outcomes. Finally, the patterns of association were unchanged when daytime movement items were omitted from the HBQ ADHD scale, with all major findings remaining significant.
RESULTS
Sample Characteristics
At recruitment (1990–1991) during the prenatal period, 15% of the 396 mothers and 18% of the fathers had a high-school degree or less, 27% and 31% had some college, and 58% and 51% had at least a 4-y college degree; median annual family income was $48,000 (range = $7,500 to $200,000+); mothers' average age was 29.6 years (standard deviation [SD] = 4.3) and fathers' average age was 31.6 years (SD = 5.3); 96% of couples were married; and most were non-Hispanic caucasians (89%). Participating youth are almost evenly divided between females (201, 51%) and males (195, 49%). The 396 participants and the remainder were not significantly different on most demographics, although participating parents on average were slightly older (0.9 years for mothers, 1.1 years for fathers, P < 0.05) and had slightly more education (0.5 years for mothers and fathers, P < 0.05). Among participants, there were no differences in either demographics or proportion with childhood sleep problems among those with and without data at age 18.
Patterns of Childhood Sleep Problems
Table 1 presents the overall prevalence of sleep problems at ages 4.5 and 9 and their persistence. More children had insomnia at age 4.5 than 9 (36% versus 20%, respectively), and the same was true for sleep movement (27% versus 18%, respectively). Among those with a given sleep problem at each age, most were characterized by only one symptom, with only 8–18% experiencing two or more symptoms. Approximately one third of children (36%) experienced insomnia at either age 4.5 or 9, with 10% at both times and the remainder at neither. Approximately one fourth (27%) experienced sleep movement at either age, and 9% at both ages.
Table 2 details item-level prevalence and persistence of sleep problems. The most common insomnia symptoms at age 4.5 were difficulty maintaining sleep and early awakening, the latter of which was also most common at age 9. At both ages, the most common sleep movement symptom was movement during sleep. Early awakening was the most persistent insomnia symptom, with 38% of children who exhibited it at age 4.5 also doing so at age 9. The three sleep movement symptoms were persistent at rates similar to one another, i.e., 29–33% of children with a given symptom at age 4.5 also exhibited it at age 9.
Possible sex differences in the prevalence of sleep problems and their persistence were examined in a series of chi-square tests, which yielded no significant findings (P = 0.13–0.82).
Associations of Childhood Concurrent Sleep Problems With Mental Health Symptoms
Multivariate and univariate results for concurrent sleep problems are presented in Table 3. In the MANOVA for age 4.5, insomnia was significantly associated with PBQ mental health symptoms; probing via univariate ANOVAs indicated that insomnia was significantly associated with hostile-aggressive and hyperactive-distractible; insomnia and anxious-fearful were not significantly associated. In pairwise comparisons, children with insomnia at age 4.5 scored higher on average than those without on the measures of hostile-aggressive (mean ± SD; 0.81 ± 0.26 versus 0.73 ± 0.30) and hyperactivedistractible (0.58 ± 0.23 versus 0.50 ± 0.26). For sleep movement, the MANOVA produced no significant association with mental health symptoms at age 4.5.
Table 3.
