Abstract
OBJECTIVE
To describe the presenting symptoms of women with depression in two obstetrics and gynecology clinics, determine depression diagnosis frequency, and examine factors associated with depression diagnosis.
METHODS
Data were extracted from charts of women screening positive for depression in a clinical trial testing a collaborative care depression intervention. Bivariate and multivariable analyses examined patient factors associated with the diagnosis of depression by an obstetrician–gynecologist (ob-gyn).
RESULTS
Eleven percent of women with depression presented with a psychologic chief complaint but another 30% mentioned psychologic distress. All others noted physical symptoms only or presented for preventive care. Ob-gyns did not identify 60% of women with a depression diagnosis. Depression severity was similar in women who were or were not diagnosed by their ob-gyns. Bivariate analyses showed four factors significantly associated with depression diagnosis: reporting a psychologic symptom as the chief complaint or associated symptom (72% compared with 18.6%, P<.001), younger age (35.5 years compared with 40.8 years, P<.005), being within 12 months postpartum (13.9% compared with 2.8%, P<.005), and a primary care-oriented visit (72% compared with 30%, P<.001). Multivariable analysis showed that reporting a psychologic symptom (adjusted odds ratio [OR] 8.90, 95% confidence interval [CI] 4.15–19.10, P<.001), a primary care oriented visit (adjusted OR 2.46, 95% CI 1.14–5.29, P=.03), and each year of increasing age (adjusted OR 0.96, 95% CI 0.93–0.96, P=.02) were significantly associated with a depression diagnosis.
CONCLUSION
The majority of women with depression presented with physical symptoms; most women with depression were not diagnosed by their ob-gyn, and depression severity was similar in those diagnosed and those not diagnosed.
Approximately one third of women in the United States regard their obstetrician–gynecologist (ob-gyn) as their primary care physician.1 Ob-gyns estimate that 37% of nonpregnant patients receive primary care solely in obstetrics and gynecology settings2 and one third of clinical visits for women younger than age 65 years is provided by ob-gyns.3 Therefore, ob-gyns are likely to encounter one of the most frequent clinical problems women experience: depression.
Depression occurs in approximately 21% of women over their lifetime,4,5 often during adolescence, early adulthood, or key developmental periods such as the postpartum6 and menopausal periods.7 The estimated depression prevalence in women attending obstetrics and gynecology clinics ranges from 4% to 22%.8–10 Despite this high prevalence, several studies have shown that in obstetrics and gynecology clinics, only 20–33% of patients with depression are accurately diagnosed.8,9 Most patients with depression in primary care present with somatic symptoms such as headache,11,12 and these patients are less likely to be diagnosed accurately compared with patients presenting with depression symptoms.
This study described the presenting symptoms of women screening positive for depression in obstetrics and gynecology settings, determined how often women with depression are diagnosed, and examined what factors were associated with the diagnosis of depression by the clinician. By enhancing understanding of symptoms depressed women present with and the variables associated with diagnosis, this study may help improve ob-gyns’ recognition of depression.
MATERIALS AND METHODS
The Depression Attention for Women Now study was a randomized, controlled clinical trial testing whether a collaborative care13 depression intervention delivered in an obstetrics and gynecology setting improved depression and functional outcomes and satisfaction with depression care in women randomized to the intervention arm compared with usual obstetric and gynecologic care. A sample size of 188 patients was needed to have 80% power to detect an effect in depression outcomes measured by the SCL-20 with a 5% significance level. Additional details of the Depression Attention for Women Now study design are described elsewhere.14 This study was approved by the institutional review board at the University of Washington School of Medicine.
The Depression Attention for Women Now study was conducted in two urban, academic obstetrician and gynecology clinics at the University of Washington in Seattle. The Harborview Women's Clinic is located in Harborview Medical Center. Harborview Medical Center is a King County Hospital that provides care predominantly to underserved, uninsured, and immigrant populations from largely lower socioeconomic backgrounds with diverse racial and ethnic groups. The University of Washington Roosevelt Women's Health Care Center largely provides care to a commercial, state, or federally insured population from mixed socioeconomic strata. Both sites provide primary, obstetric, and gynecologic care and are staffed by obstetrics and gynecology faculty and residents from the University of Washington.
