Abstract
Undergraduate medical education has undergone significant changes in development of new curricula, new pedagogies, and new forms of assessment since the Nutrition Academic Award was launched more than a decade ago. With an emphasis on a competency-based curriculum, integrated learning, longitudinal clinical experiences, and implementation of new technology, nutrition educators have an opportunity to introduce nutrition and diet behavior–related learning experiences across the continuum of medical education. Innovative learning opportunities include bridging personal health and nutrition to community, public, and global health concerns; integrating nutrition into lifestyle medicine training; and using nutrition as a model for teaching the continuum of care and promoting interprofessional team-based care. Faculty development and identification of leaders to serve as champions for nutrition education continue to be a challenge.
INTRODUCTION
It has been more than a decade since 21 schools were granted the Nutrition Academic Award from the National Heart, Lung, and Blood Institute with the goal of formally integrating nutrition education into the medical school curriculum. Significant changes in medical education have occurred over this time that provide new and challenging opportunities for nutrition educators and merit renewed efforts to resume and expand on the Nutrition Academic Award's initial achievements. Many medical schools have developed major curricular revisions by breaking down traditional departmental and discipline silos and replacing them with an integrated educational environment. Additional innovations include a competency-based curriculum, longitudinal clinical experiences that are introduced during the first year, team-based instruction and care, community engagement and service learning, as well as new state-of-the-art teaching methodologies, strategies, and technologies. It is in this new pedagogical environment of inquiry, integration, and continuity that nutrition educators are expected to introduce curricular content. This article reviews key aspects of curricular reform and provides examples of novel learning approaches for achieving excellence in medical nutrition education.
A CALL FOR REFORM IN MEDICAL EDUCATION
One hundred years after the Flexner report, which helped to change medical school training in the United States in 1910, the Carnegie Foundation for the Advancement of Teaching released a call for reform once again. In Educating Physicians: A Call for Reform of Medical School and Residency, Cooke et al (1) forecast that fundamental change in medical education will require new curricula, new pedagogies, and new forms of assessment to improve the preparation of physicians for the 21st century. Four key themes emerged, including standardization and individualization, integration of formal learning with clinical experiences, habits of inquiry and improvement, and formation of professional identity. Many of the specific recommendations resonate well with the changes needed to fully realize enhanced nutrition education in the medical school. Recommendations that have the potential to increase opportunities and emphasize the relevance of diet and nutrition across a spectrum of topics in the medical curricula include the following: 1) incorporate interprofessional education and teamwork into the curriculum; 2) engage learners in initiatives focused on population health, quality improvement, and patient safety; 3) provide opportunities for learners to experience the broader professional role of physicians; and 4) place more emphasis on the social, economic, and political aspects of health care delivery (2, 3).
Another relevant publication for nutrition educators is the 2011 Association of American Medical Colleges (AAMC)5 report, Behavioral and Social Science Foundations for Future Physicians (4). The report emphasizes that >50% of premature morbidity and mortality is caused by behavioral and social determinants of health, such as diet, exercise, smoking, and socioeconomic status. Consequently, physicians of tomorrow will need to acquire advanced knowledge, skills, and attitudes in multiple nutrition-related domains such as patient behavior, mind-body interactions in health and disease, health policy and economics, and social and cultural issues in health care, among others. Furthermore, the counseling curricula should be grounded in behavior change frameworks and theory (5). Thus, at a time when many medical schools are initiating curriculum reform, it is advantageous and timely to introduce nutrition and diet behavior–related learning experiences across the continuum of medical education.
LONGITUDINAL INCORPORATION OF NUTRITION INTO THE MEDICAL CURRICULUM
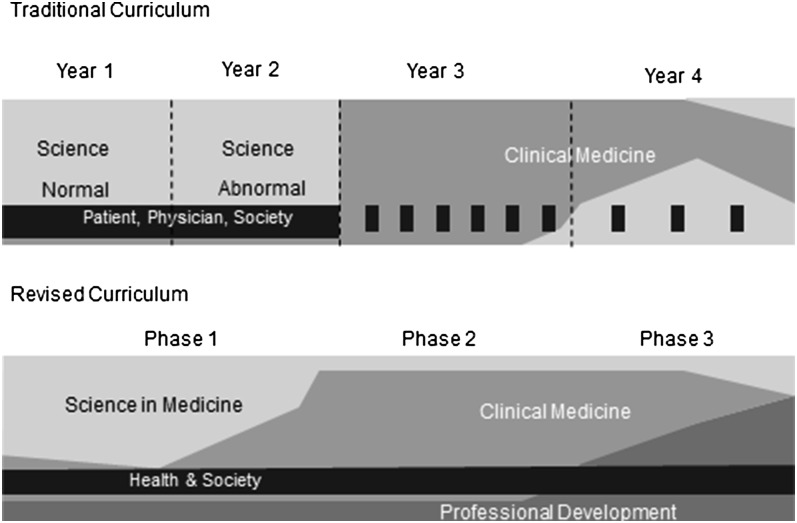
The medical school curriculum has been transformed in organization and structure over the past several years in response to specific recommendations aiming to improve both medical education and patient outcomes (6, 7). The new organization is characterized by centralized curriculum management (with didactic blocks during the first 2 y that are organized by organ system), early introduction of the foundations of clinical practice, and case-based and problem-based learning modules that involve self-directed learning. Within this structure, nutrition education can be vertically integrated across the 4-y medical school curriculum and beyond (8–10). A schematic diagram of one such newly transformed medical school curriculum is shown in Figure 1.
