Abstract
Objective
Heroin addiction is a chronic relapsing disorder that has devastating social, medical, and economic consequences. Naltrexone is an antagonist that blocks opioid effects and could be an effective medication for the treatment of opioid dependence. However, its clinical utility has been limited partly because of poor adherence and acceptability. Given the importance of compliance to naltrexone treatment for opioid dependence, the goal of the current study was to examine predictors involved in successful induction onto naltrexone treatment.
Method
Parametric and nonparametric statistical tests were performed on data from a sample of 64 individuals entering treatment who met DSM-IV criteria for opioid dependence. The relationship between naltrexone induction (i.e., inducted- vs. not-inducted onto naltrexone) and risk-taking propensity, as indexed by riskiness on the Balloon Analogue Risk Task (BART) was examined. Participants were recruited from local detoxification programs, inpatient drug treatment, and other Baltimore programs that provided services to opioid dependent adults (e.g., Baltimore Needle Exchange Program) during the period from August 2007 to September 2008.
Results
Positive association between risk-taking propensity and odds of naltrexone induction. Specifically, each five point increase in the total BART score was associated with a 25% decrease in odds of naltrexone induction (OR=0.76, 95% CI: 0.58–0.99, p = .041). This association remained statistically significant even after adjusting for potential confounds, including injection drug use and cocaine positive urine results (p = .05). After adjusting for the covariates, each five point increase in BART score was associated with 28% decrease in the odds of achieving the maintenance dose (AOR=0.73, 95% CI: 0.54–0.99, p = .046).
Conclusions
Risk taking propensity was predictive of induction onto naltrexone treatment, above and beyond injection drug use and cocaine-positive urine samples.
Keywords: Risk taking propensity, naltrexone, opioid dependence, substance abuse treatment
Heroin addiction is a chronic relapsing disorder that has devastating social, medical, and economic consequences.1 Naltrexone is an opioid that blocks opioid effects and could be an effective medication for the treatment of opioid-dependence. 2 However, its clinical utility has been limited partly because of poor adherence and acceptability. 3 Perhaps the most difficult obstacle to improving the clinical utility and adherence of naltrexone treatment is initiating naltrexone treatment. 4 Several steps and considerations must be taken in order to properly initiate opioid-dependent patients onto naltrexone. Physically dependent patients must first complete opioid detoxification, and remain abstinent before beginning naltrexone. If naltrexone is initiated too soon, there is an increased risk to precipitate the sudden onset of withdrawal symptoms among physically dependent patients. Studies have shown that fewer than 30% of opioid-dependent patients are successfully inducted onto naltrexone treatment.2
Research on naltrexone treatment for opioid-dependent patients aimed at identifying successful predictors of naltrexone outcomes is important and there have been several important investigations that have focused on this issue. For example, lengthening the detoxification period, offering monetary incentives, providing patient education, and psychotherapy have been identified as predictors of positive naltrexone outcomes.5 Additionally, employment at the start of naltrexone treatment and length of naltrexone treatment are considered potent predictors of successful outcomes at 1-month follow-up.6 Although this work is useful for understanding the factors underlying treatment outcomes during and following treatment among successfully detoxified patients, few studies focus on predicting successful induction of naltrexone treatment through the detoxification period.6
With regard to the intersection of impulsivity and treatment outcome, risk taking propensity, may be one potential predictor underlying treatment drop-out or adherence and may be related to successful induction onto naltrexone treatment. Traditionally, risk taking propensity is conceptualized as one’s decision to engage in a particular behavior that balances the probability of unpredictable rewards and punishments.7,8 For example, while drug use produces reinforcing effects, there remain potential but generally unpredictable punishers that may include compulsive drug seeking, withdrawal, adverse health effects, and potential criminal penalties.
One strategy for assessing risk taking propensity is the Balloon Analogue Risk Task (BART). This laboratory-based behavioral task models risk taking in the natural environment in which riskiness to a certain point leads to positive consequences, with further excessive risk taking leading to greater negative consequences that outweigh the positives (i.e., changing reward-punishment schedules). Recent studies have shown the BART is linked to a range of risky behaviors in adolescents, as well as community and clinical samples of drug use patients.7,9,10 However, no studies have examined performance on the BART and its relationship to treatment outcome. A detailed description of the task is provided in the method section.