English-speaking women at least 18 years of age were recruited between November 2009 and December 2011. Patients attending scheduled clinical appointments were approached by one of two full-time research assistants to determine level of interest in the study. Interested patients were screened for depression using the Patient Health Questionnaire-9.15 The Patient Health Questionnaire has been validated and used in many clinical trials of depression and accurately tracks response to treatment over time.15 In the obstetrics and gynecology setting, a Patient Health Questionnaire score of 10 has been shown to have 75% sensitivity and 90% specificity to a diagnosis of major depression by structured psychiatric interview.8 Those with Patient Health Questionnaire scores 10 or higher completed a 20-minute eligibility assessment either in person or by telephone, which verified diagnosis of major depression, dysthymia (chronic depression for over 2 years), or both with a structured psychiatric interview. Women were excluded if they had one or more of the following characteristics: homelessness, substance misuse within the last 6 months, history of bipolar disorder, schizophrenia, two or more psychiatric hospitalizations, current interpersonal partner violence, a score of 3 on item 9 of the Patient Health Questionnaire (suicidal ideation over the preceding 2 weeks), or had been hospitalized more than once for a suicide attempt. As part of the randomized controlled trial, women were asked whether they had ever received prior treatment with medications for depression, anxiety, or sleep problems.
The electronic medical records of all women enrolled in the intervention or control arms were reviewed in September 2012. Two sources were used to obtain clinical information: the clinical note from the day of study entry and the subsequent follow-up note from the same clinic. In a small minority of patients, one of the clinical notes made reference to a more detailed note authored by the same clinician and in those circumstances that note was also accessed. Data were extracted from the two clinical notes on the type of care provided to the patient (primary or specialty care), visit type (initial visit or follow-up), presenting symptoms or problems, chronic medical illness history, clinicians’ diagnoses, and whether depression or anxiety was mentioned in either of the two notes.
Two authors (J.M.C. and E.R.V.) abstracted clinical data from 10 women together to reach agreement on how to classify information found in the clinical notes. Diagnostic disagreements were resolved through discussion with the larger group of authors. The two authors divided the remaining women and individually abstracted data onto the collection form for each woman. Abstracted data for all women were entered into an Excel spreadsheet by two authors. This technique permitted further discussion of abstraction disagreements, which were then resolved through reexamination of the electronic medical record and discussion with clinical experts. The total number of reported symptom categories was determined by combining the chief complaint and all reported associated symptoms for each patient.
The chief complaint, associated problems, and chronic medical illnesses were taken directly from the two chart notes and entered into the data collection tool for each patient. Only one chief complaint was assessed for each patient. However, there was no limit to the number of associated symptoms or chronic medical problems each patient could have entered into the data collection form. The chief complaint was generally listed in the first line of the clinical note either as a “reason for visit” or “chief complaint.” The clinical notes did not follow a template design, although the associated symptoms and chronic medical illnesses were generally listed in the “subjective” portion of the note or a separate “medical history” section.
Diagnosis was obtained from the two clinical notes reviewed for each patient. The diagnosis was usually found in the “impression” part of the note and was subsequently put onto the data extraction form. There was no limit to the number of diagnoses that could be recorded for each patient.
After completing the chart review on all patients, the chief complaints, associated symptoms, chronic medical illnesses, and diagnoses for all patients were coded into one of 10 categories: psychological; health maintenance or establish care; medical nonpain (ie, dyspnea); obstetric; gynecology-related nonpain symptom; abnormal uterine bleeding; vulvovaginal complaints; gynecology-related pain syndrome; medical pain syndrome (ie, irritable bowel syndrome); or other pain (ie, back pain). This decision process was informed by the literature and by expert clinical experience in clinical obstetrics and gynecology (S.R. and J.M.) and psychiatry (W.K. and C.C.).
The type of visit (primary or specialty care) was determined after reading the entire clinical note. Specialty care visits were defined as visits with a clear consultation request documented in the note, presurgical or postsurgical visits, or evidence that the patient was referred by another physician. Patients who routinely saw the ob-gyn but had documentation of a different primary care physician were classified as having received specialty obstetrics and gynecology care. All other services, including obstetric care, were considered primary care. Consensus regarding data collection methodologies was carefully reviewed before data abstraction. Whether the patient's visit was an initial visit or follow-up visit was also determined after reading the clinical note. Follow-up visits were generally described as such by the clinician, and initial visits generally involved a more comprehensive history compared with follow-up visits. In rare circumstances in which visit status was unclear, the investigators examined several notes to see whether the clinician had written a clinical note previously.
Descriptive statistics were used to characterize the sample and women with and without an ob-gyn diagnosis of depression. χ2 tests for categorical variables and t tests for continuous variables were used for between-group comparisons. A multivariable logistic regression model was used to estimate the odds ratios of having an ob-gyn diagnosis of depression. Variables that were significantly (P<.05) different between the groups in the bivariate analyses (age, postpartum status, service type, and psychologic complaint status) were included simultaneously in the multivariable model. Individual variables were removed if they did not contribute significantly (P<.05) to the model. Analyses were completed using SPSS 19.0.
