Abstract
Nutrition is a recognized determinant in 3 (ie, diseases of the heart, malignant neoplasms, cerebrovascular diseases) of the top 4 leading causes of death in the United States. However, many health care providers are not adequately trained to address lifestyle recommendations that include nutrition and physical activity behaviors in a manner that could mitigate disease development or progression. This contributes to a compelling need to markedly improve nutrition education for health care professionals and to establish curricular standards and requisite nutrition and physical activity competencies in the education, training, and continuing education for health care professionals. This article reports the present status of nutrition and physical activity education for health care professionals, evaluates the current pedagogic models, and underscores the urgent need to realign and synergize these models to reflect evidence-based and outcomes-focused education.
INTRODUCTION
The science of nutrition has evolved rapidly over the past 50 y. In an era that requires the practice of evidence-based medicine, there is now compelling evidence that lifestyle practices, including nutrition and physical activity behaviors, influence health and disease and contribute to the leading causes of death in the United States (1–5). Experimental, observational, and controlled clinical trials have contributed to the development of national policies that emphasize dietary recommendations for the prevention and treatment of diseases, especially chronic diseases such as cardiovascular disease, diabetes, cancer, and obesity (6–8). Furthermore, diet and physical activity interventions that were once considered limited in their potential impact for the prevention and treatment of chronic diseases have increasingly shown improvement and benefits that equal if not surpass those of pharmacologic intervention, often with less risk, reduced side effects, and lower costs (9–12). For example, there are many dietary interventions that have been shown to reduce the incidence, severity, and associated morbidity of hypertension (10), dyslipidemia (13, 14), type 2 diabetes (15), breast and colorectal cancers (16, 17), and obesity (18, 19). Furthermore, there are numerous examples of beneficial patient outcomes resulting from nutrition practices in inpatient, outpatient, and community settings. In acute care settings, best nutrition practices have been shown to improve patient outcomes and reduce health care costs (20). Moreover, Rosen et al (20) underscored the value of nutrition care before, during, and after hospitalization to help prevent and treat malnutrition, avert hospital-acquired conditions, reduce hospital readmissions, lower infection and complications rates, and shorten hospital stays. Finally, the Patient Protection and Affordable Care Act (ACA5; 21) mandates modernization of the disease prevention and public health systems. This law will shift health care away from a fee-for-service model to one that is focused on preventive care and wellness (22). In this new paradigm, nutrition is expected to be a central focus of health care in the future.
The importance of including nutrition in the training of health care professionals, as well as in the continuing education of practicing clinicians, remains a low priority. The absence of required medical nutrition education within medical and other health care curricula, and the lack of curricular coordination between health professions, bears witness to this problem. The current status of nutrition education for health care professionals in the United States and for physicians in other countries such as the United Kingdom is summarized in this supplement issue (23–26). There is a need for strategies to be developed and integrated into the education and training programs of health care professionals to attain a translational impact on disease prevention, treatment outcomes, and population health. Physician nutrition education is paramount because physicians typically drive the health care system in this country; and by generating greater awareness for the importance of nutrition in the prevention and treatment of disease, they can become greater proponents and sources of referral to other relevant health care professionals. There are cross-cutting and similar nutrition competencies for all health care professionals, and these could be updated and strategically aligned across disciplines to better provide a more standardized nutrition message to patients. These competencies are applicable to medical students, residents and fellows, nurses, advanced practice nurses, dietitians/nutritionists, pharmacists, physician assistants, dentists/dental hygienists, and exercise physiologists. Having common nutrition competencies across the health care disciplines can achieve a new paradigm for improving interdisciplinary, team-based health care that provides health care benefits.
THE EVOLUTION OF NUTRITION EDUCATION IN MEDICINE
The history of nutrition education for medical professionals is depicted in Table 1. Highlights of this history are briefly presented below. In addition, discussions of medical education (23) and graduate medical education and subspecialty training (25) are presented elsewhere in this supplement issue.
TABLE 1.
History of nutrition in the medical education of physicians1
| Year | Landmark activities | Accomplishments |
| 1963 | Council on Foods and Nutrition, AMA (30) | Recognizes the lack of support for nutrition education in medical schools |
| 1977 | AMA survey by Cyborski (31) | 19% of medical schools have a nutrition course |
| 1977 | NIH's Nutrition Coordinating Committee | Reported yearly research and training in nutrition |
| 1979 | Federal government support | Grant support for nutrition education, US code 1976 |
| 1982 | The LCME (33) | 37% of medical schools have a course in nutrition |
| 1983 | Survey by Young et al (27) | First national survey of practicing physicians and identification of physician core competencies |
| 1985 | National Academy of Sciences, National Research Council (29) | Recommends a separate 25-h nutrition course with reinforcement in clinical clerkships |
| 1989 | Committee on Medical and Dental School and Residency Nutrition Education, ASCN | Published 26 priority topics for incorporation in medical school curriculum including obesity, diet, hyperlipidemias and atherosclerosis, diet and diabetes, and pregnancy and lactation |
| 1989 | National Research Council (34) | Required that physicians acquire counseling skills on diet, nutrition, and healthy lifestyles to reduce chronic disease risk |
| 1989 | Survey by Weinsier et al (28) | National consensus of medical educators on priority content of nutrition in medical schools |
| 1990 | National Nutrition Monitoring and Research Act (Public Law 1101–445, HR 1608,§302) | Empowered US medical schools to include nutrition in the curriculum and provide training of medical students, residents, and fellows in clinical nutrition |
| 1991 | Healthy People 2000 Objectives (35) | Called for the provision and requirement of courses in human nutrition to all medical schools |
| 1995 | Weinsier (37) | Provided data for the development of a successful program in medical nutrition education |
| 1995–present | NIM, University of North Carolina, Chapel Hill | Developed a Web-based free, interactive, comprehensive nutrition curriculum for medical students (38) |
| 1996 | Nutrition and Preventive Medicine Task Force of the AMSA (32) | Provide a comprehensive list of 92 topics considered essentials for developing physicians’ competency in nutrition (publication in 1996) |
| 1996 | CNIP awards, ASN (39) | ASN offers an 8-wk mentored internship to increase the medical students exposure to clinical and academic aspects of nutrition |
| 1997 | Hark et al (40) survey of the updated USMLE | Review of nutrition content in the USMLE steps 1 and 2 |
| 1998 | Physician Nutrition Specialist awards (41) | Provides financial support for the educational role of an academic physician focusing his/her career in nutrition |
| 1998 | Intersociety Professional Nutrition Education Consortium (42) | Established educational standards, certification process, and monitoring for fellowship training of physician nutrition specialists; first meeting with ASCN at Experimental Biology 1998 |
| 2000–2005 | NAA from the NHLBI of the NIH (21 medical schools) (43) | Awards to 21 medical schools to develop and enhance the medical curricula in nutrition and the prevention of cardiovascular disease, diabetes, obesity, and other chronic disease (Am J Clin Nutr publications from 2001 to 2006) |
| 2002 | NBME approved a nutrition subscore for the step 1 USMLE (44) | Based on recommendations from various nutrition interest groups, including the Michigan Medical Nutrition Education Consortium and NAA members (Am J Clin Nutr publication in 2006) (see current USMLE content at http://www.usmle.org/bulletin/exam-content/) |
| 2005 | NHLBI and ASN | Convened a symposium at Experimental Biology |
| 2006 | Survey by Hark (45) | NAA physicians and nutritionists reviewed the USMLE steps 1, 2, and 3 exams and made nutrition subscore recommendations to the NBME |
| 2010 | ASPEN (46) | Convened a summit addressing the shortage of physician nutrition experts in the United States (J Parenter Enteral Nutr publications in 2010) |
| 2010 | Survey by Adams et al (36) | 27% of medical schools have a course in nutrition (publication in Acad Med 2010) |
| 2012 | USPSTF updated report (47) | “The USPSTF recommends intensive behavioral dietary counseling for adult patients with hyperlipidemia and other known risk factors for cardiovascular and diet-related chronic disease. Intensive counseling can be delivered by primary care clinicians or by referral to other specialists, such as nutritionists or dietitians.” Rating: B recommendation |
| 2012 | NHLBI group in nutrition education (48) | Convened a group of interdisciplinary nutrition education experts to develop/renew proactive approaches to medical and health care professional nutrition education and research (Am J Clin Nutr publications in 2014) |
| 2013 | New York Academy of Sciences (49) | Convened a workshop on the capacity building in nutrition science focusing on curricula for medical professionals (J NY Acad Sci publications in 2013) |
This list includes many steps in the history of nutrition in medicine but is not exhaustive. Many meetings, workshops, presentations, and publications including descriptions, evaluations, and guidelines have contributed to the advancement of this field and are not reported in this table. Examples include calls for action and guidelines provided by a variety of authors, alliances, institutions, and organizations with regard to obesity, diabetes, and lipid screening and management, as well as malnutrition in hospitals. AMA, American Medical Association; AMSA, American Medical Student Association; ASCN, American Society for Clinical Nutrition; ASPEN, American Society for Parenteral and Enteral Nutrition; CNIP, Clinical Nutrition Internship Program; LCME, Liaison Committee on Medical Education; NAA, Nutrition Academic Award; NBME, National Board of Medical Examiners; NHLBI, National Heart, Lung, and Blood Institute; NIM, Nutrition in Medicine; USMLE, US Medical Licensing Examination; USPSTF, US Preventive Services Task Force.