Multivariate and univariate results associating childhood sleep problems with mental health symptoms
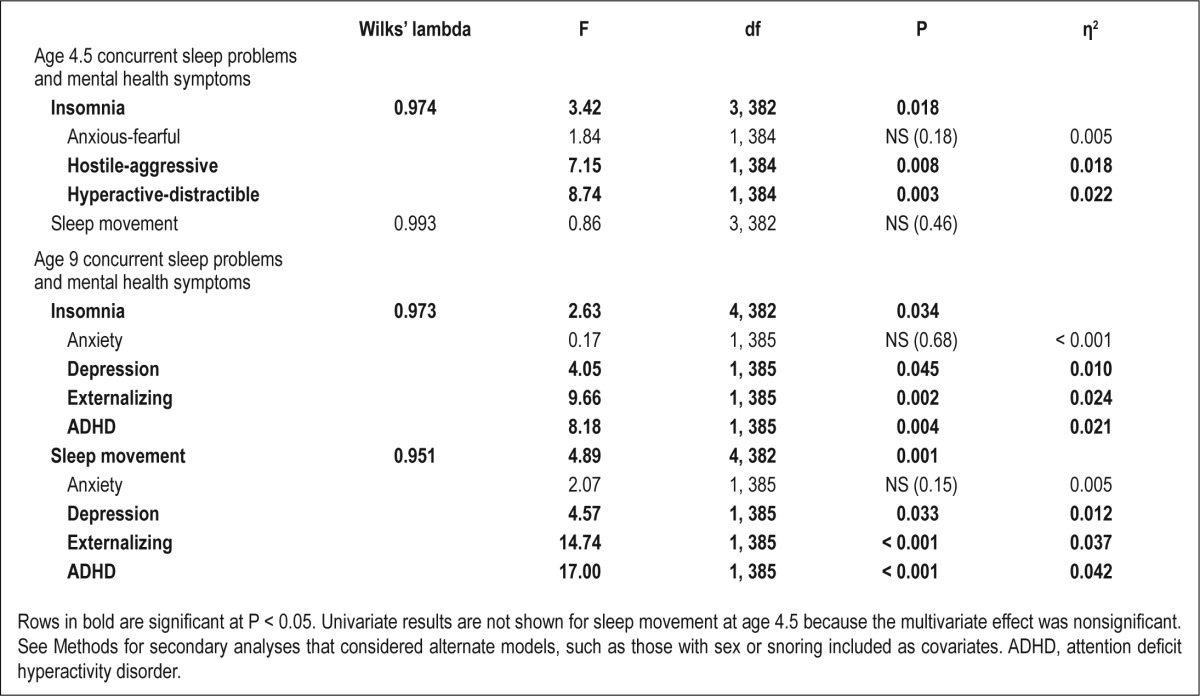
At age 9, there was a significant multivariate association between insomnia and HBQ mental health symptoms, and univariate ANOVAs indicated that insomnia was significantly associated with depression, externalizing, and ADHD; insomnia was not significantly associated with anxiety. In pairwise comparisons probing the significant univariate effects, children with insomnia scored higher than those without on the measures of depression (0.48 ± 0.15 versus 0.45 ± 0.12), externalizing (0.50 ± 0.14 versus 0.44 ± 0.13), and ADHD (0.50 ± 0.13 versus 0.44 ± 0.14). Along with the insomnia findings, the MANOVA also yielded a significant association between sleep movement and mental health symptoms. Like insomnia, sleep movement was significantly associated with depression, externalizing, and ADHD but not anxiety. Children with sleep movement at age 9 scored higher than those without on the measures of depression (0.48 ± 0.14 versus 0.45 ± 0.12), externalizing (0.52 ± 0.13 versus 0.44 ± 0.14), and ADHD (0.52 ± 0.12 versus 0.44 ± 0.14).
Associations of Childhood Sleep-Problem Persistence With Mental Health Symptoms
Multivariate and univariate results for sleep-problem persistence are reported in Table 4. Insomnia persistence was significantly associated with age 9 mental health symptoms overall, and univariate ANOVAs indicated that insomnia persistence was significantly associated with depression, externalizing, and ADHD but not anxiety. In post hoc tests using Bonferroni correction for multiple testing, children with insomnia at both age 4.5 and 9 scored higher than those with insomnia at neither time on the depression measure (both, 0.50 ± 0.15, versus neither, 0.44 ± 0.12, adjusted P = 0.019; both versus either, 0.45 ± 0.13, adjusted P = 0.061). Children with persistent insomnia also scored higher than those without on the measures of externalizing (both times, 0.54 ± 0.15, versus neither, 0.44 ± 0.13, adjusted P < 0.001; both versus either, 0.46 ± 0.14, adjusted P = 0.004) and ADHD (both, 0.53 ± 0.13, versus neither, 0.43 ± 0.14, adjusted P < 0.001; both versus either, 0.46 ± 0.14, adjusted P = 0.034). As reported in Table 4, sleep-movement persistence was also associated with age 9 mental health symptoms overall, and ANOVAs indicated that it was significantly associated with externalizing and ADHD; it was not significantly associated with either anxiety or depression. In post hoc tests, children with sleep movement at both ages 4.5 and 9 scored higher than those with sleep movement at neither age on the measures of externalizing (both 0.52 ± 0.13, versus neither, 0.45 ± 0.14, adjusted P = 0.005; both versus either, 0.46 ± 0.14, adjusted P = 0.053) and ADHD (both, 0.51 ± 0.13, versus neither, 0.44 ± 0.14, adjusted P = 0.008; both versus either, 0.47 ± 0.13, adjusted P = 0.53).