RESULTS
Patients had a mean age of 38.6 years, 69% were white, almost half were married, and 85% had completed 1 or more years of college (Table 1). Forty-two percent of the women had private insurance, 30.3% were uninsured, 19% had Medicaid, 5.6% had Medicare, and 2.6% had state insurance. Structured interview verified that 98.5% of patients had a current major depression diagnosis. Over 60% of women reported that they had received prior medication treatment for depression, anxiety, or sleep problems. A total of 82 (42%) of the 195 patients were diagnosed with depression by the obgyn clinician. Patient Health Questionnaire scores did not differ between those women with and without an ob-gyn diagnosis of depression (mean±standard deviation 16.7±4.3 compared with 15.9±3.9).
Table 1.
Characteristics of Women With Depression Without and With Depression Diagnoses Made by Obstetrician-Gynecologists
| Characteristic | Total Sample (N = 195) | No Ob-Gyn Depression Diagnosis (n=113) | Ob-Gyn Depression Diagnosis (n=82) | P |
|---|---|---|---|---|
| Demographic information | ||||
| Age (y) | 38.6±12.0 | 40.8±12.3 | 35.5±10.8 | .002* |
| Race or ethnicity | ||||
| White | 134 (68.7) | 80 (70.8) | 54 (65.9) | .46† |
| Latina or Hispanic | 18 (9.3) | 10 (9) | 8 (9.8) | .86† |
| Married | 93 (47.7) | 49 (43.4) | 44 (53.7) | .16† |
| Some college education | 167 (85.6) | 100 (88.5) | 67 (81.7) | .18* |
| Clinical information | ||||
| Pregnant | 9 (4.6) | 6 (5.4) | 3 (3.7) | .42† |
| Postpartum within 12 mo | 14 (7.5) | 3 (2.8) | 11 (13.9) | .004† |
| Prior medication for depression, anxiety or sleep | 167 (61.3) | 56 (59.6) | 39 (63.9) | .36† |
| Patient Health Questionnaire-9 score | 16.2±4.0 | 15.9±3.9 | 16.7±4.3 | .18* |
| Current major depression on structured interview | 191 (98.5) | 109 (97.3) | 82 (100) | .14† |
| Current dysthymia on structured interview | 65 (33.7) | 24 (29.3) | 36.9% (41) | .27† |
| 41 (36.9) | ||||
| Service type | ||||
| Primary care | 93 (47.7) | 34 (30.1) | 59 (72) | .001† |
| Gynecology specialty | 102 (52.3) | 79 (69.9) | 23 (28) | |
| Visit type | ||||
| Initial | 72 (36.9) | 40 (35.4) | 32 (39) | .60† |
| Follow-up | 123 (63.1) | 73 (64.6) | 50 (61) | |
| Presenting chief complaint or associated problem categories | ||||
| Psychologic | 21 (18.6) | 59 (72) | .001† | |
| Pain | 54 (47.8) | 31 (37.8) | .165† |
Ob-gyn, obstetrician-gynecologist.
Data are mean±standard deviation or n (%) unless otherwise specified.
t test.
χ2 test.
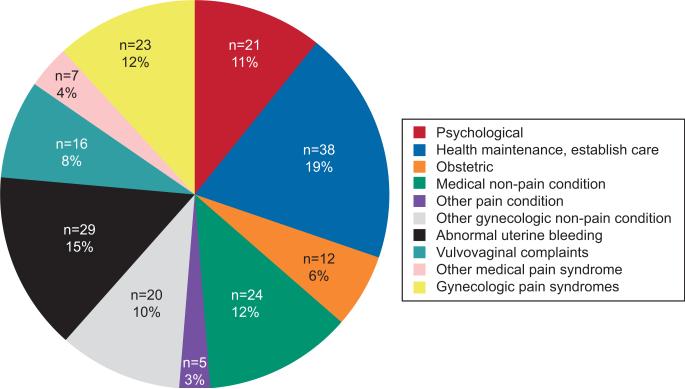
The number and percentage of patients reporting each category of problem as the chief complaint is shown in Figure 1. Only 11% of all patients with depression presented with a psychologic chief complaint; however, approximately 40% had some mention of psychologic distress either as a chief complaint or as an associated symptom in one of the ob-gyn notes. Psychologic complaints included specific symptoms of depression (eg, depressed mood), anxiety symptoms, or nonspecific evidence of distress such as a report of “stress.” Pain-related chief complaints (19%) and visits to establish care or for an annual health maintenance examination (19%) occurred almost twice as often as visits where the chief complaint was psychologic (11%).