Medical education
In 1985, the Institute of Medicine (IOM) issued a report entitled “Nutrition Education in Medical Schools” (29). The committee recommended integration of a minimum of 25–30 h of nutrition into the 4-y medical school curriculum. Early leaders in the field of medical nutrition education, including Young et al (27), Weinsier et al (28), and Winick (50), proposed core nutrition topic areas for medical students and other physicians. The core topics were built on those outlined in the 1985 IOM Committee report: energy balance, the role of specific nutrients, nutrition through the life cycle, protein and energy needs, malnutrition, the role of nutrition in disease prevention and treatment, possible risks from poor dietary practices, and social and cultural factors that influence dietary practices (29). Feldman (51) and Kushner et al (52) were among early pioneers who addressed the need to teach nutrition in a manner that could be integrated throughout the medical school curriculum, including the development of clinical practice skills. In the 1990s, the American Medical Student Association established the Nutrition Curriculum Project and later published a national consensus report on the essentials of nutrition education in medical schools (32).
Notable by its creation and commitment to this cause, the Nutrition Academic Award (NAA) was developed and funded from 1998 through 2005 by the National Heart, Lung and Blood Institute (NHLBI), along with support from the National Institute of Diabetes and Digestive and Kidney Diseases (53). Modeled after the Preventive Cardiology Awards of the 1980s when the field was rapidly advancing and needed standardized, formalized training, 21 medical schools participated in the NAA to collaborate on medical nutrition education (54). The aims of the NAA (Table 2) provided the foundation for initiating a formalized approach, starting with agreement about the content of the nutrition curriculum for medical education. The NAA program achieved success through the development of new tools, syllabi, and practice guidelines that helped to facilitate nutrition education in this setting (http://www.nhlbi.nih.gov/funding/training/naa/products.htm). The contributions and advances made by the NAA were considerable; however, the lack of sustained funding, absence of a coordinating center, and competition for local resources slowed and, in some schools, eventually halted progress.
TABLE 2.
Aims of the NAA program1
| 1. Establish a network of US medical schools committed to developing more effective education and training in human nutrition |
| 2. Develop a Nutrition Curriculum Guide for Training Physicians, which identifies learning objectives for the major content areas that should be included in undergraduate and graduate medical curricula |
| 3. Implement medical school curricula to increase opportunities for students, residents, fellows, and faculty to learn nutrition principles and clinical practice skills and to address Continuing Medical Education and the training of other health care professionals |
| 4. Incorporate the most current clinical practice guidelines related to nutrition into physicians’ clinical competencies |
| 5. Create a range of educational and clinical practice tools for use by faculty in training health care professionals |
| 6. Evaluate medical school curricula, education materials, and other teaching tools for effectiveness and feasibility |
| 7. Establish a national website to make accessible teaching modules, patient care materials, and assessment and evaluation tools developed by the NAA program for use by any interested medical or health care professional school |
| 8. Collaborate with other professional societies, organizations, and agencies working in the areas of training in human nutrition |
| 9. Disseminate NAA program activities, materials, and expertise through websites, presentations, publications, participation on expert panels, and service as consultants and advisors to other medical and health care professional schools |
NAA, Nutrition Academic Award.
As part of the NAA, unprecedented discussions with the National Board of Medical Examiners, which provides licensure examinations for physicians (the US Medical Licensing Examination), occurred in an attempt to formally assess the newly developed curricula, educational materials, and, where possible, integrate more relevant nutrition questions into board examinations. In 2003, a nutrition subscore was added to step 1 of the US Medical Licensing Examination, which supported the imperative that nutrition be recognized as a scientific discipline within the medical curriculum by both medical educators and students.
In August 2007, the Association of American Medical Colleges published a report as part of the Medical School Objective Project entitled “Contemporary Issues in Medicine: Prevention and Treatment of Overweight and Obesity,” which called on medical schools to educate medical students on obesity prevention and treatment (55).
Traditionally, the 4-y medical school curriculum has been composed of 2 preclinical years, which consist primarily of lectures in the biological sciences, followed by 2 clinical years during which clerkships are the venue for clinical training. Nutrition has been taught both in preclinical and clinical settings. The current movement toward merging classroom and clinical education will facilitate learning basic nutrition science and clinical application. Qualified faculty with nutrition expertise are needed to teach nutrition in the preclinical and clinical settings. Didactic education is frequently provided by nonclinical faculty who have little or no nutrition expertise (clinical or research) and have competing demands such as obtaining grant funding and conducting research. Moreover, there needs to be a concerted effort to raise the interest level in nutrition and advocate for its importance in patient care.
A survey conducted in 2010 reported that the percentage of medical schools offering a dedicated nutrition course had declined from 35% in 2000 to 25% in 2008 (36). In 2008, an average of only 19.6 medical school hours was devoted to nutrition education and skill building, which was less than the IOM-recommended minimum contact time of 25 h (29). Institutions that used online learning modules provided significantly more hours of nutrition instruction (24.1 compared with 13.7 h) across the 4-y curriculum than did those that did not use online learning (56). The available evidence (57, 58) indicates that few residents, fellows, and other clinicians are comfortable with managing nutrition problems of their patients. This could be because existing education is either inadequate or ineffective, both of which provide an argument for greater attention to nutrition.
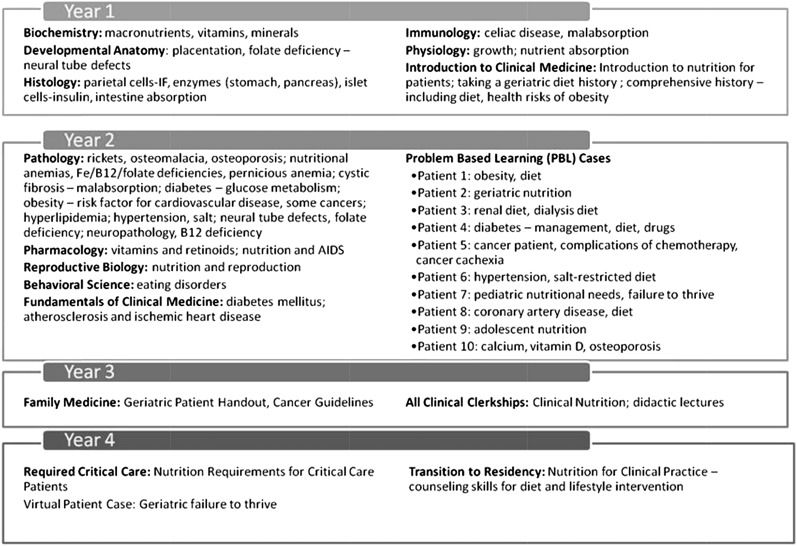
Additional survey data showed that most information about nutrition continues to be taught in the basic science courses and therefore may not be specifically identified with the discipline of nutrition in clinical practice (36). In this survey, only 26 of the 127 accredited US medical schools had a separate course dedicated to nutrition; most nutrition instruction did not occur in nutrition courses. Although most medical schools did not have dedicated didactic courses in nutrition, a small number of medical schools have well-developed longitudinal approaches that span all 4 y (59) (eg, see Figure 1). However, the task of instituting well-integrated longitudinal approaches has been limited by the absence of national standards for a nutrition knowledge base or for competencies, as well as limited recognition of best practices in nutrition.
FIGURE 1.
An example of nutrition integration throughout 4 y of medical school in basic science courses, problem-based nutrition, and clinical clerkships. B12, vitamin B-12; IF, intrinsic factor.
Graduate medical education
Knowledge and skills are synthesized into the practice of medicine during residency and fellowship training. Graduate medical education is accredited by the Accreditation Council for Graduate Medical Education (ACGME). As discussed by Lenders et al (25), ACGME standards require little nutrition training for most specialties. Not surprisingly, the majority of graduate trainees feel unprepared to address nutrition issues in patients (25), which is striking when considering the benefits of nutrition interventions or practices in many acute or chronic conditions. This leads to the identification of the most important nutrition topics in residency and fellowship training, especially those areas where tangible benefits are realized. One salient example is nutrition care in the intensive care unit where early (within 24–48 h) adequate nutrition is known to decrease morbidity and mortality (60). However, there are controversies about nutrition support for critically ill patients because there is some evidence that hypocaloric feedings provide benefits (61, 62). These examples show the complexity of medical nutrition therapy for critically ill patients and reinforce the importance of nutrition training in medical education. This evidence-based training generally falls far short of goals and must be emphasized in the future (63). Furthermore, obesity, which has been shown to be well managed by surgical techniques if severe [BMI (in kg/m2) >40] (64) and with medical treatment when less severe (65), requires specialized knowledge in nutrition.