FIGURE 1.
Depiction of traditional and revised medical curriculum at Northwestern University Feinberg School of Medicine. In the traditional design, the first 2 y are primarily devoted to normal and abnormal scientific-related topics. The third and fourth years focus on clinical medicine. The “Patient, Physician & Society” curriculum addresses a variety of topics including communication, ethics, humanities, health economics, and the practice of medicine. In the revised curriculum, the traditional 4 y are replaced with 3 competency-based phases and 4 element groups. Phase 1 includes the first 20 mo of instruction. Fourteen modules of varying lengths are organized by organ systems, with normal and abnormal functions covered in each. The modules contain all 4 elements of the new curriculum, with Science in Medicine predominating. The second phase includes intense clinical experiences through core clerkships that are department-based and span multiple disciplines. The final phase focuses on advanced clinical rotations as well as professional development in a niche focus in medicine, or Area of Scholarly Concentration, that the students research and select in the first year. Learners will immerse themselves in these specific themes in research, education, or community service (see http://www.feinberg.northwestern.edu/education/curriculum/model/phases.html).
Nutrition-based learning objectives and resources can be appropriately included in the blocks of lectures in the first 2 y that are focused on gastroenterology, endocrinology, hematology/oncology, cardiovascular, pulmonary, and renal systems. Nutrition thus becomes a focused area or thread that runs through these blocks instead of an isolated course with a distinctly separate set of knowledge and skills. Although this approach poses a potential risk that students might not recognize nutrition as a distinct discipline, strategic steps can be taken to prevent this from occurring (11). It is beneficial to coordinate and link the nutrition sessions that have been integrated across the blocks through common resources (eg, Web-based material, textbooks, and unified search terms on the electronic blackboard) and monitoring of the learning objectives and content. Evaluation of nutrition knowledge and skills can be accomplished with specific questions included in the block examinations and/or with an annual separate thread examination.
Clinical foundations and skills are now typically introduced in the first year, with a focus on learning clinical examination and assessment skills in either simulated or actual assigned clinical settings. Nutrition-relevant history-taking and examination skills can be readily integrated into this component of the curriculum. Examples are as follows: taking a dietary, physical activity, and weight history; collecting anthropometric measures and calculating BMI; understanding and interpreting relevant laboratory measures; and conducting simple measures of cardiopulmonary fitness.
Nutrition can be readily integrated into problem-based learning modules (12). These modules are typically presented and discussed in small groups that are facilitated by a heterogeneous mix of faculty who do not have training in nutrition. Nutrition faculty need to provide the relevant objectives, content, background reading, and resources for the facilitators and students. In these modules, students work through a patient scenario, with independent assignments and intellectual exploration outside of the classroom, then report their findings back to the group for discussion.
Another hallmark of medical education reform at many medical schools is a longitudinal ambulatory care externship or apprenticeship, which involves medical students in clinical experience from the first year onward. Adoption of the patient-centered medical home as an “education-centered medical home” is another example of integration (13). These ambulatory care assignments enable medical students to interact with dietetics professionals who can reinforce clinical nutrition skills.
Required clerkships in the third year of medical school provide another venue for integrating nutrition education. Clerkships such as primary care, surgery, pediatrics, psychiatry, and obstetrics/gynecology are particularly appropriate for inclusion of nutrition objectives, content, and skills. Providing content and resources to clerkship directors, as well as monitoring seminar topics, can ensure the continuation of nutrition education. Incorporating nutrition education into the fourth-year elective clerkships can be more challenging, and there is less capability of standardizing across the entire student population. However, depending on the clerkship director, further reinforcement of nutrition knowledge and skills is possible during specialty rotations, such as obesity training during endocrinology, malabsorption during gastroenterology, and specialized nutritional support during surgery. In addition, fourth-year electives provide an opportunity for deeper learning for those students interested in diet and nutrition science.