Fig. 1.
Presenting chief complaint categories for all patients (N=195).
Cerimele. Presentation of Depression. Obstet Gynecol 2013.
Bivariate analyses found four variables significantly associated with a depression diagnosis by the ob-gyn including younger age (35.5 years compared with 40.8 years, P<.005), being within 12 months postpartum (13.9% compared with 2.8%, P<.005), receiving primary rather than specialty care (72% compared with 30%, P<.001), and reporting a psychologic complaint either as a chief complaint or associated symptom (72% compared with 18.6%, P<.001) (Table 1). Multivariable analysis that included these four variables found that reporting a psychologic complaint either as a chief complaint or associated symptom (adjusted odds ratio [OR] 8.90, 95% confidence interval [CI] 4.15–19.10, P<.001) and receiving primary rather than specialty care (adjusted OR 2.46, 95% CI 1.14–5.29, P=.03) were significantly associated with a depression diagnosis. Age was also significant in the model such that each additional year of age was associated with a 4% decrease in diagnosis (adjusted OR 0.96, 95% CI 0.93–0.96, P=.02).
We explored reasons for age being associated with depression diagnosis and found that pregnant or postpartum patients (12%, n=23) who are likely to have more clinic visits were younger overall compared with nonpregnant or postpartum patients (31.0±4.9 years compared with 39.8±12.2 years). Older patients (aged 40 years or older) were found to have a significantly higher number of chronic medical problems (2.6±1.8) compared with younger women (younger than 40 years) (1.5±1.5) (P<.001), which may distract from making a depression diagnosis.
DISCUSSION
We found that women screening positive for clinically significant depressive symptoms in an obstetrics and gynecology setting were more likely to have a physical, rather than a psychologic, chief complaint. Approximately 40% of patients received a depression diagnosis and depression severity was similar in women who were and were not diagnosed. Multivariable analysis found that the odds of receiving a depression diagnosis increased in those reporting a psychologic symptom and those receiving primary care services. Each year of increased age was significantly associated with a 4% decrease in diagnosis.
This study's detection rate of approximately 40% is higher than the 20–33% rate in a prior study of depression detection in an obstetrics and gynecology setting8 but lower than the detection rate of approximately 50% reported in other primary care settings. The detection rate from this study may have been higher than in other obstetrics and gynecology settings because the two sites in our trial provide primary care services for many patients.
Previous studies demonstrated that primary care patients with depression often present with physical symptoms.11,16,17 We found that only 11% of women with depression reported a chief complaint of depressive symptoms, although an additional 30% reported an associated psychologic symptom. Thus, over half of women with depression did not report psychologic symptoms, which were found to influence ob-gyn diagnosis. Of those diagnosed with depression, approximately 72% had a psychologic complaint either as a chief complaint or as an associated symptom. These findings suggest that many obstetrics and gynecology patients with depression are unlikely to be diagnosed with depression unless asked directly about depressive symptoms.
It is not surprising that patients seen for primary care services were more likely to receive a depression diagnosis than patients seen for specialty care services. Primary care services include attention to a range of needs, which increases a patient's exposure to the physician and the chance of recognition of depression, whereas specialty consultations focus on a narrower scope of problems in a limited number of visits.
Several reasons may explain why increasing age was associated with decreased depression diagnosis. First, psychiatric illness stigma is lower in younger compared with older patients suggesting that younger patients might be more likely to report symptoms and willing to discuss depression.18 Second, younger patients were more likely to present with pregnancy and have obstetric follow-up visits compared with older patients. General obstetric practice often includes multiple physician visits, and guidelines recommend depression screening in pregnant or postpartum women, both of which could have increased depression recognition in younger patients. Third, compared with younger patients, older patients had more chronic medical problems, which has been associated with lower odds of depression being recognized and treated.19
Ob-gyns recognize the importance of treating depression, although many perceive difficulties associated with depression screening in practice.20 Our study used the Patient Health Questionnaire-9 depression screening measure,15 which can be filled out in a few minutes by the patient or administered by clinic staff. Excluding the perinatal period,21 no guidelines recommend screening for depression in obstetrics and gynecology settings. The U.S. Preventive Services Task Force recommends primary care depression screening when a system exists to confirm the diagnosis and provide evidence-based treatments.22 The importance of recognition and treatment of depression is shown by its association with functional impairment, lack of self-care for chronic medical illnesses, amplification of medical symptoms such as pain, and increased medical costs.23 There is a higher prevalence of depression in low-income and minority women and these patients often receive their only medical care in an obstetrics and gynecology setting,10 and many women consider their ob-gyn as their primary care physician.1 For these women, the only opportunity for diagnosis and treatment of depression may be in the obstetrics and gynecology setting.