Given the importance of adherence and compliance to naltrexone treatment for opioid dependence, the goal of the current study was to examine the utility of the BART in predicting successful induction onto naltrexone treatment. Heightened levels of risk taking propensity in this regard is particularly relevant to adherence and compliance given one’s decision not to induce but instead continue to use heroin (e.g., risks involved with continued use, injection use and unsafe sexual practices). This study was conducted in 64 opioid dependent adults who were offered induction onto oral naltrexone. All participants completed the BART at the start of the study, and were not under the influence of any substances during completion of the task. The current study examined differences in risk taking propensity between individual who were (“Inducted”) and were not (“Not Inducted”) successfully inducted onto oral naltrexone. We hypothesized that BART score would relate significantly to naltrexone induction outcome in that individuals with higher scores would be less likely to have been successfully inducted.
METHOD
Setting
The study was conducted with participants enrolled in a randomized clinical trial evaluating the extent to which contingent access to paid training in a therapeutic workplace would promote use of naltrexone (an antagonist that blocks the effects opioids). The study was conducted at the Center for Learning and Health (CLH) and the Behavioral Pharmacology Research Unit (BPRU), treatment-research units located at the Johns Hopkins Bayview Medical Center in Baltimore, Maryland.
Recruitment, screening and participant selection
The Johns Hopkins Institutional Review Board (IRB) approved this study. Participants were enrolled in this study from August 2007 to September 2008. To recruit participants, research staff members distributed fliers and letters to detoxification programs, recruited from inpatient drug treatment and other Baltimore programs that provided services to opioid dependent adults (e.g., Baltimore Needle Exchange Program), and local Baltimore neighborhoods. Specifically, adults addicted to heroin were encouraged to apply and enroll in a study that provided treatment, job-skills training, monetary vouchers, and medication for their drug problem. Interested individuals first completed an anonymous brief screening interview in which they were asked eight questions designed to determine quickly if they might be eligible for the study. Brief screening interviews were conducted over the phone, in person at the detoxification program or Center for Learning and Health. Applicants were invited to participate in a full interview if they were 18 years or older, were opioid dependent, unemployed, were not receiving methadone maintenance treatment, and lived within commuting distance of the therapeutic workplace.
The full screen interview included urine and breath samples collected under observation that were tested for opioids, cocaine and methadone; the Composite International Diagnostic Interview-Second Edition (CIDI-2), a structured interview that provides an assessment of whether participants met DSM criteria for cocaine, opioid, and alcohol dependence; the Addiction Severity Index Lite11, a structured clinical interview designed to assess psychosocial functioning in seven areas commonly affected by drug use; the Risk Assessment Battery (RAB)12, a 29-item self report questionnaire that assesses needle use practices and sexual behaviors associated with HIV transmission (e.g., shared needle or works, been to shooting gallery, been to crack house, traded sex for money or drugs); the Vocational/Educational Assessment (VEA)13, a questionnaire designed to gather employment-related information (e.g., employment attitudes and experience; the welfare-to-work edition of the Treatment Services Review (TSR)14, a structured clinical interview designed to assess information about treatment services that participants had received; information about physical limitations that would limit the participant’s ability to type; a personal contact information form; and the Balloon Analogue Risk Task15, a computerized task designed to assess risk-taking propensity. Because the primary variable of interest in the current study involved the behavioral measures of risk taking propensity as assessed by the BART, the BART is described in detail below.
Participants were eligible for this study if they were between the ages of 18 and 65 years, met DSM IV criteria for opioid dependence, reported using heroin at least 21 of the last 30 days while living in the community, were unemployed, were not receiving methadone treatment, and lived within reasonable commuting distance of the therapeutic workplace (e.g., all Baltimore City zip codes and several surrounding Baltimore County zip codes). Participants were not eligible for the clinical trial if they had active hallucinations, delusions, thought disorder or posed a threat to harm themselves or others, were pregnant or breastfeeding, if serum aminotransferases results were over three times normal, if the need for opioids to treat an identified medical problem was anticipated, or a physical limitation that would prevent using a keyboard appropriately and acquiring typing skills was present. These criteria helped to maintain sample homogeneity, minimize the impact of potential confounding variables, and insure patient safety and ability to provide informed consent.
There were 64 participants in the final model. Almost two thirds of the sample was male. Most had a history of injection drug use and cocaine use. The average age was around 44 years of age and the average education was less than high school. The majority of participants were African American (89% African American, remaining participants were White American).