Finally, many medical schools have a community-based, student-run free clinic that provides basic medical services to the underserved and other persons with access and affordability issues. Identifying faculty advisors and volunteers along with providing necessary resources can help to integrate nutrition practice skills into that venue.
IMPORTANCE OF BRIDGING PERSONAL (STUDENT) HEALTH AND NUTRITION TO COMMUNITY, PUBLIC, AND GLOBAL HEALTH AND NUTRITION
Medical school offers future physicians an opportunity to learn not only the constructs of health and disease but also the lifestyle behaviors that contribute to them. Previously, during a more paternalistic era, patients were expected to do as they were instructed by physicians who might or might not practice themselves what was being recommended. For example, before the Surgeon General's report linking tobacco and cancer, many physicians smoked (14). They would advise patients not to smoke, but many ignored their own advice. Eventually, the Joint Commission on Accreditation of Health Care Organizations prohibited smoking inside the hospital, and the medical profession increasingly stopped smoking (15). Likewise, it is not uncommon for physicians to advise weight management through improved diet and physical activity and yet be overweight and unfit themselves. Because data have increasingly supported the importance of these lifestyle behaviors in contributing to weight control and health, the merits of training physicians who advocate and practice these same behaviors themselves grow increasingly more compelling (16). The Institute of Medicine recommended not only that physicians and other health care providers should serve as role models for patients but also that they lead efforts in their community, state, and local environments to support obesity prevention through improved physical activity and nutritional behaviors (17).
Indeed, the value of launching medical school education by focusing on personal health habits and behaviors offers an opportunity for students to learn first-hand both the benefits and the challenges of adopting or reinforcing these behaviors in the real world. Medical nutrition education involves a personal commitment to understanding both the science and the practice related to optimizing nutritional status. Developing those lifestyle behaviors despite the environmental, economic, or time pressures common in medical school gives first-hand experience to how to meet and overcome such common challenges.
Because of the universal absence of nutrition education throughout the undergraduate school system in the United States, many students begin medical school with little more than a consumer-level awareness of basic nutrition principles and little or no knowledge of the role of macro- or micronutrients in achieving good health. Some students may have been influenced by family or friends or popular literature regarding certain eating behaviors, dietary supplement use, weight-loss strategies, and other diet advice, but they rarely understand the importance of applying evidence-based nutrition recommendations in formulating optimal nutrition recommendations for individual patients. It is important for nutrition educators to identify and challenge these personal beliefs, explore their origins, and guide the students toward using evidence-based medicine in replacing popular myths with facts.
It has been well documented that the lack of knowledge and skills undermines confidence in nutrition counseling, thereby adversely affecting a physician's ability and willingness to perform nutrition counseling (16, 18–21). The limited data available to date suggest that improving students’ own lifestyle habits helps to improve their nutrition counseling skills as well (20). By starting with themselves and examining their own lifestyle behaviors within the context of the current dietary guidelines and recommendations, medical students can acquire a useful introduction to this process that can help them be more sensitive and supportive when encountering future patients who likewise need to make these changes. The use of food diaries, and self-monitoring eating behaviors, regular weighing, and monitoring physical activity can familiarize students with the tools and techniques needed to promote ongoing adherence. At Northwestern University Feinberg School of Medicine, students complete a 10-wk Behavior Change Plan in which they self-select a health behavior to either increase (eg, exercise, fruit and vegetable intake, dental flossing) or decrease (eg, soda or fried food intake, fingernail biting), monitor baseline occurrence, set goals, and implement a change (22).
Once there is awareness of the role of diet in their personal health status, the transition to understanding and appreciating the limited access to healthy foods and nutrients in the community becomes more relevant. Students can then better appreciate barriers to consuming a healthy diet that occur at the community level, especially among minority and low socioeconomic subgroups with known health disparities. Likewise, this experience translates into a better appreciation for global nutrition issues and related health conditions that warrant public health attention on an international scale. By starting at the individual level and then broadening to local, regional, and global nutrition screening, diet assessment, and relevant dietary interventions tailored to specific nutrition deficiencies or excesses, medical education can endorse and stimulate interest in improving adherence to the evidence-based dietary recommendations established by national and international health organizations.
INTEGRATION OF NUTRITION INTO LIFESTYLE MEDICINE TRAINING
The emphasis on nutrition as an essential component of a healthy lifestyle (for student self-care and patient counseling) can be created by designing a lifestyle medicine thread. Nutrition does not stand alone. Optimal health and wellness are achieved when patients adopt positive lifestyle behaviors including choosing a healthy diet, being physically active, maintaining a healthy weight, being a nonsmoker, and limiting excessive use of alcohol. These individual lifestyle behaviors are among the multiple determinants of health as defined by Healthy People 2020, the science-based, 10-y national objectives for improving the health of all Americans (23). Unhealthy lifestyle behaviors are also at the root of the global burden of noncommunicable diseases, which are now the leading determinant of disability-adjusted life-years (24) and account for ∼63% of all deaths. Addressing these modifiable risk factors for chronic disease in the context of social and physical influences and health care delivery systems allows learners to view diet and nutrition as integral components of health outcomes. This “contextualization of patient care” in both instruction and assessment provides an opportunity to discuss multiple dimensions of diet and nutrition for assessment and treatment, including socioeconomic factors, access and affordability, cultural diversity, and health literacy, among others (25).