Specialty training in nutrition
Beginning in 2000, the Intersociety Professional Nutrition Education Consortium was established to oversee the physician nutrition specialist (PNS) training. The primary aims of the Consortium were to establish educational standards for fellowship training of PNSs and to create a mechanism for certifying physicians trained in nutrition. As the pool of PNSs increased, the goal was to enable every US medical school to have at least one PNS on the faculty who could overcome barriers to the incorporation of nutrition into the medical curriculum and residency programs (66). However, there are a few nutrition certification boards in medicine, including the American Board of Physician Nutrition Specialists (ABPNS), which certifies only physicians; the ACN, which is available for MDs and PhDs; and the National Board of Nutrition Support Certification, sponsored by the American Society for Parenteral and Enteral Nutrition, which certifies physicians, pharmacists, registered dietitians (RDs), physician assistants, and nurses. However, none of these certifications is approved by the American Board of Internal Medicine or the American Board of Medical Specialties (67). An interim proposal by the American Association of Clinical Endocrinologists seeks to develop a staged program of nutrition education and training for clinical endocrinologists that will lead to certification (68).
As discussed by Lenders et al (25), in addition to the absence of a recognized specialty board for physicians, several other factors slowed the growth of PNS training, including poor reimbursement for clinical nutrition practice by physicians and the disease-treatment orientation of medicine rather than prevention and inconsistent recognition of nutrition as a specialty unto itself.
Under the auspices of The Obesity Society, a consortium of 14 societies and organizations created a new American Board of Obesity Medicine (www.abom.org), which offered its first examination for certification in November 2012. Although not a recognized board specialty, the American Board of Obesity Medicine has had preliminary discussions with the American Board of Medical Specialties with regard to required steps for a focused practice Maintenance of Certification designation.
UK FOCUS: THE NEED FOR A NUTRITION EDUCATION PROGRAM FOR PHYSICIANS
There are initiatives ongoing around the world to improve and enhance nutrition knowledge and training of health care professionals. These global efforts may show promise in helping the ongoing efforts in the United States to improve nutrition education training of health care professionals. By extension, all of the lessons learned from the ongoing efforts globally can stimulate further improvements in nutrition education of health care professionals worldwide. This section discusses the UK program and acknowledges ongoing activities in Australia (for details of the latter, see the Web-Based Nutrition Competency Implementation Tool at http://wncit.weebly.com/).
In the United Kingdom, the Need for Nutrition Education Program (NNEdPro; http://www.nnedpro.org.uk/) was developed to increase awareness among medical/health care professionals with regard to the importance of clinical and public health nutrition in the prevention of noncommunicable diseases. NNEdPro is an independent educational innovation and evaluation program arising from the work of the Council of Europe Alliance (United Kingdom) on Hospital Food and Nutritional Care. NNEdPro has completed 2 phases of work over 5 y and is beginning a third phase. The objective of phase 1 was to measure the effectiveness of a nutrition education intervention for medical students undertaking clinical training. The objective of phase 2, Nutrition Education and Leadership for Improved Clinical Outcomes, was to assess whether a training intervention incorporating clinical/public health nutrition and change management/leadership strategies could equip junior doctors to improve nutrition awareness in UK hospitals. Phase 3 will focus on nutrition training of medical/health care professionals, research methodology training for nutritionists and dietitians in health care, work in raising awareness of the role of nutrition in noncommunicable disease and cardiovascular disease prevention and management and evaluation of the impact of all NNEdPro work. Collaboration between the University Cambridge School of Clinical Medicine and the NNEdPro group led to the formation of the Nutrition Education Review Group to incorporate nutrition into the medical school curriculum at Cambridge University.
Since 2010, NNEdPro has worked toward vertical integration of nutrition into all clinical years in the curriculum. This began with the introduction of nutrition teaching into the 4th Year, with “carousel-style” multidisciplinary workshops. The teaching incorporates a variety of interactive teaching methods and is evaluated through pre- and post–multiple-choice questionnaires and through collection of qualitative feedback.
The Nutrition Education Review Group currently is working toward integrating teaching into the 6th Year, which will focus on noncommunicable and chronic disease prevention from a nutrition perspective. This teaching will be evaluated in a similar manner to the 4th Year. Nutrition will be integrated into the 5th Year through the creation of podcasts, which will incorporate nutrition into each of the core themes. This will bring in elements of “blended” learning. There continues to be a strong interest among students in integrating nutrition into all 6 y of medical training.
NUTRITION EDUCATION AND COMPETENCIES IN NUTRITION AND DIETETICS PROFESSIONALS’ EDUCATION
Nutrition education for dietitians/nutritionists is discussed in detail by DiMaria-Ghalili et al (24). The Academy of Nutrition and Dietetics (AND; formerly the American Dietetic Association) has established extensive guidelines, curriculum content, competencies, evaluations, and registration examination criteria that are required of all accredited academic and supervised practice programs in nutrition and dietetics (69). After completion of an accredited academic program, students complete an accredited supervised practice component, which qualifies them to take the registration examination. Although there is no standard definition of the term “nutritionist,” all RDs are nutritionists, but the reverse is not always true. Many state licensure boards have legislated specific qualifications for using the term nutritionist, but this is not uniformly regulated (AND; Definition of Terms, http//www.eatright.org/scope).
In 2013, the Academy published competencies defining the scope of practice for the RD including education and credentialing requirements and RD-specific roles, services, and activities (70). Competencies also were established for the Dietetic Technician, Registered, a distinctly different professional who has met criteria for food and nutrition technical services (70). In 2013, the Nutrition and Dietetics Associate certification was created to recognize baccalaureate degree graduates from accredited didactic programs (http://www.eatright.org/ACEND/content.aspx?id=6442480304&terms=baccalaureate%20degree%20credential).
RDs must successfully complete a minimum of a baccalaureate degree granted by a US regionally accredited university or college or foreign equivalent. The relevant curriculum contributes core knowledge, including courses in the basic sciences, clinical and behavioral sciences, community nutrition, research methodology, administrative topics such as food service management and business theories, and principles of public policy (69).
The curriculum also must cover the principles of medical nutrition therapy, a specific term that encompasses skills in assessment of nutritional status of patients and provision of specialized diet modification, counseling, and therapies as appropriate (71, 72). This was further defined as part of the 2001 Medicare legislation as “nutritional diagnostic therapy and counseling services for the purpose of disease management, which are furnished by the RD or nutrition professional” (73).
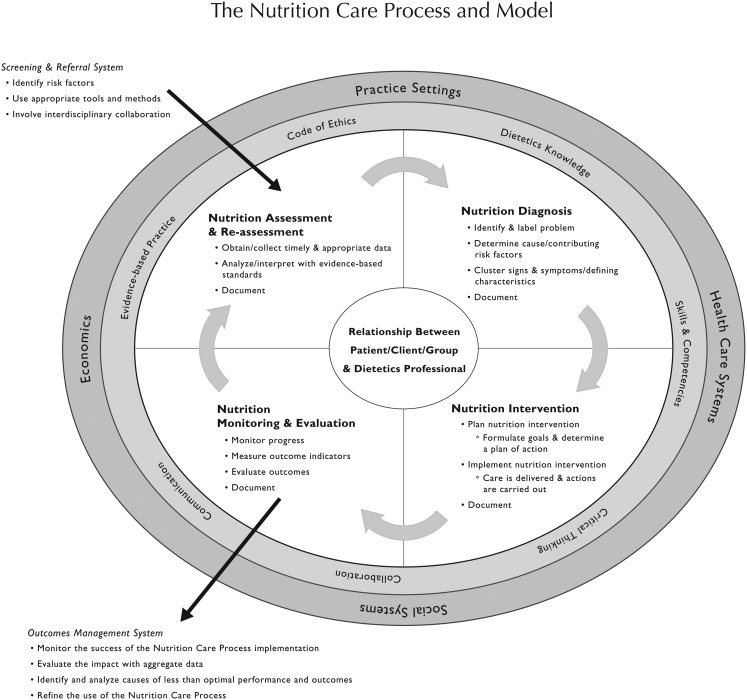
Distinct and yet synergistic with medical nutrition therapy (MNT), in 2003, the American Dietetic Association published the Nutrition Care Process (NCP) (Figure 2), defined as “a systematic problem-solving method that dietetics professionals use to critically think and make decisions to address nutrition related problems and provide safe and effective quality nutrition care” (71). The 4 steps of the NCP are as follows: 1) nutrition assessment, 2) nutrition diagnosis, 3) nutrition intervention, and 4) nutrition monitoring and surveillance.