Our study has several limitations. First, the study population was from two university-based clinics, limiting our findings’ generalizability to nonacademic settings. Second, clinical information not documented in the notes may have been missed, potentially leading to misclassification. Third, clinicians in the study clinics knew the depression clinical trial was underway and some clinicians may have become aware of the results of the Patient Health Questionnaire-9 screen for their patients, potentially causing an overestimate of the detection rate. Fourth, patients with depression were not compared with those without depression, so we cannot comment on presenting symptom differences between these two groups. Finally, our results are not generalizable to the subgroups of women excluded from the clinical trial.
Acknowledgments
Supported by grants from the National Institute of Mental Health (R01-MH085668 and 5T32-MH020021-15).
The authors thank Erin McCoy, MPH, for figure preparation.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Scholle SH, Kelleher K. Assessing primary care performance in an obstetrics/gynecology clinic. Women Health. 2003;37:15–30. doi: 10.1300/J013v37n01_02. [DOI] [PubMed] [Google Scholar]
- 2.Coleman VH, Laube DW, Hale RW, Williams SB, Power ML, Schulkin J. Obstetrician-gynecologists and primary care: training during obstetrics-gynecology residency and current practice patterns. Acad Med. 2007;82:602–7. doi: 10.1097/ACM.0b013e3180556885. [DOI] [PubMed] [Google Scholar]
- 3.Scholle SH, Chang JC, Harman J, McNeil M. Trends in women's health services by type of physicians seen: data from the 1985 and 1997-98 NAMCS. Womens Health Issues. 2002;12:165–77. doi: 10.1016/s1049-3867(02)00139-1. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSMIII-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 6.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–83. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 7.Cohen LS, Soares CN, Vionis AF, Otto MW, Harlow BL. Risk of new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63:385–90. doi: 10.1001/archpsyc.63.4.385. [DOI] [PubMed] [Google Scholar]
- 8.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 9.Smith MV, Rosenheck RA, Cavaleri MA, Howell HB, Poschman K, Yonkers KA. Screening for and detection of depression, panic disorder and PTSD in public-sector obstetric clinics. Psychiatr Serv. 2004;55:407–14. doi: 10.1176/appi.ps.55.4.407. [DOI] [PubMed] [Google Scholar]
- 10.Miranda J, Azocar F, Komaromy M, Golding JM. Unmet mental health needs of women in public-sector gynecologic clinics. Am J Obstet Gynecol. 1998;178:212–7. doi: 10.1016/s0002-9378(98)80002-1. [DOI] [PubMed] [Google Scholar]
- 11.Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–41. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg D, Bridges K, Duncan-Jones P, Grayson D. Detecting anxiety and depression in general medical settings. BMJ. 1988;297:897–9. doi: 10.1136/bmj.297.6653.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight LR, et al. Community Preventive Services Task Force. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42:525–38. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 14.LaRocco-Cockburn A, Reed SR, Melville J, Croicu C, Russo J, Inspektor M, et al. Improving depression treatment for women: integrating a collaborative care depression intervention into Ob-Gyn care. Contemp Clin Trials. doi: 10.1016/j.cct.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg DP, Bridges K. Somatic presentations of psychiatric illness in primary care setting. J Psychosom Res. 1988;32:137–44. doi: 10.1016/0022-3999(88)90048-7. [DOI] [PubMed] [Google Scholar]
- 17.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–35. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 18.Roeloffs C, Sherbourne C, Unutzer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiatry. 2003;25:311–5. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- 19.Rost K, Nutting P, Smith J, Coyne JC, Cooper-Patrick L, Rubenstein L. The role of competing demands in the treatment provided primary care patients with major depression. Arch Fam Med. 2000;9:150–4. doi: 10.1001/archfami.9.2.150. [DOI] [PubMed] [Google Scholar]
- 20.LaRocco-Cockburn A, Melville J, Bell M, Katon W. Depression screening attitudes and practices among obstetrician-gynecologists. Obstet Gynecol. 2003;101:892–8. doi: 10.1016/s0029-7844(03)00171-6. [DOI] [PubMed] [Google Scholar]
- 21.Screening for depression during and after pregnancy. Committee Opinion No. 453. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2010;115:394–5. doi: 10.1097/AOG.0b013e3181d035aa. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Preventive Services Task Force Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136:760–4. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 23.Katon W. Epidemiology and treatment of depression in patients with chronic medical illnesses. Dialogues Clin Neurosci. 2011;13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]