Table 4.
Multivariate and univariate results associating childhood sleep-problem persistence with mental health symptoms
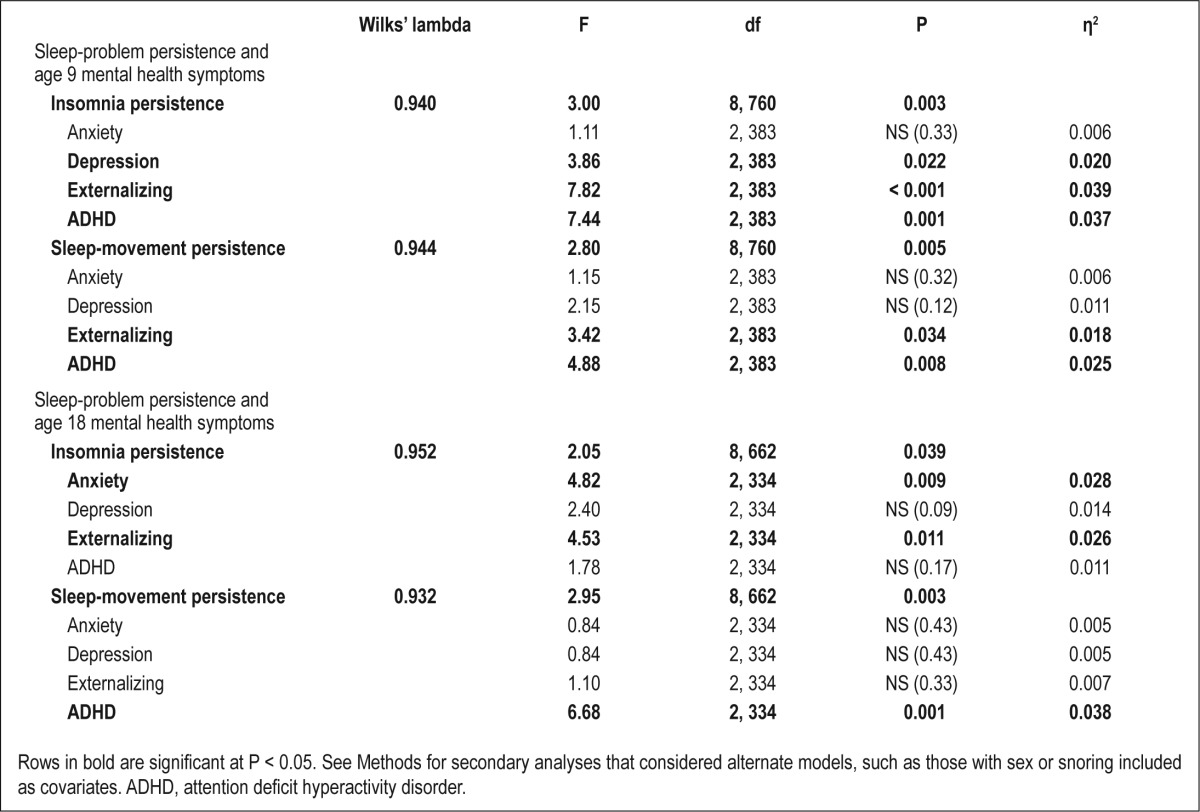
Insomnia persistence was significantly associated with mental health symptoms at age 18. ANOVAs indicated that insomnia persistence was significantly associated with adolescent anxiety and externalizing but neither depression nor ADHD. Bonferroni-corrected post hoc tests revealed that children with insomnia at both age 4.5 and 9 scored higher on the anxiety measure (0.45 ± 0.12) than those with insomnia at neither age (0.38 ± 0.14, adjusted P = 0.016) or either age (0.37 ± 0.14, adjusted P = 0.004); see Figure 1A. Similarly, children with insomnia at both ages scored higher on the adolescent externalizing measure (0.31 ± 0.11) than those with insomnia at neither age (0.23 ± 0.13, adjusted P = 0.007) or either age (0.23 ± 0.13, adjusted P = 0.010); see Figure 1B. In the age 18 MANOVA, there was also an overall association between sleep-movement persistence and mental health symptoms; as reported in Table 4, univariate ANOVAs showed that sleep-movement persistence was significantly associated only with ADHD, and not anxiety, depression, or externalizing. In post hoc tests, children with sleep movement at both ages (0.42 ± 0.14, adjusted P = 0.003) or either age (0.37 ± 0.15, adjusted P = 0.023) scored higher on ADHD than those with sleep movement at neither age (0.33 ± 0.15); see Figure 1C.