FIGURE 2.
Academy of Nutrition and Dietetics Nutrition Care Process and model (71).
Dietetics students must develop effective oral and written communication skills and patient counseling techniques and be proficient with interdisciplinary relationships with other health care professionals to meet the nutritional needs of the patient/client. With respect to the latter, dietitians work closely with nurses in identifying mechanical (ie, chewing, swallowing) problems that need to be addressed with a prescribed diet.
The Commission on Dietetic Registration (CDR) is responsible for ensuring professional accountability and continuing competence of RDs. By 2001 the CDR had implemented the Professional Development Portfolio (PDP) Project, which upheld the CDR's mission to “[administer] rigorous valid and reliable credentialing processes to protect the public and meet the needs of nutrition and dietetics practitioners, employers and consumers” (75). The PDP process comprises 5 steps: 1) professional self-reflection, 2) learning needs assessment, 3) learning plan, 4) activity log, and 5) professional development evaluation. The PDP allows RDs to identify their own unique learning needs, to create a plan based on those needs, and to carry out that plan by participating in a wide variety of activity types that cater to many different learning styles. In addition, the steps were designed to meet the Joint Commission (formerly the Joint Commission on Accreditation of Health Care Organizations) Management of Human Resources standards on competence assessment and development.
NUTRITION EDUCATION AND COMPETENCIES IN NURSING EDUCATION
The American Nurses Association describes the profession of nursing as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations” (http://nursingworld.org/EspeciallyForYou/What-is-Nursing). The Essentials of Baccalaureate Education for Professional Nursing Practice by the American Association of Critical-Care Nurses label Essential VII as “Clinical Prevention and Population Health,” which refers to individually focused interventions aimed at preventing the escalation of diseases and conditions, as well as promoting healthy conditions and behaviors to improve populating health. Nutrition is specifically document as sample content for baccalaureate nursing programs (http://www.aacn.nche.noted in the Essentials edu/education-resources/baccessentials08.pdf). In fact, most baccalaureate nursing programs require a separate nutrition course in the prehealth curriculum and incorporate nutritional concepts throughout clinical nursing courses. While caring for patients in hospital, community, and home settings, nurses are taught to perform nutritional assessments and to collaborate with other health care team members to meet the nutritional needs of patients. In their role in health promotion and disease prevention, nurses provide lifestyle counseling to patients, including diet and physical activity (63, 75–80).
The Consensus Model for Advanced Practice Registered Nurse (APRN) regulation (http://www.aacn.nche.edu/education-resources/APRNReport.pdf) states that APRNs must be educated, certified, and licensed to practice in a specific role (nurse anesthetist, nurse midwife, clinical nurse specialist, nurse practitioner) and with different populations (family/individual across life span, adult-gerontology, neonatal, pediatrics, women's health/sex-related, psychiatric-mental health). Entry-level competencies are delineated for graduates of master's, doctorate of nursing practice, and postgraduate programs. All APRN programs include courses on advanced physiology, pharmacology, and health assessment. As examples of APRN preparation in nutrition-related assessment and intervention skills, Table 3 lists selected competencies for the adult-gerontology primary care and acute care nurse practitioners that relate either directly or indirectly to nutrition (http://www.aacn.nche.edu/geriatric-nursing/adultgeroprimcareNPcomp.pdf; http://www.aacn.nche.edu/geriatric-nursing/adult-gero-acnp-competencies.pdf).
TABLE 3.
Competencies relevant to nutrition for select advanced practice nursing roles
| Role and domain | Competencies |
| Adult-gerontology primary care nurse practitioner | |
| Health promotion, health protection, disease prevention, and treatment | • Obtains a relevant health history |
| • Performs and accurately documents a pertinent, comprehensive, and focused physical examination | |
| • Assesses health promotion needs with the use of age, sex, and culturally appropriate standardized assessment instruments or processes in relation to nutrition | |
| • Differentiates between normal and abnormal changes associated with development and aging | |
| • Assesses individuals with complex health issues and comorbidities | |
| • Orders, performs, and supervises laboratory diagnostic testing and clinical procedures, and interprets results in relation to the individual's age, sex, and health status | |
| • Develops, implements, and evaluates age-appropriate health screening and health promotion programs | |
| • Provides anticipatory guidance and counseling to individuals and their families based on identified health promotion needs and health status | |
| • Prescribes and monitors the effect of therapies such as physical therapy, occupational therapy, speech therapy, home health, hospice, and nutrition therapy | |
| • Coordinates comprehensive care in and across settings | |
| Adult-gerontology acute care nurse practitioner | |
| Health promotion, health protection, disease prevention, and treatment | • Obtains relevant comprehensive and problem-focused health histories for complex acutely, critically, and chronically ill patients |
| • Performs and documents a pertinent, comprehensive, and focused physical assessment | |
| • Assesses the impact of an acute, critical, and/or chronic illness or injury and the health promotion needs by using age, sex, and culturally appropriate standardized assessment instruments or processes in relation to nutrition | |
| • Plans diagnostic strategies to screen for and prevent sequelae of acute and critical illnesses and iatrogenic conditions | |
| • Provides for promotion of health and protection from disease by assessing risks associated with care of complex acutely, critically, and chronically ill patients, such as physiologic risk, including immobility, impaired nutrition, fluid and electrolyte imbalance, and adverse effects of diagnostic/therapeutic interventions | |
| • Implements care to prevent and manage geriatric syndromes such as falls, loss of functional abilities, dehydration, delirium, depression, dementia, malnutrition, incontinence, and constipation | |
| • Initiates appropriate referrals and consultations | |
| • Prescribes and monitors the effect of therapies such as physical therapy, occupational therapy, speech therapy, home health, hospice, and nutrition therapy | |
| • Coordinates comprehensive care in and across settings |
NUTRITION EDUCATION IN DENTAL AND DENTAL HYGIENE SCHOOLS
There are 64 dental schools and 323 dental hygiene schools in the United States. Canada has 10 dental schools and 39 dental hygiene schools (81). Nutrition is expected or required in the curriculum of both.
The dental program is a 4-y postbaccalaureate program leading to the Doctor of Dental Medicine (DMD) or Doctor of Dental Surgery (DDS). This nomenclature varies by school, but the curricula are virtually indistinguishable. Dental hygiene programs are usually 2-y, post–high school programs, which are usually combined with an associate degree program, often in community college settings. Because the dentist is the primary care dental provider, they set the standards for the practice but may not be the principal nutrition care provider. That role is usually assigned to the dental hygienist as a component of preventive care (or disease prevention and health promotion). As a result, guidelines or competencies for each provider group vary. The American Dental Education Association sets the standards for dental education and for dental hygiene education (83).
In an earlier iteration of the accreditation competencies for dental education, nutrition education was specifically identified as a requirement. Currently, the relevant competency is broadened to health promotion but does mention nutrition care. Dental hygiene schools are required to teach nutrition. In each case, the purpose of the nutrition competency is to educate providers to deliver appropriate nutrition care for oral health promotion and disease prevention.
For both of these clinical disciplines, the nutrition curriculum should have a strong clinical component, focusing on diet assessment, patient education, and referral. A major concern in both disciplines is often the lack of faculty with a clinical nutrition background. Past studies have indicated a wide range of expertise of faculty teaching nutrition. Very few faculty are RDs or other nutrition professionals (83). In dental schools, nutrition education often is the responsibility of biochemistry or the preventive dentistry faculty. In dental hygiene schools, it is often an interested hygiene faculty member who assumes this responsibility (83). Other barriers are the difficulty of integrating nutrition education into the curriculum (more so in dental than in dental hygiene programs), the lack of resources such as core curricula and models for clinical nutrition implementation, and the lack of faculty who can teach nutrition in the clinical setting (84). In many schools, nutrition still has not evolved beyond biochemistry. For the past 50 y, schools have been challenged with integrating basic and applied nutrition into the curriculum, and specifically into the clinical curriculum.
Several past studies have shown the number of hours devoted to nutrition has remained fairly consistent and is low compared with other topics in the curriculum (85). A 2001 survey of US and Canadian dental schools found that only 41% of schools reported that students provided diet counseling for patients and only 28% of schools had an RD on the faculty to provide clinical nutrition education (86). Another study found that although dentists were motivated to include nutrition in their clinical care, most felt unqualified to provide diet guidance to their patients (87).