Measure of risk propensity
Risk taking propensity was assessed using the Balloon Analogue Risk Task (BART).15 The BART is a computerized task on which participants have the opportunity to win or lose potential earnings, where persistent responding increases gains but also increases the risk of loss in each trial. In the task, a computer screen displayed four items: a small balloon accompanied by a balloon pump, a reset button labeled “Collect $$$,” a “Total Earned” display, and a second display labeled “Last Balloon” that listed the money earned on the last balloon. With each pump, money (5 cents per pump) was accumulated in a temporary bank. When a balloon exploded, all money in the temporary bank was lost, and the next uninflated balloon appeared on the screen. The participant could stop pumping the balloon at any time and click the “Collect $$$” button. If the participant clicked the “Collect $$$” button, the amount of money accumulated in the temporary bank was added to the amount in the “Total Earned” display. A new balloon appeared after each balloon explosion or money collection until a total of 20 balloons (trials) were completed. Each balloon had the probability to pop between 1 and 128 pumps, with an average breakpoint of 64 pumps. Specific information regard the balloon breakpoint determination was not provided to participants, who are simply informed that the balloon can break anywhere from the first pump all the way through enough pumps to make the balloon fill the screen. After the participant completed the task, the participants received the amount of money they accumulated in the “Total Earned” display in vouchers that were exchangeable for goods and services (see description of the voucher program below).
Detoxification and naltrexone induction
Opioid detoxifications and naltrexone inductions were conducted in community treatment programs, at our residential research unit in the BPRU, and/or through some combination of community programs and the BPRU. Participants who were recruited from 28-day community inpatient programs and who did not use opioids before beginning our study began naltrexone treatment immediately after discharge. Participants who enrolled without completing a lengthy detoxification in a community treatment (e.g., those recruited from the community or those who completed a brief detoxification in the community) were given opioid detoxification services at the BPRU treatment program on an inpatient and/or outpatient basis. Finally, participants were invited to attend the Therapeutic Workplace (procedures described below) or participate in Therapeutic Workplace procedures via remote computer terminal following the opioid detoxification period. The Therapeutic Workplace participation was used in these cases to motivate patients to stay in treatment and remain abstinent from opioids, both of which were necessary before naltrexone treatment initiation.
Naltrexone induction began after participants underwent opioid detoxification. The naltrexone dose increased until the patient tolerated 50 mg, at which point the dosing schedule changed to 100 mg on Mondays and Wednesdays, and 150 mg on Fridays (with some exceptions for holidays, missed days). The maintenance routine was continued until three consecutive doses were ingested, after which the induction period ended and oral naltrexone treatment was discountined. Participants received oral naltrexone for an average of 1.3 weeks (range 1–2 weeks) at the workplace. Staff members who conducted BART sessions were not the same individuals facilitating naltrexone induction. The medical and nursing staff who supervised naltrexone induction were blind to BART results. Study participants were not under the influence of any substances during the performance of the BART and were completely detoxified.
Therapeutic Workplace
Based on the tenets of operant conditioning, the Therapeutic Workplace is a novel employment-based intervention that uses wages for work to reinforce clinically important behavior change. Drug abuse patients are hired and paid in a model workplace to promote clinically important behaviors, whereby wages are arranged contingent both on work and on the emission of those behaviors. In the current study, the Therapuetic Workplace was used to promote naltrexone pharmacotherapy for the maintenance treatment of primary opioid abusers. Once inducted on naltrexone, participants were required to take scheduled doses of naltrexone to gain and maintain access to the workplace. After naltrexone ingestion, the participant was allowed to work and earn wages that day and on subsequent weekdays until the next scheduled naltrexone dose. While in the workplace, participants could work 4 hours every weekday on computerized typing and keypad training programs and earn $8/hour in base pay and about $2/hour for performance on the training programs. If an individual missed a naltrexone dose during this phase, the participant was not allowed to work that day and his/her base pay reset to $1/hour. Participants’ base pay increased $1/hour for every consecutive day that the participant worked. All pay was provided in vouchers exchangeable for goods and services. See Silverman et al.16 for a detailed description of the Therapeutic Workplace setting and procedures.
While attending the Therapeutic Workplace participants had thrice weekly urine drug testing and breathalyzer testing. Other standard treatment services were offered to all study participants throughout the study including drug abuse counseling, case management referrals, smoking cessation, and HIV risk reduction counseling.