Figure 1.
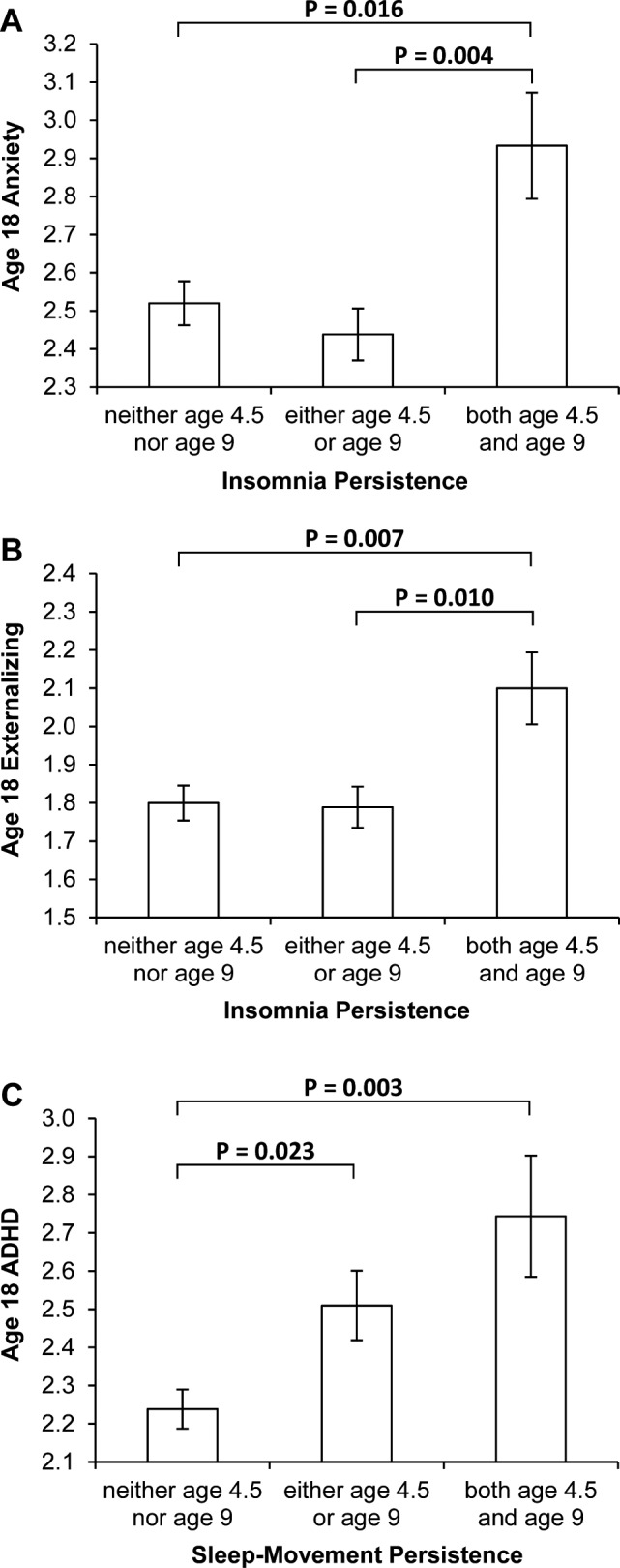
Post hoc comparisons for significant associations between sleep-problem persistence and age 18 mental health symptoms, specifically (A) insomnia persistence and anxiety, (B) insomnia persistence and externalizing, and (C) sleep-movement persistence and attention deficit hyperactivity disorder (ADHD). Although analyses were run on log-transformed variables, untransformed variables are graphed for easier interpretation. Whiskers represent ± 1 standard error of the mean and are centered on group means. P values reflect Bonferroni correction for multiple testing.