NUTRITION EDUCATION FOR HEALTH CARE PROFESSIONS MUST KEEP PACE
There is evidence that adherence to best nutritional practices alone has not been adequate to promote consistent advancement of nutrition education for health care providers. There now are several additional trends that are the impetus for remodeling nutrition education for health care professionals. The trends include policy and legislative mandates, new pedagogic approaches being adopted in the training of health care professionals, and the emergence and mandate of interprofessional education.
The ACA
As discussed by Levy et al (26), the ACA mandates increased knowledge and awareness of disease-prevention strategies across the continuum of medical and health care professions, starting with education in preparation for these career paths. In particular, the ACA Title IV Prevention of Chronic Disease and Improving Public Health should be viewed as a call to action to show that nutrition training for health care professionals can achieve beneficial health outcomes. It also is an opportunity to partner with federal, state, and local agencies that are motivated by ACA mandates.
Trends in medical education
Specific recommendations to reform medical education over the past 2 decades (88, 89) have led to substantial changes in the overall organization and structure of the curriculum at an increasing number of medical schools. Changes include greater emphasis on competency-based curricula, interprofessional and team-based education, and information technology–empowered learning (89). Importantly, there also has been a shift toward earlier integration of clinical applications in the basic sciences. Increased incorporation of nutrition education, especially in the first 2 y, is consistent with the growing demand for more clinically relevant knowledge, especially with respect to the trend of teaching by organ system. The clinical foundations component of the curriculum, now more likely to begin in year 1 rather than being deferred, can readily include nutritionally relevant aspects of the physical examination and dietary assessment (90). This also sets the stage for introducing resources that can be used by medical students throughout the continuum of postgraduate training and residency. For example, relevant nutrition knowledge, skills, and resources can be appropriately included in the blocks of lectures focused on gastroenterology, endocrinology, hematology, and the cardiovascular and renal systems. This approach accommodates a strong emphasis on nutrition without necessitating a separate nutrition course within an already overcrowded teaching environment.
Problem-based learning and small-group experiences are another hallmark of the new medical education environment (91), with self-directed learning and evaluation recognized as important across the continuum of undergraduate, graduate, and continuing medical education (92). Nutrition science and clinical practice issues can be readily integrated into problem-based learning cases and scenarios that are provided, without time being added to the schedule of classes and activities (90). Longitudinal ambulatory care externships or apprenticeships, another hallmark of medical education reform, involve medical students in clinical experiences beginning at year 1. These ambulatory care assignments provide the opportunities to help students recognize how nutrition knowledge and skills contribute to clinical care and to model appropriate interprofessional approaches.
Interprofessional education
Interprofessional education in the training of health care professionals, as discussed by DiMaria-Ghalili et al (24) and Kushner et al (23) in this supplement issue, has become an important approach promoted by the IOM and adopted by the Association of American Medical Colleges, ACGME, American Dental Education Association, AND, and APRN.
Health care is reorganizing around high-functioning teams to address medical problems (93). One study reported that a multidisciplinary team achieved results similar to specially trained physicians for patients in intensive care units (94). This approach provides the rationale for interprofessional nutrition education as a potential solution to a shortage of PNSs or other qualified nutrition professionals.
A recent IOM report underscored the importance of a multidisciplinary team-based approach in achieving a more effective health care delivery system (95). Nutrition education requires a team-based approach involving health care professionals with the requisite nutrition training to develop nutrition competencies needed for practice. The Interprofessional Education Collaborative has provided the rationale and framework for development of interprofessional competencies (96). To further facilitate this approach, common competency domains across health care professions have been developed recently (97).
REMODELING NUTRITION EDUCATION FOR HEALTH CARE PROFESSIONALS
The rationale to advance nutrition education of health care professionals is compelling. However, to move forward, a unified interprofessional approach is needed. Lessons learned from the NAA experience were clear. Coordination and sustainability of the nutrition education model is crucial to perpetuate the medical nutrition education agenda going forward. Championing this cause, the NHLBI convened a workshop in the fall of 2012 (see http://www.nhlbi.nih.gov/meetings/workshops/nutrition.htm), bringing together a multidisciplinary network composed of some of the NAA faculty, as well as leaders in a broad range of nutrition education efforts and policy development (98), to consider how best to move forward the nutrition education agenda for health care professionals.
Among the conclusions reached by workshop members was that definition of a core nutrition knowledge base and competencies is needed. Furthermore, it is evident that best nutrition practices are relevant to all venues where health care is practiced. The ACA provides the momentum to link care of the individual with public health, and nutrition training should strive toward this link. Another conclusion from the workshop is that there are opportunities to educate and promote skills at each stage of training or continuing education. Although the focus here has been in early-stage education, mechanisms are needed to advance nutrition awareness, knowledge, and skills of practicing health care providers, as well as improve their referral patterns to other qualified nutrition providers.
At this time, there is a limited number of certified PNSs, many of whom were trained in specialties/subspecialties. This elite group represents a highly valuable resource in offering guidance and training in their academic medical centers. Together with other qualified nutrition faculty, these individuals can take a leadership role in developing and teaching the nutrition topics of relevance to the curriculum.
The workshop provided a valuable opportunity for interprofessional interaction and initiated the process of developing common interprofessional goals and competencies. Additional interprofessional issues discussed included defining the specific roles in nutrition education for each discipline. An interprofessional team approach with the adoption of best practices appears to be a viable solution for the shortage of PNSs and qualified nutrition educators in clinical care. However, because of their inherent knowledge and training in nutrition, qualified dietitians/nutritionists should assume a key role in educating the health care professional team. Dietitians already exist in many health care environments, but their role in the education of other health care professionals is highly variable and often unrecognized. The interprofessional team needs to examine how to systematically incorporate the RD into their education.
Guiding principles for the future
Future efforts to transform the ways in which we integrate nutrition and physical activity into the education and training of health care professionals need to follow a clearly defined set of guiding principles that are built on a multidisciplinary approach. The principles presented below are applicable to all health care professionals and thus are inherently cross-cutting themes for health care professional training:
1) Health care professionals should implement recommended nutrition practices and promote current dietary guidance issued by federal agencies and professional societies for the prevention and treatment of disease. The practices and principles should be evidence-based, reflect the current state of the science, and be implemented according to best practices.
2) The fundamentals of the NCP, a systematic approach that currently is used mostly by dietitians/nutritionists for providing high-quality nutrition care that includes nutrition assessment, diagnosis, intervention based on root cause, and monitoring/evaluation (71) should be adapted as appropriate to other health care providers. This process should define specific roles, such as who refers and when, interactions between the professions, and how multidisciplinary teams work together for the best health outcomes for their patients. Interprofessional nutrition education is critical to instill a team approach to teaching, training, and learning and to patient care.
3) It is important to recognize and promote the unique role of the RD on the health care team, partnering with physicians in the nutrition assessment, therapeutic recommendations, and joint follow-up of patients as a cornerstone of the NCP. Although strongly endorsing a multidisciplinary approach, the unique and essential role of the dietitian in the care process needs to be underscored. RDs also play a key role in teaching and providing training for other health care professionals.
4) Nutrition education in medical/professional schools needs to be delivered in the context of the most up-to-date approaches for curriculum design and delivery by using a longitudinal, integrated approach rather than focusing on single courses or a discrete discipline. These approaches move the focus away from rote memorization and toward a more meaningful integration of new constructs with existing knowledge (90).
5) Nutrition educational experiences should involve the collaborative effort of multiple stakeholders and the most innovative approaches for effective teaching, such as problem-based learning, case-based learning, behavioral methodologies such as motivational interviewing, simulation, role playing, and other modalities (99). Resources for providing nutrition content in the context of these approaches should be fully available to the teaching teams.
6) It is important to understand the application of evidence-based research in the development of diet and nutrition guidelines for public health and to be able to apply that knowledge toward better patient outcomes. The educational experience should include a thorough explanation of how evidence-based guidelines are derived as well as interactive training on the evaluation of future research findings and their application to clinical practice.
7) There should be an increased emphasis on education research that identifies and validates strategies for providing nutrition education to health care professional students and practicing clinicians. The new nutrition education approaches implemented in the future will require objective assessments for efficacy and effectiveness. There will be a need to study educational approaches throughout the medical/health care professional realm, especially with respect to incorporating nutrition into newly evolving medical/health care professional training curricula.
Health care professionals must be mindful of the population health issues that affect different cohorts. Inherent to this is having an understanding of the social determinants of health to be effective managers of change (100).
Research recommendations
Based on the reality that nutrition education curricula for health care professionals have not been well integrated in education and training programs, there is a need to conduct research to identify the best education and training models and their effect on health care professionals’ practices, the subsequent benefits on patient outcomes, and the impact on public health and associated costs. A considerable investment in research is needed to develop and implement the most effective nutrition education programs across the continuum of medical and health care professional education and training. These are classified as cross-cutting recommendations for all health care professionals as well as those that are specifically relevant to medical schools, residency and fellowship programs, and other health care professionals (Table 4).