Data analysis plan
The analyses were designed to determine if risk propensity as measured on the BART predicted whether or not participants were successfully inducted onto oral naltrexone. The adjusted average number of pumps on the BART task was used to measure risk propensity. This measure has been used in all BART studies as the primary index of risk taking propensity, and has been associated with impulsivity and risk behavior including regular smoking, alcohol use, polysubstance use, unsafe sex, infrequent seat belt use, stealing, and gambling (Lejuez et al. 2002). Participants were categorized as successfully inducted onto naltrexone if they received three consecutive maintenance doses of naltrexone (i.e., 100 mg on Mondays and Wednesday and 150 mg on Fridays). The analysis sought to determine whether performance on the BART predicted naltrexone induction after adjusting for sex and other potential confounds.
In the first stage of the data analysis plan, exploratory analyses were conducted using Pearson correlation coefficients to assess the nature of potential relationships between behavioral and self-reported risk behaviors, urinalysis samples, and induction onto naltrexone treatment. Next, to examine the extent to which scores across behavioral and self-reported measures of risk taking propensity contributed to naltrexone induction (including relevant covariates), both unadjusted and adjusted logistic regression analyses were conducted. The regressions were adjusted for sex, cocaine positive urinalysis samples, and injection drug use. Inclusion of both adjusted and unadjusted was to display potential confounds. All p values were 2-tailed and the statistical significance threshold was set at p < 0.05.
RESULTS
Preliminary Analyses
Of the original 67 participants included in the study, three participants were missing urine results. Because the number of participants with missing values was below 5% of the sample, we chose to proceed with the analysis dropping these three cases. Therefore, we conducted analyses on 64 participants. Table 1 shows demographic information stratified by naltrexone maintenance dose.
Table 1.
Demographic information including stratified by naltrexone maintenance dose.
| No Maintenance Dose (N = 20) |
Maintenance Dose (N = 44) |
|
|---|---|---|
| Sex (Male) | 7 (35.0%) | 16 (36.4%) |
| Cocaine-Positive Urine | 13 (65.0%) | 22 (50.0%) |
| Injection Drug Use | 17 (85.0%) | 26 (59.1%) |
| Age (Mean and SD) | 42.90 (8.01) | 45.36 (8.06) |
| Education (Mean and SD) | 11.25 (1.80) | 11.87 (1.95) |
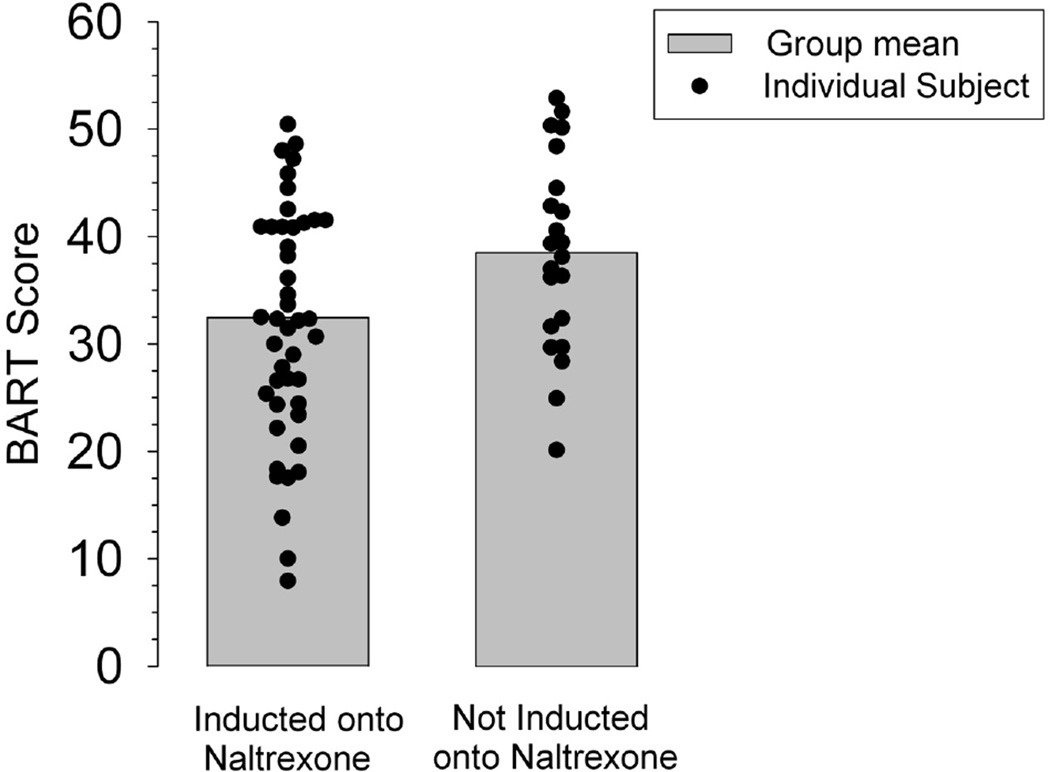
Pearson correlation coefficients were conducted to assess the nature of potential relationships between behavioral and self-reported risk behaviors, urinalysis results, and induction onto naltrexone treatment (see Table 2). History of cocaine injection and history of heroin injection were strongly associated with each other (r = .513, p < .001). Total BART score was associated with induction onto naltrexone and positive cocaine urine samples. Figure 1 shows the individual and mean BART scores for individuals successfully inducted onto naltrexone and for those who failed.