Lifestyle medicine is a new discipline that has recently emerged as a systematized approach for management of chronic disease along with defined competencies (26). In the second edition of his textbook aptly entitled Lifestyle Medicine, Rippe (27) provides the most comprehensive definition as “the integration of lifestyle practices into the modern practice of medicine both to lower the risk factors for chronic disease and/or, if disease already present, serve as an adjunct in its therapy. Lifestyle medicine brings together sound, scientific evidence in diverse health related fields to assist the clinician in the process of not only treating disease, but also promoting good health.” Northwestern University Feinberg School of Medicine has incorporated a Lifestyle Medicine Thread that is sewn throughout the curriculum to highlight the importance of healthy lifestyle behaviors to enhance wellness, prevent disease, and manage chronic illness. During the first 2 y of instruction, each organ system block includes lifestyle topics and themes that are pertinent to the system. For example, during the cardiovascular block, the concept of cardiovascular health metrics and “Life's Simple 7,” which combines 4 health behaviors (smoking, diet, physical activity, and body weight) with 3 health factors (plasma glucose, cholesterol, and blood pressure) to assess cardiovascular risk, is introduced (28). The use of a Lifestyle Medicine Thread allows educators to sequentially and purposely introduce new learning experiences that emphasize foundational lifestyle concepts.
INTEGRATION OF NUTRITION AS A MODEL FOR TEACHING THE CONTINUUM OF CARE
The integration of nutrition and physical activity knowledge, attitudes, and skills training differs along the continuum of care. In acute care settings, the patient is often not part of the decision-making process for implementation of treatment. For instance, in intensive care units, enteral and parenteral nutrition is delivered with the primary objective directed toward the learner's knowledge about the nutritional benefits of enteral and parenteral care. If a nutrition care team exists, the learner also benefits from skills related to teamwork. In this setting, however, the treatment is administered to the patient and patient “adherence” is less salient than in the outpatient–chronic care setting. Another important topic in this setting is end-of-life issues, if the patient and family choose not to have their loved one fed.
In chronic care, both the student and the patient need to move forward on the knowledge, attitude, and skills spectrum. The student in training has to learn a body of information related to how nutrition and physical activity can affect the treatment of a condition, convey that information to the patient, and also understand and help facilitate the patient's behavior change. This involves much more than recognizing the importance of nutrition or physical activity and requires insights and skills that include but are not limited to health literacy, listening, and approaches such as motivational interviewing and harm reduction. Exposure to these skills further underscores the value of taking a nonjudgmental, empathetic approach to care. Whether students who are better trained in nutrition, physical activity, and behavior change become more effective practitioners in general constitutes a potential area for future research.
The final and perhaps most compelling consideration in the continuum of care is prevention. Students require evidence documenting preventive strategies that have the greatest potential to improve the quality and length of life, and to save health care costs. Training in prevention encompasses knowledge of chronic care plus the broader issues related to allocation of community resources, capacity building, and specific environmental factors that will either facilitate healthful behaviors (access to affordable and healthful foods, safe play space, fewer fast-food outlets, more family meals, more home cooked meals, etc).
INTERPROFESSIONAL EDUCATION CAN INTEGRATE NUTRITION AND PROMOTE TEAM-BASED CARE
Training initiatives that prepare physicians on how to integrate nutrition into their practice will benefit from the growing trend toward an interprofessional teamwork approach across the continuum of health professions. This has received increasing endorsement not only as a means to improve the quality of health care delivery but also as a way to decrease medical errors (29). The AAMC has identified interprofessional education as an important strategic issue (30), and the Accreditation Council on Graduate Medical Education has established a competency guide emphasizing interprofessional teamwork to enhance patient safety and care quality that is being used by many undergraduate programs in medicine (31, 32). The need for professional health education redesign is recognized at the global level as well. An independent global commission on Education of Health Professionals for the 21st Century recently cited failure of the professions to work as a team (tribalism of the professions) as an important reason why efforts to improve health-system performance have not been more successful (33). In May 2011, an expert panel of the Interprofessional Education Collaborative (IPEC) released the report, Core Competencies for Interprofessional Practice (29). IPEC sponsors included the AAMC as well as the American Association of College Nursing, the American Association of Colleges of Osteopathic Medicine, the American Association of Colleges of Pharmacy, the American Dental Education Association, and the Association of School of Public Health. The report was “inspired by a vision” of the IPEC group that future educational initiatives promote continuously evolving interprofessional competencies as part of the learning process, so that health professions students “enter the workforce ready to practice effective teamwork and team-based care.” The report built on the Institute of Medicine's 5 core competencies for all health care professionals (34): provide patient-centered care, work in interdisciplinary teams, use evidence-based practice, apply quality improvement, and use informatics. However, whereas a number of US medical schools have begun to adopt interprofessional education courses and student activities, a comprehensive, integrated approach on the national level as advocated by the AAMC, Institute of Medicine, and other organizations remains a work in progress (29).