To further probe the significant effects at age 18, univariate ANCOVAs examined the effects of controlling on age 9 levels of the symptom in question. Insomnia persistence was significantly associated with age 18 anxiety when controlling for age 9 anxiety, F(2, 330) = 5.96, P = 0.003, η2 = 0.035. The association between insomnia persistence and age 18 externalizing was not significant when controlling for age 9 externalizing, F(2, 331) = 1.86, P = 0.16. Finally, sleep-movement persistence remained significantly associated with age 18 ADHD when age 9 ADHD was entered as a covariate, F(2, 331) = 3.87, P = 0.022, η2 = 0.023.
DISCUSSION
Sleep problems are common in childhood, and the current study of an unselected birth cohort found that insomnia and sleep-movement problems were reported for sizeable minorities of children at ages 4.5 and 9. Overall prevalence rates observed here and the occurrence of specific sleep-problem symptoms are consistent with prior studies of preschoolers and early elementary school students.13,14,45 Further, the prevalence of both insomnia and sleep movement diminished over time, consistent with epidemiological46 and longitudinal13 studies. From middle to late childhood, certain sleep problems may resolve for many children as their sleep regulatory systems mature.15 This idea is supported in the current study, particularly by the marked decrease over time in the number of children who had difficulty sleeping through the night. Nevertheless, a subset of children had sleep problems that continued over time; for insomnia and for sleep movement, 9–10% of children exhibited the problem at both ages 4.5 and 9.
Sleep difficulties were associated with an array of mental health symptoms in childhood. Insomnia in preschool was associated with externalizing and ADHD problems, and at age 9 both insomnia and sleep movement were associated with depression, externalizing, and ADHD symptoms. These cross-sectional findings are in line with the frequent clinical observation that childhood sleep difficulties and emotional and behavioral problems often present as a constellation of intertwined complaints that can be mutually exacerbating.47 However, sleep movement in preschool was not associated with mental health problems, suggesting that movement during sleep, movement while falling asleep, and/or nocturnal bruxism do not necessarily signal increased risk for co-occurring emotional or behavioral issues at age 4.5; however, associations were found at age 9 and, as discussed below, at ages 9 and 18 for sleep-movement persistence. Although there was little specificity at age 9 in the associations of insomnia, sleep movement, and their persistence with mental health symptoms, the associations of persistent child sleep problems with mental health at age 18 were specific, with unique associations for insomnia persistence compared with sleep-movement persistence. These findings are especially noteworthy given the strengths of the methodological design and data-analytic strategies detailed in the Methods section. Specifically, when considering possible confounding variables, such as snoring and psychostimulant use, the observed pattern of results was unchanged. Further, steps were taken to limit the problem of inflated associations due to measure overlap and shared method variance by, for example, excluding a number of sleep-related items from the mental health measures and pairing sleep data from mothers with mental health data from multiple informants at age 9 and adolescents themselves at age 18.