Table 2.
Intercorrelations among primary variables of interest to assess the relationship between behavioral and self-reported risk behaviors, drug use, and naltrexone induction.
| 1 | 2 | 3 | 4 | 5 a | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Naltrexone Induction | --- | ||||||
| 2. Cocaine-positive Urine | −.140 | --- | |||||
| 3. Cocaine Injection | −.293 | .262* | --- | ||||
| 4. Heroin Injection | −.194 | .172 | .513** | --- | |||
| 5. Injection Drug Use | −.256* | .166 | .506** | .873** | --- | ||
| 6. Sex (Male) | .012 | .038 | .006 | −.066 | .031 | --- | |
| 7. BART Score | −.265* | .255* | −.054 | .054 | .078 | .198 | --- |
Note:
p < .05;
p < .001;
represents participants who endorsed any history of heroin, cocaine, or heroin and cocaine injection use.
Figure 1.
BART scores between individuals successfully inducted onto naltrexone and for those who were not inducted onto the maintenance dose of naltrexone. Black dots represent individual BART scores, and the shaded bars represent group means of those inducted and not inducted onto naltrexone. These data are based on assessments collected at study intake.
No other associations were observed between potential covariates.
BART Predicting Naltrexone Induction
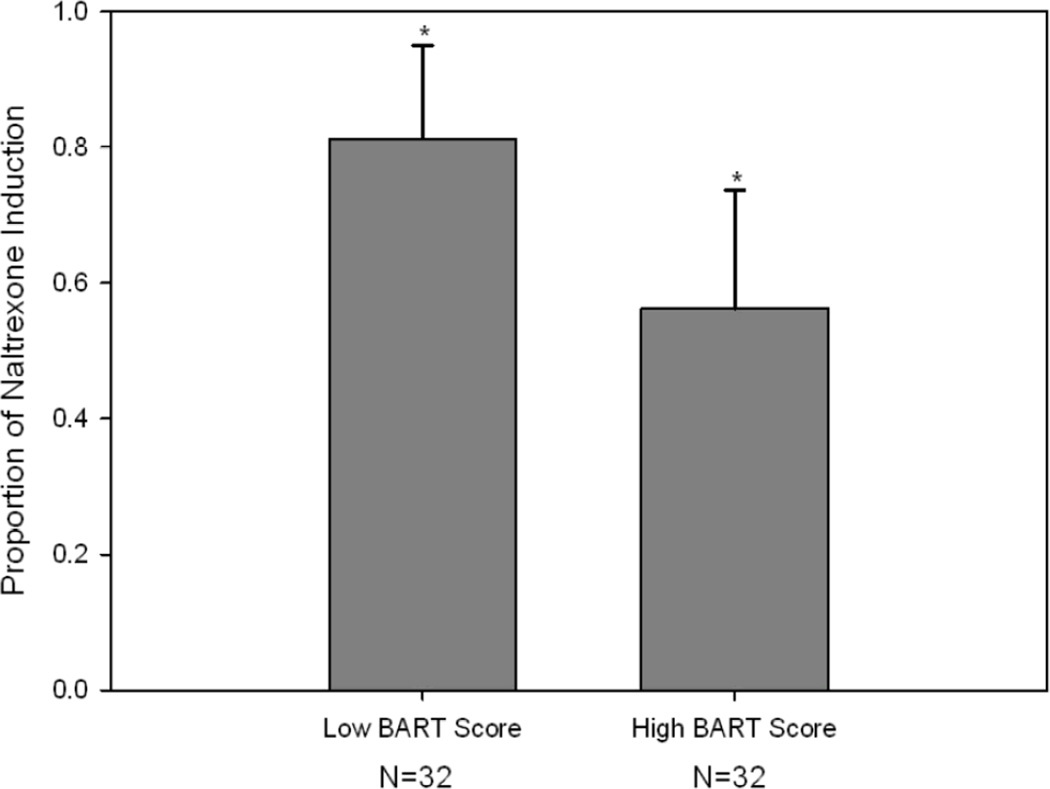
To test the hypothesis that BART scores (indicative of greater risk-taking propensity) would be associated with failure to achieve naltrexone induction, both adjusted and unadjusted logistic regression analysis were conducted, controlling for injection drug use and positive cocaine sample. Based on the exploratory analysis using Lowess plotting of the BART score and induction onto naltrexone, we elected to fit a model with the BART score as a continuous variable in the subsequent logistic regression model. Table 3 shows the unadjusted odds ratios (OR) and the adjusted odds ratios (AOR) for each covariate from the logistic regression analysis. BART scores were divided by five to provide a more meaningful interpretation of the odds ratios. Consistent with our hypothesis, the results evidenced an inverse association between risk-taking propensity and odds of naltrexone induction. Specifically, each five point increase in the total BART score was associated with a 25% decrease in odds of naltrexone induction (OR=0.76, 95% CI: 0.58–0.99, p = .041). This association remained significant even after adjusting for potential confounds, including injection drug use and cocaine positive urine results (p =.05). After adjusting for the covariates, each five point increase in BART score was associated with 28% decrease in the odds of achieving the maintenance dose (AOR=0.73, 95% CI: 0.54–0.99, p = .046). No other variables were significantly associated with naltrexone induction. A Hosmer-Lemeshow test indicated the model adequately fit the data (χ2=3.50, df=8, p=0.899). Figure 2 shows the proportion of individuals inducted onto naltrexone based on BART performance.
Table 3.