Our work group also endorses the need for medical education to prepare physicians to practice as part of a multidisciplinary team, and nutrition should be a major player on that team. The aforementioned transformation of medical education to better encompass interdisciplinary care offers a perfect opportunity to achieve this goal. As medical schools seek to weave collaborative experiences into their revised curricula, we encourage the inclusion of a strong nutrition presence. Along with physicians, the interprofessional team should include, but not be limited to, dietitians, nurses, pharmacists, and dentists. As we work to integrate nutrition into physician training, we hope to encourage a team approach to teaching, training, and learning and to patient care. When health care professionals “deliberately work together” (29), the expected result is a health care system that is safer, more patient-centered, and better oriented to the community.
In addition to the involvement of nutrition in interprofessional education efforts, we also emphasize the need for studies that explore and document how interprofessional nutrition education with multidisciplinary teams contributes to more coordinated care and improved patient outcomes. Recent Cochrane reviews have examined the overall impact of interprofessional education on professional practice and health care outcomes, concluding that, whereas positive outcomes were seen, more rigorous studies are needed to reach generalizable conclusions about its various elements (35, 36). Likewise, research studies on the effectiveness and efficacy of nutrition as a part of the interprofessional curriculum redesign will be needed to guide future educational efforts to integrate nutrition into team-based care.
DEVELOPING COMPETENCIES AND METRICS
The key reference resource for both learners and instructors of medical nutrition is the Nutrition Curriculum Guide for Training Physicians, the comprehensive and annotated description of critical nutrition competencies for physicians in general practice as well as for clinical nutrition specialists. This document is available online (37). Proposed core nutrition competencies for medical students are listed in Table 1. Continuous updates to the Nutrition Curriculum Guide are of the utmost importance because this is the only document that currently lays out what a medical student should know about nutrition and how to apply such knowledge in clinical practice. Development of an updated version has been given the highest priority among proposed measures for the improvement of nutrition education for health care professionals (38). Internal audits at medical schools can cross-reference existing nutrition instruction with the items in the Nutrition Curriculum Guide to identify gaps. The fact that most US medical schools provide <25 h of required nutrition education (39) makes it unlikely that they can meet these educational goals.
TABLE 1.
Proposed core nutrition competencies for medical students1
| Proposed core nutrition competency |
| Level 1 (years 1 and 2: preclinical) |
| 1) Micronutrients and macronutrients—Dietary Reference Intakes |
| 2) Energy metabolism—calculating basal energy expenditure, body composition |
| 3) Nutrition assessment—BMI, weight gain/loss, nutrient deficiencies |
| 4) Nutrient requirements throughout the life cycle |
| 5) Taking a diet/physical activity history, prescription for physical activity |
| 6) Stages of change—5 A's of counseling patients |
| Level 2 (years 3 and 4: clinical clerkships and transition to residency) |
| 1) Nutrition in health promotion and disease prevention—US Dietary Guidelines and Healthy People 2020 |
| 2) NIH guidelines for prevention and treatment of obesity, diabetes, hypertension, coronary artery disease, cancer, osteoporosis—ATPIII, DASH, etc |
| 3) Outpatient and inpatient nutrition management—medical nutrition therapy for acute and chronic disease |
| 4) Critical care—enteral and parenteral nutrition |
| 5) Referral to an RD for nutrition consult |
ATPIII, Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults; DASH, Dietary Approaches to Stop Hypertension; RD, registered dietitian; 5 A's, Ask, Advise, Assess, Assist, Arrange.
Intramural assessment of medical student performance typically relies on written examinations. Many schools also use objective structure clinical examinations with actors as standardized patients. The observed performance is very effective to assess the preparedness of individual students and the efficacy of entire courses (40). Objective structure clinical examinations have the added benefit that they provide rare opportunities for the students to get feedback based on monitored clinical performance. The problem is the high cost and limited number of specific nutrition competencies that can be assessed with a particular trained patient. Newer online assessment methods, particularly through interactive exercises, gaming environments, and virtual patient encounters, are becoming increasingly available. Such online tools can ease the mind-numbing burden of boring text-based examinations while maintaining reproducible standardized results.