Children with insomnia at both ages 4.5 and 9 exhibited higher levels of anxiety symptoms at age 18 than those who had experienced no or only isolated insomnia; at age 18, children with persistent insomnia also reported elevated externalizing symptoms, but not depression or ADHD. The adolescent anxiety findings are striking in that no concurrent associations were found in childhood between either insomnia and anxiety or sleep movement and anxiety, nor were persistent sleep problems associated with anxiety at age 9. These age 18 findings are consistent with prior work that found recurrent (although nonspecific) sleep problems from ages 5 to 9 predictive of higher rates of anxiety disorders, but not depression, in early adulthood.29 As in that study, prediction here of later anxiety from childhood sleep problems was significant even when controlling for childhood symptom levels. The current study extends earlier reports regarding nonspecific sleep problems by associating persistent childhood insomnia with later anxiety symptoms, a finding that may provide clues regarding the developmental progression of anxiety in some children. The specificity of the link between early insomnia and later adolescent (rather than concurrent childhood) anxiety, and the lack of a link between persistent childhood insomnia and adolescent depression symptoms, suggests that processes may be at work that are unique to anxiety, despite its common comorbidity with mood disorders. Persistent childhood insomnia may represent subclinical, prodromal precursors of anxiety,29 perhaps reflecting the beginning of the presleep cognitive arousal and hypervigilance that can lengthen sleep onset and disrupt deep sleep and that also have been theorized to underlie the development of anxiety.47,48 Childhood insomnia was also linked to externalizing symptoms at age 18, thus extending prior research.31,33 Childhood insomnia (rather than sleep problems generally), and especially persistent insomnia, was associated with externalizing at age 9 and age 18; the latter finding was not significant when controlling for age 9 externalizing, indicating that the age 9 finding persists into but is not further amplified in adolescence. Links between sleep problems and externalizing behaviors such as aggression, conduct problems, and oppositional-defiant behavior have received much less attention than other disorders such as anxiety, depression, and ADHD35 and thus is an area ripe for further study.
The connections between sleep-movement persistence and mental health tell a somewhat different story than insomnia. Sleep-movement persistence was associated with ADHD and externalizing symptoms at age 9 and only ADHD at age 18. The adolescent findings were significant even after controlling for earlier ADHD. Unlike insomnia, where children with childhood insomnia at both ages 4.5 and 9 had higher anxiety and externalizing symptom levels at age 18 than those with insomnia at neither or either age, children with persistent sleep movement in childhood as well as those with sleep movement limited to either age 4.5 or 9 had higher levels of ADHD symptoms in adolescence than children with no reported sleep movement. Although children with isolated versus persistent sleep movement were not significantly different on age 18 ADHD, visual inspection of Figure 1C suggests that, with a larger sample size and increased power, we might have detected a linear dose-response effect. Regardless, the findings suggest that childhood sleep movement is most closely associated with ADHD symptoms over time. Cross-sectional observational studies have previously found increased nocturnal motor activity among children with ADHD.49 The current findings suggest that the link between childhood sleep movement and ADHD extends well into adolescence. Further research is needed to better understand how sleep movement and ADHD are related, for example, by considering whether this association may be partially indicative of biological processes, such as dopaminergic dysfunction, that have been postulated to underlie both sleep problems and ADHD.21,49,50
Limitations and Strengths
There are several limitations of the current study. Only questionnaires were used to assess sleep, and findings may differ with other measures of sleep problems such as polysomnography and actigraphy. Further, prevalences of only persistent insomnia and persistent sleep movement were sufficient for study here, thus excluding other sleep difficulties from consideration. The relative ethnic/racial homogeneity of the sample also limits generalizability. Although the community setting of the current study provided an opportunity to study a sample that was not preselected, future research should seek to extend this work to clinical samples.