TABLE 4.
Cross-cutting research recommendations
| • Identify and evaluate new approaches or strategies for educating health care professionals about nutrition and healthy lifestyle behaviors |
| • Conduct research on how interprofessional nutrition education with multidisciplinary teams contributes to more coordinated care and better performance and patient outcomes |
| • Evaluate newer models of instruction (eg, competency-based curricula, interprofessional team-based education, information technology–empowered learning, patient and population centered) on health care professionals’ skills and competencies |
| • Evaluate the efficacy of the 2 types of training (integrative and traditional approaches) or their combinations on nutrition learning and assess patient outcomes of the traditional and nontraditional (integrative/innovative) models |
| • By using new technologies (electronic medical records, electronic monitoring devices for food intake and physical activity), test whether health care professional training improves compliance with diet and healthy lifestyle modification among patients |
| • Conduct studies that evaluate the nutrition content of board examinations |
| • Evaluate the current curricula of medical schools, residency and fellowship programs, and continuing education programs (eg, for other health care professionals such as nurses, dentists, and pharmacists) to assess their nutrition content |
| • Update and evaluate the effectiveness of the Nutrition Academic Award Curriculum Guide for the Health Professions through coordinated nutrition education, research, and training activities for health care professionals, including those for medical students, residents and fellows, nurses, pharmacists, dentists, physician assistants, and other clinicians and health care professionals to encourage interprofessional training and collaboration |
| • Evaluate the updated competency-based curricula in nutrition for all health care professionals |
| • Identify “best practices” related to nutrition education and patient care in medical schools, residency and fellowship programs, and in other health care professional programs (eg, nursing, dental, dietetics, pharmacy) |
| • Test new approaches for incorporating nutrition in the training of residents, fellows, and other health care professionals (eg, use of new technology and training modules) |
| • Determine how one can build capacity to increase nutrition knowledge and practice by considering continuing professional education by dietitians and nutrition researchers to update nurses, nurse practitioners, and other health care providers |
Ownership of the challenge/solution
The institutes of the NIH are providing strong leadership for a new and enhanced model of biomedical nutrition education that will become an integral part of the training of medical and other health care professionals. With their guidance and support, we are developing innovative new strategies that build on previous initiatives such as the NAA and take this important health care component to the next level of excellence. To ensure that this effort and progress will be sustained, the collaboration of a wide range of stakeholders will be required. Major stakeholders include the following: institutions of higher learning, professional societies, credentialing boards, practicing health care professionals, education specialists, policy makers, health care consumers, public health care professionals, and the health care industry as a whole (both providers and insurers). Efforts to achieve buy-in for this initiative will be enhanced by the establishment of the core competencies, which provide an organized framework for informing stakeholders and bringing them into the discussion (101). Likewise, collaboration between educators and clinicians will enhance both the development of new educational approaches as well as the crucial research studies needed to provide the scientific evidence of their effectiveness (102). It is hoped that groups such as the NHLBI and ASN will work together to create common nutrition competencies and curriculum guidelines that are adopted across different disciplines to improve the education and training of health care professionals for the betterment of population health.
SUMMARY
Improving the delivery of nutrition care to patients in different settings (ie, from the hospital to the clinic and the community) is essential to improve population health in an era where increasing chronic diseases related to aging, obesity, and lifestyle practices contribute dramatically to public health challenges and associated health care costs. There is an urgent need to better prepare health care professionals to address nutrition-related conditions using best practices. This will require that dietitians and nutrition professionals assume a leadership role in medical education training for health care professionals. There also is a pressing need to conduct research that improves health care professional education and health care practice, patient outcomes and education, and population health. We recommend as a next step that relevant stakeholder groups launch an initiative to tackle these relevant health care professional education and training needs. Implicit to this is the need to evolve (and teach) evidence-based standards for nutritional care. In addition, including nutrition in clinical training at all levels is necessary to maintain a focus on its critical role in patient care. Also, a multidisciplinary team educational approach will be required to realize best practices and patient outcomes. This is a major undertaking that will require coordination among involved stakeholders to accomplish a transformation in the education of health care professionals. Success will be dependent on sustained funding and commitment by the health care delivery infrastructure at all levels in the United States and globally. We are mindful that this is a long-term and multistep process that involves many components, which include establishing a coordinating center to manage all aspects of the nutrition education programs for health care professionals and developing education competencies and curricula for health care professionals. It is time that the health care professionals rise to the demands of society to improve patient care and population health.
Acknowledgments
The authors’ responsibilities were as follows—PMK-E and LVH: described dietetics education; SRA, CWB, BB, MSE, MDL, CLR, ES, and DLS: wrote sections on physician education; BB, CML, ES, and DLS: wrote about nutrition education for medical residents; LB: described nursing education; CA Palmer: described dental education; CL and SR: described medical education in the United Kingdom; CML, CA Pratt, and LVH: described the Nutrition Academic Award; and PMK-E, CA Pratt, ES, and LVH: had oversight for all aspects of the manuscript. All of the authors contributed to writing the manuscript. CML receives research and educational support from the New Balance Foundation, the Boston Nutrition Obesity Research Center (P30DK46200), as well as the National Institute of Diabetes and Digestive and Kidney Diseases (5-K23DK082732). BB is a consultant for Nestlé. DLS receives research and educational support from the Vanderbilt Digestive Disease Research Center (P30DK058404). None of the other authors declared a conflict of interest.
Footnotes
Abbreviations used: ACA, Patient Protection and Affordable Care Act; ACGME, Accreditation Council for Graduate Medical Education; AND, Academy of Nutrition and Dietetics; APRN, Advanced Practice Registered Nurse; CDR, Commission on Dietetic Registration; IOM, Institute of Medicine; NAA, Nutrition Academic Award; NCP, Nutrition Care Process; NHLBI, National Heart, Lung, and Blood Institute; NNEdPro, Need for Nutrition Education Program; PDP, Professional Development Portfolio; PNS, physician nutrition specialist; RD, registered dietitian.
REFERENCES
- 1.Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR, Kraus WE, Kris-Etherton PM, Krummel DA, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation 2012;126:1514–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Institute for Cancer Research/World Cancer Research Fund. Food, nutrition, physical activity and the prevention of cancer: a global perspective: a project of World Cancer Research Fund International. Washington, DC: American Institute for Cancer Research, 2007. [Google Scholar]
- 3.USDA. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010. Washington, DC: US Department of Health and Human Services, 2010. [Google Scholar]
- 4.Eckel RH, Jakicic JM, Ard JD, Hubbard VS, de Jesus JM, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Miller NH, et al. AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation (Epub ahead of print 12 November 2013). [Google Scholar]
- 5.Hoyert D, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep 2012;61:1–64. [PubMed] [Google Scholar]
- 6.Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation 2011;123:2870–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomson CA, Ravia J. A systematic review of behavioral interventions to promote intake of fruit and vegetables. J Am Diet Assoc 2011;111:1523–35. [DOI] [PubMed] [Google Scholar]
- 8.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation (Epub ahead of print 12 November 2013). [DOI] [PubMed] [Google Scholar]
- 9.Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, et al. primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. [DOI] [PubMed] [Google Scholar]
- 10.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 11.The Look AHEAD Research Group. Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, Coday M, Crow RS, Curtis JM, Egan CM, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williamson DA, Rejeski J, Lang W, Van Dorsten B, Fabricatore A, Toledo K, The Look AHEAD Research Group Impact of a weight management program on health-related quality of life in overweight adults with type 2 diabetes. Arch Intern Med 2009;169:163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clin Cardiol 2009;32:365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleming P, Godwin M. Low-glycaemic index diets in the management of blood lipids: a systematic review and meta-analysis. Fam Pract 2013;30:485–91. [DOI] [PubMed] [Google Scholar]
- 15.Knowler WC, Barrett-Connor E, Fowler S, Hamman R, Lachin J, Walker E, Nathan D. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hastert TA, Beresford SAA, Patterson RE, Kristal AR, White E. Adherence to WCRF/AICR cancer prevention recommendations and risk of post-menopausal breast cancer. Cancer Epidemiol Biomarkers Prev 2013;22:1498–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vargas AJ, Thompson PA. Diet and nutrient factors in colorectal cancer risk. Nutr Clin Pract 2012;27:613–23. [DOI] [PubMed] [Google Scholar]
- 18.Ledikwe JH, Rolls BJ, Smiciklas-Wright H, Mitchell DC, Ard JD, Champagne C, Karanja N, Lin P-H, Stevens VJ, Appel LJ. Reductions in dietary energy density are associated with weight loss in overweight and obese participants in the PREMIER trial. Am J Clin Nutr 2007;85:1212–21. [DOI] [PubMed] [Google Scholar]
- 19.de Souza RJ, Bray GA, Carey VJ, Hall KD, LeBoff MS, Loria CM, Laranjo NM, Sacks FM, Smith SR. Effects of 4 weight-loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J Clin Nutr 2012;95:614–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosen BS, Maddox P, Ray N. A position paper on how cost and quality reforms are changing healthcare in America: focus on nutrition. JPEN J Parenter Enteral Nutr 2013;37:796–801. [DOI] [PubMed] [Google Scholar]
- 21.Patient and Affordable Care Act, HR 3590, 111th Congress, Sec. 1001, August 25 (2010). Available from: http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf (cited 25 March 2014).