The Liaison Committee on Medical Education (LCME) sets the accreditation standards for US medical schools and enforces them through annual survey reviews and less-frequent full-site visits. The questionnaire asks about the extent of nutrition instruction as part of required coursework. It is interesting to note that the 2011–2012 survey included the assignment to “Illustrate how the curriculum committee would know where in the curriculum ‘osteoporosis’ and ‘clinical nutrition’ are taught,” which shows some attention to the need for adequate nutrition education. The LCME will introduce a new Curriculum Inventory Portal beginning in 2014 that will capture more fine-grained curriculum information at more frequent intervals. There is a need for better enforcement of a minimum of nutrition instruction. LCME action will be much more likely with a strong consensus on the specific standards for nutrition education, whether based on the current Nutrition Curriculum Guide or on an updated version.
The various components of the US Medical Licensing Examination determine whether medical students are ready for clinical practice. However, the items on these examinations appear to capture only a fraction of the nutrition knowledge and clinical practice skills detailed in the Nutrition Curriculum Guide. The most recent systematic comparison (41) did not actually match the content of the questions to a specified nutrition curriculum standard and also cannot reflect all new developments and continuous efforts that need to be made to monitor the alignment of the examinations with the Nutrition Curriculum Guide. The quantity of nutrition questions does not reliably reflect adequate coverage of key competencies needed in clinical practice. Lack of full representation of key nutrition competencies on the examinations is one of the more important reasons for the neglect of comprehensive nutrition education at medical schools. With the ever-growing scope of medical competencies, instructors and medical students unavoidably focus on the items for which they will be held accountable. US Medical Licensing Examination test developers and administrators, in turn, tend to tailor the examinations to the prevalent teaching practices in medical schools. It will take a determined effort by all involved parties to break through this vicious cycle of low expectations.
Dynamic knowledge acquisition, appropriate application, and skilled performance represent the ultimate goals for medical residents who start to work in clinical practice. The few surveys conducted on nutrition knowledge and nutrition-related practice patterns revealed major gaps. Recent medical school graduates in a comprehensive survey indicated almost unanimously that they consider nutrition counseling of their patients important, but that they do not have the requisite skills (42). Many also lacked much of very basic nutrition knowledge listed in the Nutrition Curriculum Guide. More such efforts need to be made to assess on an ongoing basis the readiness of medical school graduates to use nutrition principles in clinical practice.
NEED FOR CONTENT EXPERTS, CHAMPIONS, AND MENTORS TO LEAD CURRICULUM AND AREAS OF SCHOLARLY CONCENTRATION
The 2010 US Dietary Guidelines (43) and Healthy People 2020 Objectives for the Nation (23) both call for greater attention to nutrition, weight status, and physical activity. These guidelines are important for training health care professionals and especially physicians who treat patients with chronic diseases that are related to poor diet and physical inactivity. Many medical schools lack qualified faculty who are experts in nutrition and physical activity, and therefore, medical students are not being adequately trained to prevent or treat diabetes, obesity, hypertension, and heart disease. Although, ideally, each medical school should have a physician nutrition specialist (PNS) who serves as the champion for nutrition education, this remains unrealistic because of inadequate reimbursement for nutrition services and the ongoing shortage of board-certified PNS faculty. Fortunately, it is often possible to identify and engage nutrition faculty who have advanced degrees, many of whom are also existing registered dietitians (RDs), with advanced training in clinical nutrition and motivational interviewing and who can serve as role models and preceptors for medical students. Working together within the various medical specialties, the MD-RD team approach provides medical students with appropriate training in assessment of patients as well as counseling skills. Medical students should also learn the importance of referring their patients to an RD for in-depth counseling beyond what their time and expertise allows.
Successful achievement of this model in medical schools requires oversight and involvement at both the local and national levels. Locally, the curriculum committee and education deans must recognize the importance of training students in the area of nutrition and preventive medicine. The curriculum committee should have a subcommittee on nutrition that oversees the integration of nutrition and evaluation of students’ nutrition knowledge and clinical skills throughout the 4-y curriculum. Nationally, the ASN could serve as the liaison professional organization to provide MD/PhD mentors for medical school faculty and students. Ideally, the ASN Clinical Nutrition Internship Program should grant more summer internship awards to medical students and more training for underrepresented medical nutrition educators. This would foster development of medical school networks throughout the United States that could work together to train medical students. In addition, more PNS awards through the ASN would inspire primary care residents and young physicians to become nutrition experts. Importantly, other nutrition and relevant societies can promote attention to nutrition by establishing awards for nutrition-related education and research.