The study has a number of strengths as well. It used a well-established measure of child sleep problems to distinguish specific types of sleep disturbances, and repeated assessment allowed for consideration of the persistence of both insomnia and sleep movement from middle to late childhood. This study also carefully assessed mental health symptoms, with multi-informant measures at age 9 and adolescent self-report at age 18 that limited the problem of inflated associations due to shared variance with mother-report of child sleep problems. In addition, a series of secondary analyses helped rule out the possibility that observed effects were due to measurement artifacts or factors such as psychostimulant use. The study's prospective, longitudinal design enabled consideration of the associations of persistent childhood insomnia and sleep-related movement with child and adolescent mental health symptoms, most notably finding connections of childhood insomnia with anxiety at age 18 and childhood sleep movement with adolescent ADHD that remained significant after controlling for earlier mental health symptoms. These findings suggest that persistent sleep problems in childhood may provide an important opportunity for early intervention to help forestall the development of mental problems from childhood to adolescence. Future research should build on these findings to further explicate the ways that specific child sleep problems and mental health symptoms and disorders relate to one another over time.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by National Institutes of Health grants R01-MH044340, P50-MH052354, P50-MH069315, P50-MH084051, R21-MH082705, and P20-DA017589; the John D. and Catherine T. MacArthur Foundation Research Network on Psychopathology and Development; and the School of Medicine and Public Health and the Graduate School of the University of Wisconsin–Madison. Partial support for PLR was provided by the Canadian Institutes of Health Research Postdoctoral Fellowship. Dr. Benca has consulted for Merck. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Carvalho Bos S, Gomes A, Clemente V, et al. Sleep and behavioral/ emotional problems in children: a population-based study. Sleep Med. 2009;10:66–74. doi: 10.1016/j.sleep.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 2.Chervin RD, Archbold KH, Dillon JE, et al. Associations between symptoms of inattention, hyperactivity, restless legs, and periodic leg movements. Sleep. 2002;25:213–8. [PubMed] [Google Scholar]
- 3.Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/ depression in childhood. Psychiatry Res. 2000;94:93–102. doi: 10.1016/s0165-1781(00)00145-1. [DOI] [PubMed] [Google Scholar]
- 4.Itani O, Kaneita Y, Ikeda M, et al. Disorders of arousal and sleep-related bruxism among Japanese adolescents: a nationwide representative survey. Sleep Med. 2013;14:532–41. doi: 10.1016/j.sleep.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts RE, Duong HT. Depression and insomnia among adolescents: A prospective perspective. J Affect Disord. 2013;148:66–71. doi: 10.1016/j.jad.2012.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160:1147–56. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 9.Schredl M, Alm B, Sobanski E. Sleep quality in adult patients with attention deficit hyperactivity disorder (ADHD) Eur Arch Psychiatry Clin Neurosci. 2007;257:164–8. doi: 10.1007/s00406-006-0703-1. [DOI] [PubMed] [Google Scholar]
- 10.Soehner AM, Harvey AG. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. Sleep. 2012;35:1367–75. doi: 10.5665/sleep.2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore M, Allison D, Rosen CL. A review of pediatric nonrespiratory sleep disorders. Chest. 2006;130:1252–62. doi: 10.1378/chest.130.4.1252. [DOI] [PubMed] [Google Scholar]
- 12.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children: a community survey. Arch Pediatr Adolesc Med. 1997;151:473–80. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 13.Petit D, Touchette É, Tremblay RE, Boivin M, Montplaisir J. Dyssomnias and parasomnias in early childhood. Pediatrics. 2007;119:e1016–25. doi: 10.1542/peds.2006-2132. [DOI] [PubMed] [Google Scholar]
- 14.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115:241–9. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 15.Hoban TF. Sleep disorders in children. Ann N Y Acad Sci. 2010;1184:1–14. doi: 10.1111/j.1749-6632.2009.05112.x. [DOI] [PubMed] [Google Scholar]
- 16.Forbes EE, Bertocci MA, Gregory AM, et al. Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:148–55. doi: 10.1097/chi.0b013e31815cd9bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu X, Buysse DJ, Gentzler AL, et al. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep. 2007;30:83–90. doi: 10.1093/sleep/30.1.83. [DOI] [PubMed] [Google Scholar]
- 18.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:e60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 20.Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48:894–908. doi: 10.1097/CHI.0b013e3181ac09c9. [DOI] [PubMed] [Google Scholar]