Unadjusted and adjusted logistic regression analyses examining the association between BART score and induction onto naltrexone.
| N (% Inducted onto Naltrexone) |
Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|
| Sex (Male) | 45 (68.29) | 0.89 (0.30–2.66) | 1.23 (0.37–4.12) |
| Cocaine-Positive Urine | 35 (62.86) | 0.52 (0.17–1.53) | 0.80 (0.24–2.66) |
| Injection Drug Use | 44 (61.36) | 0.26 (0.07–1.04) | 0.24 (0.05–1.04) |
| BART Score a | --- | 0.94 (0.89–1.00)* | 0.94 (0.88–1.00)* |
Note:
Increments of 5 pumps;
p = .05.
Figure 2.
The proportion of individuals who were inducted onto naltrexone by BART performance. The BART score was split at the median value of 35 pumps. Those below 35 represent the "Low BART Score" group and those above 35 represent the "High BART Score" group. The error bars represent the upper limit of the 95% confidence interval of the proportions. These data are based on assessments collected at study intake.
DISCUSSION
The relationship between risk taking propensity and induction onto naltrexone treatment for opioid dependence was examined. In line with our hypotheses, risk-taking propensity, as indexed by participants’ BART responses indicated a significant relationship to naltrexone induction groups (i.e., inducted- vs. not-inducted onto naltrexone). Specifically, there was evidence that the task predicted naltrexone induction above and beyond other theoretically-relevant risk behaviors (injection drug use and biochemically-confirmed cocaine urine samples).
Participants’ propensity to engage in risk-taking was assessed through scores on the BART. The findings suggest that the most risk-prone participants were less likely to complete naltrexone induction. Risk taking propensity might have predicted naltrexone induction given its role on one’s ability to become drug-free. Essentially, participants who were unsuccessfully inducted onto naltrexone may have been more influenced by their heightened level of riskiness and poor decision-making to terminate treatment. Because the success of naltrexone treatment depends largely on the patient’s adherence and compliance to a set regimen, it is plausible that the strong relationship between risk-taking propensity on the BART may have worked in concert to increase one’s vulnerability to terminate treatment prematurely. Considering the context of the larger literature on impulsivity and drug abuse treatment, novel measures with the ability to predict patients’ likelihood to succeed during the induction phase of treatment has the potential to improve retention, compliance, and long term treatment outcomes. In particular, patients with increased levels of risk taking may be prime candidates for longer periods of detoxification and other supportive measures; whereas, standard protocols of naltrexone induction may well be adequate for patients with lower levels of risk taking. With a better understanding of risk taking and impulsiveness tendencies among opioid-dependent patients, such findings may provide information on increasing the acceptability of naltrexone treatment.