- 22.Tuma PA. An overview of the intentions of health care reform. J Acad Nutr Diet 2012;112(suppl):S56–63. [DOI] [PubMed] [Google Scholar]
- 23.Kushner RF, Van Horn L, Rock CL, Edwards MS, Bales CW, Kohlmeier M, Akabas SR. Nutrition education in medical school: a time of opportunity. Am J Clin Nutr. 2014;99(suppl):1167S–73S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DiMaria-Ghalili RA, Mirtallo JM, Tobin BW, Hark L, Van Horn L, Palmer CA. Challenges and opportunities for nutrition education and training in the health care professions: intraprofessional and interprofessional call to action. Am J Clin Nutr 2014;99(suppl):1184S–93S. [DOI] [PMC free article] [PubMed]
- 25.Lenders CM, Deen DD, Bistrian B, Edwards MS, Seidner DL, McMahon MM, Kohlmeier M, Krebs NF. Residency and specialties training in nutrition: a call for action. Am J Clin Nutr 2014;99(suppl):1174S–83S. [DOI] [PMC free article] [PubMed]
- 26.Levy MD, Loy L, Zatz LY. Policy approach to nutrition and physical activity education in health care professional training. Am J Clin Nutr 2014;99(suppl):1194S–201S. [DOI] [PMC free article] [PubMed]
- 27.Young EA, Weser E, McBride HM, Page CP, Littlefield JH. Development of core competencies in clinical nutrition. Am J Clin Nutr 1983;38:800–10. [DOI] [PubMed] [Google Scholar]
- 28.Weinsier RL, Boker JR, Brooks CM, Kushner RF, Visek WJ, Mark DA, Lopez-S A, Anderson MS, Block K. Priorities for nutrition content in a medical school curriculum: a national consensus of medical educators. Am J Clin Nutr 1989;50:707–12. [DOI] [PubMed] [Google Scholar]
- 29.Committee on Nutrition in Medical Education, Food and Nutrition Board; Council on Life Sciences; National Research Council. Nutrition education in U.S. medical schools. Washington, DC: The National Academies Press, 1985. [Google Scholar]
- 30.Council on Foods and Nutrition; American Medical Association. Nutrition teaching in medical schools. JAMA 1963;183:955–7. [Google Scholar]
- 31.Cyborski CK. Nutrition content in medical curricula. J Nutr Educ 1977;9:17–8. [Google Scholar]
- 32.American Medical Student Association's Nutrition Curriculum Project Essentials of nutrition education in medical schools: a national consensus. Acad Med 1996;71:969–71. [PubMed] [Google Scholar]
- 33.Association of American Medical Colleges. The Liason Committee on Medical Education (LCME) annual medical school questionnaire. Washington, DC: Association of American Medical Colleges, 1982. [Google Scholar]
- 34.National Research Council. Diet and health: implications for reducing disease risk. Washington, DC: National Academy Press, 1989. [PubMed] [Google Scholar]
- 35.US Department of Health and Human Services, Public Health Service. Healthy People 2000: national health promotion and disease prevention objectives. Washington, DC: US Government Printing Office; Department of Health and Human Services, 1991.
- 36.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med 2010;85:1537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weinsier RL. National Dairy Council Award for Excellence in Medical/Dental Nutrition Education Lecture, 1995: medical-nutrition education—factors important for developing a successful program. Am J Clin Nutr 1995;62:837–40. [DOI] [PubMed] [Google Scholar]
- 38.Nutrition in Medicine. Homepage. Available from: http://nutritioninmedicine.org/ (cited 25 March 2014).
- 39.American Society for Nutrition. Clinical nutrition internship program. Available from: http://www.nutrition.org/education-and-professional-development/graduate-and-professional-development/clinical-nutrition-internship-program/ (cited 3 August 2013).
- 40.Hark LA, Iwamoto C, Melnick DE, Young EA, Morgan SL, Kushner R, Hensrud DD. Nutrition coverage on medical licensing examinations in the United States. Am J Clin Nutr 1997;65:568–71. [DOI] [PubMed] [Google Scholar]
- 41.American Society for Nutrition. Physician Nutrition Specialist Award. Available from: http://www.nutrition.org/education-and-professional-development/medical-professional-development/physician-nutrition-specialist-award/ (cited 3 August 2013).
- 42.Bringing physician nutrition specialists into the mainstream: rationale for the Intersociety Professional Nutrition Education Consortium Am J Clin Nutr 1998;68:894–8. [DOI] [PubMed] [Google Scholar]
- 43.Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW. Translation of nutritional sciences into medical education: the Nutrition Academic Award Program. Am J Clin Nutr 2001;74:164–70. [DOI] [PubMed] [Google Scholar]
- 44.US Medical Licensing Examination. Examination content. Available from: http://www.usmle.org/bulletin/exam-content/ (cited 2 August 2013).
- 45.Hark LA. Lessons learned from nutrition curricular enhancements. Am J Clin Nutr 2006;83(suppl):968S–70S. [DOI] [PubMed] [Google Scholar]
- 46.American Society for Parenteral and Enteral Nutrition. ASPEN press release. Available from: http://www.nutritioncare.org/Press_Room/Press_Releases/Physician_Summit_Press_Release/ (cited 14 July 2013).
- 47.US Preventive Services Task Force. USPSTF A and B recommendations. Available from: http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm#more (cited 3 August 2013).
- 48.National Heart, Lung, and Blood Institute. Working Group on Future Directions for Implementing Nutrition across the Continuum of Medical and Health Professions Education and Training, and Research. Executive summary. Available from: http://www.nhlbi.nih.gov/meetings/workshops/nutrition.htm (cited 14 July 2013).
- 49.New York Academy of Sciences. Workshop on nutrition education. Available from: http://www.nyas.org/Publications/EBriefings/Detail.aspx?cid=d00a05a8-b1c3-4f55-93e9-4b7004381a64 (cited 3 August 2013).