CONCLUSIONS
This is an exciting time for nutrition educators. Medical schools have embarked on rigorous curricular reform that includes integration, interdisciplinary team-based learning, and longitudinal active learning environments, creating an exceptional window of opportunity for nutrition to become a mainstream component of medical education. With the involvement and oversight of faculty with training and interest in nutrition, vertical integration of nutrition education can be successfully accomplished across the 4-y medical school curriculum. To respond to the overwhelming prevalence of chronic diseases expected in the decades ahead, 21st-century physicians must develop competency in the implementation of a healthy lifestyle, of which diet is an essential component. Bridging personal (student) health and nutrition is important because this enables medical students to learn the lifestyle behaviors and challenges faced by patients, in addition to the constructs of health and disease. A major challenge facing medical schools is to identify faculty who are knowledgeable and skilled in clinical nutrition and nutritional basic science who can lead curricular implementation. Recommended strategies include using an interprofessional approach to nutrition education and encouraging a team approach to learning and to patient care. Provided key faculty and resources can be identified, the opportunities offered by curricular reform as summarized in this article can foster novel learning approaches for achieving excellence in medical nutrition education and transform the ability of physicians to proficiently deliver nutritional care.
Acknowledgments
The authors’ responsibilities were as follows—RFK, LVH, CLR, MSE, CWB, MK, and SRA: wrote the manuscript; and RFK: had primary responsibility for final content. All authors read and approved the final manuscript. None of the authors declared a conflict of interest.
Footnotes
Abbreviations used: AAMC, Association of American Medical Colleges; IPEC, Interprofessional Education Collaborative; LCME, Liaison Committee on Medical Education; PNS, physician nutrition specialist; RD, registered dietitian.
REFERENCES
- 1.Cooke M, Irby DM, O'Brien BD. Educating physicians: a call for reform of medical school and residency. The Carnegie Foundation for the Advancement of Teaching. Preparation for the professions. San Francisco, CA: Jossey-Bass, 2010.
- 2.Irby DM, Cooke M, O'Brien BC. Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med 2010;85:220–7. [DOI] [PubMed] [Google Scholar]
- 3.Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med 2006;355:1339–44. [DOI] [PubMed] [Google Scholar]
- 4.Report of the Behavioral and Social Science Expert Panel. Behavioral and social science foundations for future physicians. Washington, DC: Association of American Medical Colleges, 2011. Available from: www.aamc.org/socialsciencesfoundation (cited 29 July 2013).
- 5.Hauer KE, Carney PA, Chang A, Satterfield J. Behavior change counseling curricula for medical trainees: a systematic review. Acad Med 2012;87:956–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Report of the Ad Hoc Committee of Deans. Education doctors to provide high quality medical care: a vision for medical education in the United States. Washington, DC: Association of American Medical Colleges, 2004. [Google Scholar]
- 7.Group on Educational Affairs. Implementing the vision. Group on Educational Affairs responds to the IIME dean's committee report. Washington, DC: Association of American Medical Colleges, 2006. [Google Scholar]
- 8.Krebs NF, Primak LE. Comprehensive integration of nutrition into medical training. Am J Clin Nutr 2006;83(suppl):945S–50S. [DOI] [PubMed] [Google Scholar]
- 9.Drees BM, Arnold L, Jonas HS. The University of Missouri-Kansas City School of Medicine: thirty-five years of experience with a nontraditional approach to medical education. Acad Med 2007;82:361–9. [DOI] [PubMed] [Google Scholar]
- 10.Lenders C, Gorman K, Milch H, Decker A, Harvey N, Stanfield L, Lim-Miller A, Salge-Blake J, Judd L, Levine S. A novel nutrition medicine education model: the Boston University experience. Adv Nutr 2013;4:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh CO, Ziniel SI, Delichatsios HK, Ludwig DS. Nutrition attitudes and knowledge in medical students after completion of an integrated nutrition curriculum compared to a dedicated nutrition curriculum: a quasi-experimental study. BMC Med Educ 2011;11:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edwards MS, Rosenfeld GC. A problem-based learning approach to incorporating nutrition into the medical curriculum. Med Educ Online. 2006;11:10. Available from: http://www.med-ed-online.org (cited 29 July 2013). [DOI] [PubMed]
- 13.Henschen BL, Garcia P, Jacobson B, Ryan ER, Woods DM, Wayne DB, Evans DB. The patient centered medical home as curricular model: perceived impact of the “education-centered medical home”. J Gen Intern Med 2013;28(8):1105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frank E, Elon L, Spencer E. Personal and clinical tobacco-related practices and attitudes of US medical Students. Prev Med 2009;49:233–9. [DOI] [PubMed] [Google Scholar]