These findings must be considered in light of the study’s limitations. One limitation of the current study is regarding the timing of when the BART was administered. For example, is it important to have participants detoxified before or after completing the BART? If participants are detoxified before completing the BART, they may have established an ability to tolerate the physical effects of withdrawal. Therefore, it is plausible that participants with heighten risk-taking propensity who did not persist through the process of detoxification before entering the study were missed. Additionally, would individuals with heightened levels of risk taking propensity after successful detoxification be less inclined to have become drug-free (i.e., inducted onto naltrexone).
Another important point to consider is the fact that higher BART scores were associated with more voucher earnings for the patients, and thus, may be considered as more adaptive responding on a laboratory measure predicting treatment induction? One interpretation issue that occurs with virtually all BART studies is that participants always have an average number of pumps that is lower than 64 (the point where earnings are maximized). 17 Therefore, in all studies where BART pumps are related to risk behavior, it is also the case that higher earnings are related to risk behavior as well. As this was the case here as well, this could be used to conceptualize the current results as showing that more adaptive responding is related to less treatment induction. Although this interpretation certainly should be considered, this does not obviate the fact that the risk averse strategy on the BART via fewer pumps was related to treatment induction. Future BART work must consider what the implications of this complex relationship are but the complication of earnings does not change the relationship between level of risk taking and induction.
Another limitation involves the fact that the current study included a homogeneous sample of inner-city, substance abusers from the Baltimore area. Accordingly, there needs to be some caution before making generalizations to other samples. While not necessarily generalizable to all samples of inner-city substance abusers, the current study provides valuable data on a group of substance abusers whose personality characteristics (risk proneness) might allow for the development of targeted treatment opportunities. Future studies should expand these methods to more diverse samples to examine the scope and generalizability of these findings to other substance abusing groups. In addition to identifying the processes by which risk taking propensity relates to successful naltrexone induction, it is important to examine what role, if any, risk taking plays in relapse following naltrexone treatment, or treatment adherence following successful naltrexone induction.
This study is the first to show the relationship between risk taking propensity and naltrexone induction, in that, individuals with higher risk-taking propensity may be difficult to successfully induct onto naltrexone treatment. This is of great public health importance, given the clear relationship between initiating, remaining in treatment and long-term abstinence. Clinically, these results suggest the potential value of targeting individuals with high levels of risk proneness to receive modified and/or specialized treatment modules emphasizing effective decision-making skills, risk modulation, behavioral control and treatment adherence, which may be especially important during the early stages of treatment.
CLINICAL POINTS.
Behavioral measures to assess risk-taking propensity have considerable promise for opiate-dependent patients who may be candidates for modified and/or individualized treatment with a focus on decision-making strategies, risk modulation, behavioral control and treatment adherence.
To improve the clinical utility and adherence of naltrexone treatment, assessing risk-taking propensity and impulsiveness is especially important during the early stages of treatment.
Acknowledgments
The authors thank Paul Nuzzo, MA (University of Kentucky), for helpful comments on earlier versions of this manuscript, Haley Brown, BA (Johns Hopkins University School of Medicine), Megan Duffy, BA (Johns Hopkins University School of Medicine), Jacqueline Hampton (Johns Hopkins University School of Medicine), and Amanda Rodriquez, BA (University of Maryland Baltimore County), for assistance with data collection. None of whom have conflicts of interest.
Funding/support: This research was supported by funding by grants from the National Institute on Drug Abuse to Dr. Silverman (R01DA019386; R01DA019497) and Dr. Bigelow (T32DA07209).
Footnotes
Financial disclosure: None of the authors have personal affiliations or financial relationships with any commercial interest to disclose relative to this article.
Previous presentation: Portions of this manuscript were presented at the 71st Annual Meeting at The College on Problems of Drug Dependence.