- 50.Winick M. Nutrition education in medical schools. Am J Clin Nutr 1993;58:825–7. [DOI] [PubMed] [Google Scholar]
- 51.Feldman EB. Educating physicians in nutrition—a view of the past, the present, and the future. Am J Clin Nutr 1991;54:618–22. [DOI] [PubMed] [Google Scholar]
- 52.Kushner RF, Thorp FK, Edwards J, Weinsier RL, Brooks CM. Implementing nutrition into the medical curriculum: a user's guide. Am J Clin Nutr 1990;52:401–3. [DOI] [PubMed] [Google Scholar]
- 53.Van Horn L. The Nutrition Academic Award: brief history, overview, and legacy. Am J Clin Nutr 2006;83(suppl):936S–40S. [DOI] [PubMed] [Google Scholar]
- 54.Stone EJ. The Preventive Cardiology Academic Award program: a focus on physician education. Am J Prev Med 1990;6(suppl):6–13. [PubMed] [Google Scholar]
- 55.Association of American Medical Colleges. Contemporary issues in medicine: the prevention and treatment of overweight and obesity. Washington, DC: Medical School Objectives Project, 2007. [Google Scholar]
- 56.Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Pract 2010;25:471–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Delegge MH, Alger-Mayer S, Van Way CW, Gramlich L. Specialty residency training in medical nutrition education: history and proposal for improvement. JPEN J Parenter Enteral Nutr 2010;34(suppl):47S–56S. [DOI] [PubMed] [Google Scholar]
- 58.Friedman G, Kushner R, Alger-Mayer S, Bistrian B, Gramlich L, Marik PE. Proposal for medical school nutrition education: topics and recommendations. JPEN J Parenter Enteral Nutr 2010;34(suppl):40S–6S. [DOI] [PubMed] [Google Scholar]
- 59.Edwards MS, Rosenfeld GC. A problem-based learning approach to incorporating nutrition into the medical curriculum. Med Educ Online 2006;11:10. [DOI] [PubMed] [Google Scholar]
- 60.Hoffer LJ, Bistrian BR. Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr 2012;96:591–600. [DOI] [PubMed] [Google Scholar]
- 61.Miller JP, Choban PS. Feeding the critically ill obese patient: the role of hypocaloric nutrition support. Respir Care Clin North Am 2006;12:593–601. [DOI] [PubMed] [Google Scholar]
- 62.Gerlach AT, Murphy C. An update on nutrition support in the critically ill. J Pharm Pract 2011;24:70–7. [DOI] [PubMed] [Google Scholar]
- 63.Marshall AP, Cahill NE, Gramlich L, MacDonald G, Alberda C, Heyland DK. Optimizing nutrition in intensive care units: empowering critical care nurses to be effective agents of change. Am J Crit Care 2012;21:186–94. [DOI] [PubMed] [Google Scholar]
- 64.Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wadden TA, Neiberg RH, Wing RR, Clark JM, Delahanty LM, Hill JO, Krakoff J, Otto A, Ryan DH, Vitolins MZ, et al. Four-year weight losses in the Look AHEAD Study: factors associated with long-term success. Obesity (Silver Spring) 2011;19:1987–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Heimburger DC. Physician-nutrition-specialist track: if we build it, will they come? Intersociety Professional Nutrition Education Consortium. Am J Clin Nutr 2000;71:1048–53. [DOI] [PubMed] [Google Scholar]
- 67.Apovian CM, Shah MS, Ruth MR, August D, Kushner R, McMahon MM, Alger-Mayer S. Board certification and credentialing in nutrition. JPEN J Parenter Enteral Nutr 2010;34(suppl):78S–85S. [DOI] [PubMed] [Google Scholar]
- 68.McMahon MM, Hurley D, Mechanick J, Handelsman Y. American Association of Clinical Endocrinologists’ Position Statement on clinical nutrition and health promotion in endocrinology. Endocr Pract 2012;18:633–41. [DOI] [PubMed] [Google Scholar]
- 69.The Academy Quality Management Committee and Scope of Practice Subcommittee of the Quality Management Committee. Academy of Nutrition and Dietetics. Scope of practice for the registered dietitian. J Acad Nutr Diet 2013;113(suppl):S17–28. [DOI] [PubMed] [Google Scholar]
- 70. The Academy Quality Management Committee and Scope of Practice Subcommittee of the Quality Management Committee. Academy of Nutrition and Dietetics: Scope of practice for the dietetic technician, registered. J Acad Nutr Diet 2013;113:S46ndash55. [DOI] [PubMed]
- 71.Lacey K, Pritchett E. Nutrition care process and model: ADA adopts road map to quality care and outcomes management. J Am Diet Assoc 2003;103:1061–72. [DOI] [PubMed] [Google Scholar]
- 72.Academy of Nutrition and Dietetics (Formerly the American Dietetic Association). International Dietetics & Nutritional Terminology (IDNT) reference manual: standardized language for the nutrition care process. 4th ed. Chicago, IL: Academy of Nutriti; on and Dietetics, 2013. [Google Scholar]
- 73.Centers for Medicare and Medicaid Services. HHS (November 1, 2001). Medicare program; revisions to payment policies and five-year review of and adjustments to the relative value units under the physician free schedule for calendar year 2002. Federal Register 66. Available from: http://www.gpo.gov/fdsys/pkg/FR-2001-11-01/pdf/01-27275.pdf (cited 30 July 2013). [PubMed]
- 74.Commission on Dietetic Registration. Homepage. Available from: http://cdrnet.org/about (cited 25 March 2014).
- 75.Allen JK, Himmelfarb CRD, Szanton SL, Bone L, Hill MN, Levine DM. COACH trial: a randomized controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers: rationale and design. Contemp Clin Trials 2011;32:403–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Driehuis F, Barte JCM, ter Bogt NCW, Beltman FW, Smit AJ, van der Meer K, Bemelmans WJE. Maintenance of lifestyle changes: 3-year results of the Groningen Overweight and Lifestyle Study. Patient Educ Couns 2012;88:249–55. [DOI] [PubMed] [Google Scholar]
- 77.Sargent GM, Forrest LE, Parker RM. Nurse delivered lifestyle interventions in primary health care to treat chronic disease risk factors associated with obesity: a systematic review. Obes Rev 2012;13:1148–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chan BC, Laws R, Williams A, Davies G, Fanaian M, Harris M. Is there scope for community health nurses to address lifestyle risk factors? The community nursing SNAP trial. BMC Nurs 2012;11:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Perry L, Hamilton S, Williams J, Jones S. Nursing interventions for improving nutritional status and outcomes of stroke patients: descriptive reviews of processes and outcomes. Worldviews Evid Based Nurs 2013;10:17–40. [DOI] [PubMed] [Google Scholar]
- 80.Murphy JL, Girot EA. The importance of nutrition, diet and lifestyle advice for cancer survivors—the role of nursing staff and interprofessional workers. J Clin Nurs 2013;22:1539–49. [DOI] [PubMed] [Google Scholar]
- 81.American Dental Association. Homepage. Available from: www.ada.org (cited 13 March 2013).
- 82.American Dental Education Association. ADEA competencies for dental education. Available from: www.adea.org (cited 13 March 2013).
- 83.Touger-Decker R, Benedict Barracato JM, O'Sullivan-Maillet J. Nutrition education in health professions programs: a survey of dental, physician assistant, nurse practitioner, and nurse midwifery programs. J Am Diet Assoc 2001;101:63–9. [DOI] [PubMed] [Google Scholar]
- 84.Touger-Decker R. Nutrition education of medical and dental students: innovation through curriculum integration. Am J Clin Nutr 2004;79:198–203. [DOI] [PubMed] [Google Scholar]
- 85.Touger-Decker R, Gilbride JA. Nutrition education of dental students and professionals. Topics Clin Nutr 1997;12:23–32. [Google Scholar]
- 86.Romito L. The prevalence of dietary counseling activities in North American dental schools. Abstracts of the American Dental Education Association annual session in conjunction with the Association of Canadian Faculties of Dentistry. J Dent Educ. 2003;67(2):206 (abstr 91). [PubMed]
- 87.Palmer CA. Applied nutrition in dental education; issues and challenges. J Dent Educ 1990;54:513–8; discussion 9–20. [PubMed] [Google Scholar]
- 88.Report of the Ad Hoc Committee of Deans. Educating doctors to provide high quality medical care: a vision for medical education in the United States. Washington, DC: Association of American Medical Colleges, 2004. [Google Scholar]
- 89.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923–58. [DOI] [PubMed] [Google Scholar]
- 90.Krebs NF, Primak LE. Comprehensive integration of nutrition into medical training. Am J Clin Nutr 2006;83(suppl):945S–50S. [DOI] [PubMed] [Google Scholar]
- 91.Drees BM, Arnold L, Jonas HS. The University of Missouri-Kansas City School of Medicine: thirty-five years of experience with a nontraditional approach to medical education. Acad Med 2007;82:361–9. [DOI] [PubMed] [Google Scholar]
- 92.Group on Educational Affairs. Implementing the vision: Group on Educational Affairs responds to the IIME dean's committee report. Washington, DC: Association of American Medical Colleges, 2006. [Google Scholar]
- 93.Rhea M, Bettles C. Future changes driving dietetics workforce supply and demand: future scan 2012-2022. J Acad Nutr Diet 2012;112(suppl):S10–24. [DOI] [PubMed] [Google Scholar]
- 94.Kim MM, Barnato A, Angus D, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 2010;170:369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mitchell P, Wynia M, Golden R, McNellis B, Okun S, Webb C, Rohrbach V, Von Kohorn I. Core principles & values of effective team-based health care. Washington, DC: National Academies Press, 2012. [Google Scholar]
- 96.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel. Washington, DC: Interprofessional Education Collaborative, 2011. [Google Scholar]
- 97.Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med 2013; 88:1088–94. [DOI] [PubMed] [Google Scholar]
- 98.Lauer MS. A policy for science. J Am Coll Cardiol 2012;59:2154–6. [DOI] [PubMed] [Google Scholar]
- 99.Krueger PM, Neutens J, Bienstock J, Cox S, Erickson S, Goepfert A, Hammoud M, Hartmann D, Puscheck E, Metheny W. To the point: reviews in medical education teaching techniques. Am J Obstet Gynecol 2004;191:408–11. [DOI] [PubMed] [Google Scholar]
- 100.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Farrow S, Gillgrass D, Pearlstone A, Torr J, Pozniak E. Setting CME standards in Europe: guiding principles for medical education. Curr Med Res Opin 2012;28:1861–71. [DOI] [PubMed] [Google Scholar]
- 102.Lövquist E, Shorten G, Aboulafia A. Virtual reality-based medical training and assessment: the multidisciplinary relationship between clinicians, educators and developers. Med Teach 2012;34:59–64. [DOI] [PubMed] [Google Scholar]