- 15.Lesser LI, Cohen D, Brook R. Changing eating habits for the medical profession. JAMA 2012;308:983–4. [DOI] [PubMed] [Google Scholar]
- 16.Schlair S, Hanley K, Gillespie C, Disney L, Kalet A, Darby P, Frank E, Spencer E, Harris J, Jay M. Medical students’ behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. J Nutr Educ Behav 2012;44:653–7. [DOI] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Accelerating progress in obesity prevention. Washington, DC: National Academies Press, 2012. [Google Scholar]
- 18.Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med 2004;79:156–61. [DOI] [PubMed] [Google Scholar]
- 19.Laschinger HK, Tresolini C. An exploratory study of nursing and medical students’ health promotion counseling self-efficacy. Nurse Educ Today 1999;19:408–18. [DOI] [PubMed] [Google Scholar]
- 20.Frank E, Elon L, Hertzberg V. A quantitative assessment of a 4-year intervention that improved patient counseling through improving medical student health. MedGenMed. 2007;9:58. Available from: http://www.ncbi.nim.nih.gov/pmc/articles (cited 27 July 2013). [PMC free article] [PubMed]
- 21.Frank E, Hedgecock J, Elon L. Personal health promotion at US medical schools—a quantitative study and qualitative description of deans’ and students’ perceptions. BMC Med Educ 2004;4:29. Available from: http//www.biomedcentral.com (cited 8 March 2014). [DOI] [PMC free article] [PubMed]
- 22.Kushner RF, Kessler S, McGaghie WC. Using behavior change plans to improve medical student self-care. Acad Med 2011;86:901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Healthy People 2020. Available from: http://www.healthypeople.gov/2020/default.aspx (cited 8 March 2014).
- 24.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews GK, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–2260. (Published erratum appears in Lancet 2013;381(9867):628.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwartz A, Weiner SJ, Harris HB, Binns-Calvey A. An educational intervention for contextualizing patient care and medical students’ abilities to probe for contextual issues in simulated patients. JAMA 2010;304:1191–7. [DOI] [PubMed] [Google Scholar]
- 26.Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA 2010;304:202–3. [DOI] [PubMed] [Google Scholar]
- 27.Rippe JM. 2nd ed. New York, NY: CRC Press, 2013:xix–xxii. [Google Scholar]
- 28.American Heart Association. My life check. Live better with Life's Simple 7. Available from: http://mylifecheck.heart.org/Default.aspx?NavID=1&CultureCode=en-us (cited 8 March 2014).
- 29.Blue AV, Mitcham M, Smith T, Raymond J, Greenberg R. Changing the future of health professions: embedding interprofessional education within an academic health center. Acad Med 2010;85:1290–5. [DOI] [PubMed] [Google Scholar]
- 30.Association of American Medical Colleges. Learn, serve, lead: the mission, vision and strategic policies of the AAMC. Washington, DC: Association of American Medical Colleges, September 2007.
- 31.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel. Washington, DC: Interprofessional Education Collaborative, 2011. [Google Scholar]
- 32.Accreditation Council for Graduate Medical Education. Common program requirements. Chicago, IL: Accreditation Council for Graduate Medical Education, 2011. [Google Scholar]
- 33.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923–58. [DOI] [PubMed] [Google Scholar]
- 34.Institute of Medicine. Health professions education: a bridge to quality. Washington, DC: The National Academies Press, 2003. [PubMed] [Google Scholar]
- 35.Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2009;3:CD000072. [DOI] [PubMed] [Google Scholar]
- 36.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev 2013;3:CD002213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Curriculum Committee of the Nutrition Academic Award Program. Nutrition curriculum guide for training physicians. Available from: http://www.nhlbi.nih.gov/funding/training/naa/curr_gde.pdf (cited 27 July 2013).
- 38.Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, Laur C, Lenders CM, Levy MD, Palmer CA, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiven ess. Am J Clin Nutr 2014;99(suppl):1153S–66S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med 2010;85:1537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taren DL, Thomson CA, Koff NA, Gordon PR, Marian MJ, Bassford TL, Fulginiti JV, Ritenbaugh CK. Effect of an integrated nutrition curriculum on medical education, student clinical performance, and student perception of medical-nutrition training. Am J Clin Nutr 2001;73:1107–12. [DOI] [PubMed] [Google Scholar]
- 41.Hark LA, Iwamoto C, Melnick DE, Young EA, Morgan SL, Kushner R, Hensrud DD. Nutrition coverage on medical licensing examinations in the United States. Am J Clin Nutr 1997;65:568–71. [DOI] [PubMed] [Google Scholar]
- 42.Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr 2008;27:287–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.US Department of Agriculture. 2010 US dietary guidelines for Americans. Available from: http://www.cnpp.usda.gov/DietaryGuidelines.htm (cited 27 July 2013).