REFERENCES
- 1.Rawson RA, McCann MJ, Shoptaw SJ, et al. Naltrexone for opioid dependence: Evaluation of a manualized psychosocial protocol to enhance treatment response. Drug Alcohol Rev. 2001;20:67–78. [Google Scholar]
- 2.Tucker TK, Ritter A, Maher, et al. A randomized control trial of group counseling in a naltrexone treatment program. J Subst Abuse Treat. 2004;27(4):277–288. doi: 10.1016/j.jsat.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Nunes EV, Rothenberg JL, Sullivan MA, et al. Behavioral therapy to augment oral naltrexone for opioid dependence: A ceiling on effectiveness. Am J Drug Alcohol Abuse. 2006;32(4):503–517. doi: 10.1080/00952990600918973. [DOI] [PubMed] [Google Scholar]
- 4.Preston KL, Silverman K, Umbricht A, et al. Improvement in naltrexone treatment compliance with contingency management. Drug Alcohol Depend. 1999;54(2):127–135. doi: 10.1016/s0376-8716(98)00152-5. [DOI] [PubMed] [Google Scholar]
- 5.Greenstein RA, Evans BD, McLellan AT, et al. Predictors of favorable outcome following naltrexone treatment. Drug and Alcohol Dependence. 1983;12(2):173–180. doi: 10.1016/0376-8716(83)90042-x. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan MA, Garawi F, Bisaga A, et al. Management of relapse in naltrexone maintenance for heroin dependence. Drug and Alcohol Dependence. 2007;91(2–3):289–292. doi: 10.1016/j.drugalcdep.2007.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aklin WM, Lejuez CW, Zvolensky MJ, et al. Evaluation of a behavioral measure of risk-taking propensity with inner-city adolescents. Behav Res Ther. 2005;43(2):215–228. doi: 10.1016/j.brat.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Leigh BC. Peril, chance, and adventure: Concepts of risk, alcohol use and risky behavior in young adults. Addiction. 1999;94(3):371–383. doi: 10.1046/j.1360-0443.1999.9433717.x. [DOI] [PubMed] [Google Scholar]
- 9.Lejuez CW, Simmons BL, Aklin WM, et al. Behavioral and self-report personality predictors of HIV-risk behaviors in a sample of treatment seeking drug users. Addictive Behaviors. 2004;29:1643–1647. doi: 10.1016/j.addbeh.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 10.Lejuez CW, Bornovalova M, Daughters S, et al. Differences in impulsivity and sexual risk-taking behavior among inner-city crack/cocaine and heroin users. Drug Alcohol Depend. 2005;77:169–175. doi: 10.1016/j.drugalcdep.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 11.McLellan AT, Cacciola JS, Zanis D. The Addiction Severity Index-“Lite” (ASI-“Lite”), Center for the Studies of Addiction, University of Pennsylvania/Philadelphia VA Medical Center. 1997 [Google Scholar]
- 12.Navaline HA, Snider EC, Petro CJ, et al. Preparations for AIDS vaccine trials: An automated version of the risk assessment battery (RAB): Enhancing the assessment of risk behaviors. AIDS Res Hum Retroviruses. 1994;10:281–283. [PubMed] [Google Scholar]
- 13.Zanis DA, Coviello D, Alterman AI, et al. A community-based trial of vocational problem-solving to increase employment among methadone patients. J Subst Abuse Treat. 2001;21(1):19–26. doi: 10.1016/s0740-5472(01)00177-5. [DOI] [PubMed] [Google Scholar]
- 14.McLellan AT, Alterman AI, Cacciola J, et al. A new measure of substance abuse treatment: Initial studies of the treatment services review. J Nerv and Ment Dis. 1992;180(2):101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Lejuez CW, Read JP, Kahler CW, et al. Evaluation of a behavioral measure of risk-taking: The Balloon Analogue Risk Task (BART) J Exp Psychol Appl. 2002;8(2):75–84. doi: 10.1037//1076-898x.8.2.75. [DOI] [PubMed] [Google Scholar]
- 16.Silverman K, Wong CJ, Needham M, et al. A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. J Appl Behav Anal. 2007;40(3):387–410. doi: 10.1901/jaba.2007.40-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aklin WM, Tull MT, Kahler CW, Lejuez CW. Risk-taking propensity changes throughout the course of residential treatment. Personality and Indiv Differences. 2009;46:454–459. doi: 10.1016/j.paid.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]