- 21.Yoon SYR, Jain U, Shapiro C. Sleep in attention-deficit/hyperactivity disorder in children and adults: past, present, and future. Sleep Med Rev. 2012;16:371–88. doi: 10.1016/j.smrv.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Pullen SJ, Wall CA, Angstman ER, Munitz GE, Kotagal S. Psychiatric comorbidity in children and adolescents with restless legs syndrome: a retrospective study. J Clin Sleep Med. 2011;7:587–96. doi: 10.5664/jcsm.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106:67–74. doi: 10.1542/peds.106.1.67. [DOI] [PubMed] [Google Scholar]
- 24.Insana SP, Gozal D, McNeil DW, Montgomery-Downs HE. Community based study of sleep bruxism during early childhood. Sleep Med. 2013;14:183–8. doi: 10.1016/j.sleep.2012.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lam MHB, Zhang J, Li AM, Wing YK. A community study of sleep bruxism in Hong Kong children: association with comorbid sleep disorders and neurobehavioral consequences. Sleep Med. 2011;12:641–5. doi: 10.1016/j.sleep.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Quach J, Hiscock H, Canterford L, Wake M. Outcomes of child sleep problems over the school-transition period: Australian population longitudinal study. Pediatrics. 2009;123:1287–92. doi: 10.1542/peds.2008-1860. [DOI] [PubMed] [Google Scholar]
- 27.El-Sheikh M, Bub KL, Kelly RJ, Buckhalt JA. Children's sleep and adjustment: a residualized change analysis. Dev Psychol. 2013;49:1591–601. doi: 10.1037/a0030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gregory AM, Rijsdijk FV, Lau JYF, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32:189–99. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gregory AM, Caspi A, Eley TC, Moffitt TE, O'Connor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol. 2005;33:157–63. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- 30.Gregory AM, Eley TC, O'Connor TG, Plomin R. Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. J Am Acad Child Adolesc Psychiatry. 2004;43:744–51. doi: 10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- 31.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcohol Clin Exp Res. 2004;28:578–87. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- 33.Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009;10:787–96. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang J, Lam SP, Li SX, Li AM, Lai KYC, Wing Y-K. Longitudinal course and outcome of chronic insomnia in Hong Kong Chinese children: a 5-year follow-up study of a community-based cohort. Sleep. 2011;34:1395–402. doi: 10.5665/SLEEP.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16:129–36. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 36.Hyde JS, Klein MH, Essex MJ, Clark R. Maternity leave and women's mental health. Psychol Women Q. 1995;19:257–85. [Google Scholar]
- 37.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children's Sleep Habits Questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008;29:82–8. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- 38.Lewandowski AS, Toliver-Sokol M, Palermo TM. Evidence-based review of subjective pediatric sleep measures. J Pediatr Psychol. 2011;36:780–93. doi: 10.1093/jpepsy/jsq119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. [PubMed] [Google Scholar]
- 40.Behar L, Stringfield S. A behavior rating scale for the preschool child. Dev Psychol. 1974;10:601–10. [Google Scholar]
- 41.Boyce WT, Essex MJ, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. I: Exploring the “headwaters” of early life morbidities. J Am Acad Child Adolesc Psychiatry. 2002;41:580–7. doi: 10.1097/00004583-200205000-00016. [DOI] [PubMed] [Google Scholar]
- 42.Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. II: Developing the MacArthur Health and Behavior Questionnaire. J Am Acad Child Adolesc Psychiatry. 2002;41:588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 43.Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce WT, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: mixing and matching contexts and perspectives. Am J Psychiatry. 2003;160:1566–77. doi: 10.1176/appi.ajp.160.9.1566. [DOI] [PubMed] [Google Scholar]
- 44.Burk LR, Armstrong JM, Park J-H, Zahn-Waxler C, Klein MH, Essex MJ. Stability of early identified aggressive victim status in elementary school and associations with later mental health problems and functional impairments. J Abnorm Child Psychol. 2011;39:225–38. doi: 10.1007/s10802-010-9454-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fricke-Oerkermann L, Plück J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–7. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Dahl RE, Harvey AG. Sleep in children and adolescents with behavioral and emotional disorders. Sleep Med Clin. 2007;2:501–11. [Google Scholar]
- 48.Gregory AM, Willis TA, Wiggs L, Harvey AG. Presleep arousal and sleep disturbances in children. Sleep. 2008;31:1745–7. doi: 10.1093/sleep/31.12.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep Med. 2010;11:652–8. doi: 10.1016/j.sleep.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 50.Picchietti MA, Picchietti DL. Advances in pediatric restless legs syndrome: Iron, genetics, diagnosis and treatment. Sleep Med. 2010;11:643–51. doi: 10.1016/j.sleep.2009.11.014. [DOI] [PubMed] [Google Scholar]


